Adolescents are estimated to make up 16 % of the global population, with approximately 1⋅3 billion adolescents in the world today(1). The classification of the adolescent period can vary, with the UN defining it as the period of life between 10 and 19 years of age, and the WHO expanding the age of adolescence to encompass those from 10 to 24 years(Reference Sawyer, Azzopardi and Wickremarathne2). Ultimately, adolescence is the period of transition from childhood to adulthood, generally co-occurring with the onset of puberty and culminating with the achievement of legal independence from parents/guardians i.e. ‘adulthood’(Reference Jaworska and MacQueen3). Adolescence is a critical life stage characterised by major biological, psychological, emotional, and social growth and development. The rapid pace of physical and cognitive growth in adolescence is second only to the growth of infancy, with this time classed as the second ‘developmental period’(Reference Larsen and Luna4,Reference Best and Ban5) .
Consequentially, nutritional needs increase during adolescence, with requirements for most nutrients higher than those of adults relative to body weight and energy requirements(6,7) . Despite the importance of this life stage, the health priorities of adolescents remain somewhat neglected, with their needs widely overlooked in global health and nutrition policies(Reference Patton, Sawyer and Santelli8). The Lancet Commission on Adolescent Health and Wellbeing brought this issue to the fore and has labelled adolescent nutrition as a ‘hidden crisis’(9). The commission criticised the general omission of adolescents from global policies and emphasised the need for investment to protect the health of youth and future adult populations(Reference Patton, Sawyer and Santelli8). As a transitional life stage and period of increased autonomy, this age group often no longer receive the benefits and protection of the care devoted to childhood(10). Additionally, adolescence is largely considered a period of good health and decreased susceptibility to disease, leading to this age group generally being overlooked in public health discourse(9). However, as a pivotal life stage in which the foundations of health are laid(Reference Norris, Frongillo and Black11) and exposure to health risks increases(Reference Sawyer, Reavley, Bonell, Bundy, Silva, Horton, Jamison and Patton12), the exclusion of adolescents from global nutrition efforts is an oversight that could undermine the progress that has been made in childhood health(Reference Bhutta, Lassi and Bergeron13). Consideration of this age group's nutrition and health needs, and action to ensure these needs are fulfilled and protected, is critical in ensuring a healthy population, both now and in the future.
This review aims to present key considerations and characteristics of adolescent nutrition and health, identify a selection of the causes and consequences of poor nutrition in adolescence, and highlight potential opportunities to improve nutrition and health within this age group, with a focus on evidence and opportunities within an Irish context.
Nutritional and dietary characteristics of adolescents
Nutritional vulnerability in adolescence
Adequate nutrient intake is critical in all stages of life but particularly during the adolescent years, not only to facilitate rapid physiological growth and development but also to lay the foundations of good health for later life(Reference Koletzko, de la Guéronnière and Toschke14). Consistent increases in life expectancy mean that the youth of today are projected to live long and productive lives(Reference Kontis, Bennett and Mathers15). The quality and quantity of nutrition consumed during the formative years of adolescence has long-term effects on health and well-being throughout life(Reference Koletzko, de la Guéronnière and Toschke14). Leading nutrition experts have emphasised the need for societies to prioritise the nutritional needs of youth and provide clear dietary guidance and action on nutrition for adolescents(Reference Koletzko, de la Guéronnière and Toschke14).
Adolescents are vulnerable to the ‘triple burden’ of malnutrition, encompassing undernutrition, micronutrient deficiencies and overnutrition(Reference Rah, Melse-Boonstra and Agustina16). This age group is consistently identified as failing to meet recommendations for a variety of nutrients(Reference Christian and Smith17) while also displaying a rising incidence of energy overnutrition and overweight/obesity(18). Both adolescent undernutrition and obesity coexist across low- and middle-income countries(18,Reference Caleyachetty, Thomas and Kengne19) , with the issue of obesity tending to be the most pervasive dietary challenge amongst youth in high-income countries(Reference Mahumud, Sahle and Owusu-Addo20). The increased nutrient requirements of adolescence, coupled with changes in dietary habits, behaviours, and environmental exposures mean that this age group generally have a high risk of dietary inadequacy(Reference Norris, Frongillo and Black11,21) . Adolescents, along with women and children, have been identified as bearing much of the global burden of micronutrient deficiency(Reference Bailey, West and Black22), with vitamins A, B6, B2, D, E, folate, calcium, iron, iodine, zinc and selenium reported as micronutrients of particular concern for this age group(10,Reference Miller, Spiro and Stanner23,Reference Rippin, Hutchinson and Jewell24) , both in Ireland(25) and internationally(Reference Jun, Cowan and Dodd26–Reference Estecha Querol, Al-Khudairy and Iqbal30).
Iron inadequacy is a common dietary deficiency in this age group, with a particularly high burden in lower-affluence countries(Reference Zimmermann and Hurrell31). Iron requirements increase substantially in adolescence to facilitate intensive muscular and cognitive growth and development, increased blood volume and the onset of menstruation in females(Reference Bresson, Burlingame and Dean32). Inadequate iron intake is a prevalent issue for female adolescents across Europe, with policy-based interventions proposed as a potential avenue to reduce the scale of iron deficiency(Reference Rippin, Hutchinson and Jewell24). Albeit, Irish adolescents in general display sufficient intakes of dietary iron(25,Reference Mesías, Seiquer and Navarro33) , largely attributed to the widespread consumption of fortified ready-to-eat breakfast cereals and meat(Reference Lyons, Walton and Flynn34). However, female adolescents in Ireland do tend to consume lower amounts of dietary iron(35) and 9 % display intakes below recommendations(25), indicating that attention is still required to ensure adequate consumption of this essential mineral amongst this population group.
