Global evidence
There is a substantial body of literature exploring the relationship between severe mental illness (SMI; including non-organic psychotic disorders and bipolar affective disorder) and homelessness in high-income countries;Reference Fazel, Geddes and Kushel1–Reference Folsom, Hawthorne, Lindamer, Gilmer, Bailey and Golshan5 however, little is known about the situation in low- and middle-income countries (LMICs). In a systematic review and meta-regression of studies of homeless populations from high-income countries, the prevalence of psychotic disorders ranged from 3 to 42%, compared with approximately 1% in the general population.Reference Fazel, Khosla, Doll and Geddes2 Reviews from LMICs have thus far been limited to child/adolescent populations.Reference Woan, Lin and Auerswald6
People who are homeless are vulnerable to myriad health and social problems, which are exacerbated by the presence of mental illness,Reference Fazel, Geddes and Kushel1,Reference Geddes and Fazel7 and those with SMI who become homeless are at an elevated risk for long-term homelessness.Reference Fazel, Geddes and Kushel1 People with SMI may become homeless as a direct result of the symptoms of their illness, or as the consequence of eroded social and economic networks, or both.Reference Sullivan, Burnam and Koegel8,Reference Lovisi, Ferri, Amado and Prince9 In turn, the experience of homelessness can both precipitate and exacerbate symptoms of mental illness, whether alone or in the context of substance misuse.Reference Bresnahan, Collins and Susser10
Need for evidence from low- and middle-income countries
The prevalence of homelessness in high-income countries is affected by national-level differences in health and social care infrastructure as well as the availability of housing stock. These factors are likely to be reduced in low-income countries and this compounded by low treatment coverage for SMI may lead to a higher prevalence of SMI among the homeless population in comparison with high-income countries.Reference Lora, Kohn, Levav, McBain, Morris and Saxena11 On the other hand, differing family support systems, cultural responses to SMI and economic factors may influence the composition of the homeless population, and accordingly prevalence may be affected. The causes and consequences of homelessness in people with SMI in LMICs may thus differ from high-income country settings. Evidence from high-income countries supports the effectiveness of housing programmes for people with SMI who are homeless, where individuals are given accommodation and case management supportive services;Reference Pearson12 however, this type of intervention may not be feasible in lower-resourced settings.
A scoping review is appropriate for gathering information from a wide variety of sources, identifying gaps in the literature and informing future research, policy and interventions.Reference Peters, Godfrey, Khalil, McInerney, Parker and Soares13,Reference Arksey and O'Malley14 With these goals in mind, we set out to conduct a scoping review addressing the broad question: what is known about the causes, extent and impacts of co-occurring homelessness and SMI among adults living in LMICs and what responses are being implemented to address this issue? We focused on gaps in the evidence base and implications for future research and intervention development.
Method
Our scoping review was conducted according to the guidelines described in the Joanna Briggs Institute handbook on scoping reviews.Reference Peters, Godfrey, McInerney, Soares, Khalil and Parker15
Population
The target population for the review was adults with SMI who are homeless and living in LMICs. We operationalised homelessness as follows: (a) current (street) homelessness, (b) current residence in a homeless shelter/refuge, (c) current admission in psychiatric facilities or religious healing communities with immediately preceding homeless episode and/or no place of residence to go to post-discharge and (d) previous street homelessness.
This definition of homelessness excluded the following groups: (a) individuals described only as ‘unstably housed’, (b) ‘landless’ individuals or those living in accommodation with insecure tenancy, (c) individuals living in slums/shanty towns but in stable accommodation, (d) refugees or internally displaced people and (e) youth/child homeless populations <18 years of age.
SMI was operationalised broadly, as follows: any diagnosis of schizophrenia, schizoaffective disorder, bipolar affective disorder or major depression with psychotic features defined according to ICD-10 (1992)16 or DSM-5 (2013)17 guidelines or clinical assessment. The broader terms of SMI or psychosis were ascertained according to case notes or research assessment using the following methods: clinical assessment, brief interview and key informant report.
