The main risk factor for catheter-associated urinary tract infections (CAUTIs) appears to be prolonged catheterization.Reference Meddings, Rogers, Macy and Saint1 Previous research has shown promising results using reminder interventions to reduce urinary catheter use.Reference Meddings, Rogers, Macy and Saint1, Reference Meddings, Rogers, Krein, Fakih, Olmsted and Saint2 However, we have been unable to identify any studies evaluating electronic reminders at the point of care for urinary catheters or studies that have included randomization in their design. A reminder intervention is a mechanism that prompts the nurse or physician to review the ongoing need for catheterization. Catheter reminder interventions evaluated in previous research included verbal or written reminders, a sticker on the catheter bag or patient’s chart, computer-generated reminders, or stop orders.Reference Meddings, Rogers, Macy and Saint1, Reference Meddings, Rogers, Krein, Fakih, Olmsted and Saint2 The 2 main objectives of the our study were (1) to examine the efficacy of an electronic reminder system, the CATH TAG, in reducing the duration of catheterization in hospitalized patients and (2) to explore the effects of the CATH TAG on nurses’ ability to deliver patient care.
Methods
Study design and setting
A stepped-wedge, randomized, controlled design was performed in 10 wards of a large, principal referral, Australian hospital over a 24-week period (Supplementary Fig. S1 online). The wards included medical and surgical wards, in addition to the intensive care unit (ICU). The study commenced in November 2017 and concluded in May 2018. A cross-sectional anonymous online survey was conducted at the end of the study period, in addition to a focus-group interview. The study was registered with the Australian and New Zealand Clinical Trial Registry (no. ACTRN12617001191381), and a study protocol has been published.Reference Fasugba, Cheng, Russo, Northcote, Rosebrock and Mitchell3
Participants and eligibility
All hospitalized patients in eligible wards of the hospital who had an indwelling urinary catheter as part of their usual clinical care were included in the study. Patients <2 years old were excluded. The participants in the online survey and focus group were nursing staff; this group was chosen because they were directly involved in the intervention and urinary catheter care.
Ethics
Ethics approval was obtained from the human research ethics committees of Avondale College of Higher Education (2017: 15) and Townville Hospital and Health Service (no. HREC17QTHS19). A waiver of individual patient consent was obtained for this study.
Randomization and blinding
Using computer-generated randomization, eligible wards in the hospital were randomly assigned to cross over to the intervention every 4 weeks over the trial duration. Randomization was performed by a person not involved in the study. The allocation was performed immediately prior to the commencement of the study. Wards were not blinded because it was not feasible to blind the staff to the intervention.
Intervention
The intervention was the use of the CATH TAG. The CATH TAG is an electronic device in the form of a sticker that attaches to the catheter bag with adhesive (Supplementary Fig. S2 online). It is lightweight and has a nonintrusive green light that flashes intermittently for a period of 24 hours upon activation. After 24 hours, the green flashing light changes to red, flashing with increased rapidity and visibility. The red flashing light is an indication that the nurse should reassess the need for a urinary catheter and should remove it if it is no longer required. There is no option for nurses to manipulate the flashing light or amend the flashing cycle.
A variety of methods were used to raise awareness about the how to use the CATH TAG, including wall posters, flyers, information leaflets, and engagement with the nursing managers at the ward level. These focused on the use of the CATH TAG and study, not catheterization practices or duration. Further details regarding the intervention, including fidelity, are detailed in supplementary material.
Outcomes
We considered two primary outcomes for the study: (1) urinary catheter duration and (2) the perceptions of nurses about the ease of use of the CATH TAG. In our initial protocol, the primary outcomes were the urinary catheter device utilization ratio and the perceptions of nurses. Prior to analysis, it became evident that the research team was not able to obtain patient-day data that aligned precisely with the date when a ward switched from the control to the intervention. Therefore, the team decided to amend the primary outcome to urinary catheter duration, which is consistent with the approach taken in other studies.Reference Meddings, Rogers, Krein, Fakih, Olmsted and Saint2 The change was approved by the clinical trial registry prior to analysis being undertaken.
Secondary outcomes included the number of cases of catheter-associated asymptomatic bacteriuria per 100 catheter days, perceptions of nurses about effectiveness of the CATH TAG, changes in ownership or interest by patients in catheter management, and barriers to the CATH TAG working successfully in various types of patients.
Perceptions of nurses
A phenomenological approach, seeking to understand the participants’ lived experience of a phenomenon, was the theoretical underpinning for the data collection and analysis methods used in association with the focus group. The purpose of the focus group was to gain an in-depth understanding of a sample of participants. Focus-group participants received a gift card to compensate them for their time because attendance occurred on their own time.