Adolescence is a pivotal stage of bone mineralisation, with approximately 40–60 % of adult bone mass accrued during adolescence(Reference Golden36). Hence, requirements for calcium(Reference European Food Safety Authority37) and phosphorus(Reference European Food Safety Authority38) are higher in adolescence than in all other stages of life, with an increased intake of Vitamin D also advised for this age group(39). With that being said, there is a high prevalence of inadequate intakes of calcium and vitamin D amongst adolescents, with evidence from Europe(Reference Rippin, Hutchinson and Jewell24), the UK(40,Reference See, Edwards and Farrar41) , the USA(Reference Bailey, Dodd and Goldman42) and Brazil(Reference de Assumpção, Dias and de Azevedo Barros43) indicating that the majority of adolescents fail to meet recommendations for these nutrients. Within an Irish context, 94 % of adolescents have been identified as having inadequate intakes of vitamin D, and 67 % consume below the recommendations for calcium(Reference Cashman, Kehoe and Kearney44). Evidence of declining consumption of dairy foods(Reference Hohoff, Perrar and Jancovic45) and low intake of supplements(25) amongst Irish adolescents raises significant concerns regarding future consequences on bone health for this age group.
The adolescent years have been suggested to pose the potential for catch-up nutrition and growth, providing a possible opportunity for childhood nutritional deficiencies and insufficient growth to be somewhat ameliorated(Reference Campisi, Carducci and Söder46). The brain undergoes intense growth and remodelling during adolescence, with this life stage considered a time of heightened cognitive malleability(Reference Steinberg47,Reference Fuhrmann, Knoll and Blakemore48) . This heightened neuroplasticity increases the vulnerability of the brain to nutritional and environmental risks such as dietary deficiencies(Reference Norris, Frongillo and Black11). Nutritional intake can have profound effects on the construction and strengthening of neurocircuitry, with energy and protein undernutrition, consumption of high fat and high sugar diets and inadequate intake of essential nutrients including B vitamins, iron, iodine zinc, and PUFA all considered risks to neurodevelopment(Reference Norris, Frongillo and Black11,Reference O'Connor and Cryan49–Reference Lowe, Morton and Reichelt51) . Therefore, ensuring adequate nutrient intake, particularly essential micronutrients, is imperative in establishing good health in youth and equipping them to lead long, healthy and productive lives.
Optimisation of nutritional intake during adolescence is essential in ensuring the health of adolescents themselves and protecting the health of future offspring. Globally, nearly one-third of women become pregnant during their adolescent years, highlighting the critical need to ensure nutritional adequacy for the health of vulnerable young women and infants(Reference Patton and Sawyer52). Suboptimal micronutrient status is a key nutritional challenge amongst adolescent mothers, with iron, iodine and folic acid emphasised as nutrients of particular concern(Reference Patton and Sawyer52). Iodine is a vital mineral in the production of thyroid hormones and normal neurodevelopment, with iodine deficiency in youth associated with impairments in mental and physical functioning(Reference Zimmermann53). Adequate iodine intakes become particularly essential as women enter childbearing age, with iodine deficiency leading to intellectual impairments and cognitive and behavioural problems in offspring(Reference Bath54). European adolescents, particularly females, have been identified as consistently displaying lower iodine intakes than other age groups(Reference Bath, Verkaik-Kloosterman and Sabatier55). National dietary surveys of Irish adolescents have indicated a decline in milk consumption(25) and consistently low intakes of fish and seafood(35), raising concerns about iodine intakes amongst this age group.
The commencement of supplementation with folic acid is recommended for all women upon reaching childbearing age to prevent the occurrence of neural tube defects in pregnancy(Reference Viswanathan, Treiman and Kish-Doto56). However, awareness of the need for folic acid is poor amongst adolescent females, with low consumption of folic acid supplements across this age group globally(Reference Matsuo, Kagohashi and Senga57). Indeed, in Ireland, overall supplement use is low amongst all adolescents, with only 14 % reporting consuming a supplement(25). While voluntary fortification of food products with folic acid has resulted in the improvement of folate status at a population level(Reference Pfeiffer, Sternberg and Zhang58), there is a clear need for increased folic acid fortification and the use of education and outreach to promote folic acid intake amongst young women. The overall risk of complications in maternal and neonatal health outcomes is substantially greater for adolescent mothers compared to those of adult women(Reference Gurung, Målqvist and Hong59), meaning that ensuing nutritional adequacy in adolescent females is one of the several essential efforts that should be made to improve the lives and safety of these young women.
While undernutrition remains a prevalent dietary challenge for adolescents in lower affluence countries, the issue of overnutrition and its resultant effects on excessive weight gain is fast becoming the forerunning issue for adolescent health globally(18). While energy requirements increase substantially in adolescence, modern lifestyle behaviours such as decreased energy expenditure, increased sedentary activity and high consumption of energy-dense foods mean that adolescents can easily tend towards a daily energy surplus(Reference Sonneville and Gortmaker60). This energy imbalance is the main driver of excessive weight gain and can be particularly heightened during adolescence, with analyses of adolescent cohorts across several countries showing clustering of unhealthy energy-balance-related behaviours during this life stage(Reference Collese, De Moraes and Fernández-Alvira61).
Dietary intakes: deterioration of diet quality during adolescence
Consumption of a poor-quality diet is one of the largest contributors to the global burden of non-communicable diseases and is considered a key modifiable risk factor for chronic diseases(Reference Green, Sutherland and Dangour62). Adolescents have been consistently identified as displaying the poorest quality diets of all population groups(Reference Winpenny, Greenslade and Corder63), with the Dietary Guidelines for Americans highlighting that the difference between recommended food group intakes and actual consumption is greatest for adolescents aged 14–18 years compared to other age groups(21). Diet quality tends to decrease in the transition from childhood to adolescence, with those aged 14–18 years ranking approximately ten points lower in Healthy Eating Index scores than younger children(Reference Banfield, Liu and Davis64). Poor-quality diets have been consistently identified amongst adolescents across a range of countries and regions, including Brazil(Reference Ronca, Blume and Cureau65), Turkey(Reference Çağiran Yilmaz, Çağiran and Özçelik66), Canada(Reference Storey, Forbes and Fraser67), the USA(Reference Liu, Rehm and Onopa68), the UK(Reference Roberts, Steer and Maplethorpe69) and Europe(Reference Moreno, Gottrand and Huybrechts70), with poor diet quality generally characterised by low consumption of fruit, vegetables, wholegrains, lean meat and low-fat dairy, and high intake of confectionery, high-sugar beverages, fats, processed meats, refined grains, and ready meals(Reference Liu, Rehm and Onopa68–Reference Moreno, Gottrand and Huybrechts70). ‘Unhealthy’ and ‘sandwich’ dietary patterns have been previously identified as the most predominant amongst Irish adolescents, with these patterns associated with a higher intake of fat, saturated fat, and total sugars, and lower intakes of fibre and vitamins(Reference Hearty and Gibney71). Additionally, poor dietary habits such as meal skipping and replacement of meals with snacks are frequently reported amongst adolescents globally(Reference Monzani, Ricotti and Caputo72,Reference Moreno, Rodriguez and Fleta73) and contribute to significant deteriorations in diet quality amongst this age group(Reference Murakami and Livingstone74–Reference Spruance, Clason and Burton76).