Studies were excluded if they investigated the following populations: (a) individuals who are homeless and diagnosed only with alcohol/substance use disorders, (b) individuals who are homeless and diagnosed with common mental disorders,Reference Goldberg and Huxley18 (c) populations affected by humanitarian crises and (d) migrant populations. When studies presented information about homeless populations with results stratified according to SMI versus these excluded conditions, they were retained in the review.
LMICs were defined using the World Bank classification of countries as low income, lower-middle income or upper-middle income at the time that the study was conducted. We excluded all Eastern European countries after the electronic search, regardless of country income bracket at the time of publication, as their health and social support systems differ from other LMICs. We had no restriction on the year of publication. The search was carried out between April and June 2018.
Search strategy
We conducted an electronic search of the literature and consulted with experts in the field. The electronic search for literature was conducted in three phases: (a) an initial limited search of the MEDLINE and Cochrane library databases to finalise search terms, (b) a second search using all identified keywords and index terms in the databases Embase, MEDLINE, PsychInfo, PsychArticles, Global Health and Ovid Journals (Journals@Ovid), and (c) a manual search of references in published full-text papers related to SMI and/or homelessness in LMICs.
The consultation phase of the review was conducted simultaneously and used a snowball-sampling method to identify and contact experts in the field. We also attempted to contact study authors for further information when data were incomplete or presented only as conference abstracts. Our search of the grey literature was limited to references identified in full-text papers and sources directed to us by expert consultation.
The detailed search strategy is presented in Supplementary File 1 available at https://doi.org/10.1192/bjo.2019.32.
Data extraction and quality assessment
Title and abstract screening
All citations from the searches were downloaded into EndNote and duplicates removed. Two reviewers (C.S. and S.F.) screened titles and abstracts of all citations based on the inclusion and exclusion criteria. Full-text articles for all potentially relevant citations were obtained.
Full-text screening
All full-text articles were assessed for eligibility according to the inclusion and exclusion criteria detailed above. The reason for exclusion of articles was documented. Where there were disagreements, a third reviewer (C.H.) was consulted and consensus reached.
Data extraction
Data charting forms included the following sections: (a) reference information, (b) study design, (c) study population, (d) study measures/variables, (e) study results, (f) quality appraisal and (g) references (relevant references and citations). See Supplementary File 2.
The two screeners (C.S. and S.F.) independently extracted data from two papers randomly selected in each category of study design (quantitative, qualitative and narrative studies) and compared their results. Because the extracted data were 100% consistent across both screeners, the lead author carried out the remaining data extraction thereafter and consulted the other reviewers if any uncertainty arose.
Quality appraisal
Quality appraisal was assessed and consensus reached for each publication according to the Mixed Methods Appraisal Tool (MMAT) version 2011Reference Pluye, Robert, Cargo, Bartlett, O'Cathain and Griffiths19 for Windows and Mac by both C.S. and S.F. Use of MMAT allowed for ratings across heterogeneous study designs including quantitative, qualitative and mixed-methods approaches.
Ethical appraisal
C.S. and S.F. evaluated each included publication presenting data collected from human research participants for the presence or absence of the following three ethical considerations: (a) whether ethical approval had been obtained before starting the research project, (b) whether informed consent of participants had been sought and documented, and (c) whether any additional measures had been taken to attend to the complexities of conducting research with such a vulnerable population (including but not limited to: appropriate assessment of capacity to consent to participate; respectful and consent-driven methods of study recruitment, including methods for in-patient commitment where relevant; and the provision of free medication or other medical treatment). The quality and ethical appraisals were used in the analysis; they were not used to exclude studies.
For the purposes of this review, the word ‘study’ refers to a discrete research project undertaken in a given setting and following a fixed methodology (including sample selection, etc.), whereas ‘publications’ refers to any written discussion of the study. We included only English-language publications.
