CLINICIAN'S CAPSULE
What is known about the topic?
Patients with coronavirus disease 2019 (COVID-19) present with various influenza-like symptoms, making it difficult to distinguish from other viral infections for frontline physicians.
What did this study ask?
Do COVID-19 positive patients have higher prevalence of self-reported anosmia/hyposmia and dysgeusia/ageusia than COVID-19 negative patients?
What did this study find?
This study found that anosmia/hyposmia and dysgeusia/ageusia were respectively 14 and 11 times more likely to be associated with COVID-19 positivity.
Why does this study matter to clinicians?
Using anosmia/hyposmia and dysgeusia/ageusia as specific criteria may lead to improved clinical diagnosis of COVID-19 positive patients.
INTRODUCTION
Coronavirus disease 2019 (COVID-19) is an international outbreak of respiratory illness characterized by high transmission rate, particularly in individuals with no or mild symptoms.Reference Gandhi, Lynch and del Rio1,Reference Bai, Yao and Wei2 A key step in minimizing transmission is to screen and isolate those infected with COVID-19 using specific clinical criteria. While several symptoms are used to screen, there is lack of data to suggest specific symptoms of COVID-19. Anosmia/hyposmia and ageusia/dysgeusia have emerged as potential specific symptoms, as reported in recent studies from the United States and Europe.Reference Spinato, Fabbris and Polesel3–Reference Moein, Hashemian and Mansourafshar5 Spinato et al. described 64.4% of altered smell or taste among Italian adults with mild symptoms and Yan et al. described 68% and 71% of anosmia and dysgeusia, respectively, in COVID-19 positive individuals with an odds ratio (OR) of 10.Reference Spinato, Fabbris and Polesel3,Reference Yan, Faraji, Prajapati, Boone and DeConde4 A recently published study from Quebec reported 51.5% of anosmia.Reference Carignan, Valiquette and Grenier6 These reports suggest that anosmia/hyposmia and dysgeusia/anosmia have the potential to be used to specifically screen for individuals with mild symptoms. However, there are wide variations in the reported prevalence of anosmia/hyposmia and ageusia/dysgeusia across different regions, potentially suggesting variable geographic presentations of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).Reference Vroegop, Eeckles and Van Rompaey7 Therefore, it is imperative that we further examine this potential association between loss of smell and taste and COVID-19 diagnosis in the Canadian and Ontario context. The objective was to evaluate the prevalence and association of anosmia/hyposmia and dysgeusia/ageusia in patients who underwent COVID-19 testing using self-reported measures.
METHODS
Study design and patient population
The approval of this study was granted by the Research Ethics Board at Unity Health Toronto, Toronto, Ontario, through Clinical Trials Ontario (CTO ID: 2142). We designed a cross-sectional survey of adults (over 18 years of age) who had undergone polymerase chain reaction–confirmed COVID-19 testing via nasopharyngeal swab at the COVID-19 Assessment Centre at St. Michael's Hospital, Toronto, Ontario, between March 16 and April 15, 2020. Patients were contacted by phone for an invitation to a secure online survey, which was constructed using Snap Software, fully compliant with the Personal Health Information Protection Act, after being notified of the results of their swab. During this period, we identified 102 unique COVID-19 positive patients and 1,243 unique negative patients. Due to a large number of negative patients, we randomly sampled negative patients in a 1:3 ratio.
Outcome measures and data collection
Baseline characteristics were collected and included: age, gender, medical comorbidities, and smoking status. We listed chronic rhinosinusitis and history of recent severe upper respiratory tract infection (URTI) or flu as a separate comorbidity, as these may impact baseline sense of smell. COVID-19 diagnosis, symptoms, and hospitalizations were collected. Smell and taste-specific questions included the presence of smell or taste loss around the onset of COVID-19-like symptoms (5 days earlier or any time after), as well as the current ability to smell. The type of taste loss was collected (sweet, salty, sour, bitter, and savoury).
