The advances of neurosciences in mental healthcare underline the importance of integrating neuropsychiatry and clinical neuroscience in the training of mental health professionals.Reference Insel and Quirion1 There is increasing international recognition that the future professional role of a psychiatrist will demand a greater knowledge of brain functions than that which is currently taught.Reference Kandel2 The ability of tomorrow's psychiatrists to give their patients the benefits of a neuroscience-enhanced understanding of psychopathology, diagnosis and treatment is related to the capacity of postgraduate training programmes to provide adequate training in basic, applied and clinical neuroscience.Reference Benjamin3 This training should be understood inclusively, in conjunction with the humanistic aspects of psychiatry and not in a dualistic manner.
Importantly, psychiatric diagnosis relies on cross-sectional biobehavioural dimensions that are common to multiple categories of heterogeneous disorders. Research domain criteria (RDoC)Reference Cuthbert and Insel4 have been proposed to advance the research into aetiology and pathophysiology as well as the development of new treatments. This advancement relies on adequate knowledge not only of the psychopathology of mental disorders but also of their neuropsychiatric and neuroscientific foundations.
The World Health Organization (WHO) considers neuropsychiatric disorders to be the most important causes of disability worldwide,5 and the psychiatric complications of neurological diseases are considered to cause major distress and burden to patients and their carers.Reference Mitchell and Agrawal6 However, the majority of hospital-based neuropsychiatric disease is still being treated by liaison psychiatrists, old age psychiatrists, general adult psychiatrists and, often reluctantly, by medical teams. This is due not only to a lack of specialist neuropsychiatrists but also to the inadequate training for hospital specialists,Reference Mitchell and Agrawal6 which is an international problem.
Training, practice and continuing professional development in neuropsychiatry vary across different countries. There is a substantial global recognition of the need to incorporate this field into the postgraduate training of psychiatrists.Reference Benjamin3,Reference Mitchell and Agrawal6–Reference Ross, Travis and Arbuckle8 However, the definition of neuropsychiatry is still unclear in different countries, varying from a more global concept of neuropsychiatryReference Berrios and Markova9,Reference Agrawal, Bhattacharya and Rickards10 and clinical neuroscience to the basic neurological concepts that are taught during medical school or postgraduate training. Several related terms, such as ‘biological psychiatry’, ‘organic psychiatry’, ‘cognitive neurosciences’ and ‘behavioural neurology’, have perpetuated this confusion.Reference Mitchell and Agrawal6 A better definition and a specific curriculum are needed. This differentiation of neuropsychiatry as a specialty is also supported by numerous textbooks in this area.Reference Silver11
As regards neuropsychiatry as part of the psychiatrist's training curricula,Reference Faulkner, Juul, Pascuzzi, Aminoff, Crumrine and Dekosky12 it seems that most training has been placed in the neurology training period, without really developing a specific curriculum for neuropsychiatry. Although psychiatry and neurology both deal with brain diseases, there is a need to have a combined neuropsychiatric approach, which requires the delineation of a neuropsychiatric territory and the competencies that should be achieved.Reference Sachdev and Mohan13
This is not a new concept, as previous surveys have been conducted on both neuroscience and neuropsychiatry curricula. For example, in Australia and the USA this issue has been addressed and results have pointed to the necessity and readiness of psychiatry training programmes to provide increased neuroscience and neuropsychiatry education.Reference Mitchell and Agrawal6,Reference Rego, Eratne, Walterfang and Velakoulis14 Importantly, an international curriculum for neuropsychiatry and behavioural neurology has been developed describing in detail the objectives of training in neuropsychiatry and the key competencies that should be achieved.Reference Benjamin3,Reference Sachdev and Mohan13 Other studies have investigated the content of the training provided in psychiatry programmes, reporting that in 80% of the countries studied, a placement in a non-psychiatric specialty such as neurology or internal medicine was mandatory, although it was not always considered enough or well-structured.Reference Juul, Lyness, Thomas and Faulkner15,Reference Baessler, Zafar, Gargot, Pinto