The quality of the diet consumed by adolescents has shown slight improvements in recent years, with US youth showing a modest improvement in diet quality scores from 1999 to 2016, characterised by decreased consumption of sugar-sweetened beverages and added sugar, and increased intake of wholegrains, fruit and vegetables, poultry and eggs(Reference Liu, Rehm and Onopa68). However, poor diet quality remains a persistent issue amongst adolescents, with those aged 12–19 years displaying the highest prevalence of a poor-quality diet in the USA(Reference Liu, Rehm and Onopa68). Gradual improvements in dietary intake have been observed in regions of Europe and North America, with evidence of increased fruit and vegetable consumption by adolescents across most countries, including Ireland, from 2002 to 2010(Reference Vereecken, Pedersen and Ojala77). However, infrequent consumption of fruit and vegetables remains a characteristic of adolescents globally(Reference Beal, Morris and Tumilowicz78,Reference Diethelm, Jankovic and Moreno79) . Some improvements have been observed in the current diets of Irish adolescents, with modest increases in the consumption of fruit, vegetables and high-fibre cereals and slight reductions in the intake of free sugars and salt(25). However, Irish adolescents still display poor adherence to food and nutrient recommendations, with an average daily intake of fewer than three portions of fruit and vegetable, poor intake of fibre, and excessive intake of salt, saturated fat, and ‘top-shelf’ foods(25). Poor compliance with dietary guidelines is characteristic of adolescents globally, with this age group consistently displaying low intakes of recommended foods and excessive intakes of more unfavourable foods(Reference Banfield, Liu and Davis64,Reference Brettschneider, Lage Barbosa and Haftenberger80,Reference Handeland, Kjellevold and Wik Markhus81) .
Analysis of trends in the dietary intakes of US adolescents has identified an increased consumption of ultra-processed foods in recent years, with 68 % of adolescent energy intake derived from ultra-processed foods in 2018(Reference Wang, Martínez Steele and Du82). While the level of processing is not a marker of the healthfulness of food, nutrient profiling of the consumed foods did also suggest a higher proportion of carbohydrates, added sugars, sodium, and lower level of protein and fibre in foods classed as ultra-processed v. unprocessed foods(Reference Wang, Martínez Steele and Du82). Intake of highly processed foods is similarly pervasive amongst Irish adolescents, with high intakes of white bread, pizza, savoury snacks, chips, processed meats, and confectionery noted in 2020(35). Diets with a high proportion of highly processed, energy-dense, nutrient-poor foods, encompassing fast foods, confectionery, snacks, cakes, refined grains, and sugar-sweetened beverages, are increasingly prevalent amongst this age group(Reference Dunford and Popkin83,Reference Kerr, Rennie and McCaffrey84) and have been associated with an increased risk of overweight/obesity(Reference Liberali, Kupek and Assis85). The widespread consumption of industrially produced convenience foods poses these foods as potential targets for reformulation and dietary intervention to improve the diets of adolescents and indeed the general population.
Adolescence is a pivotal time of personal development, in which lifelong traits and habits can be discovered and established. This life stage has been highlighted as an important but overlooked time for the establishment of lasting health behaviours, with adolescence posed as a ‘window of opportunity’ for the establishment of dietary patterns(Reference Chong86). Childhood dietary behaviours have been shown to track relatively strongly into adulthood, with behaviours from late adolescence displaying the strongest continuation into adulthood(Reference Craigie, Lake and Kelly87). An energy-dense, high-fat, low-fibre dietary pattern has been shown to track from early-to-late adolescence(Reference Appannah, Pot and Oddy88), with overall diet quality generally tending to decrease with age(Reference Banfield, Liu and Davis64,Reference Thomson, Tussing-Humphreys and Goodman89) . Certain longitudinal cohort studies have indicated that adolescents with the closest adherence to dietary patterns, including ‘traditional’, ‘health-conscious’, ‘high-protein, high-fat’ and ‘vegetarian-style’, display significant tracking of similar dietary patterns 20 years later(Reference Mikkilä, Räsänen and Raitakari90,Reference Movassagh, Baxter-Jones and Kontulainen91) . However, the longevity of adolescent dietary patterns in later life has been questioned, with other longitudinal evidence showing poor tracking of energy and macronutrient intakes from early-to-mid-adolescence(Reference Robson, Gallagher and Livingstone92) and from adolescence into young adulthood(Reference Boreham, Robson and Gallagher93). Nevertheless, the establishment of healthful dietary patterns is imperative in meeting the nutritional requirements of adolescence and could potentially aid in the creation of lifelong healthy behaviours.
Risk factors related to adolescent nutrition and health: causes and consequences
Causes of poor nutrition and diet in adolescence
Adolescents' dietary behaviours and nutrient intake are influenced by a plethora of different factors, from individual-level decisions to broader social and structural determinants. A summary of the complex interplay of factors that influence this age group's food-related behaviours is presented in Fig. 1.