Statistical analysis
Demographic and clinical characteristics were summarized descriptively by reporting the median and interquartile (IQR) range for continuous variables and the frequency and proportion for categorical variables. Differences in characteristics between two comparison groups were compared using the Kruskal-Wallis test for continuous variables and Fisher's exact test for categorical variables. Unadjusted ORs were calculated with univariable logistic regression. Adjusted OR was calculated using multivariable logistic regression analysis with a priori criteria. To prevent over-fitting, we included the loss of smell or taste around the onset of COVID-19-like symptoms and four other covariates with a statistically significant magnitude of association of at least twofold (i.e., OR > 2.0 or OR < 0.5).
RESULTS
Of 102 positive patients and 306 negative patients who were contacted, 56 (50%) positive patients and 72 (23.5%) negative patients completed the survey between April 15 and May 1, 2020. Baseline information is summarized in Table 1. Positive patients were younger than negative patients (38.0 IQR 31.8–47.2 v. 43.0 IQR 33.5–55.0, p < 0.05). Gender, smoking status, and comorbidities relevant to smell function (head trauma, chronic rhinosinusitis, and recent URTI/flu) were well-balanced. There was a longer time lapse between the diagnosis and the survey among the negative patients compared with the positive patients (67.6% for negative v. 30.4% for positive for more than 4 weeks since the diagnosis).
Table 1. Comparisons of baseline characteristics of groups by COVID-19 diagnosis
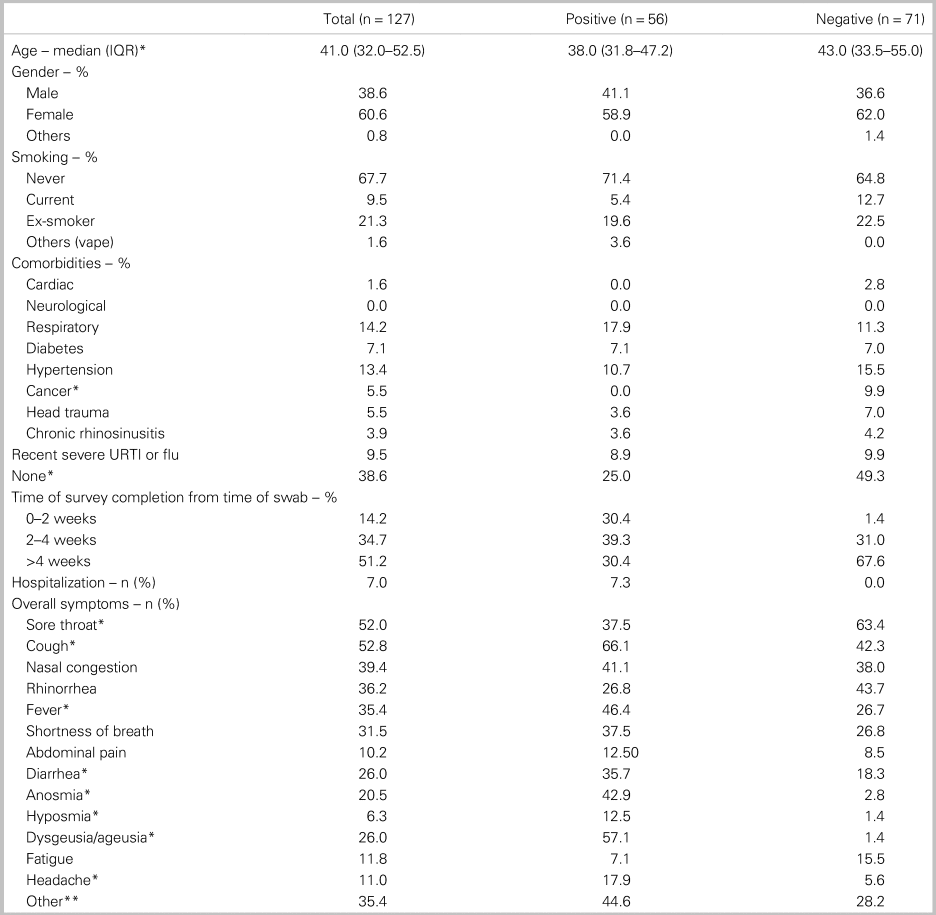
Notes:
*Statistically significant p-value (< 0.05). Kruskal-Wallis test for continuous variables and Fisher's exact test for categorical variables.
