Almost all physicians in a hospital prescribe antimicrobials, and their attitudes toward prescribing antimicrobials are influenced by the characteristics of the patient population, the physician’s prescribing habits, local resistance patterns, and the antimicrobial agents available in their hospital. Reference Teixeira Rodrigues, Roque, Falcao, Figueiras and Herdeiro1 Although prescribing antimicrobials for a severe bacterial infection is appropriate, inappropriate antimicrobial use can result in various, adverse outcomes, including antimicrobial resistance (AMR), drug toxicity, and even death. Reference van de Sande-Bruinsma, Grundmann and Verloo2–Reference Davey and Marwick5
Infectious diseases (ID) consultation has contributed to reducing inappropriate antimicrobial prescriptions and has thereby improved patient outcomes. Reference Spec, Olsen, Raval and Powderly6–Reference Goto, Jones and Schweizer8 Typically, the ID consultant provides a recommendation after examining a patient, monitors the patient daily, then signs off when deemed appropriate after issuing final recommendations on continued care. Signing off occurs at the discretion of each ID consultant, and its optimal timing remains unclear. Even the best recommendations are rendered ineffective Reference Lo, Rezai and Evans9 if the patient fails to adhere to the recommendations, and understanding the factors affecting adherence is necessary to improve post–sign-off patient care. However, research on health-related events after ID consultants have signed off is scarce. The incidences of other healthcare-associated infections (HAIs) during index hospitalization and antimicrobial use not included in the ID consultant’s final recommendations remain unknown, as do other outcomes such as nosocomial onset of fever, new-onset HAIs, and adverse drug effects (ADEs) caused by the recommended antimicrobial agents.
We investigated the clinical courses of patients after ID consultants signed off, including additional antimicrobial use and in-hospital complications related to antimicrobial use, such as antimicrobial-associated ADEs and HAIs. Our research included the epidemiology and predictors of nonadherence to ID recommendations after the termination of consultation.
Methods
Study design and setting
This retrospective cohort study included data from January 2019 to December 2019 at Tokyo Metropolitan Tama Medical Center, a 790-bed tertiary-care center with 34 subspecialties, including a division of infectious diseases. In July 2013, ID consultation was begun by an infectious diseases physician certified by the American Board of Internal Medicine (ABIM). ID consultation at the study center is delivered in a manner similar to that at US institutions. The division of infectious diseases at the study center has no dedicated hospital beds and only provides hospital-wide ID consultations on request. Overall, ∼700 patients annually receive ID consultations at the request of the primary care team. Attending physicians may request consultation via a telephone call to the ID physician in charge. These requests are answered during working hours, and only urgent cases are handled overnight or on weekends. During the study period, 2 board-certified attending physicians with ID consultation credentials, 2 ID fellows, and rotating residents provided ID consultation. The ID consultation team performed daily rounds, including on weekends, to monitor the patients under consultation and documented their clinical assessments and treatment recommendations in the electronic medical records (EMRs) until signing off. All of these recommendations were later communicated by telephone or in person to the primary physician. All ID recommendations and the decision to sign off were made under the supervision of the attending ID physicians, who also made the decision to sign-off on ID consultations for clinically stable patients, those receiving no antimicrobial therapy, and those with a management plan for any current infection.
Participants
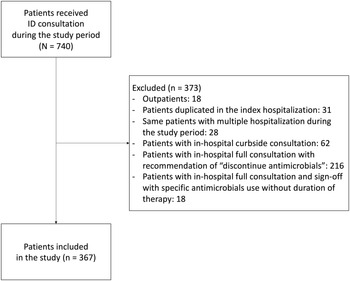
Patients who received ID consultation or treatment recommendations for a confirmed or suspected infection were enrolled. If the patients had received multiple ID consultations during index hospitalization or were admitted more than once during the study period, only the first ID consultation was included. The exclusion criteria were (1) outpatients, (2) curbside consultations (ie, telephone consultations), (3) cases in which an ID consultant recommended discontinuation of antimicrobial therapy as the final recommendation, and (4) cases in which an ID consultant recommended the use of specific antimicrobials without specifying the treatment period as the final recommendation. The institutional review board at the study center approved this study.
