Introduction
The United States has seen a significant increase in prescription drug misuse, leading to the opioid crisis. In 2020, an estimated 2.7 million people in the United States had an opioid use disorder (OUD). 1 The annual OUD-related cost to the United States was US$786.8 billion in 2018. Reference Murphy2
Despite the attention OUD has received, opioid deaths have significantly increased over the last decade. 3 The emergence of emergency department (ED)-based medication for OUD (MOUD) programs has been beneficial in expanding access to treatment. Reference D’Onofrio, O’Connor and Pantalon4,Reference Reuter, Smith, McKinnon, Varley, Jouriles and Seaberg5 However, there are individuals in the community who are struggling, but for reasons that have not been firmly identified, are simply not connecting with addiction treatment services. Recent reports describing escalating rates of substance abuse Reference Murphy2,3 related to the pandemic highlight the importance of continued programmatic growth to ensure sufficient access to potentially life-saving treatment. However, in the Akron, Ohio area, Emergency Medical Services (EMS) are observing an ever-increasing number of patients who, due to refusing transport after naloxone rescue, represent an access void at the point of overdose. Prehospital initiation of buprenorphine treatment for OUD by paramedics is an emerging potential intervention. Reference Carroll, Wasserman and Shah6,Reference Hern, Lara and Goldstein7 Many patients who may be at high risk for overdose deaths may never engage in treatment because they frequently refuse transport. Recent data have demonstrated a significant increase in both short- and long-term mortality following an opioid overdose. Reference Ashburn, Ryder and Angi8
To address these ongoing challenges, the primary purpose of this study was the development of an interdisciplinary program aimed at expanding access to MOUD through a prehospital setting.
Methods
The interdisciplinary team expanded two hospital based MOUD programs into the prehospital setting through the Akron Fire Department (AFD; Akron, Ohio, USA). The team worked with AFD to identify appropriate patients in real-time for treatment and referral of OUD patients. In 2022, AFD had 45,216 encounters. Of the total calls in 2022, 2.5% were for overdoses. They have several innovative programs that work to engage the community, identify patients for OUD treatment, and reduce EMS and ED visit utilization in this patient population.
The team received an Ohio Department of Health (Columbus, Ohio, USA) grant, which allowed AFD and the two major health systems in Akron that provide MOUD to collaborate. Both hospitals provide addiction care coordinators (ACCs) and peer counselors to help engage patients in their MOUD program. The Summa Health Institutional Review Board approved the program as an exempt quality improvement initiative.