da Costa, Biskup and De Picker16 A survey of 100 trainees in England investigated the attitudes of neurologists and psychiatrists to strengthening their links, showing that psychiatrists, in general, were even more aware of links between the two specialties.Reference Schon, MacKay and Fernandez17 A survey in Australia involving 47 trainees who had worked in the neuropsychiatry unit at the Royal Melbourne Hospital reported very positive feedback, particularly on the breadth of clinical presentations, research and educational opportunities.Reference Rego, Eratne, Walterfang and Velakoulis14 Other studies that assessed the attitudes of trainees, chief residents or residency programme directors in the USA described broad support for neuroscience education and a desire to increase its representation in psychiatric training.Reference Fung, Akil, Widge, Roberts and Etkin18–Reference Benjamin, Travis, Cooper, Dickey and Reardon20
Some countries, such as the USA,Reference Silver11,Reference Coffey, Silver, McAllister and Restak21 and Australia22 have developed specific curricula for neuropsychiatry trainees, recognising neuropsychiatry as a subspecialty. In the UK, while neuropsychiatry is not formally endorsed as a subspecialty by the Gneral Medical Council (GMC), advanced training and education in neuropsychiatry are available through specialist training posts and through the MSc in Clinical Psychiatry provided by the University of Birmingham and King's College London.23
However, to date little is known about the opinions of early career psychiatrists (ECPs) around the world on their neuropsychiatry training experiences. Their opinions regarding barriers to neuropsychiatry training and practice have not been addressed. This study aimed to investigate the views of ECPs on their training experiences and the barriers to neuropsychiatry training and practice across different countries around the world.
Method
Study design
This online survey was distributed to ECPs in 35 countries worldwide (Australia, Austria, United Arab Emirates, Brazil, Chile, Croatia, Ecuador, Egypt, El Salvador, France, Germany, Guinea-Bissau, Indonesia, Iran, Italy, Japan, Kosovo, North Macedonia, Malaysia, Nepal, Nigeria, Philippines, Portugal, Russia, Sri Lanka, Slovenia, Spain, Switzerland, Sweden, South Africa, Taiwan, Thailand, Turkey, the UK and USA). In this study ECPs is used to refer to psychiatric trainees and psychiatrists in their first 7 years of working as consultants.
Study instrument
The questionnaire was developed in collaboration with the Spanish Clinical Neuroscience Section, the European Federation of Psychiatric Trainees (EFPT) and the Section of Early Career Psychiatrists of the World Psychiatric Association (WPA).
The questionnaire was developed in English and asked participants about their training opportunities in neuropsychiatry. The questions were grouped into four main domains: (I) sociodemographic details; (II) neuropsychiatry training experience; (III) barriers to neuropsychiatry training; and (IV) opinions regarding neuropsychiatry training/practice.
The following description of the term ‘neuropsychiatry' was included at the beginning of the survey: ‘Neuropsychiatry in a broad sense refers to the clinical study, evaluation and treatment of brain–behavior relationships as revealed through the psychiatric manifestations of neurological disorders and the neurobiology of psychiatric disorders’.Reference Benjamin3
In the literature the terms ‘neuropsychiatry', ‘neuroscience' and ‘clinical neuroscience' are used to refer to components of neuropsychiatry training, and in this article we retain the term.
Participants
Participants for this study met the following inclusion criteria: qualified medical doctor training in psychiatry, or psychiatrist in the first 7 years of working as a consultant.
Data collection
The questionnaire was distributed in each country through the study's national representatives, who were responsible for contacting their national psychiatry associations or scientific societies.
Participants were contacted by email and an online questionnaire was sent via Survey Monkey with a URL to a survey webpage. Information about the study was provided on the webpage. Responses were collected between 1 January to 31 March 2018.
Data analysis
Data were analysed using SPSS version 17.0 for Windows. Data are presented as means with standard deviations (s.d.) or frequencies and percentages, as appropriate. Missing data were omitted on an analysis-by-analysis basis and valid percentages are reported.
Consent and study approvals
By responding to the questionnaire, participants provided informed consent for their anonymous responses to be used in this study.
