Failure to adhere to antipsychotic and rehabilitative treatment programmes as a result of poor insight contribute to a poorer outcome in schizophrenia (Reference Bartko and ZadorBartkó & Zádor, 1988; Reference SchwartzSchwartz, 1997). Psychoeducational materials (Reference Pekkala and MerinderPekkala & Merinder, 2001) and cognitive—behavioural therapy (CBT; Reference Tarrier, Beckett and HarwoodTarrier et al, 1993) have been developed to improve understanding and facilitate enhanced coping. Cognitive—behavioural therapy aimed at improving adherence to medication has been shown to be effective (Reference Kemp, Hayward and ApplewhaiteKemp et al, 1996) and durable (Reference Kemp, Kirov and EverittKemp et al, 1998). Controlled studies of CBT have shown increased benefit in the treatment of positive symptoms (Reference Tarrier, Yusupoff and KinneyTarrier et al, 1998) and also in negative symptoms (Reference Sensky, Turkington and KingdonSensky et al, 2000). This study set out to test whether the benefits that accrue in terms of improvement in the symptoms of schizophrenia with highly trained, skilled therapists can be replicated in the community when the intervention is delivered by non-expert therapists who received a brief training programme (Reference Jones, Cormac and MotaJones et al, 1999).
METHOD
Study population
Lists of patients with schizophrenia receiving treatment within psychiatric secondary care services and within the age range 18-65 years were constructed at six sites in the UK (Belfast, Glasgow, Hackney, Newcastle, Southampton and Swansea) according to the ICD—10 (World Health Organization, 1992) research criteria. The null hypotheses being tested in this study were a prediction of no difference in outcome, either statistical or in terms of clinical significance, between the two groups at follow-up on overall symptoms, insight, depression, symptoms of schizophrenia and burden of care.
Sampling method
The lists were compiled from in-patient and out-patient case lists, depot and clozapine clinics, mental health keyworkers and Care Programme Approach registers. Any patient who was deteriorating and who needed in-patient care or intensive home treatment was excluded from the study. Similarly, any patient with a primary diagnosis of drug or alcohol dependence, organic brain disease or learning disability severe enough to interfere with rating was excluded from entry. Responsible medical officers and keyworkers were approached to seek permission for the inclusion of their patients and carers in the study. Where permission was given, the case notes were fully perused and the patients were approached by the community psychiatric nurse (CPN) employed at each site. Patients were randomised only after they had given full consent. Randomisation was conducted by computer-generated blocks of six random numbers and stratified by site. The results were placed in sealed envelopes and only opened at the time of treatment allocation. The ratio of active intervention to treatment as usual (TAU) was 2:1. This was done to improve recruitment and allow inter-site comparisons. All TAU patients were told that they would receive the CBT intervention at the end of the follow-up rating period. A power calculation based on a pilot study (Reference Turkington and KingdonTurkington & Kingdon, 2000) predicted that with 90 patients at each site (60 receiving the intervention and 30 receiving treatment as usual) and assuming a 20% drop-out rate, there was a 90% chance of detecting a 25% difference in overall symptomatology at the 0.01% level of significance, should such a difference exist.
Assessments
Independent raters (psychiatrists, nurses and psychologists) were trained together at the start of the study to ensure interrater reliability across sites. The intraclass correlation coefficient on measuring overall symptoms was acceptable at 0.71. Baseline demographic characteristics recorded at study entry included age, gender, ethnic group, marital status, employment status and housing status. All patients were seen initially for consenting by the centre's therapist and asked not to reveal or even hint at their treatment allocation to the raters. Raters were informed that some study material would be left with TAU patients to help to preserve the blindness of the ratings.
Standardised measures were used to assess the primary outcomes of the study at baseline and at the end of therapy (mean 20 weeks). The primary outcome measures were of overall symptomatology (Comprehensive Psychopathological Rating Scale, Reference Åsberg, Montgomery and PerrisÅsberg et al, 1978), insight (Insight Rating Scale; Reference DavidDavid, 1990) and carer burden (Burden of Care Questionnaire; Reference Mueser, Webb and PfeifferMueseret al, 1996). Secondary outcome measures included change in schizophrenic symptoms (Schizophrenia Change Scale; Reference Montgomery, Taylor and MontgomeryMontgomery et al, 1978) and depression (Montgomery—Åsberg Rating Scale; Reference Montgomery and ÅsbergMontgomery & Åsberg, 1979). Measures of patient and carer satisfaction were devised for the purposes of this study. For the patient, the questions covered issues such as quality of therapy relationship, understanding, coping, mood and overall satisfaction. The carer satisfaction questionnaire contained similar questions to be answered in relation to their role as carer. The questions were answered on a seven-point visual analogue scale. Results were sent from each of the six sites to an independent central database for data entry and independent statistical analysis. Details of medication, converted to chlorpromazine equivalents using the World Health Organization's Anatomical Therapeutic Chemical Classification System (World Health Organization, 1993) in the case of typical neuroleptics, along with the number of atypical neuroleptics and pre-study hospitalisation, were taken from the medical case notes. These were then rechecked at the end of the study period to check for any significant differences between the groups. Further assessments of primary outcome scales and of rehospitalisation will be carried out on all groups 9 months after the end of therapy to ascertain whether the effects of treatment are durable.