**Includes nonspecific symptoms, such as body aches, dizziness, ear pain, and myalgia with small prevalence.IQR = interquartile range; URTI = upper respiratory tract infection.
The overall symptoms are summarized in Table 1. A significantly higher proportion of positive patients reported anosmia (42.9% v. 2.8%, p < 0.001), hyposmia (12.5% v. 1.4%, p < 0.05) and dysgeusia/ageusia (57.1% v. 1.4%, p < 0.001) compared with negative patients. In addition, cough, fever, diarrhea, and headache were more common among positive patients. On the other hand, sore throat was more common among negative patients (63% v. 37%, p < 0.01).
Characterization of anosmia/hyposmia and dysgeusia/ageusia is summarized in Table 2. When patients were inquired about their smell loss around the time of COVID-19-like symptom onset (5 days before or any time after), there was a significantly higher proportion of COVID-19-positive patients compared with the negative patients (41.1% v. 4.2%, p < 0.001). Of 23 positive patients with anosmia/hyposmia, 12 (52.2%) patients reported that anosmia/hyposmia was one of the early symptoms. There was a significantly higher proportion of positive patients reporting dysgeusia/ageusia compared with negative patients (46.4% v. 5.6%, p < 0.001). Twenty (35.7%) positive patients reported concomitant smell and taste loss.
Table 2. Characterization of anosmia/hyposmia and ageusia/dysgeusia by COVID-19 diagnosis
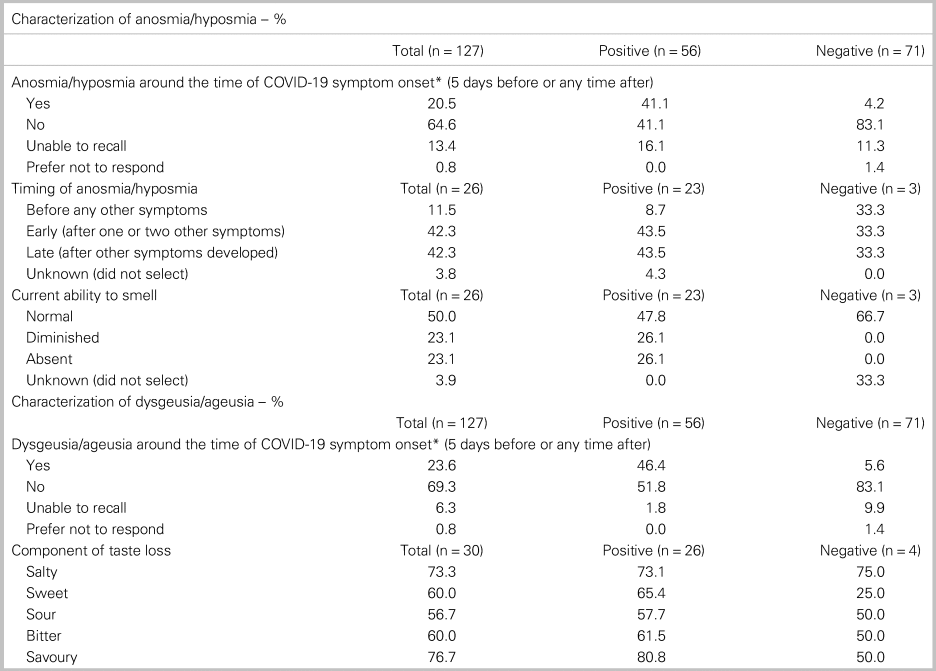
*Statistically significant p-value (< 0.05). Kruskal-Wallis test for continuous variables and Fisher's exact test for categorical variables.
On the univariable analysis, anosmia/hyposmia and dysgeusia/ageusia were highly associated with COVID-19 positivity OR 19.7 (95% confidence interval [CI] 6.1–88.7) and OR 13.2 (95% CI 4.6–48.0), respectively (Table 3). Fever, cough, sore throat, and headache were included in the multivariable analysis with either anosmia/hyposmia or dysgeusia/ageusia. In the multivariable models, smell loss and taste loss demonstrated high adjusted ORs with COVID-19 positivity (OR 14.4 [95% CI 4.0–70.5] and OR 11.4 [95% CI 3.6–45.3], respectively). Sore throat was negatively associated with COVID-19 positivity. Other symptoms were statistically not significant.