Data collection and definitions
All data were retrospectively extracted by a manual review of EMRs. Data on patient demographics, antimicrobial allergy, pre-existing medical conditions, length of hospital stay (LOS), status at discharge, consultant specialty, the reason for ID consultation, dates of ID consultation and signing off, infectious disease diagnosis, antimicrobial use, and post–sign-off events during the treatment of an established infection (ie, treatment failure, antimicrobial-associated ADEs, HAIs, withdrawal of care, ID re-consultation) were collected. HAI was defined as any infection associated with the index hospitalization and appearing 48 hours or more after admission. Reference Farinas, Saravia and Calvo-Montes10 Nonadherence to ID recommendations and reasons for nonadherence were also collected in a review of each patient’s EMR. Adherence to ID recommendations was defined as following the ID consultant’s final recommendation, including the antimicrobial regimen, dosing, and treatment duration. Patients receiving ID reconsultation during the treatment of an established infection after signing off and who were following the consultant’s final recommendations were included in the adherence group.
Statistical analysis
Categorical variables were expressed as a number and percentage, and continuous variables were expressed as the median with the interquartile range (IQR). In univariate analysis, categorical variables were compared using the χ2 test or the Fisher exact test as appropriate, and continuous variables were compared using the Mann-Whitney U test.
Multivariate logistic regression was performed to predict the factors associated with nonadherence to ID recommendations. Variables of interest and factors related to nonadherence to ID recommendations in a previous study, including primary service, Reference Lo, Rezai and Evans9 were forced into the final model. Additionally, for factors of interest or factors with P < .10 on univariate analysis with clinical plausibility, multicollinearity was assessed by examining variance inflation factors and 2×2 tables to ensure the independence of the explanatory variables. The Hosmer-Lemeshow test was used to assess the goodness-of-fit of the logistic regression model. All tests for significance were 2-tailed, and P < .05 indicated statistical significance. We calculated 95% confidential intervals (CIs). All analyses were performed using Stata version 16 software (StataCorp, College Station, TX).
Results
During the study period, among 740 patients who received ID consultation, 367 met the inclusion criteria and their cases were analyzed (Fig. 1). Supplementary Table 1 shows the clinical characteristics; their median age was 70 years (interquartile range [IQR], 56–80), and 197 (53.7%) were male. The department of critical care medicine provided 49 (13.4%) of the 367 consultations, followed by the general surgery department, which provided 48 consultations (13.1%), and the orthopedic department, which provided 47 consultations (12.8%). Management of confirmed or established infectious diseases was the most common reason for requesting ID consultation (n = 214, 58.3%). Table 1 shows the post–sign-off events and outcomes in patients with ID consultation. Post–sign-off events occurred in 59 (16.1%) of 367 patients; antimicrobial-associated ADEs accounted for 26 (44.1%) of these 59 cases and HAIs accounted for 13 (22.0%) of these cases. Care, including antimicrobial therapy, was discontinued in 16 (27.1%) of these 59 patients. ID reconsultation during the post–sign-off period was requested in 44 (12.0%) of all 367 patients with a post–sign-off event, and ID reconsultation was provided to 36 (61.0%) of the 59 patients with a post–sign-off event. The in-hospital mortality rate in the study cohort was 8.2% (30 of 367).

Fig. 1. Patient selection. Note. ID, infectious diseases.
Table 1. Post–Sign-Off Events and Outcomes

Note. HAI, healthcare-associated infection; ID, infectious disease; IQR, interquartile range.
a Units unless otherwise specified.
Table 2 shows the details of nonadherence to subsequent ID recommendations. Nonadherence to ID recommendations was identified in 55 (15.7%) of 351 patients. Also, 25 (45.5%) of these 55 patients discontinued antimicrobial therapy before the recommended date; the most common reason was patient transfer or discharge (n = 10, 18.2%). Meanwhile, 30 patients (54.5%) continued their antimicrobial therapy.
Table 2. Details of Nonadherence to Subsequent ID Recommendation

Note: ID, infectious disease; HAI, healthcare-associated infection.
a Patients with withdrawal of care were excluded (n=16).
b Units unless otherwise specified.
In multivariate analysis, 5 variables of interest were included in the final model based on the total number of cases of nonadherence to ID recommendations (following the rule-of-thumb of 1 covariate per 10 events): age, antimicrobial-associated adverse drug event, treatment failure of an established infection, new HAIs, and variables associated with nonadherence to ID recommendation in a previous study (ie, primary service). The Hosmer-Lemeshow test was used for goodness of fit for logistic regression with P = .351. Development of a new HAI after sign off was independently associated with nonadherence to ID recommendations (adjusted odds ratio, 3.78; 95% CI, 1.14–12.52) (Table 3). Table 4 shows the differences in outcomes between the nonadherence and the adherence groups. Length of hospital stay was longer in patients who did not adhere to the ID recommendations (35 vs 30 days; P = .019).