Treatment groups
For delivery of the active intervention, CPNs received 10 days of intensive training in the use of CBT. The manual was developed from an original description of these strategies (Reference Kingdon and TurkingtonKingdon & Turkington, 1994) and abbreviated into a phased approach designed to be supplemented by specific written material. The CPNs were trained by experts in CBT (D. T. and D. K.) and were tested on their skills through demonstration, role play and written examination. Supervision was provided by a variety of methods during the study, including individual, group and telephone. Patients in the CBT group saw the nurse for a total of up to six hour-long sessions over a period of two or three months. If the patient's carer agreed to take part in the programme, he or she received a total of three sessions over the same time period. Patients who attended less than three CBT sessions were classified as drop-outs.
All the phases of CBT were included in the brief approach, including assessment and engaging, developing explanations, case formulation, symptom management, adherence, working with core beliefs and relapse prevention. In conjunction with the phased approach, and integral to each session, were a series of ten specially developed educational booklets — five for patients and five for carers. The booklets covered treatment, self-care and lifestyle, leisure time and relationships, drug and alcohol advice, symptom management and sources of help, and were worked through in a flexible manner according to the patient's and carer's individual needs. Appropriate homework was generated. All of the patients were treated in the community or, if appropriate, following attendance at depot clinic, community mental health team or out-patient appointments. Carers were seen most often in the family home.
The patients and carers randomised to receive treatment as usual were left to the care of their own community mental health teams but were aware that CBT would be offered at the end of the study period. All assessments carried out in the intervention group were also completed in this group.
Treatment fidelity
All sessions were audiotaped when patients agreed to this. Independent evaluation of a stratified sample of tapes was carried out using the cognitive therapy scale modified for psychosis (Reference Haddock, Devane and BradshawHaddock et al, 2001). A cut-off score of 30 was taken as indicating acceptable quality of therapy analysis. This revealed that the vast majority of sessions were above this level (mean=38.84, 95% CI 35.78-41.9).
Statistical analysis
Results were analysed using SPSS version 10 and Stata version 6 on an intention-to-treat basis. Differences between the two groups were assessed using analysis of covariance and chi-squared tests, with risk ratios calculated for categorical variables. Tests of skewness and normality across clinical variables were within acceptable limits. Primary and secondary outcome measures were assessed in relation to whether there was a significant difference using intention-to-treat (n=422) analysis of covariance. The covariates used were treatment group and baseline measurements for the corresponding dependent variables. Post therapy, missing data were estimated by calculating the respective post-therapy group means of those patients who returned for follow-up. These means were entered for those patients who dropped out. The level of improvement in the main outcome measures indicating a good clinical improvement was taken as 25%. This was decided on an a priori basis in relation to other published work. Analysis of clinically significant results was then carried out using chi-squared tests.
RESULTS
The characteristics of the patient sample are described in Table 1. There were no statistically significant baseline differences between the groups. Severity, as estimated by number of previous relapses and by number of previous days in hospital for schizophrenia, was not statistically significantly different between the groups. The CBT intervention group had a mean of 4.71 previous admissions for schizophrenia (95% CI 4.09-5.33) with a mean number of previous days in hospital for schizophrenia of 48.53 (95% CI 37.84-59.21). In comparison, the TAU group had a mean of 5.18 admissions (95% CI 4.33-6.03) and 52.01 days in hospital (95% CI 37.94-66.07). Medication dose as given by chlorpromazine equivalence and use of atypical neuroleptics was not statistically significantly different between the two groups. The CBT intervention group had a mean figure for chlorpromazine equivalence of 746.88 mg (95% CI 602.79-890.96) and the TAU group of 886.58 mg (95% CI 660.72-1112.44). Of those on atypical neuroleptics, 55 were in the CBT intervention group and 25 in the TAU group.