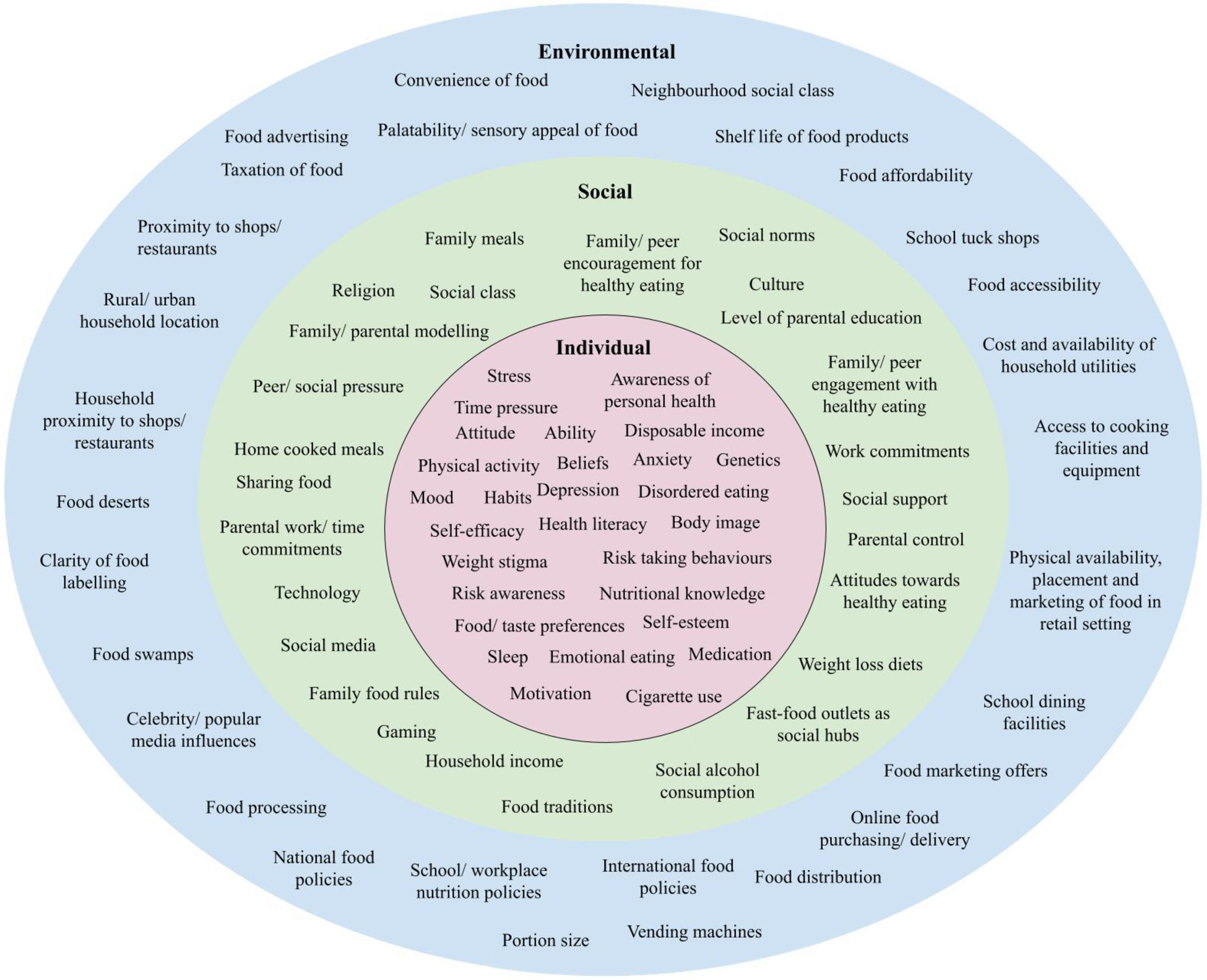
Fig. 1. Individual, social, and environmental factors influencing adolescent nutrition and diet.
Individual factors influencing adolescent nutrition and health
Adolescence has long been considered a period of ‘storm and stress’ in which disruptions in mood, increases in risk-taking behaviour, and increased conflict with parents/guardians can contribute to turbulent thoughts, emotions, and behaviours(Reference Arnett94). The adolescent years bring drastic changes in lifestyle, eating behaviours, and increased exposure to environmental influences, all of which can increase the nutritional vulnerability of this age group(10). Motivations and barriers to healthy food choices in adolescents have been presented in a previous review(Reference Daly, O'Sullivan and Kearney95), with personal factors such as body image, preferences, level of autonomy, interest in health, and nutrition knowledge identified as key considerations for health and food choices in this age group. Additionally, there are numerous psychosocial factors including attitudes, beliefs, self-efficacy, food preferences, mood, and mental health(Reference McClain, Chappuis and Nguyen-Rodriguez96), and biological determinants such as appetite, hunger, taste, weight status, and allergies(Reference Watts, Kanoski and Sanchez-Watts97) which exert strong influences on adolescent eating behaviour and dietary intake.
Self-restriction of food intake and poor eating patterns are considerable challenges to adolescent nutrition and risk factors for poor nutritional status(10). Adolescents have an increased susceptibility to food fads(Reference Athanasian, Lazarevic and Kriegel98), restrictive diets(Reference Raffoul, Leatherdale and Kirkpatrick99) and disordered eating(Reference Smink, van Hoeken and Hoek100), which, in addition to habits of skipping and substituting meals(Reference Monzani, Ricotti and Caputo72), pose significant risks to nutritional adequacy and quality of diets consumed by this age group. Intrapersonal factors such as perceived benefits, self-regulation, goals, and motivation are associated with the consumption of a better-quality diet during adolescence(Reference Kalavana, Maes and De Gucht101). However, these personal factors are subject to strong influences from the outside world, with the effects of the social and physical environment suggested as more prominent in the determination of adolescent food choice than individual factors(Reference Sleddens, Kroeze and Kohl102).
Social factors influencing adolescent nutrition and health
Adolescence is a period of enhanced social interaction and engagement with family members, peers, work colleagues, and wider society. The development of the ‘social brain’ in adolescence makes this age group particularly aware of and receptive to the influence of others on their decision-making(Reference Andrews, Ahmed and Blakemore103). The family unit remains one of the strongest influential factors and has been identified by Irish adolescents as the most important thing in their lives(Reference McNamara, Murphy and Murray104). Parental characteristics such as education level, social class, income, health, marital relationships, parenting style, stress, efficacy, habits, and preferences have been identified as exerting a relevant influence on the lives, and indeed the diets, of adolescents(Reference McNamara, Murphy and Murray104,Reference Zhang, Farris and Sun105) . Parental weight status has been consistently associated with a higher risk of overweight and obesity and less healthful behaviours amongst adolescent offspring(Reference Jiang, Yang and Guo106,Reference Bahreynian, Qorbani and Khaniabadi107) , with parents' attitudes and behaviours relating to diet and exercise often reflected in their children(Reference Fleary and Ettienne108). Siblings also exert an influence on adolescents' dietary behaviours, with a systematic review indicating that this influence is often more negative than positive(Reference Ragelienė and Grønhøj109).