Results
Eligible studies
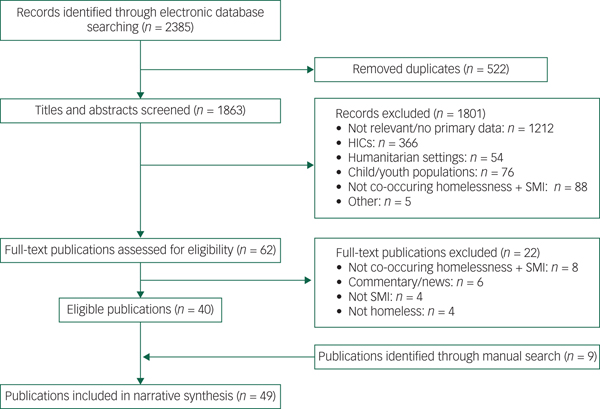
Figure 1 details the search. A total of 49 publications from 34 studies met inclusion criteria and were included in the review.
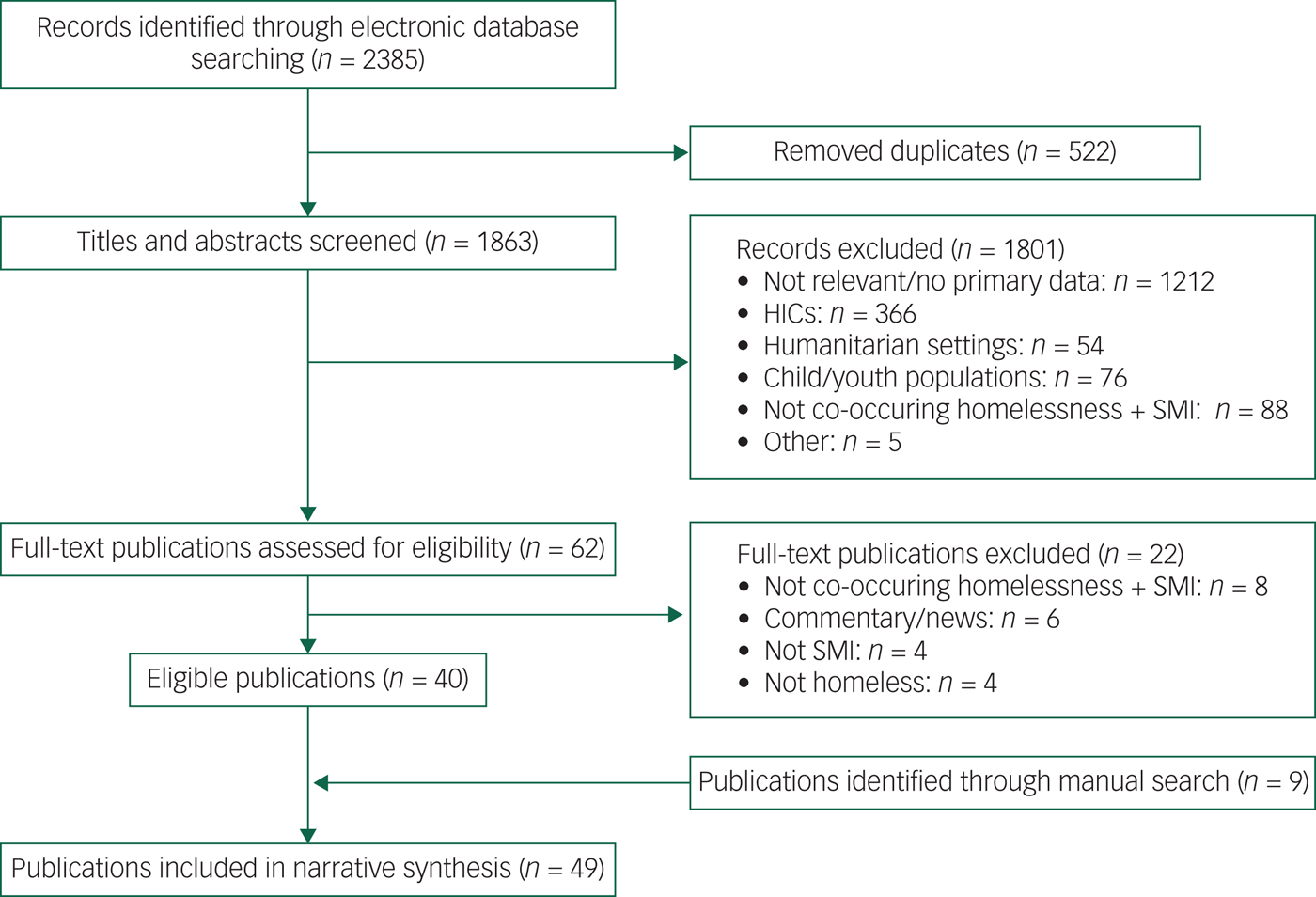
Fig. 1 PRISMA (Preferred Reporting for Systematic Reviews and Meta-Analysis) flow diagram. HICs, high-income countries; SMI, severe mental illness.