Table 3. Univariable and multivariable analysis for the association between influenza-like symptoms and COVID-19 diagnosis
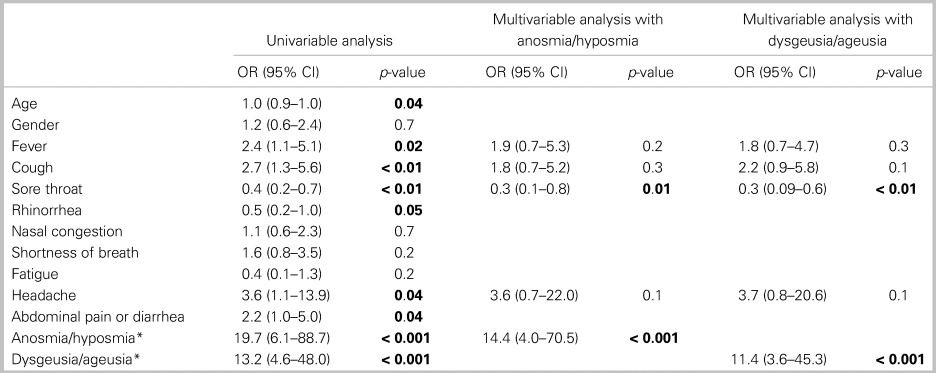
Notes: Boldface text indicates statistically significant p-value (< 0.05).
*Smell and taste loss based on reported data around the time of self-reported COVID-19 symptom onset (5 days before or any time after); OR = odds ratio; CI = confidence interval.
There were no differences between patients with and without anosmia/hyposmia in terms of age, smoking, relevant comorbidities (chronic rhinosinusitis, recent URTI/flu, head trauma), and symptoms (rhinorrhea and nasal congestion) (Table 4). There were significantly more COVID-19-positive patients in the group with smell loss than the one without (88.5% v. 28.1%, p < 0.001).
Table 4. Comparison of clinically relevant variables between the group with and without anosmia/hyposmia
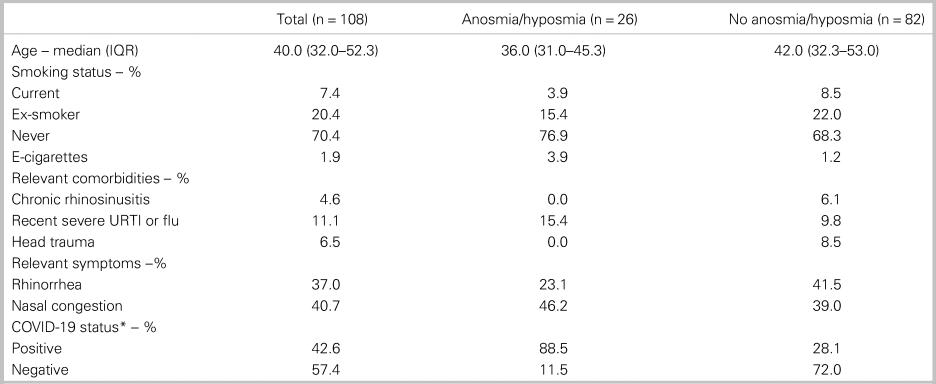
Notes:
*Statistically significant p-value (< 0.05). Kruskal-Wallis test for continuous variables and Fisher's exact test for categorical variables.
IQR = interquartile range; URTI = upper respiratory tract infection.
Among those with anosmia/hyposmia (n = 25, 1 did not answer), 13 (52%) patients reported their sense of smell at the time of survey to be normal. Twelve (48%) patients who had persistent smell loss were within less than 4 weeks from the diagnosis. All eight patients who completed the survey more than 4 weeks after the diagnosis reported a normal sense of smell.
DISCUSSION
Interpretation of findings
This study suggests that there is a higher prevalence of self-reported chemosensory impairment in COVID-19-positive patients compared with negative patients with early recovery of smell function in a large proportion of patients. In our series, olfactory and gustatory impairments were respectively 14 times and 11 times more likely to be associated with COVID-19 positivity. Overall, our findings suggest that loss of smell and loss of taste have a higher chance of identifying COVID-19-positive patients among those with influenza-like symptoms seen on an ambulatory basis.