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
This study did not involve a prospective evaluation or involve animals or vulnerable participants (e.g. patients). The research did not pose risks, harm or disadvantage to the participants, as it assessed anonymous data from competent adults only. According to the procedures in comparable cases, ethical approval was therefore not required.
Results
Sociodemographic data
A total of 522 participants took part in this study and 509 fully completed the questionnaire. Sociodemographic data are shown in Table 1. The mean age was 33.5 years (s.d. = 6.1 years); 53% (n = 275) were female and 46% (n = 240) male. Most responses were collected from Europe (n = 234, 45%) and Asia (n = 217, 42%). Only 3.5% of the sample were currently specialised in neuropsychiatry.
Table 1 Sociodemographic data for respondents

The majority of the respondents (n = 432, 83%) reported that they had a mandatory rotation in neurology; fewer (n = 71, 14%) said that this rotation was not mandatory. In countries where this rotation was mandatory, its duration ranged from 1 to 6 months (mean 2.6, s.d. = 1.4).
Neuropsychiatry units and training experiences
A quarter of the respondents (n = 139, 27%) reported that they knew of a neuropsychiatry unit in their city, but the majority (n = 375, 72%) of the participants did not answer this question or answered ‘no’ or ‘I don't know’. Nearly half of the participants (n = 241, 46%) reported that a clinical neuropsychiatry rotation was not mandatory, and only a few (n = 82, 16%) reported neuropsychiatry as mandatory (Table 2).
Table 2 Respondents’ description of their neuropsychiatry training

The majority (n = 333, 64%) of participants were not aware of any neuropsychiatry postgraduate training in clinical neuropsychiatry in their countries; many (n = 312, 60%) were not interested in going abroad for further training in neuropsychiatry. Some (n = 304, 58%) reported that they were expected to get involved in research projects in neuropsychiatry and fewer (n = 138, 26%) were expected to conduct a PhD in neuropsychiatry or clinical neuroscience. Among the main fields to go abroad for during the postgraduate training period, some (n = 75, 14%) rated neuroscience among the most requested fields (neuropsychiatry was not included as a choice in this question) (Table 2). Others requested fields such as psychotherapy (n = 66, 13%) and clinical management strategies (n = 141, 27%).
Barriers to and implementation of neuropsychiatry training
Lack of interest among specialty societies, lack of time during postgraduate training, and political and economic limitations were the main barriers to the implementation of neuropsychiatry in training (Table 3).
Table 3 Respondents’ opinions regarding neuropsychiatry training
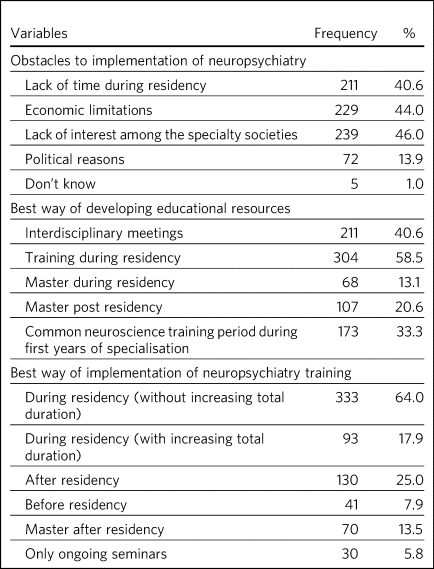
The preferred timings on when best to provide neuropsychiatry training were during and after the training period (n = 333, 64% and n = 130, 24% respectively). However, most respondents who chose ‘during training’ preferred this to be done by increasing the duration of training (n = 93, 18%), compared with ‘without increasing duration’ (n = 33, 6%). Just a few (n = 41, 8%) thought it should be implemented before psychiatry training.
On a Likert scale from 1 to 10, most agreed on the priority for a better relationship between neurology and psychiatry (mean 8.4, s.d. = 1.8), followed by the necessity for further training in neuropsychiatry (mean 7.7, s.d. = 1.9), as well as the need for further training in research into neuropsychiatry (mean 7.7, s.d. = 1.9) and research into neuroscience (mean 7.4, s.d. = 2.1) (Tables 3 and 4).