Table 1 Characteristics of patient sample
| Characteristic | Number | % |
|---|---|---|
| Gender | ||
| Male | 325 | 77.01 |
| Female | 97 | 22.99 |
| Age (years) | ||
| Mean (95% CI) | 40.47 (39.78-41.88) | |
| Marital status | ||
| Single | 300 | 71.09 |
| Married | 58 | 13.74 |
| Divorced/widowed | 64 | 15.17 |
| Ethnic group | ||
| White | 358 | 88.90 |
| African—Caribbean | ||
| Black African | 42 | 7.40 |
| Black other | ||
| Asian other | 22 | 3.10 |
| Employment status | ||
| Unemployed | 371 | 88.00 |
| Full/part time | 13 | 3.00 |
| Sheltered workshop | 12 | 2.84 |
| Other | 26 | 6.16 |
| Housing status | ||
| Independent | 190 | 45.02 |
| Family | 111 | 26.30 |
| Staffed home | 91 | 21.56 |
| Unstaffed home | 21 | 4.98 |
| Homeless/unknown | 9 | 2.13 |
| Carer participation | ||
| Treated with carer | 97 | 43.10 |
| Treated without carer | 128 | 56.90 |
Statistically significant improvements were seen in the CBT intervention group compared with the TAU group (Table 2) in overall symptoms, insight and depression. Of the primary outcome measures, insight, but not overall symptomatology, was clinically significantly improved by CBT compared with treatment as usual (risk ratio=1.15; 95% CI 1.01-1.31). The number needed to treat (NNT; Reference Laupacis, Sackett and RobertsLaupacis et al, 1988) in relation to a good clinical outcome on insight improvement was 10. The NNT for improvement in overall symptoms was 13.
Table 2 Baseline scores (mean and 95% CI) and change scores (mean and 95% CI) after treatment
| Measure | Cognitive—behavioural therapy intervention | Treatment as usual | Comparison of change scores (ANCOVA) | ||
|---|---|---|---|---|---|
| Baseline score | Change score | Baseline score | Change score | Mean difference | |
| Overall symptomatology | 23.27 (21.64-24.9) | 3.65 (2.42-4.88) | 24.30 (22.11-26.49) | 1.69 (-0.04 to 3.34) | -2.29 (P=0.015) |
| Insight1 | 8.72 (8.33-9.10) | -1.16 (-1.57 to 0.75) | 8.68 (8.18-9.18) | 0.12 (-0.39 to 0.63) | 1.30 (P<0.001) |
| Depression | 5.44 (4.93-5.94) | 0.83 (0.38-1.27) | 6.08 (5.38-6.79) | 0.29 (-0.29 to 0.86) | -0.87 (P=0.003) |
| Symptoms of schizophrenia | 5.26 (4.72-5.81) | 0.58 (0.14-1.02) | 5.50 (4.79-6.20) | 0.33 (-0.24 to 0.89) | -0.35 (P=0.258) |
| Burden of care | 76.48 (71.46-81.51) | -2.17 (-0.69 to 5.02) | 81.84 (73.33-90.35) | -1.01 (-6.76 to 4.75) | -4.25 (P=0.126) |
Most patients were satisfied with the programme, and nearly 57% rated the overall programme as ‘it has helped me more than anything previously to understand my illness’. The median total patient satisfaction score was 44 out of a possible 49, and one-third of the 132 patients who completed the questionnaire gave maximum points. Of the 45 carers who completed the questionnaire, over three-quarters were satisfied with the programme. The median total carer satisfaction score was 47 out of 49.
There were no significant differences by the end of the intervention in symptoms of schizophrenia or burden of care on comparing the two groups (Table 2). Also, there was no significant difference between therapists who delivered an intervention of an acceptably high quality. There was a non-significant 3% improvement in the group of patients who had a carer involved compared with those who had no carer involved, indicating no specific benefit by end of therapy analysis. There was one suicide during the treatment period; this occurred in the TAU group. In general, there was no evidence of increased suicidal ideation with improving insight in either group.
Recruitment and drop-out details are presented in Fig. 1. It is of note that there were significantly more drop-outs in the TAU group (22.4%) than in the CBT intervention group (12.5%; P<0.05). Dropouts were not more likely to be more severely ill, less insightful or more depressed, but there was a statistically significantly increased drop-out rate in those patients who were not White (P<0.0001). This group mostly comprised African—Caribbean and Black African patients.