The social and emotional importance of peers increases during adolescence, with peers and social norms exerting strong influences on decision-making and behaviour(Reference Ragelienė and Grønhøj109). This includes dietary behaviours, with adolescents' consumption of both healthy foods, such as wholegrain and dairy, and negative dietary components including fast food, sugar-sweetened beverages, and snacks similar to those of their peers(Reference Chung, Ersig and McCarthy110). This peer influence is present in person and online, with adolescents' social media accounts frequently portraying food images, the majority of which are high in energy and low in nutrients(Reference Holmberg, Chaplin J and Hillman111).
Social class and socioeconomic status are amongst the strongest determinants of health-related behaviours, as financial resources, job type and education level often determine the environments people are exposed to and how they interact with them. A strong income gradient of weight status and dietary intake has been repeatedly observed, with those who experience greater levels of deprivation consistently displaying poorer quality diets and the highest risk of overweight and obesity(Reference Noonan112–Reference Desbouys, De Ridder and Rouche115). A similar socioeconomic gradient has been observed in Ireland, where adolescents from lower affluence backgrounds have lower consumption of fruit and vegetables, higher consumption of sugar-sweetened beverages and chips(Reference Kelly, Callaghan and Molcho116) and a significantly increased risk of overweight/obesity(Reference Moore Heslin, O'Donnell and Kehoe117). Socioeconomic factors are considered high-priority determinants of adolescent obesity due to strong links between social disadvantage and obesity-related behaviours(Reference Inchley, Currie and Jewell118). Socioeconomic position and financial resources determine adolescents' interaction with the wider environment, with those affected by social disadvantage more vulnerable to obesogenic environments due to lack of choice and less financial freedom(119).
Environmental factors influencing adolescent nutrition and health
Physical, economic, social, cultural, and political environments exert major influences on dietary and health behaviours. External environmental factors have been identified as the most influential on the food choice of Irish adolescents, with price, convenience, food characteristics, and the surrounding physical and social environment exerting a greater effect on food choice than intrapersonal factors such as emotions and restraint(Reference Daly, O'Sullivan and Walton120,Reference Share and Stewart-Knox121) . These results indicate that influencing the external food environment and the use of targeted health promotion messaging may aid in improving adolescents' food choices.
Adolescents' consumption of ‘non-core’, high-sugar and high-fat foods is considerably higher outside the home(Reference Toumpakari, Tilling and Haase122), with the offerings of the school and retail environments often saturated by affordable and appealing nutrient-poor, energy-dense foods(Reference Toumpakari, Haase and Johnson123). The presence of school vending machines and additional food outlets close to the school has been associated with poorer dietary intake and an increased risk of obesity in adolescent students(Reference Gonçalves, Figueiredo and Silva124). External food options have been associated with poorer dietary habits in Irish adolescents, with students attending schools that were near fast-food establishments having a lower likelihood of consuming fruit and vegetables(Reference Kelly, Callaghan and Molcho116). The proximity of schools to unhealthy food retailers is a particular issue in Ireland, with 46 % of Irish secondary schools found to be within a 1 km radius of a fast-food restaurant in 2012, with a higher concentration in more deprived areas(Reference Kelly, Callaghan and Molcho125). Available food options can determine adolescents' lunch choices and nutritional intake, with an analysis of lunches consumed by Irish adolescents indicating a poorer nutritional profile of lunches from school and food outlets compared to homemade lunches(Reference Browne, Staines and Barron126). Indeed, results from a systematic review found a direct association between proximity to ‘unhealthy’ food establishments and overweight/obesity in youth(Reference da Costa Peres, Gardone and Costa127). In addition to the physical food environment, online and social media are increasingly becoming the primary avenues for adolescent exposure to food messaging and marketing. From peer posting of food images, prolific food advertising, product placement, and increasing use of online food delivery services, the exposure of adolescents to readily available unhealthy food products is just as, if not more, pervasive in the online space as in the physical environment(Reference Boyland, McGale and Maden128). Consideration of and intervention in all elements of the modern food environment are required to safeguard the health of adolescents.
Consequences of poor nutrition and dietary intake in adolescence
Nutritional deficiencies: impairments in adolescent growth and development
Poor dietary patterns and inadequate intake of nutrients are reflected in suboptimal nutrient status amongst adolescents. Vitamin D deficiency is a highly prevalent condition in this age group, with 80 % of European adolescents displaying suboptimal serum vitamin D concentrations(Reference González-Gross, Valtueña and Breidenassel129). Irish adolescents have a higher prevalence of vitamin D deficiency than younger children(Reference Scully, Laird and Healy130), with a fifth of this group identified as being at an increased risk of deficiency(Reference Cashman, Kehoe and Kearney44). Vitamin D deficiency is negatively associated with adolescent bone density(Reference Sarra, Karantza and Papaefthymiou131) and is possibly linked to an increase in infectious and autoimmune diseases(Reference Patseadou and Haller132), posing concerns for immediate and future health in this age group.
Folate has been highlighted as a nutrient of predominant concern amongst adolescents, with 35 and 30 % of European adolescents displaying insufficient concentrations of plasma folate and erythrocyte folate, respectively(Reference Moreno, Gottrand and Huybrechts70). Additionally, 71 % of European adolescent females displayed erythrocyte folate concentrations below the threshold of 906 nmol/l deemed to be maximally protective against neural tube defects(Reference Moreno, Gottrand and Huybrechts70). In addition to folate, the status of other essential B vitamins including B12, B6 and riboflavin(Reference Kerr, Livingstone and Bates133) have been shown to decrease from childhood to adolescence, potentially due to increased physiological requirements, posing risks to neurological, psychological and cardiovascular health(Reference McNulty, Ward and Hoey134).
Iron deficiency is the leading contributor to adolescent disability-adjusted life years associated with micronutrient deficiencies(Reference Akseer, Al-Gashm and Mehta135) and is amongst the leading causes of death, illness, and disability in young women(Reference Kassebaum, Jasrasaria and Naghavi136). Suboptimal iron status and anaemia in adolescence can have significant effects on academic performance and school attendance due to symptoms of increased fatigue and susceptibility to infectious diseases(10). Intervention to improve the iron status of adolescents, particularly amongst at-risk females, is imperative in protecting the health and future of this vulnerable group.
