Introduction
Acute otitis media is a common ear condition in childhood and a principle reason for children to be seen in primary care, with approximately 75 per cent of children experiencing an episode by the age of five years.Reference Liese, Silfverdal, Giaquinto, Carmona, Larcombe and Garcia-Sicilia1 Some patients develop recurrent acute otitis media, defined as: three or more episodes in 6 months, or four or more episodes in 12 months, with at least one episode in the past 6 months.Reference Venekamp, Mick, Schilder and Nunez2
Conservative and medical measures for recurrent acute otitis media have a mixed evidence base.Reference Cheong and Hussain3 Methods to prevent recurrent acute otitis media can include advising parents on modifiable risk factors, or advocating for pneumococcal and Haemophilus influenzae type B vaccinations, which are known to reduce the frequency of otitis media caused by these organisms.Reference Venekamp, Mick, Schilder and Nunez2 Medical treatment requires either repeated acute courses with a variety of antibiotics, or long-term low-dose antibiotic prophylaxis. Some studies recommend sulfamethoxazole with trimethoprim, but our team feels that anecdotal prescribing trends may have led to the erroneous use of trimethoprim monotherapy for prophylaxis.Reference Principi, Marchisio, Massironi, Grasso and Filiberti4
The surgical insertion of grommets is also offered for recurrent acute otitis media, but evidence for its benefit is mixed.Reference Venekamp, Mick, Schilder and Nunez2,Reference Cheong and Hussain3 Adenoidectomy for recurrent acute otitis media also has no clear evidence of efficacy.Reference Venekamp, Mick, Schilder and Nunez2,Reference Boonacker, Rovers, Browning, Hoes, Schilder and Burton5
Concerns about complications of persistent recurrent acute otitis media may have driven a tendency to prescribe antibiotics, but UK evidence reassuringly suggests a number needed to treat of 4831 to prevent 1 child from developing mastoiditis.Reference Thompson, Gilbert, Long, Saxena, Sharland and Wong6
Given a desire to optimise our service, and the varied strategies available to manage recurrent acute otitis media, our hypothesis was that treatment would be varied between centres. We sought to assess the baseline practice of National Health Service (NHS) ENT departments across England.
Materials and methods
We sourced ENT department contact details using the NHS England website.7 Researchers telephoned the ENT registrar (resident specialist registrar) on-call between 10am and 7pm during weekdays.
A telephone script (Figure 1) was used for up to three contact attempts per site. If the switchboard put the researcher through to specialist registrars covering multiple hospitals, these duplicates were not repeated if they related to the same consultant (attending) cohort. This is a newly devised survey tool related to the baseline recording of practice for the treatment of recurrent acute otitis media.
Fig. 1. Telephone script used when contacting ENT departments.
No research ethics review was sought as no patients were involved in this survey. The study was registered with our institutional review board (Alder Hey Clinical Audit Governance and Quality Assurance Department). As this was a healthcare worker telephone audit of baseline practice, no ethical board review was required.
Clinician respondents were informed of our intention to publish the research and were invited to collaborate in future study.
Results
Telephone surveys were conducted between March 2020 and June 2020. Of 130 NHS Trusts, 23 centres did not respond. Ninety-six centres (74 per cent) provided complete information. Only the data from the centres with complete information were included in the final analysis.
Trimethoprim prophylaxis was prescribed by 33 out of 96 centres (34 per cent). Prophylaxis duration was varied (Figure 2).
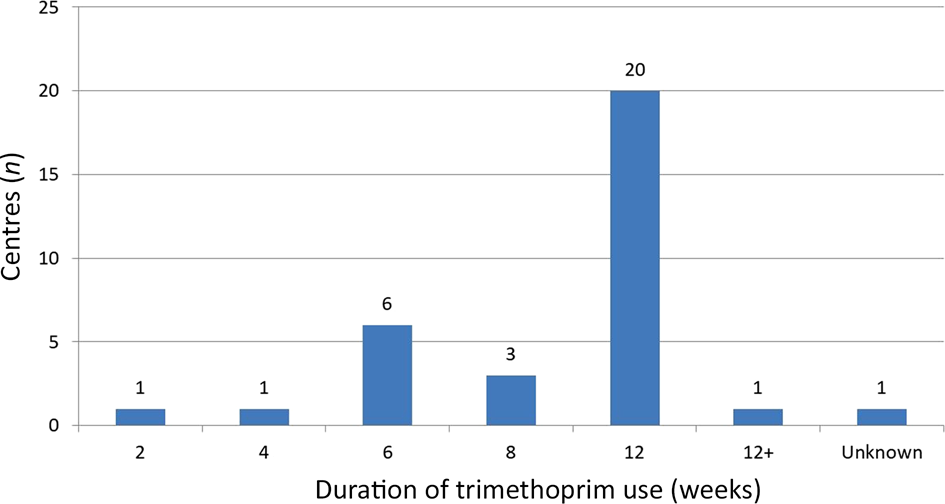
Fig. 2. Numbers of centres prescribing trimethoprim, by duration of use in weeks.