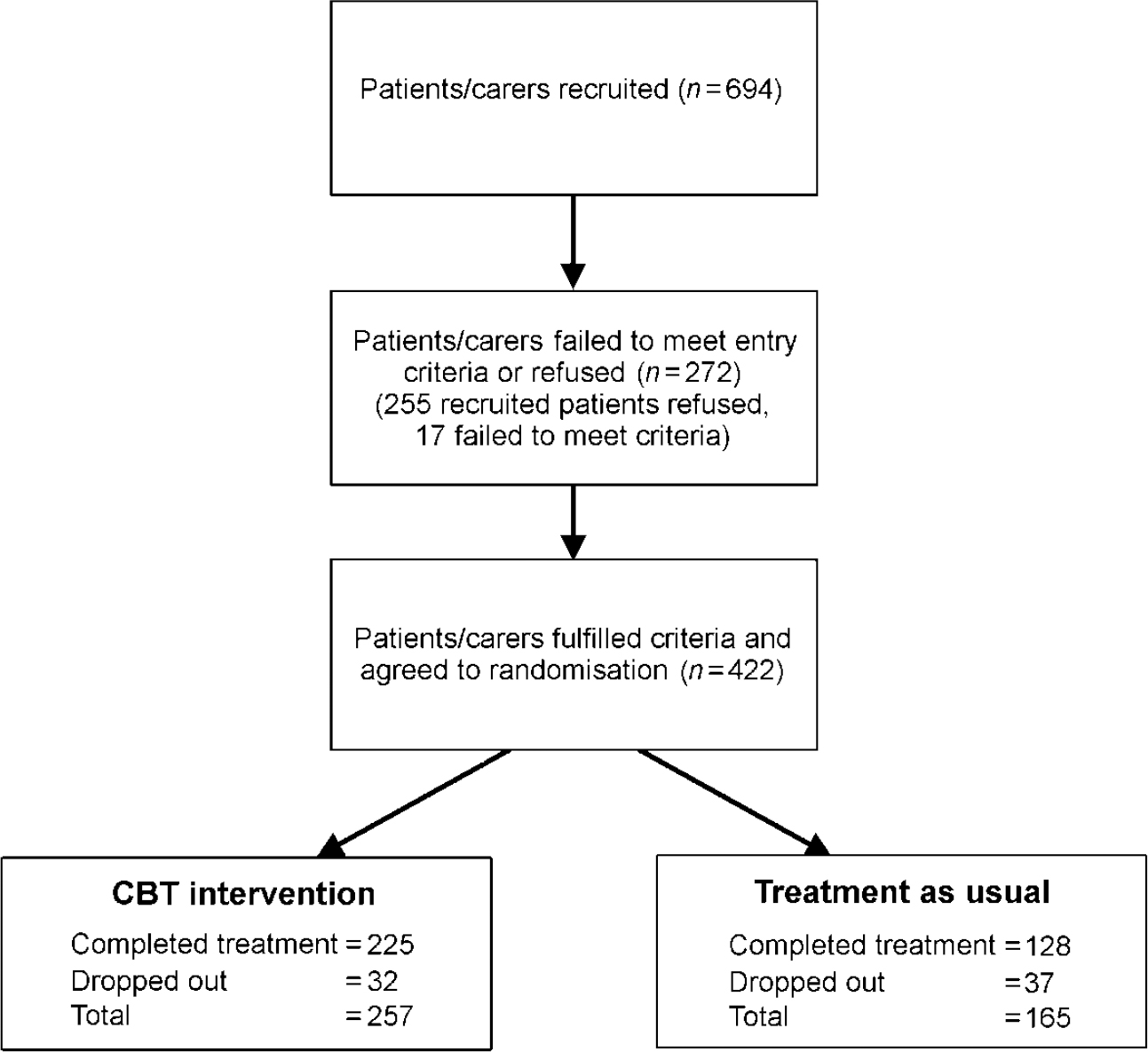
Fig. 1 Flow chart showing patient recruitment and treatment allocation.
DISCUSSION
Our study shows that a brief CBT intervention, along with psychoeducational materials, can be delivered by CPNs in the community with the help of carers to achieve symptomatic improvement without increasing suicidality. Overall symptomatology, insight and depression were significantly improved in the CBT group as compared to the TAU group. This improvement in insight was clinically significant in the CBT group, which could suggest that patients receiving CBT may show a potential for improved adherence, better use of coping skills and perhaps, in the longer term, reduced length of time in hospital. The NNT of 13 for improvement in overall symptoms was compatible with the results achieved when CBT was delivered by expert therapists (Reference Kuipers, Garety and FowlerKuipers et al, 1997) and better than that of psychoeducation or family therapy alone (NHS Centre for Reviews and Dissemination, 2000). It remains to be seen whether the effects of this briefer intervention will be durable.