Analysis of the iodine status of adolescent females in Ireland indicated that this age group was generally iodine sufficient, with median urinary iodine concentration within the lower end of the sufficient range(Reference Mullan, Hamill and Doolan137). However, analysis of similarly aged schoolgirls in the UK found indications of mild iodine deficiency within this age group(Reference Vanderpump, Lazarus and Smyth138), showing that iodine status remains in a relatively precarious position amongst adolescents. With intakes of dairy and fish low amongst Irish adolescents, monitoring of iodine status is required to ensure this age group remains within the range of iodine sufficiency.
Adolescent overweight and obesity
Overweight and obesity is a chronic non-communicable disease and is associated with a range of acute and long-lasting health issues in adolescents(Reference Must and Strauss139,Reference Reinehr140) . Obesity is increasingly identified as disproportionately affecting adolescents, with the recent plateauing of childhood obesity levels observed in affluent countries(Reference Wabitsch, Moss and Kromeyer-Hauschild141), including Ireland(Reference O'Donnell, Buffini and Kehoe142), not reflected in trends in the weight status of adolescents(Reference Moore Heslin, O'Donnell and Kehoe117). A rapidly increasing prevalence of adolescents living with obesity has become apparent in recent years, with one in four adolescents in Europe identified as living with overweight/obesity in 2022(143). Similar rising trends have been observed across several high-income regions including the USA(Reference Fryar, Kruszon-Moran and Gu144) and much of Europe(Reference Shah, Hagell and Cheung145), with adolescent obesity identified as a serious public health challenge(Reference Inchley, Currie and Jewell118). The rising rates of overweight/obesity have also been observed in Irish adolescents, with 24 % of adolescents identified as living with overweight/obesity in 2020, a significant increase from 18 % in 2006 and 13 % in 1990(Reference Moore Heslin, O'Donnell and Kehoe146). The issue of adolescent overweight/obesity is not confined only to high-income countries, with an estimated 21⋅4 % of adolescents in low- to middle-income countries affected by overweight/obesity(Reference Caleyachetty, Thomas and Kengne19).
Overweight/obesity in adolescence has long-term associations with adult weight status, with longitudinal studies consistently reporting a significant association between adolescent overweight/obesity and increased risk of obesity and severe obesity in adulthood(Reference Singh, Mulder and Twisk147–Reference Woo, Zhang and Fenchel150). Additionally, adolescents are increasingly presenting with a higher grade of obesity, with this age group found to display the highest prevalence of severe obesity of all youth age groups(Reference Pinhas-Hamiel, Hamiel and Bendor151). Immediate physical consequences of obesity in adolescents include obstructive sleep apnoea, musculoskeletal complaints, and deteriorations in psychosocial health(Reference Pujalte, Ahanogbe and Thurston152). Living with a high grade of obesity in adolescence is associated with increased cardiometabolic risks, with adolescent-onset obesity demonstrating a more severe lifelong impact of comorbidities than adult-onset obesity(Reference Weihrauch-Blüher, Schwarz and Klusmann153). Obesity is associated with a substantial mental health burden and decreased quality of life, with adolescents living with obesity displaying an increased presentation of psychological comorbidities including depression, anxiety and low self-esteem(Reference Rankin, Matthews and Cobley154). These psychological consequences are often mediated by the negative societal attitudes and weight stigma frequently experienced by those living with obesity, with these pressures having a particularly strong effect on adolescents(Reference Fismen, Galler and Klepp155).
It is suggested that the primary prevention of obesity in adolescence should become a public health priority, with this life stage considered a critical period for obesity development(Reference Narciso, Silva and Rodrigues156). Exposure to obesity-related risk factors increases during this time as youth begin to interact with their environment. The short period in which the exponential increase in adolescent overweight/obesity has occurred indicates that current trends are likely attributed to drastic changes in the modern food environment and lifestyles as opposed to biological changes(Reference Jebeile, Kelly and O'Malley157). As the prevalence of adolescents affected by overweight is currently greater than the prevalence of those living with obesity, there is vast potential for early obesity prevention strategies targeting youth with overweight who are at high risk of developing obesity(Reference Lee and Yoon158). The chronic, refractory nature of obesity, underpinned by mechanisms such as the biological defence of body weight(Reference Shin, Zheng and Berthoud159) and consolidation of dietary and lifestyle behaviours(Reference Craigie, Lake and Kelly87) poses adolescence as a critical stage for effective obesity prevention. Therefore, a drastic scaling up of obesity treatment and prevention is required to subside and prevent the epidemic of adolescent obesity.
Impairments in metabolic health
Dietary risks and overweight/obesity are leading risk factors for non-communicable diseases and are strongly associated with impairments in health and metabolic functioning(143). While the health consequences of a poor-quality diet arise mainly in later life, the quality of the diet consumed during adolescence can mediate the development of metabolic risk factors that contribute to disease development(Reference Dahm, Chomistek and Jakobsen160). Numerous studies have indicated associations between the consumption of a poor-quality diet and increased biomarkers of cardiovascular and metabolic risk amongst adolescents(Reference Summer, Jenkins and Inge161–Reference Hooshmand, Asghari and Yuzbashian165). However, the consequences of a poor-quality diet on metabolic health may not necessarily become immediately apparent, with other analyses indicating a presentation of cardiometabolic risk factors only in late adolescence(Reference Moore, Singer and Bradlee166) or later in life(Reference Winpenny, van Sluijs and Forouhi167).