Reasons for exclusion at each stage of the of selection process were documented in a hierarchical manner as follows: not relevant/no primary data (n = 1212), high-income country settings (n = 366), populations affected by humanitarian crises/migrant populations (n = 54), child/youth homeless populations (n = 76), not including variables specific to co-occurring homelessness and SMI (n = 88) and other (n = 5: duplicates not identified electronically, n = 1; publications not in English, n = 4). The reasons for exclusion of full-text publications (n = 62) were: not including variables specific to co-occurring homelessness and SMI (n = 8), commentary/news articles (n = 6), not meeting operational criteria for SMI (n = 4) and not meeting operational criteria for homelessness (n = 4). The references of all full-text papers were searched for relevant citations, and all papers referring to either SMI or homelessness in LMICs were retrieved and read; through this process and from expert consultation we identified a further nine publications.
A total of 24 publications were from Asia (China, 15 publications from 5 studies;Reference Cao, Fu, Jia, Chiu, Ungvari and Ng20–Reference Wang, Zhang, Yan, Lu, Gao and Zhao34 India, 8 publications from 7 studies;Reference Chatterjee and Hashim35–Reference Chatterjee and Roy42 Turkey, 1 publication/studyReference Binbay, Halis, Hayriye and Alptekin43), 18 were from Africa (Nigeria, 7 publications from 7 studies;Reference Harding44–Reference Onofa, Fatiregun, Fawole and Adebowale50 Ethiopia, 7 publications from 4 studies;Reference Alem, Kebede, Fekadu, Shibre, Fekadu and Beyero51–Reference Teferra, Shibre, Fekadu, Medhin, Wakwoya and Alem57 Benin, Côte de Ivoire and Nigeria, 1 publication/study;Reference Eaton, Des Roches, Nwaubani and Winters58 Egypt and Lesotho, 1 publication/study;Reference Baasher, Elhakim, El Fawal, Giel, Harding and Wankiiri59 Ghana, 1 publication/study;Reference de-Graft Aikins60 Mozambique, 1 publication/studyReference Gouveia, Massanganhe, Mandlate, Mabunda, Fumo and Mocumbi61) and 7 were from South America (Brazil, 5 publications from 4 studies;Reference da Costa Borysow and Furtado62–Reference da Silva, Mason, Abelha, Lovisi and Cavalcanti66 Colombia, 1 publication/study;Reference Sarmiento, Correa, Correa, Franco, Alvarez and Ramírez67 Peru, 1 publication/studyReference Moquillaza-Risco, León, Dongo and Munayco68). At the time of publication, all of the South American and Asian study countries were middle income (lower or upper middle) and all of the African study countries were low income. In general, quality of the publications was low; they were characterised by poor or unclear methodology and reporting of results. Of the 38 publications assessed using MMAT, only nine were rated highly on all criteria.
The publications were classified according to base population under study (Table 1) and by the types of research questions guiding the studies (see Supplementary Table S1). A total of 15 publications from 3 studies were community-based cohorts of individuals with SMI; 16 publications from 15 studies drew samples from psychiatric facilities; 8 publications from 7 studies were from urban samples of individuals who were homeless at the time of assessment; and the remaining 10 publications from 10 studies were specific to populations with co-occurring homelessness and mental illness, and comprised interventions (intervention study n = 1), programmes (programme descriptions n = 4), qualitative appraisals of such services (n = 2) and descriptive analyses of co-occurring homelessness and mental illness in LMIC settings (n = 3). See Table 1 and Supplementary Table S1.