Note. ID, infectious disease: OR, odds ratio; CI, confidence interval; IQR, interquartile range; HIV, human immunodeficiency virus; SSTI, skin and soft-tissue infection; NSTI, necrotizing soft-tissue infection; SSI, surgical-site infection; HAI, healthcare-associated infection; N/A, not available.
a Based on the total number of cases with nonadherence to ID recommendation following the rule-of-thumb of 1 covariate per 10 events, the final model included 5 variables: the variable of interest (antimicrobial-associated adverse drug events), the variable associated with nonadherence to ID recommendation in a previous study (primary service), and variables with a P value < 0.1 on bivariable analysis with clinical plausibility (age, treatment failure of established infection, and new HAIs). The Hosmer-Lemeshow test was used for goodness of fit for logistic regression, with a P value of 0.351.
b Patients with withdrawal of care were excluded (n = 16).
c Units unless otherwise specified.
d Endovascular infection included endocarditis, catheter-related bloodstream infection, cardiac implantable electronic device infection, mycotic aneurysm, prosthetic vascular graft infection, and septic thrombophlebitis.
e Included central nervous system infection; sexually transmitted disease; Clostridioides difficile infection; ear, nose and throat infection; cyst infection; pyometra; mediastinitis; phlebitis, dog bite; pelvic inflammatory disease; tetanus; endometritis; endophthalmitis; and salpingitis.
Table 4. Outcome of Included Patients Stratified by Adherence to Subsequent ID Recommendation (n = 35 a )

Note. ID, infectious disease; IQR, interquartile range.
a Patients with withdrawal of care were excluded (n = 16).
b Units unless otherwise specified.
Discussion
We examined the clinical course of patients receiving ID consultation during the post–sign-off period and the epidemiology of nonadherence to ID recommendations during the same period. Post–sign-off events related to antimicrobial therapy were frequently observed, and the development of new HAIs during this period was independently associated with nonadherence to ID recommendations. Moreover, nonadherence occurred in nearly one-sixth of the patients and indicated a need for additional approaches by treating physicians to ensure continued patient safety and care.
Various adverse events (AEs) occur during hospitalization. Previous studies have shown their incidence to be ∼10%. Reference Rafter, Hickey and Condell11–Reference Schwendimann, Blatter, Dhaini, Simon and Ausserhofer13 In line with these studies, we also found post–sign-off events related to antimicrobial therapy in 16% of the cohort, with AEs, namely HAIs and antimicrobial-associated ADEs, accounting for 10% of the cases. These findings demonstrate that patient safety declined during the post–sign-off period. Interestingly, a 22 (84.6%) of 26 patients received a reconsultation for issues related to an established infection (eg, antimicrobial-associated ADE (or treatment failure; 4 of 4, 100%); however, only 9 (69.2%) of 13 patients received reconsultation for a newly acquired HAI. Notably, the development of a new HAI after sign off led to nonadherence to ID recommendations. Presumably, the treating physicians were reluctant to request further consultation or were confident of treating the cases without consultation. Because HAIs are more likely to involve AMR and are potentially preventable, Reference Cassini, Hogberg and Plachouras14,Reference Bearman, Doll, Cooper and Stevens15 proactive ID consultation to avoid post–sign-off events is strongly recommended. For example, a weekly audit of patients during the sign-off period and the proactive offer of further consultation by the ID physician may enable early intervention to minimize potential harms to the patient. Also, the establishment of a multidisciplinary approach involving nurses and antimicrobial stewardship pharmacists may help facilitate ID reconsultation to deal with post–sign-off events.