The AFD has a Quick Response Team (QRT) that visits people struggling with OUD to assist in guiding them toward definitive care. The program includes a team comprised of a paramedic, police officer, and Recovery Coach employed by the Summit County Health Department (Akron, Ohio, USA). This team visited eligible patients (i.e., history of an opioid overdose and received prehospital care the previous week and did not have an active warrant for arrest) at the patient’s home every Thursday. To ensure the program’s success, the implementation team developed a prehospital MAT protocol (Figure 1) and a two-hour training course for QRT personnel. Consultation with an ACC and peer counseling was offered to each patient. Each week, AFD had between three to eight opioid overdose patients who received naloxone and were either transported to the hospital or refused transport.
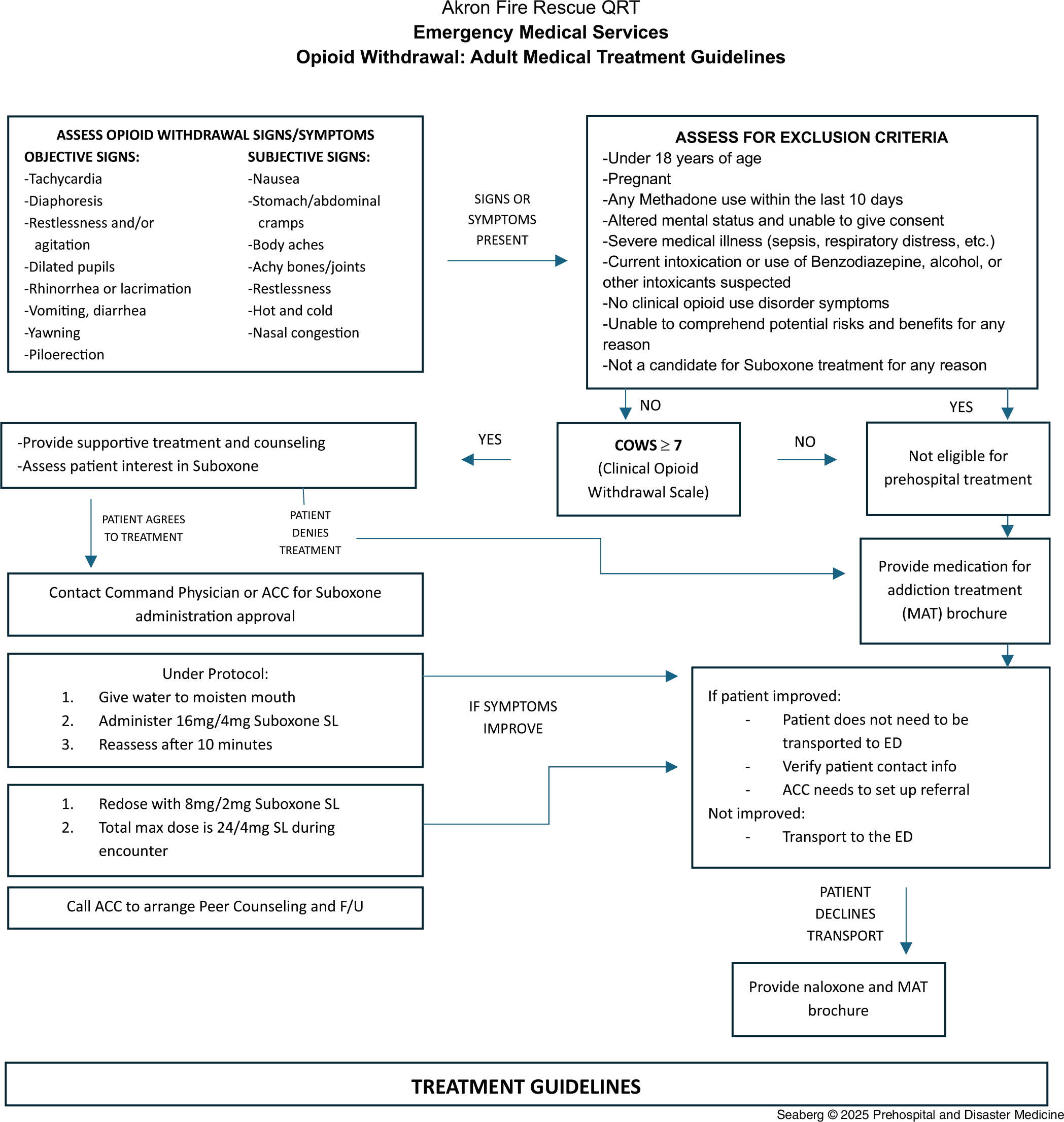
Figure 1. Akron Fire Department Prehospital MOUD Protocol.
Abbreviations: ACC, addiction care coordinator; COWS, clinical opiate withdrawal scale; ED, emergency department; F/U, follow-up; MAT, medication for addiction treatment; MOUD, medication for opioid use disorder; QRT, Quick Response Team.
The implementation steps included six separate components. First, the development of a contract between AFD and the two area hospitals to provide prehospital MOUD was required. Second, QRT protocols were revised to incorporate MOUD. Third, a two-hour mandatory MAT training for the QRT was developed, which included an overview of the MAT program, the pharmacology of MAT programs, a treatment protocol review, patient follow-up education, and data collection through the Research Electronic Data Capture (REDCap) program (Vanderbilt University; Nashville, Tennessee USA). Fourth, a process for telemedicine consults with a hospital-based ACC using iPads (Apple Inc.; Cupertino, California, USA) was developed. Fifth, an application was made to the state for a drug license for the QRT vehicle to carry suboxone. A policy was created for hospital pharmacies to stock and restock suboxone on the QRT vehicle. Lastly, each hospital developed a pamphlet describing their MOUD programs and how to access addiction services if they refused prehospital MOUD.
The effectiveness of the QRT team in enrolling OUD patients in the prehospital MOUD program was evaluated. Outcome metrics included the number of patients seen by the QRT, the number of patients who were enrolled in the prehospital MOUD program, and the number of pamphlets and naloxone kits dispensed. A REDCap electronic survey was developed to collect data on individuals being visited. During the visit, the REDCap survey was used to collect data related to the treatment options that the patient accepted by the QRT member: (1) Patient elected to participate in the treatment program (e.g., spoke to an ACC or was transported to an ED to speak to one); (2) Patient had an ACC virtual visit; (3) Patient was transported to an ED; (4) Patient was administered suboxone; (5) Patient was given a naloxone kit; and (6) Patient connected to a -peer recovery specialist.
Results
The project team worked with AFD to identify appropriate patients in real time for treatment and referral of OUD. The QRT made 348 visits during the six-month study period. Of these, QRT successfully contacted 83 individuals, and no individuals elected to be evaluated for MAT treatment or survey participation. Nine fatal opioid overdoses occurred during the study period.
The QRT visits successfully facilitated the delivery of life-saving naloxone kits in 55 (66%) patients and the dissemination of MOUD program education, resources, and Hope bags (a small bag with first aid supplies and a list of community resources) to all 83 patients.