Table 1 Characteristics and quality appraisal of included studies
Studies marked as ‘n/a’ were unable to be assessed with the MMAT because their designs were incompatible with the tool. MMAT, Mixed Methods Appraisal Tool; SMI, severe mental illness; n/a, not applicable; n.d., not determined.
a. MMAT is rated out of a total of four possible criteria, with higher scores reflecting higher quality.
Epidemiology of homelessness in LMICs
See Supplementary Table S1. In eight publications from seven studies, the prevalence of SMI in street and shelter homeless populations was assessed using various diagnostic approaches, with the estimated prevalence of SMI varying from 8.0 to 47.4%. In 17 publications from 6 studies, the point prevalence of homelessness was reported in individuals with SMI: 2.3–8.2% were homeless at the point of assessment, however, several studies conflated homelessness with individuals lost to follow-up for unknown reasons and/or of unknown whereabouts. In 26 publications from 17 studies, cross-sectionally ascertained characteristics of individuals with co-occurring homelessness and mental illness were reported.
Incidence of homelessness in those with SMI was presented in only one publication (one study): after 10 years of follow-up, there was an incidence rate of 0.9/100 person-years of homelessness in the cohort from rural China. Seven publications (seven studies) examined the course and outcome of SMI in people who were homeless; these were all follow-up studies drawn from case records of psychiatric in-patients who were homeless.
A number of publications included analytic components: 15 publications (7 studies) identified factors associated with homelessness among SMI populations; 3 publications (2 studies) assessed factors associated with SMI among street and shelter homeless populations; 1 publication (1 study) studied predictors of homelessness among SMI cohorts; and 2 publications (2 studies) examined homelessness as a predictor of clinical outcomes in people with SMI. Detailed findings about physical health and disability, diagnostic profile, course of illness, treatment history and outcomes, social aspects of homelessness, family-related variables and sociodemographic characteristics are presented in Supplementary Files 3–11.
A total of 12 publications (12 studies) provided information about services, programmes, interventions and/or broader societal context surrounding the issue of co-occurring homelessness and mental illness in LMICs (these are described in Supplementary Table S1 as ‘descriptive analyses’).
Programmes and interventions for individuals with mental illness who are homeless in LMICs
Table 2 lists the main components of the identified programmes and interventions.
Table 2 Characteristics of programmes for adults with mental illness who are homeless in low- and middle-income countries
a. Only in cases that could not be managed in the community.
b. Including individual and group psychotherapy, psychoeducation and counselling.
We included studies of two religiously affiliated charities for homeless individuals with mental illness located in rural areas in three West African countries;Reference Colwill47,Reference Eaton, Des Roches, Nwaubani and Winters58 two non-governmental organisation for homeless individuals with mental illness in large cities in India;Reference Chatterjee and Hashim35,Reference Gopikumar, Easwaran, Ravi, Jude and Bunders36,Reference Rao39,Reference Chatterjee and Roy42 and an intervention study from Mozambique, based out of the country's primary psychiatric hospital.Reference Gouveia, Massanganhe, Mandlate, Mabunda, Fumo and Mocumbi61 Despite their different settings, all but one of these initiatives described delivery of centre-based care of unlimited duration for residents to recover from prolonged periods of SMI and street homelessness, with eventual family reintegration as the main treatment objective. Assessment and treatment by mental health specialists (including provision of medication), limited psychological therapies and vocational/occupational training were provided by all programmes. The only non-residential programme was a social work-based outreach service for people living on the streets in urban India.Reference Chatterjee and Roy42 In this case, the programme first tried to engage and treat individuals within the communities in which they were living and moved them to other locations only where this first strategy was considered unfeasible. The Mozambique study was the only formally evaluated intervention: 52.2% of study participants with schizophrenia were reintegrated with their families 3 months post-discharge. However, there was no control group and only individuals who were in regular contact with family members at baseline were eligible to participate, so this finding is limited by selection bias.