The reported prevalence of olfactory dysfunction varies significantly from 5.1% in a Chinese study to 85.6% in a European study.Reference Spinato, Fabbris and Polesel3–Reference Moein, Hashemian and Mansourafshar5,Reference Vroegop, Eeckles and Van Rompaey7–Reference Vaira, Salzano, Deiana and De Riu9 Our results are consistent with previous reports that showed a higher prevalence of self-reported smell or taste loss among COVID-19-positive patients. Interestingly, in our study, although 31 out of 56 (55.4%) of COVID-19-positive survey participants included anosmia or hyposmia as one of their overall symptoms, only 23 (41.1%) patients maintained that they lost their sense of smell around the time of COVID-19 symptom onset (5 days prior or thereafter) with a 16% rate of “unable to recall.” This discrepancy likely represents recall bias, which is common in cross-sectional studies. Therefore, we believe that the 40% rate of smell loss around the time of COVID-19 symptom onset is a more accurate representation than the 55% overall rate.
Comparison with previous studies
Our rate of anosmia/hyposmia of 41.1% is lower than the rate of 60%–85% in recently published studies with comparable study designs or 51.5% found in another Canadian study.Reference Spinato, Fabbris and Polesel3,Reference Yan, Faraji, Prajapati, Boone and DeConde4,Reference Carignan, Valiquette and Grenier6,Reference Lechien, Chiesa-Estomba and De Siati8 There may be several explanations for this difference. One consideration is the cultural difference in olfactory perception.Reference Candau10–Reference Ferdenzi, Roberts and Schirmer12 In fact, participants in other cultures may have different thresholds for their smell loss. Another possible explanation is the presence of mutant strains with varying pathogenicity, as evidenced from genomic studies in multiple nations.Reference Gudbjartsson, Helgason and Jonsson13–Reference Yao, Lu and Chen16 These different strains may cause varying degrees of chemosensory impairment with regional discrepancy, although this has not been scientifically proven. Therefore, it is important to collect and examine regional data to depict a representative landscape for our population. Lastly, we do note that this difference could be a simple function of recall bias from cross-sectional surveys, as other studies do not report an “unable to recall” option, thus forcing patients to choose with an altered response rate of self-reported smell loss. Regardless, all published studies unanimously support the inclusion of smell and taste loss as important markers of COVID-19.
Clinical and research implications
A possible mechanism of olfactory dysfunction caused by SARS-CoV-2 has been demonstrated in experimental models with inoculation of coronaviruses. Coronaviruses can damage the olfactory neuroepithelium via apoptosis with a subsequent reduction of mature sensory neurons and disordering of olfactory epithelium.Reference Mori, Goshima and Imai17–Reference Schwob, Saha, Youngentob and Jubelt19 Another line of research suggests that the anosmia/hyposmia may result from infection of the support and perivascular cells in olfactory epithelium, via angiotensin-converting enzyme 2 receptors, which are identified as the receptors of SARS-CoV-2.Reference Brann, Tsukahara, Weinreb, Logan and Datta20,Reference Zhou, Yang and Wang21 Clinically, nasal inoculation of coronavirus resulted in olfactory impairment in healthy volunteers.Reference Åkerlund, Bende and Murphy22 Dysgeusia/ageusia is generally regarded to be secondary to loss of smell, as it may be difficult to distinguish between flavor and taste. In a large study investigating taste disorders unrelated to COVID-19, many reported loss of taste without any objective gustatory loss but found to have olfactory deficits alone.Reference Deems, Doty and Settle23 While it is possible that loss of taste in COVID-19 may be a distinct mechanism,Reference Vaira, Salzano, Fois, Piombino and De Riu24 the rate of taste loss in our patients likely represents subtle olfactory deficits. In our series, 52% of the affected individuals reported a normal sense of smell at the time of survey with many recovering within 4 weeks. This finding is consistent with previous reports and suggests that the damage to the olfactory function by COVID-19 may not be permanent.Reference Yan, Faraji, Prajapati, Boone and DeConde4 However, this warrants further investigation with follow-up assessments of smell function. All in all, the presence of loss of smell and taste may be a distinguishable feature of COVID-19 from other viral URTIs.