Discussion
This study aimed to increase access and patient enrolment to MOUD in a prehospital setting through an interdisciplinary team. However, no individuals elected to participate in the program. Possible contributing factors may have included patient readiness and engagement, logistical and environmental barriers, concern about possible incarceration and lack of perceived benefit of treatment.
MOUD induction with buprenorphine has become the gold standard of treatment in OUD, secondary to its demonstrated abilities to reduce harm and save lives. Prehospital clinicians are the first contact health care professionals for many of these patients. In 2017, the United States Congress enacted the Protecting Patient Access to Emergency Medications Act (PPAEMA).
The PPAEMA permits EMS professionals to administer buprenorphine in the same manner it permits them to administer other controlled substances, such as fentanyl. Unlike most other controlled substances, however, EMS administration of buprenorphine for OUD requires that the authorizing medical director or other official have obtained an X-waiver because a standing order for buprenorphine technically qualifies as a prescription of the medication under federal law. Despite this law, buprenorphine use by EMS is relatively rare. The first case series published was out of Camden, New Jersey, where buprenorphine was given by EMS to three patients who had received Narcan for opioid overdose. Paramedics treated each patient with 16mg of buprenorphine to relieve and prevent withdrawal symptoms. Patients were provided with outpatient follow-up, irrespective of ED transport. There were no complications in giving prehospital buprenorphine. Reference Carroll, Wasserman and Shah6
A second prehospital buprenorphine program was initiated in Contra Costa County, California. The program, known as the EMS Buprenorphine Use Pilot (EMSBUP) program, Reference Hern, Lara and Goldstein7 allowed responding paramedics to initiate MOUD with buprenorphine in the field for patients experiencing withdrawal symptoms independently or following naloxone reversal. In the first year of the study, 36 patients enrolled received prehospital buprenorphine. Of those patients receiving buprenorphine, only one patient signed out against medical advice on scene. All other patients were transported to an ED, and their clinical outcomes and seven-day and 30-day follow-ups were determined by the substance use navigator (SUN). Thirty-six of 36 patients had follow-up data obtained in the short term, and none experienced any precipitated withdrawal or other adverse outcomes. Patients had a 50% (18/36) rate of treatment retention at seven days, and 36% (14/36) were in treatment at 30 days. Reference Hern, Lara and Goldstein7,Reference Ashburn, Ryder and Angi8
Another prehospital buprenorphine program was out of San Antonio, Texas. Over three years, a total of 263 patients were evaluated by EMS for MOUD induction, and 99 patients met the criteria and received at least one dose by EMS staff. There were no adverse events reported to either the EMS system or the receiving addiction treatment facility related to dosing by EMS clinicians in the prehospital environment. Specifically, no events of respiratory depression, subsequent overdose, or need for naloxone administration were observed. Reference Martin, Miramontes, Wampler and Churchwell9
As the opioid addiction crisis continues unabated, community needs will remain substantial for the foreseeable future, potentially necessitating more frequent QRT intervention with consequent increases in programmatic service delivery, including MOUD. Despite the absence of patients who participated in this MOUD program, several successes were identified. The protocol for community-based care, which can increase patient access to care through the prehospital MOUD program, was established. Collaboration with community partners increases the available resources for patients struggling with OUD. The hospital’s expansion to prehospital MAT treatment provides another level of substance use disorder (SUD)/OUD treatment for patients.
The AFD was receptive to developing the prehospital MAT program. They initiated the training programs for their QRT members and participated in the state grant team meetings. Even though they could not enroll patients in the prehospital MOUD program, continued discussions about expanding the program to specific medic units in real-time (not just through the QRT) are ongoing.
Future studies may investigate engagement approaches, including timing, such as follow-up care and post-hospital discharge, as well as enhancing patient education efforts to address stigma and convey the benefits of MOUD more effectively. Finding the reasons for care refusal will help us address this treatment gap.
Limitations
This study describes the process for instituting an EMS-based MAT program. The study’s major limitation was that it involved only one EMS system based in Akron, Ohio, and the program could not induct any prehospital patients with buprenorphine. A grant from the Ohio Department of Mental Health and Addiction Services supported the program. It required a collaborative approach with the city EMS and the two health systems that provided ED-based MAT. This may be difficult to implement in other systems, but the program has established a stepwise template for others.
Conclusion
This prehospital MOUD program expanded the treatment options and opportunities available to those who have experienced an opioid overdose using EMS providers. Challenges were encountered in the expansion of services through this pathway. However, the program has succeeded in establishing new relationships, developing treatment protocols, designing and implementing team training, and identifying a new approach to prehospital MOUD treatment initiation that did not exist.
Conflicts of interest/funding
Funding from Ohio Department of Health: Sustaining Emergency Department Comprehensive Care (ED21). The authors declare no conflicts of interest.