Adolescents are increasingly presenting with abnormal blood lipid profiles early in life(Reference Nguyen, Kit and Carroll168), with a significant proportion of this age group increasingly identified as having high total cholesterol concentrations and low HDL-cholesterol(Reference Nguyen, Kit and Carroll168). Older youth and adolescents living with obesity are more likely to be affected, with the prevalence of low HDL-cholesterol almost five times higher amongst youth with obesity compared to those with healthy body weight(Reference Nguyen, Kit and Carroll168). Irish adolescents with excess adiposity have been shown to display a more unfavourable metabolic health profile, characterised by increased LDL-cholesterol, TAG and C-reactive protein(Reference Heslin, Walton and Flynn169). Early exposure to CVD risk factors has been robustly linked to poor cardiometabolic health in adulthood, with findings from long-term epidemiological studies indicating that abnormal blood lipid profiles in adolescence predict pre-clinical atherosclerosis(Reference Li, Chen and Srinivasan170), adverse cardiovascular events(Reference Jacobs, Woo and Sinaiko171), type 2 diabetes(Reference Twig, Zucker and Afek172) and premature morbidity and mortality in adulthood(Reference Horesh, Tsur and Bardugo173). Blood lipid screening and evaluation of cardiovascular risk factors in youth have been long recommended by guidelines(174) but are conducted rarely in practice(Reference de Ferranti, Rodday and Parsons175). The increasing presentation of metabolic risk factors early in life accentuates the need for early detection, treatment and mitigatory action for adolescents to aid in the primordial prevention of metabolic diseases.
Opportunities to improve adolescent nutrition and health
Adolescents as agents of change
The years of adolescence are a period of increased opportunity for change as youth become more active agents in their lives(Reference Lerner, Theokas and Jelicic176). The current generation of adolescents is termed the ‘do-it-yourself’ generation based on their increased sense of autonomy and self-reliance due to a heightened awareness of societal issues and the ability to immediately share their thoughts(Reference Singh and Dangmei177). This motivation is apparent in the various youth-led social movements of recent years(Reference O'brien, Selboe and Hayward178,Reference Haenschen and Tedesco179) . Adolescents' desire to improve the status quo is translating into the area of nutrition, with youth-led campaigns such as Bite Back 2030(180) and Act4Food Act4Change(181) leading calls for the improvement of the food system to protect youth health.
The increased autonomy that growing up brings, coupled with the beginnings of financial freedom mean that adolescents exercise greater choice and control over what and when they eat(Reference Patton, Neufeld and Dogra182). Adolescents have been shown to possess a modest level of nutrition knowledge(Reference Sichert-Hellert, Beghin and De Henauw183) and tend to be relatively accurate in their assessments of their diet quality, with a higher level of dietary awareness associated with consumption of a better-quality diet(Reference Vanhelst, Béghin and Duhamel184). However, the accuracy of adolescents' self-assessment of their diet can vary, with a study of Brazilian adolescents showing that more than half of those objectively deemed to have a poor-quality diet considered their diet to be very good/good(Reference Carvalho, Barros Filho and Barros185). Additionally, adolescents sometimes struggle to define some processed and energy-dense foods as being healthy or unhealthy, with mixed dishes, chips, biscuits and confectionery listed as the most difficult foods to categorise(Reference Barco Leme, Fisberg and Baranowski186). Efforts have been made to integrate nutrition education and skills into school curricula in Ireland and elsewhere(187–190), with analyses of the impact of nutrition education interventions showing positive attitudes(Reference Partida, Marshall and Henry191) and some evidence of beneficial dietary behaviour change amongst adolescent participants(Reference Chung and Fong192).
However, nutritional knowledge does not always translate into action, as reflected in the sentiment of ‘We know what we should eat but we don't’ which is pervasive amongst Irish adolescents(Reference Browne, Barron and Staines193). While the provision of tailored evidence-based dietary information is crucial in informing adolescents, education only goes so far in improving health. Indeed, education-based interventions are listed as only more effective than ‘monitoring/doing nothing’ on the Nuffield intervention ladder(Reference Kar-Purkayastha194). There is a need to move towards a whole systems approach to improve the upstream environmental determinants of adolescent health.
Transformation of the food environment to promote health in adolescents
The current trajectories of transitions in the modern food environment are detrimental in their contribution to diet-related non-communicable diseases. There is an urgent need for transformation of the global food system to protect the health and future of both people and planet(Reference Willett, Rockström and Loken195). Independent interaction with and exposure to the wider world occurs for the first time in adolescence, with this age group particularly susceptible to the structure, influences and offerings of the obesogenic food environment. The home, school, retail and online food environments are particularly salient in the lives of adolescents, with each offering unique opportunities for intervention.
Parental modelling of healthy behaviour has been associated with a lower BMI amongst adolescents, with a need for parental consistency in words and actions to encourage a healthy diet and physical activity and create a healthy home environment(Reference Berge, Wall and Bauer196). Family based behavioural interventions targeting diet, sedentary behaviours, physical activity and sleep quality have been recommended as a first-line approach for the treatment of adolescent obesity(Reference Jebeile, Kelly and O'Malley157) and dietary improvement, with a need to tailor interventions to be appropriate, understandable, applicable and easily implemented by the family and adolescents themselves. Additionally, peer-led interventions have been emphasised as feasible and acceptable amongst adolescents(Reference Story, Lytle and Birnbaum197), with evidence indicating some improvements in dietary behaviour using positive peer modelling(Reference Vangeepuram, Angeles and Lopez-Belin198) and youth role models who can serve as beacons of influence(Reference Chung, Vieira and Donley199).
Environmental interventions such as the optimisation of schools and community food systems and regulation of the cost and marketing of food and drinks may be effective in improving adolescent food choices(Reference Evans200). Schools play a critical role in promoting the health of adolescents and can be useful avenues for health promotion and obesity prevention. Results from a qualitative study of Irish secondary schools indicated diverging views between school staff and students regarding facilitators and barriers to healthy eating, with teachers emphasising the role of education and knowledge, while adolescents themselves instead identified the issue of unsupportive food environments(Reference Browne, Barron and Staines193). The study identified a clear mandate by students for schools to create healthy food spaces, implement healthy eating policies and take responsibility for student welfare(Reference Browne, Barron and Staines193). While there is a definite role in equipping adolescents with nutritional literacy to encourage healthy eating, the contribution of the wider food environment in influencing adolescents' food choices should be examined and targeted for change.