There were 46 publications (31 studies) that presented data collected from human research participants: of these, 27 publications (16 studies) reported having documented ethical approval for their research projects, 24 (14 studies) reported obtaining informed consent from participants and 10 (9 studies) reported taking additional ethical considerations or precautions when working with this population. The most common measure described was the provision of free medical and/or psychiatric treatment. Only three studies described precautions taken when approaching potential participants before engagement with research or treatment activities.Reference Chatterjee and Roy42,Reference Fekadu, Hanlon, Gebre-Eyesus, Agedew, Solomon and Teferra53,Reference Whiteford, Degenhardt, Rehm, Baxter, Ferrari and Erskine69 The results of the ethical appraisal are presented in Supplementary File 12.
Discussion
In this scoping review we identified studies that were diverse in terms of their focus, design and setting. The heterogeneity of sampled populations, quality concerns and methods used for the assessment and categorisation of both mental illness and homelessness make comparisons across studies problematic and limits the generalisability of our findings. However, the study findings converge to indicate that individuals in LMICs who have mental illness and are homeless have high burdens of both mental and physical ill health and live socially marginalised lives with extensive unmet needs for care.Reference Fekadu, Hanlon, Gebre-Eyesus, Agedew, Solomon and Teferra53 There is a lack of evidence about how best to meet these unmet needs and to guide the appropriate care of homeless people with SMI in LMICs.
Both the prevalence of SMI in homeless populations and the prevalence of homelessness in SMI cohorts are higher than would be expected by chance alone.Reference Whiteford, Degenhardt, Rehm, Baxter, Ferrari and Erskine69,Reference Tipple and Speak70 Moreover, the prevalence of homelessness among those with SMI was likely underestimated because samples were drawn from mainly clinical, help-seeking SMI sub-populations; selection bias is similarly likely to have affected studies of SMI in people who are homeless where samples were recruited from those engaged with services for the homeless. Despite the limitations common to the studies, there remains strong evidence for an association between homelessness and SMI.
Definitions of SMI varied from study to study. Many of the studies were limited to individuals diagnosed with schizophrenia while bipolar disorder and schizoaffective disorder were inconsistently considered. Another problematic point of divergence among the studies was their varying approaches to dual diagnosis: whereas some studies explicitly accounted for dually diagnosed individuals, others excluded those with alcohol or substance use disorders. Mislabelling individuals with dually diagnosed SMI and substance misuse may have introduced misclassification bias.
Gaps in the evidence base
The two most notable gaps in the evidence base we identified were the lack of information regarding the complex interrelationship and direction of causality between SMI and homelessness and the absence of rigorous evaluations of interventions for people with SMI who are homeless. None of the studies in the review addressed the issue of causality adequately: directionality between the two is very difficult to disentangle, and bi-directionality is probable. Rather than having a primary focus on populations with co-occurring homelessness and mental illness, the current literature overwhelmingly examines this problem from the lens of either clinical or homeless populations, which limits our ability to draw conclusions about pathways to and factors associated with homelessness. Better understanding of the underlying mechanisms might help in the design of preventive interventions and reduce the burden of co-occurrence.
There is a pressing need for rigorous evidence on how homelessness adversely affects access to mental healthcare in people with SMI; evidence is also needed on the quality, delivery and outcomes of such care. Similarly, better evidence on how the presence of SMI affects access to and the outcomes of optimal models of social care and rehabilitation for people who are homeless is crucial. There was also little information regarding how the specific needs of this population were being identified and met in LMIC settings; the few examples of programmes or interventions described in the included publications had weak evaluation, little evidence of a wider uptake and were overwhelmingly non-governmental.
Ethical considerations
Preservation of the right to autonomy with respect to participation in research activities was commonly overlooked in the identified studies. In many publications containing data from human participants, there was no documentation of ethical approval or any attempt to obtain informed consent. Individuals who are homeless and have SMI may present a unique challenge in this respect, with researchers struggling with the need to determine who can give consent in a community setting. Researchers must put safeguards in place to protect research participants from abuse.