Service implications
The benefits as shown here support the further dissemination of psychosocial interventions among CPNs (Reference Haddock, Sellwood and TarrierHaddock et al, 1994) and other mental health care professionals. This study supports the uncontrolled findings from the evaluation of Thorn nursing initiatives, which also showed benefit (Reference Lancashire, Haddock and TarrierLancashire et al, 1997). Engagement rates were very high with CBT and the drop-out rate in the TAU group was almost twice that in the CBT intervention group. The impact of ethnicity on drop-out probably relates to problems in engaging and developing explanations in patients from different cultural backgrounds. It may also point to a need for the psychoeducational materials to be available in a number of different languages. Training in ethnicity awareness issues should be made more widely available for community mental health professionals who are attempting to deliver CBT.
Critical appraisal
This study population is not representative of all patients with schizophrenia but is representative of those patients who are on the case-loads of community mental health team members. There was no difference between the groups at baseline in terms of general characteristics, medication dose or type, or severity of illness as indicated by number of visits or days in hospital. It is clear, therefore, that medication and illness severity are ruled out as confounding factors, which might explain the study results. Similarly, there was no difference in these parameters over the study period. However, the differential drop-out rate between the groups may have influenced these results. It is important to remember that the TAU comparison group does not control for the non-specific effects of the nurse's contact time with the patient. Although attempts were made to protect blinding, there remains the possibility of compromised blinding of ratings due to inadvertent patient disclosure of therapy material.
Implications for carers
Carers were well engaged also and implications for carers displayed high levels of satisfaction with the CBT intervention. The high levels of satisfaction expressed by carers highlight the importance of delivering interventions in which carers feel involved and which do not lead to feelings of alienation. Those patients treated with their carer did not do significantly better than those treated alone. Burden of care was not shown to be improved by the end of therapy, and this mirrors the findings of other studies using this measure (Reference Haddock, Sellwood and TarrierHaddock et al, 1994). However, it is encouraging that such a brief intervention can, in an illness such as schizophrenia, produce a clinically detectable improvement for the patient linked to high carer satisfaction.
Implications for training
Statistically significant improvements in insight occurred in the CBT intervention group compared with the TAU group but importantly, this did not in general lead to an increase in depression or suicidality. However, there was a trend indicating that sudden increases in insight of greater than 25% were to be avoided and needed to be contained within a therapeutic relationship. This issue needs to be stressed further in psychosocial training and risk assessment. It is of interest that the improvements seen did not relate primarily to improvement in psychotic symptoms, but it may well be that follow-up might reveal improvement through the mechanism of improved coping and adherence due to insight improvement. To be able to deliver this intervention, CPNs require 10 days of intensive training combined with weekly supervision. If this was made available, CPNs would be able to deliver brief viable interventions of proven benefit rather than delivering intensive case management, which is known to add little to standard case management. The study supports the general principle contained in the National Service Framework for Mental Health (Department of Health, 1999) of increased training and implementation of high-quality psychosocial interventions in schizophrenia.
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
• Community psychiatric nurses, given training and appropriate supervision, can safely and effectively deliver a brief cognitive—behavioural therapy intervention to patients with stable schizophrenia in a community setting.
-
• Overall symptomatology, insight and depression can be improved in schizophrenia by such a programme without increasing depression or suicidality.
-
• In the future, there may be an increased role for psychological treatments in schizophrenia with greater involvement of carers.
LIMITATIONS
-
• The study used a ‘treatment as usual’ comparison group that did not control for contact time.
-
• Psychotic symptoms were not significantly improved by the end of therapy.
-
• This sample was not epidemiologically representative of all patients with schizophrenia.
Acknowledgements
The members of the Insight into Schizophrenia Research Group are: Glynis Addinell, Noel Armour, Katy Bateman, Alison Brabban, Mark Corrin, Melissa Cunningham, Dr Peter Curran, Tony Davies, Dr Peter Donnelly, Paul French, Penny Giles, Robert Golding, Stef Hackney, Professor David Kingdon, Julia Macleod, Nick Maguire, Joseph McKane, Lisa McNay, Ann Millar, Steve Moorhead, Norma Morgan, Paul Murray, Judy Newman, Jeremy Pelton, Declan Phelan, Ben Pollinger, Dr Shanya Rathod, Annette Scannell, Ron Siddle, Ann Stevenson, Dr Douglas Turkington, Dr Trevor Turner, Jonathan Warren, Stuart Whyte and Dr Alistair Wilson.
We also acknowledge the significant contribution of the Insight into Schizophrenia Advisory Board: Paul Farmer, Jimmy Glass, Richard Gray, Lisa Haywood, Professor Julian Leff, Nigel Maguire, Dr Diana Morrison, Professor David Cunningham Owens, Brian Rogers and Marjorie Wallace.






eLetters
No eLetters have been published for this article.