Table 4 Opinions regarding neuropsychiatry training/practice (Likert scale of 1–10, where 10 is maximum agreement)

Discussion
Key findings
This study provides further evidence of an ongoing unmet need in the provision of pathways to gaining neuropsychiatry practice and raises awareness of the willingness for further training in neuropsychiatry among ECPs in different parts of the world. Most respondents were not aware of any neuropsychiatric training in their curricula or of local neuropsychiatric units. Most agreed that training in neuropsychiatry training should be done during the psychiatry training period or after training. Of those who considered that training in neuropsychiatry should take place during psychiatry training, most felt this should be achieved by increasing the duration of training.
Neuropsychiatry education is not integrated into psychiatric training in most countries. The majority of the participants reported that learning about neuropsychiatry is not included in their psychiatric curricula as a mandatory rotation. Lack of interest among specialty societies, lack of time during postgraduate training, political and economic reasons are regarded as main barriers.
Comparison with the literature
Regarding the most general sociodemographic details of this survey, we know that psychiatric training has changed across different countries in recent decades and that several subspecialties, such as psychotherapy and addiction, have been integrated into psychiatric curricula as mandatory rotations, not only in high-income but also in low- and middle-income countries on different continents;Reference Fiorillo, Luciano, Giacco, Del Vecchio, Baldass and De Vriendt24-Reference Brittlebank, Hermans, Bhugra, Pinto da Costa, Rojnic-Kuzman and Fiorillo27 this has not been the case for neuropsychiatry. This finding is consistent with previous reports from the UK, in which 73% of the sample had no previous clinical training experience in neuropsychiatry, but 74% expressed a wish specifically to train in this subject and 87% stated a desire for a clearly defined curriculum.Reference Conn28,Reference Rai, Karki, Thapaliya and Molina29 In the UK the RCPsych curriculum was amended to enhance neuroscience and neuropsychiatry (MRCPsych Syllabus amendment23). According to a survey of psychiatry residency programme directors in the USA, 64% and 60% agreed that knowledge of neuropsychiatry and knowledge of psychiatric neuroscience respectively were either very important or critically important for providing excellent care.Reference Benjamin, Travis, Cooper, Dickey and Reardon20
Regarding the most general sociodemographic details of this survey, we know that psychiatric training has changed across different countries in recent decades and that several subspecialties, such as psychotherapy and addiction, have been integrated into psychiatric curricula as mandatory rotations, not only in high-income but also in low- and middle-income countries on different continents;Reference Fiorillo, Luciano, Giacco, Del Vecchio, Baldass and De Vriendt24-Reference Brittlebank, Hermans, Bhugra, Pinto da Costa, Rojnic-Kuzman and Fiorillo27 this has not been the case for neuropsychiatry. This finding is consistent with previous reports from the UK, in which 73% of the sample had no previous clinical training experience in neuropsychiatry, but 74% expressed a wish specifically to train in this subject and 87% stated a desire for a clearly defined curriculum.Reference Conn28,Reference Rai, Karki, Thapaliya and Molina29 In the UK the RCPsych curriculum was amended to enhance neuroscience and neuropsychiatry (MRCPsych Syllabus amendment23). According to a survey of psychiatry residency programme directors in the USA, 64% and 60% agreed that knowledge of neuropsychiatry and knowledge of psychiatric neuroscience respectively were either very important or critically important for providing excellent care.Reference Benjamin, Travis, Cooper, Dickey and Reardon20
In the subsample from Nepal in our survey, two-thirds of respondents stated that there is no neuropsychiatry training during psychiatry training in their country. However, in a study on neuropsychiatry training in Nepal the majority of ECPs (85%) stated that neurology is integrated into their training course as a mandatory rotation.Reference Rai, Karki, Thapaliya and Molina29 These results highlight the need for specific training in neuropsychiatry beyond the neurology rotation.