There was also little evidence of consideration of the circumstances determining when it might be appropriate to facilitate hospital admission for a homeless individual with mental illness to access treatment and the procedures that should be followed in such cases. In many LMICs, mental health legislation does not exist or, if it does, it may not be implemented effectively or consistently.71 Where efforts are made to address street homelessness by governmental and non-governmental services, these initiatives may be politically motivated to ‘clean up the streets’ as much as to put people in a ‘safe place’, and often only serve to move people to other settings. Where they lead to hospital admission, legal justification may be inadequately considered and no rehabilitation services provided. Potential ethical concerns need to be addressed when researchers collaborate with such initiatives.
Models of good ethical practice were identified in this review, for example, where people who were homeless were befriended before entering rehabilitation services.Reference Chatterjee and Roy42,Reference Eaton, Des Roches, Nwaubani and Winters58 This type of outreach can help to ensure that the rights of these individuals are not ignored during efforts to deliver housing and/or medical care, however well intentioned. Greater transparency and understanding is needed to inform this process in LMICs to ensure that the rights of people with SMI are upheld before admission to hospital, during treatment and after they are discharged back into the community or to other settings.
However, awareness about these complex issues is increasing and therefore appropriate resources are being developed.72 When interpreting the Convention on the Rights of Persons with Disabilities, all of those responsible for decision-making need to balance the competing values of the right to personal autonomy versus the rights to housing and to health in the context of SMI.Reference Freeman, Kolappa, de Almeida, Kleinman, Makhashvili and Phakathi73
Limitations
Funding and time limitations meant that our review was restricted to English-language publications and our search of the grey literature was not systematic or complete. An informal internet search identified several non-governmental organisations that are apparently active in providing support and care to people with mental illness who are homeless in a few LMICs, but we found no formal descriptions or evaluations of these programmes online or in published form. We did not undertake a mapping process of the locally available interventions in practice which did not make it into the literature. We were therefore likely to have missed many community-level assets. Future reviews should extensively search grey literature sources to identify interventions operating in LMICs which are not currently engaged in research/dissemination activities. We were also limited in our ability to contact and consult with experts; several authors of positively screened abstracts were contacted for further information but did not respond.
Future directions
Programmes run by non-governmental organisations show that, even in low-resource settings, there is a commitment to support people with SMI who are homeless and that it is possible to establish comprehensive, integrated services that are driven by compassion. Rigorous evaluation of existing programmes, however, is sorely lacking. Evaluation of these programmes is needed to identify key aspects required for individuals to achieve social inclusion and sustainable recovery. There is also a need to evaluate potentially transferable models that have been found to be effective in high-income settings, such as those predominantly based around the provision of housing, welfare or livelihood activities. Programmes aimed at addressing extreme poverty or homelessness in LMICs could also be tailored to include this specific group. More information about operating costs and staffing structure of the existing models presented here would help to guide the development of feasible and acceptable responses to the unmet needs of people with SMI who are homeless in LMICs.
Promising initial results from the family reintegration study in Mozambique demonstrate that the psychiatric hospital setting is another potential site for intervention. It may require substantial political and institutional will to admit and treat individuals who are homeless in resource-constrained settings where psychiatric hospital beds are scarce; however, using pre-existing resources offered by such settings is likely to be cost effective. Reforms of healthcare services and systems currently underway in the field of global mental health should consider this population and include special provisions.
More prospective studies following individuals with SMI who are homeless in LMICs are urgently needed to assess the factors that influence return to stable housing, favourable treatment outcomes and recovery from mental illness. It is not easy to recruit and follow-up such populations, but such research must be undertaken if we are to truly understand the unique experiences of people who are homeless and have mental illness and identify appropriate and effective points of intervention. Respect for human rights – including the rights to housing, health and personal autonomy – should be paramount when conducting research with this population.
Supplementary material
Supplementary material is available online at https://doi.org/10.1192/bjo.2019.32.





eLetters
No eLetters have been published for this article.