There are multiple other antibiotics prescribed either as primary prophylaxis or secondary alternatives (Figure 3). The most common durations for alternative antibiotics were 12 weeks (13 centres) or 6 weeks (11 centres). Azithromycin was offered for 12 weeks by eight centres and amoxicillin was offered for 12 weeks by five centres. No centres offered alternative prophylaxis for longer than 12 weeks.
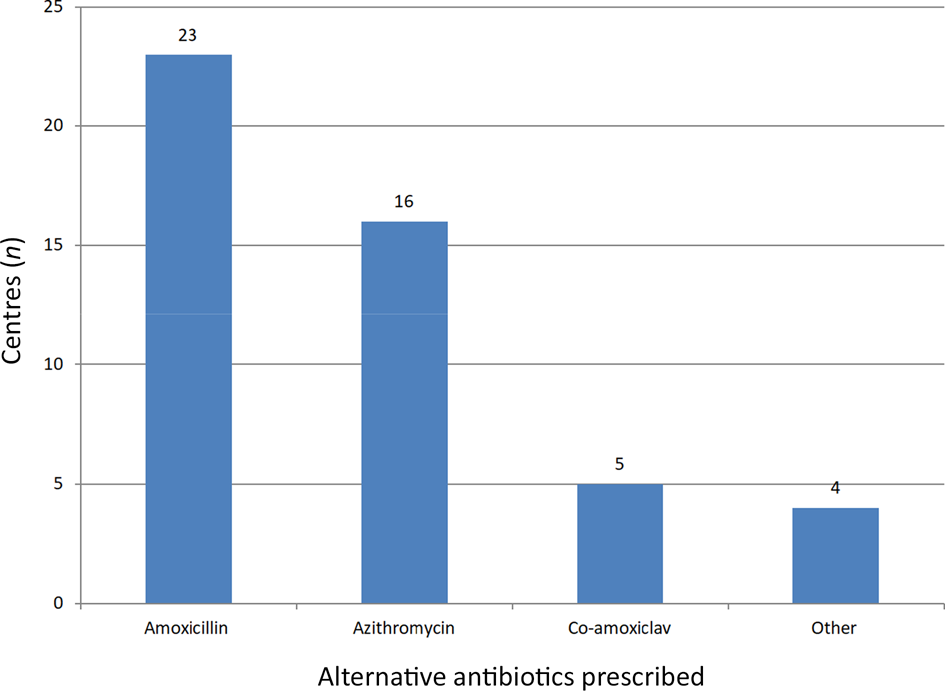
Fig. 3. Numbers of centres prescribing alternative antibiotics.
No prophylactic antibiotics were offered by 29 out of 96 centres (30 per cent). Four of these centres also did not offer grommets (i.e. no antibiotic or surgical treatment). Grommets were offered by 87 centres (91 per cent). Six of these centres reported trying to ‘avoid’ grommets, and used this treatment as a ‘last resort’. Two centres used grommet surgery in conjunction with adenoidectomy after failed medical treatment.