The design and offerings of the physical and online retail food environment strongly influence adolescents' food choices. Food retailers and manufacturers have increasingly been engaging in efforts to encourage healthier diets through responsible marketing policies, accessible nutrition labels and the promotion of fruit and vegetables(201). However, certain practices have been highlighted as causes for concern, including different definitions of ‘healthy’ products, slow progress on voluntary product reformulation and poor compliance with recommendations for marketing products to youth(201). There is much scope for improvement in the practices of food retailers, with concerns that certain supermarkets target those in lower socioeconomic areas with unhealthy food choices, likely contributing to obesity and health-related issues in these areas(Reference Cameron, Thornton and McNaughton202). Additionally, online advertising of unhealthy food is prolific and poorly regulated compared to traditional media(Reference Théodore, López-Santiago and Cruz-Casarrubias203). As frequent users of online and social media, adolescent exposure to online food advertising is a common occurrence and can significantly influence their food-related thoughts and behaviours(Reference Boyland, McGale and Maden128). Engagement with food retailers to modify food environments has the potential to be very effective in promoting more healthful dietary choices, as shown by the reductions in intakes of sugar-sweetened beverages as a result of traffic light labelling(Reference Boelsen-Robinson, Backholer and Corben204), increased prices(Reference Blake, Peeters and Lancsar205), and marketing of healthier alternatives within retail settings(Reference von Philipsborn, Stratil and Burns206).
Society has a duty of care towards adolescents and should take responsibility for protecting the health of our future. Supportive food environments that enable and promote healthy choices as the easiest and most accessible options are essential in protecting adolescent health. However, improvement of these food environments will not occur without action across all elements of the environment, with a need for strong policies to motivate and monitor improvements in these areas.
Policies to protect adolescent nutrition and health
The omission of adolescents from health and nutrition policies has been criticised by global leaders in nutrition and health(9), with the need for consideration and direct involvement of adolescents in policy emphasised as key in improving and protecting the health of this age group(Reference Neveux, Ayuandini and Klepp207). Strong policy action to transform the current obesogenic environment is essential in encouraging and promoting healthy behaviours in adolescents and indeed the wider population.
There can be at times a myopic focus on personal responsibility in diet and obesity intervention, with the influence of the social and environmental determinants often overlooked. Leading behavioural scientists have highlighted issues with targeting individual frame actions to combat societal issues without changing the wider system in which these individuals operate(Reference Chater and Loewenstein208). While these ‘individual-frame’ nudge approaches have been proposed as a promising avenue for influencing healthy food choices(Reference Ensaff209), care must be taken not to frame policy issues in terms of the individual rather than the wider system. Indeed, systemic actions such as taxation and regulation can often prove to be more effective in enabling healthier choices and actions(Reference Chater and Loewenstein208). This is evidenced by the taxation of sugar-sweetened beverages, with a 10 % reduction in purchasing and consumption apparent following the introduction of the tax(Reference Teng, Jones and Mizdrak210). A recent systematic review found little evidence of efficacy for individual-orientated and school-based adolescent overweight/obesity prevention measures and emphasised the need to target the environmental determinants of adolescent obesity, with a particular focus on social inequalities(Reference Flodgren, Helleve and Lobstein211).
Improving the nutritional content of commonly consumed foods through reformulation and fortification is a promising method to improve the quality of diets consumed by adolescents(Reference Berner, Keast and Bailey212). Reformulation is likely to have significant impacts on adolescent nutrition, with modelling scenarios from the USA indicating the potential of a 5 % reduction in consumption of total sugars, a 4 % reduction in intake of saturated fat and an 11 % increase in dietary fibre intake if foods popular amongst adolescents were reformulated to meet current USA healthfulness standards(Reference Muth, Karns and Mancino213). Laws regulating the nutritional standards of school food have prompted food manufacturers to reduce the energy, saturated fat, sodium and sugar content of school snack products(Reference Jahn, Cohen and Gorski-Findling214), suggesting that similar laws may have the potential to improve the standard of school food globally. Product reformulation has been proposed to be potentially more effective than enhanced front-of-pack labels in promoting more healthy consumer food purchasing behaviour(Reference Bablani, Ni Mhurchu and Neal215). This may be particularly applicable for adolescents, as a certain degree of nutritional knowledge, literacy and interest is required to interpret nutritional labelling, skills which may be somewhat underdeveloped in this age group.
There is a need for a whole system, life course approach to improve adolescents' dietary intake and health-related behaviours, where rather than just targeting individual, social, or environmental factors in isolation, all determinants are combined and targeted holistically. Adolescents themselves should be at the centre of all interventions and should ideally be involved in each stage of the conception, research, planning, implementation, and evaluation of interventions to ensure they are understandable, applicable and effective for them. The effectiveness of this approach has been evidenced by the CO-CREATE project, in which youth collaborate as equal partners in the development, testing, and communication of policy ideas to address the factors that influence obesity(Reference Neveux, Ayuandini and Klepp207). All resources, interventions, and policies intended for this age group should be tested for acceptability and relevance amongst adolescents themselves, with them involved as ‘active partners’ in local and global efforts to promote health(Reference Neufeld, Andrade and Ballonoff Suleiman216).
Conclusions
Promoting and protecting adolescent health to ensure optimal growth and development is an extremely wise investment to protect our future. Global trends of ageing populations and declines in fertility accentuate the need to avoid a loss of human potential caused by preventable issues in youth. Adolescent health should not be left as solely the responsibility of the health sector, with action required across all areas of society including education, retail, government, and infrastructure to cultivate a more health-promoting environment for this age group. This review highlights the growing breadth of research and evidence pertaining to adolescent nutrition and health. There is now a need for this evidence to be translated into public health action to effect real benefits for adolescents. Failure to improve nutritional intake and dietary behaviours during this life stage is likely to have severe repercussions on lifelong health, well-being, and the ability of future generations to face impending and inevitable challenges. Adolescents require and deserve action in protecting their health, not only as their needs are different to and indeed greater than other stages of life, but also because they, as current and future agents of change, will confer great benefits to society and will be whom we come to rely upon. Therefore, it is imperative that their health is protected and promoted during their formative years to provide them with the greatest opportunities and foundations for success.
Acknowledgements
The authors acknowledge the Irish Section of the Nutrition Society for the opportunity to present this review as part of the Postgraduate Competition 2022.
Financial Support
This work was supported by funding from the Irish Department of Agriculture, Food and the Marine under the project; ‘National Teen's Food Survey II’.
Conflict of Interest
The authors declare no conflict of interest.
Authorship
A. M. H. completed the review article. B. Mc.N. advised in relation to the content and critically reviewed the manuscript. Both authors reviewed and approved the final manuscript submitted for publication.