As regards barriers to neuropsychiatry training and views on its implementation, more than half of the participants (58.5%) expressed interest in participating in neuropsychiatric research projects. The increasing interest of psychiatrists, particularly ECPs, has also been previously reported in Asia.Reference Roche, Fung, Ransing, Noor, Shalbafan and El Hayek30 This is consistent with other findings in Nepal concerning the need for future training in neuropsychiatry, where the median score on a ten-point Likert scale was 7.9.Reference Rai, Karki, Thapaliya and Molina29 In two different USA nationwide surveys, most participants (chairs of psychiatry departments, psychiatrists and psychiatric trainees) agreed with the need for more neuroscience education.Reference Fung, Akil, Widge, Roberts and Etkin18,Reference Benjamin, Travis, Cooper, Dickey and Reardon20 Similar results were reported in the UK.Reference Conn28
In addition, 24% of participants in our study stated that the best way to develop their knowledge in this field is the integration of neuropsychiatry training into the psychiatric training course: 18% by modifying the duration of postgraduate training and 6% without modifying it. Only 8% stated neuropsychiatry training should be done before postgraduate training. Of note, 25% considered it should be done after postgraduate training. This is a very interesting finding because, after the modification of psychiatric training courses as a specialty for medical graduate physicians, the duration of training in psychiatry has been increased from 4 to 5 years in almost all European countries (Table 1), including education on subspecialties such as addiction and psychotherapy.Reference Eissazade, Shalbafan, Eftekhar Ardebili and Pinto da Costa25 The knowledge, skills and competencies in neuropsychiatry could be included as core components of the main curriculum of training in psychiatry, as training modules as part of the main rotations, such as acute in-patient unit rotations or community psychiatry placements, which are the two main common periods of training of psychiatrists worldwide.Reference Brittlebank, Hermans, Bhugra, Pinto da Costa, Rojnic-Kuzman and Fiorillo27
Our findings suggest that lack of interest among specialty societies, lack of time during postgraduate training, and political and economic limitations are the main obstacles to the implementation of neuropsychiatry training. Similarly, previous studies in the USAReference Benjamin, Travis, Cooper, Dickey and Reardon20 found insufficient neuropsychiatry faculty (39%) and absence of neuroscience faculty (36%) to be the main barriers to the implementation of neuropsychiatry, even if three-quarters indicated that faculty resources were available in their departments. This means that even in the presence of several curriculum ideas that have been promulgated in this area,Reference Benjamin3,Reference Sachdev and Mohan13 their adoption is not yet widespread and a lack of structural or faculty resources limits their adequate implementation.
With respect to the neuropsychiatry training experience, about three-quarters of our participants were not aware of neuropsychiatric clinics in their city or district. Although neuropsychiatric clinics have been developed and increased in recent decades,Reference Danes-Brozek31 there is a lack of awareness about them among ECPs. This highlights the need for greater collaboration between neuropsychiatric clinics and psychiatric departments. Neuropsychiatry and brain and cognition clinics should pay attention to this and try to develop their collaboration with other psychiatrists.
Strengths and limitations
To the best of our knowledge, this is the first international survey on the experiences, attitudes and challenges of ECPs regarding neuropsychiatry in their psychiatric training course and practice.
However, several limitations should be acknowledged. The concepts of neuropsychiatry and (clinical) neuroscience are still difficult to establish, since these are terms elusive in natureReference Berrios and Markova9,Reference Martin32 and understanding of them might vary across different countries. In some countries training in these fields might be limited to some training in neurology, basic neuroscience or just research into the biological components of mental disorders. We tried to unpick this in this survey by enquiring about specific rotations in neurology or neuropsychiatry. Participants’ responses might be affected by a lack of a similar understanding of what neuropsychiatry is, as well as differences in their prior exposure to neuropsychiatry.
Another limitation of our survey is the small sample from some world regions, such as the UK, USA, Australia and Africa, as the sample mainly came from Asian and European countries. This limits the generalisation of our findings.
Implications of the findings for practice and research
There is a need for coherent and shared international consensus on what constitutes neuropsychiatry and what its training curriculum should entail. These findings can help guide scientific societies and professional organisations representing psychiatrists or responsible for setting the standards for postgraduate training in psychiatry towards further consensus on these concepts.