Adherence to ID recommendations was independently associated with favorable patient outcomes. Reference Farinas, Saravia and Calvo-Montes10,Reference Sellier, Pavese, Gennai, Stahl, Labarere and Francois16 According to previous studies, the nonadherence rate was 18%–40% and varied by the type of recommendation Reference Lo, Rezai and Evans9,Reference Farinas, Saravia and Calvo-Montes10,Reference Sellier, Pavese, Gennai, Stahl, Labarere and Francois16,Reference Vehreschild, Morgen and Cornely17 ; recommendations for antimicrobial treatment (nonadherence rate, 8%–17%) were more acceptable than those for diagnostic or monitoring tests (nonadherence rate, 13%–35%). Reference Lo, Rezai and Evans9,Reference Sellier, Pavese, Gennai, Stahl, Labarere and Francois16–Reference de La Blanchardiere, Boutemy, Thibon, Michon, Verdon and Cattoir18 Because we focused on therapeutic management, the nonadherence rate was well within the reported range at 15.7%, consistent with the findings of previous studies. Reference Lo, Rezai and Evans9,Reference Sellier, Pavese, Gennai, Stahl, Labarere and Francois16–Reference de La Blanchardiere, Boutemy, Thibon, Michon, Verdon and Cattoir18 However, for 31% of patients who did not adhere to the recommendations, the attending physician prematurely discontinued antimicrobial therapy because of the patient discharge, transfer, or clinical improvement (Table 2). Although data on outcomes following hospital discharge were not collected, treatment failure caused by inadequate antimicrobial use did occur. Reference Zilberberg, Nathanson, Sulham, Fan and Shorr19 In contrast, 15% of patients who did not adhere to ID recommendations received prolonged antimicrobial therapy beyond the recommended duration because of abnormal laboratory findings or clinical deterioration. Simply prolonging antimicrobial therapy without assessing such developments is unlikely to lead to favorable patient outcomes. Moreover, unnecessary antimicrobial use may promote antimicrobial-associated AEs and AMR. Reference Tamma, Avdic, Li, Dzintars and Cosgrove3,Reference Davey and Marwick5 Prolonging antimicrobial therapy also suggests the treating physicians’ lack of knowledge or awareness about AMR; fear of more serious, infectious disease-related complications; or fear of overlooking an infection. Reference Teixeira Rodrigues, Roque, Falcao, Figueiras and Herdeiro1,Reference Christensen, Haug, Berild, Bjornholt, Skodvin and Jelsness-Jorgensen20 Indeed, changing physicians’ antimicrobial prescribing behaviors is challenging. However, confirmation of the correctness of consultation-based changes to antimicrobial therapy by the ID physician and the deployment of a multidisciplinary approach, as mentioned above, may strengthen the treating physicians’ confidence in the correctness of their actions and raise their awareness of the importance of appropriate therapy and adherence to ID recommendations. Furthermore, ID physicians should understand that nonadherence to their recommendations will sometimes occur during the post–sign-off period, and they must constantly strive to improve adherence.
In the present study, length of hospital stay (LOS) was longer in the nonadherence group than in the adherence group owing either to the confounding of longer LOS and ID consultation by the development of post–sign-off events or to nonadherence to ID consultation resulting in increased LOS. Notably, the development of new HAIs more frequently occurred in the nonadherence group after the sign off. Obviously, in-hospital AEs led to prolonged LOS. Reference Rafter, Hickey and Condell11,Reference Hoogervorst-Schilp, Langelaan, Spreeuwenberg, de Bruijne and Wagner12 Moreover, nonadherence itself might induce excessive antimicrobial use leading to unnecessary hospitalization. In fact, more than half of patients not adhering to ID recommendations received antimicrobials for a prolonged period in our study. Although the current study showed no difference in the mortality rate between the groups, nonadherence to ID recommendations should be minimized because prolonged hospitalization (including hospitalization due to nonadherence) is a potential cause of additional AEs and poorer health-related quality of life involving extra healthcare costs. Reference Rojas-Garcia, Turner, Pizzo, Hudson, Thomas and Raine21 Thus, ensuring adherence to ID recommendations is warranted for patient welfare.
This study had several limitations. First, because our study was monocentric and retrospective, its findings may have limited generalizability, and the data collected may be limited in scope despite the use of standardized definitions and data collection forms. Second, the reasons for nonadherence to ID recommendations were not documented in EMR for approximately one-third of the nonadherence group in whom potentially modifiable, prescriber-related factors may have been overlooked. Last, even after adjusting for known predisposing factors, other unmeasured factors may have contributed to nonadherence to ID recommendations.
In conclusion, despite the treatment recommendations made by ID physicians, antimicrobial therapy was sometimes modified by treating physicians following sign-out by the ID physicians. In the hospital, antimicrobial treatment-related adverse events commonly occur during the sign-off period, leading to nonadherence to treatment recommendations made by ID physicians. Because nonadherence during this period can have a detrimental effect on patient safety and outcomes, ID physicians should make clear to the attending physicians that consultation will still be available even after signing off.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/ash.2023.121
Acknowledgments
We are indebted to Mr. James R. Valera for his assistance editing the manuscript.
Financial support
This work was funded by the Japan Society for the Promotion of Science (JSPS grant no. 19K10501).
Conflicts of interest
All the authors declare no conflicts of interest related to this article.