Statistical analysis
Catheter duration
The analysis employed an intention-to-treat strategy and involved the inclusion of all patients in the randomized clusters in the analysis, regardless of any deviations from the study protocol. We used a Cox proportional hazards model to assess the rate of removal of catheters, with the duration of catheterization censored at the time of patient transfer and the intervention considered as a time-varying covariate. That is, the effect of the intervention was assumed to relate to the ward on which the patient was cared for. In this model, the hazard ratio (HR) represents the hazard of catheter removal, such that HR >1 represents earlier removal. In a subanalysis, we repeated the Cox proportional hazards regression, excluding patients in the intensive care unit (ICU). There is a strong rationale for subanalysis based on differing results between ICU and non-ICU settings for CAUTI interventions.Reference Saint, Greene and Krein4 In a sensitivity analysis, we repeated the model, adjusting for sex, age and the presence of a primary infective diagnosis. We assessed the risk of bacteriuria using a conditional logistic regression, with intervention as the only independent variable, adjusted for clustering at the patient level.
Survey and focus group
Mean responses to Likert questions were calculated. An independent t test was used to compare means. For reliability testing, we calculated Cronbach’s α. The overall approach used to analyze the qualitative data from the focus groups can best be described as a ‘thematic coding approach.’Reference Robson and McCartan5 However, in this study, we also grouped data into a number of predetermined topics, established by the study’s research questions and objectives, before they were inductively coded using the thematic coding approach in NVivo software (QSR International, Melbourne, Australia).
Sample size and power estimation
Our sample size calculation was based on being able to detect a difference of 20% relative risk (10% absolute risk) reduction in catheterization, using a stepped-wedge design.Reference Fasugba, Cheng, Russo, Northcote, Rosebrock and Mitchell3
Results
Participants
Hospital participants
During the study period, 1,167 patients had a urinary catheter on the study wards and were included in our study (Table 1). The median age for the study group was 65 years (range, 16–103 years), and 45% of participants were female.
Table 1. Characteristics of Study Participants with an Indwelling Urinary Catheter

Nurse participants
In total, 82 nurses completed the online survey, representing an estimated 27% response rate. The completion rate was 100%; that is, all respondents who started the survey completed it fully. The median age for the study group was 33 years (range, 19–75), and 77 participants (93.9%) were female. In addition, 63 participants (76.8%) worked outside the ICU. Additional information regarding respondents is provided in the Supplementary Table S3 online. The focus group was composed of 5 nurses (age range, 28–74 years). All were female, and they worked in a variety of wards, including subacute, surgical, infection control, and oncology.
Catheter duration
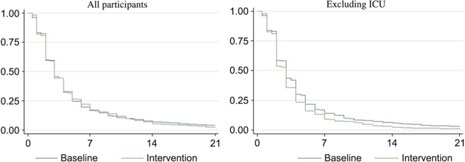
The duration of catheterization was slightly lower in patients for whom the CATH TAG was used (hazard ratio [HR], 1.02; 95% confidence interval [CI], 0.91–1.14; P = .75). The mean duration in the control and intervention phases was 5.51 days (95% CI, 4.9–6.2) and 5.08 days (95% CI, 4.6–5.6), respectively (Figure 1). Similar results were obtained after adjusting for sex, age, and infectious diagnoses (HR, 0.98; 95% CI, 0.87–1.10; P = .74). A nonsignificant reduction in catheter-associated asymptomatic bacteriuria was observed (odds ratio [OR], 0.90; 95% CI, 0.52–1.53; P = .69). For patients who were not transferred or transferred to a ward in the same phase of the study, there was no effect (HR, 1.09; 95% CI, 0.97–1.24; P = .15).
Excluding patients from the ICU, the duration of catheterization was significantly lower in patients for whom the CATH TAG was used (HR, 1.20; 95% CI, 1.06–1.37; P < .01). The mean duration of catheterization decreased by 23% from 5.00 days (95% CI, 4.44–5.56) to 3.84 days (95% CI, 3.47–4.21).