Discussion
We believe this is the first published survey of secondary care treatment practices for recurrent acute otitis media in the UK. ENT department treatment of recurrent acute otitis media across England is varied. Although not every centre in England was included in this comparison of practice, almost three-quarters of centres contributed, and our survey offers a meaningful insight into practice across the nation. It is important to establish reliable recommendations to effectively reduce recurrence, as symptoms in young children can have a significant effect on their quality of life, as well as on that of their families and carers.Reference Brouwer, Rovers, Maillé, Veenhoven, Grobbee and Sanders8
• Recurrent acute otitis media treatment by ENT departments across England is not uniform
• Trimethoprim prophylaxis for recurrent acute otitis media does not have a robust evidence base
• Antibiotic first- and second-line prophylaxis offered by ENT varies across centres, as does the role of grommet surgery
• A new collaborative prospective study of effective treatments for recurrent acute otitis media in England is recommended
Where antibiotics are used, there is heterogeneity in first- and second-line treatment. A third of centres used trimethoprim, which has no evidence base for treating the most likely pathogens in this condition.Reference Williams, Chalmers, Stange, Chalmers and Bowlin9 Almost a third of centres do not prescribe prophylactic antibiotics, which may relate to: perceptions about the causative organism, antibiotic side effects or concerns about antibiotic resistance. Centres prescribing azithromycin may have been influenced by its common use for many respiratory conditions as a prophylactic for between 6 weeks and 12 months.Reference Corvol, Taytard, Thouvenin, Périsson, Nathan and Clement10 The role of grommets was varied, ranging from never being offered to being offered as the sole, primary or second-line treatment in some centres. We did not collect data on the specific barriers and facilitators when centres offered grommets. However, future studies may wish to undertake qualitative interviews to explore this, and barriers to antimicrobial stewardship, further.
The timing of this survey (during the first UK wave of the coronavirus disease 2019 (Covid-19)) pandemic may have influenced our findings regarding prescribing habits. Interviewers were encouraged to describe historical (pre-coronavirus) prescribing practices, as many centres had adjusted their in-person out-patient activity at this time. In addition, the phrasing of our interview schedule deliberately asked ‘Do any of the consultants prescribe…’, as during our study development, many registrars and consultants reported that even a single consultant's practice during training had influenced their own subsequent prescribing behaviour. Nonetheless, this may overestimate how frequently antibiotic prophylaxis is actually prescribed in England currently, and it may not reflect the individual and varied prescribing preferences of every consultant at the centres we surveyed.
In the USA, the American Academy of Pediatrics and American Academy of Family Physicians discourage the prescription of prophylactic antibiotics, in order to reduce the frequency of acute otitis media episodes in children with recurrent acute otitis media, but consider grommets a treatment option.Reference Lieberthal, Carroll, Chonmaitree, Ganiats, Hoberman and Jackson11
A recent meta-analysis of European guidelines for acute otitis media found national guidelines for only 17 of 32 European countries. These demonstrated varied approaches to antibiotic administration, both between countries and against World Health Organization guidelines. Long-term prophylaxis and recurrent acute otitis media were not the focus of that paper.Reference Suzuki, Dewez, Nijman and Yeung12
Equipoise regarding treatment may lead to pragmatic collaborative approaches that cannot be appreciated from this survey. A Cochrane review concluded ‘Antibiotics will reduce the number of episodes of acute otitis media per year from around three to around 1.5’, but this needs to be considered in the context of longer-term antibiotic side effects and worsening antimicrobial resistance.Reference Leach and Morris13 Recurrent acute otitis media can have implications for hearing, balance, and the development of communication and socialisation for the child. Further to antibiotic side effects and potential grommet-related complications, parents and physicians may need to weigh the individual patient's co-morbidities against the risk of complications from repeat infection or general anaesthetic.
Evidence comparing culture-specific antibiotic treatment with standard care suggested that an individualised approach can reduce recurrent acute otitis media incidence and grommet placement, but logistic and cost implications were not considered.Reference Pichichero, Casey and Almudevar14 Another Cochrane review found only five randomised, controlled trials, with an unclear or high risk of bias (conducted prior to the introduction of pneumococcal vaccination).Reference Venekamp, Mick, Schilder and Nunez2 They concluded low or very low-quality evidence, suggesting that children receiving grommets were less likely to have recurrences compared to those receiving conservative management or placebo, but the effect was modest, with around one fewer episode at 6 months and a less noticeable effect by 12 months.
Following our survey, we hope discussion and comparison will be stimulated internationally in this area. Further work is planned in the form of a multicentre trial assessing antibiotic treatment for recurrent acute otitis media, which will try and establish safe and effective treatment recommendations in an era of increasing need for antimicrobial stewardship and evidence-based medicine.
Data availability statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Competing interests
The first author receives funding from the Wellcome Trust (grant number: 203919/Z/16/Z). There are no other conflicts of interest, financial or otherwise, that are directly or indirectly related to this manuscript, for any of the co-authors.