Our results have strong implications in public health measures. A recent study demonstrated 56% of residents to be COVID-19 positive but “asymptomatic” in a skilled nursing facility.Reference Arons, Hatfield and Reddy25 However, this study did not include the loss of smell or taste in the symptom assessment. In a previous study from Italy and our study, both demonstrate that a significant portion of the patients complained of decreased sense of smell or taste during the early phase of their disease.Reference Spinato, Fabbris and Polesel3 Hence, it would be essential to incorporate anosmia/hyposmia and dysgeusia/ageusia as part of future epidemiologic COVID-19 surveillance studies and tailor the screening criteria for COVID-19 accordingly. Furthermore, these symptoms can be easily assessed in the context of telemedicine and virtual care. This can, in turn, facilitate improved patient counselling for the screening of COVID-19 and help curb the spread of COVID-19 in the vulnerable population, including those in long-term care facilities and remote communities where testing may be limited. Currently, while several provincial bodies have implemented loss of smell/taste as screening symptoms, the self-assessment tool from the Canadian Federal Government still does not incorporate these symptoms. With our Ontario regional data demonstrating a high probability of COVID-19 positivity with loss of smell/taste, there is now evidence to expand public awareness of this association and ultimately improve our public health response to this pandemic.
Limitations
Interpretation of our study results is limited by recall bias, as there is a significant time lapse between diagnosis and survey administration. The recent media spotlight of COVID-19 and anosmia might have resulted in elevated rates of self-reported anosmia. We tried to mitigate this issue by asking similar, but differently worded, questions for internal validity. Future studies could be administered at the time of swab to avoid this bias. We also acknowledge non-response bias. While the study results are limited by the nature of a single-institutional-based study, we collected data over a longer period of time than previous reports to improve our sampling.Reference Spinato, Fabbris and Polesel3,Reference Yan, Faraji, Prajapati, Boone and DeConde4 Furthermore, the testing criteria focused on frontline workers from at-risk settings, such as healthcare or long-term care, residents in group homes, and returning travelers. This may reduce external validity. Lastly, with ethical concerns of transmission to our research team and preservation of personal protective equipment, we are presently unable to objectively measure smell in symptomatic patients during the point of assessment.
We acknowledge the need for large-scale epidemiologic studies to further investigate this association between smell and taste loss and COVID-19 positivity. Our research group currently has ongoing projects to investigate a larger regional population and to incorporate self-reported objective measures of smell using common household items. Despite the limitations, the baseline characteristics between positive and negative groups were comparable, and our data emphasize the importance of considering smell and taste as screening symptoms.
CONCLUSION
Our results demonstrate that there is a higher rate of self-reported anosmia/hyposmia and concurrent dysgeusia/ageusia among COVID-19 patients in a regional sample of Canadians in Toronto, Ontario. Our study offers strong support for clinicians to use loss of smell and loss of taste as key symptoms for the clinical diagnosis of COVID-19, especially in settings with limited testing. Future population-based studies are needed to further investigate this association.
Acknowledgements
The authors sincerely thank Cheryl Pedersen and the Survey Research Unit at St. Michael's Hospital for survey administration and study support and The Dunin Foundation for research support. We would like to acknowledge Drs. Jonathan Overdevest and Stuart Firestein for the initial survey design. We would like to thank Dr. Jennifer Anderson for her support of this study.
Author contributions
Study concept and design: D. Lee, J. Lockwood, P. Das, R. Wang, E. Grinspun, J. Lee
Acquisition of data: D. Lee, J. Lockwood, P. Das, J. Lee
Analysis and interpretation of data: D. Lee, R. Wang, J. Lee
Initial draft of the manuscript: D. Lee
Critical revision of the manuscript for important intellectual content: D. Lee, J. Lockwood, P. Das, E. Grinspun, R. Wang, J. Lee
Administrative, technical or material support: D. Lee, J. Lee
Study supervision: J. Lee
All authors have given their agreement for this study.
Financial support
This study was funded by The Dunin Foundation.
Competing interests
JML has received honoraria from Baxter Corporation. All other authors have declared no potential conflicts of interest.