As shown by previous studies, a neuropsychiatry provision closely allied with neuroscience centres should be adopted widely to bring consistency across international neuropsychiatry training pathways to try to avoid undesirable variability and unmet needs.Reference Agrawal, Bhattacharya and Rickards10,Reference Agrawal, Fleminger, Ring and Deb33
It has also been stated that training can improve clinical careReference van Os, van den Brink, Tiemens, Jenner, van der Meer and Ormel34 but these need to be accompanied by systemic local organisational change to be effective.Reference Gilbody, Whitty, Grimshaw and Thomas35
The fact that more than half of the participants showed an interest in neuropsychiatric research projects also emphasises a need for more structured and well-designed courses of neuropsychiatry in psychiatric training across the world. International associations such as the WPA could be involved in such processes. This might help psychiatric departments, particularly in low- and middle-income countries, to improve neuropsychiatric education.
Action is warranted to address our findings that the lack of interest among specialty societies, lack of time during postgraduate training, and political and economic limitations might be among the main obstacles to training in neuropsychiatry.
About the authors
Rosa Molina-Ruiz, Department of Psychiatry, Hospital Clínico Universitario San Carlos, Madrid, Spain; Yukako Nakagami, Department of Psychiatry, Kyoto University Graduate School of Medicine, Kyoto, Japan. Sabrina Mörkl, Department of Psychiatry and Psychotherapeutic Medicine, Medical University of Graz, Graz, Austria. Martin Vargas, Facultad de Medicina, Hospital Universitario Río Hortega, Universidad de Valladolid, Valladolid, Spain. Mohammadreza Shalbafan, Mental Health Research Center, Psychosocial Health Research Institute (PHRI), Department of Psychiatry, School of Medicine, Iran University of Medical Sciences, Tehran, Iran; and Brain and Cognition Clinic, Institute for Cognitive Sciences Studies, Tehran, Iran. Jane Pei-Chen Chang, Department of Psychiatry, China Medical University Hospital, Taichung, Taiwan. Yugesh Rai, Essex Partnership University NHS Foundation Trust, Colchester, UK. Champion T. Seun-Fadipe, Nottinghamshire Healthcare NHS Trust, Nottingham, UK. Gamze Erzin, Department of Psychiatry, Diskapi Training and Research Hospital, Ankara, Turkey. Firoz Kazhungil, NMC Royal Hospital, Abu Dhabi, United Arab Emirates. Pablo Vidal, Hospitalario Universitario de A Coruña, A Coruña, Spain. Sawitri Brihastami, Department of Psychiatry, Faculty of Medicine, Universitas Airlangga, Surabaya, Indonesia. Eren Yıldızhan, Department of Neurology and Neurosurgery, Bakirkoy Mazhar Osman Research and Training Hospital for Psychiatry, Istanbul, Turkey. Tanay Maiti, South West Yorkshire NHS Foundation Trust, Dewsbury, UK. Ilya Fedotov, Ryazan State Medical University, Ryazan, Russia. Irena Rojnic-Palavra, University Psychiatric Hospital Sveti Ivan, Zagreb, Croatia. Toru Horinouchi, Department of Psychiatry and Neurology, Hokkaido University Graduate School of Medicine, Sapporo, Japan. Vasanth Renganathan, Fortis Malar Hospital, Chennai, India. Mariana Pinto da Costa, Institute of Psychiatry, Psychology & Neuroscience, King's College London, London, UK; and Institute of Biomedical Sciences Abel Salazar, University of Porto, Porto, Portugal.
Data availability
The data is available from the corresponding author on reasonable request.
Acknowledgements
We would like to thank Dr Irene Serrano for providing support with the initial exploratory statistical analysis of this study. We would also like to thank Dr Lee Abreo for proofreading the final version of this article.
Author contributions
R.M.-R. designed the study and M.P.d.C. provided supervision. Y.N., J.P.-C.C. and M.V. conducted the statistical analysis. R.M.-R. and M.P.d.C. drafted the manuscript. All authors contributed to the data collection. All authors commented on and approved the final manuscript. R.M.R. is the guarantor of this study.
Funding
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Declaration of interest
None.








eLetters
No eLetters have been published for this article.