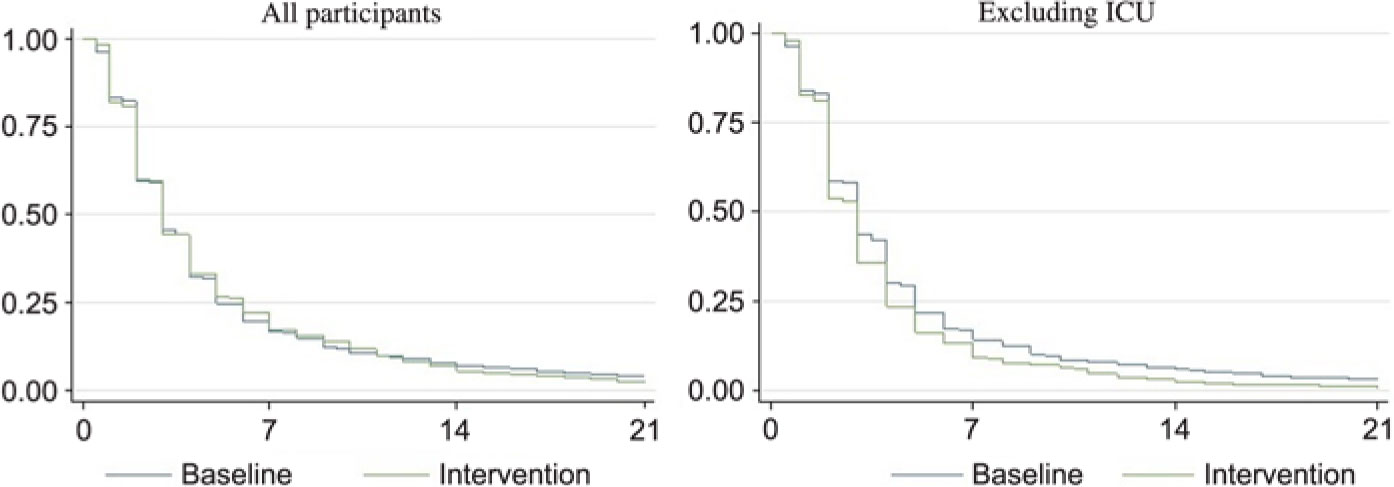
Fig. 1. Proportion of patients with a urinary catheter during the baseline (no CATH TAG) and intervention (CATH TAG) phases of the study. X axis: days since insertion; Y axis: proportion of patients with catheter. Legend: Blue line indicates the proportion of patients with a catheter during the control (baseline phase). Green line indicates the proportion of patients with a catheter during the control (baseline phase). All participants refers to the data from all wards participating in the study. Excluding ICU refers to all wards in the study, excluding the intensive care unit.
Perceptions of use
Online survey
There was a positive response to the CATH TAG, as demonstrated by participant answers to a range of questions (Table 2 and Supplementary Table S4 online). When comparing responses between ICU and non-ICU staff, non-ICU staff indicated a significantly higher level of agreement to several questions. For example, they indicated that the CATH TAG was helpful in daily routines (P = .003) and as a reminder to check the ongoing need for catheterization (P < .001). In the ICU, patients were less likely to ask about the CATH TAG (P < .001) or to notify nurses of a change in the CATH TAG light (P = .002). Non-ICU nurses were more satisfied (P < .001), were more likely to recommend the CATH TAG (P < .001), and had a more positive experience than ICU nurses (Table 3).
Table 2. Likert Scale Responses of Nurses to Survey Questions Regarding the CATH TAG
Note. SD, standard deviation; ICU, intensive care unit.
Table 3. Nurses Responses to Online Survey Regarding Their Experience with the CATH TAGa

Note. SE, standard error; ICU, intensive care unit.
a Respondents were asked to respond on a scale of 0–100.
Focus group
Three main themes emerged in the focus group: (1) issues related to the practical use of the CATH TAG during the project; (2) patient care and patient perceptions; and (3) future use of the CATH TAG (Table 4). Detailed results are provided in the supplementary material online.
Table 4. Experience with the CATH TAG: Summary of Findings From Focus-Group Participants
Discussion
We identified a reduction in urinary catheter duration after an intervention in which a novel electronic reminder system was attached to urinary catheter bags. A significant reduction in catheterization duration (23%) was identified outside the ICU. The use of the device was received positively by nursing staff and could be implemented easily into clinical practice. The study was enhanced by a mixed-methods approach, which helped us further understand the findings.
Interventions, such as a reminder system, to reduce the duration of catheterization have been shown to be effective in other studies.Reference Apisarnthanarak, Thongphubeth and Sirinvaravong6–Reference Crouzet, Bertrand, Venier, Badoz, Husson and Talon9 However, our study is distinct due to the use of randomization in the study design.Reference Apisarnthanarak, Thongphubeth and Sirinvaravong6–Reference Huang, Wann and Lin8 In our subanalysis exploring non-ICU patients, we identified a significant reduction in catheterization duration. This result is consistent with a French study that demonstrated an association between a reminder system and a reduction in catheter use in some, but not all, clinical wards within a hospital environment.Reference Crouzet, Bertrand, Venier, Badoz, Husson and Talon9 Similarly, a notable national prevention CAUTI program in the United States was also associated with a reduction in catheter use and CAUTI in non-ICUs.Reference Saint, Greene and Krein4
The mixed-methods approach we used provides further important contextual information that facilitates understanding of the results. There were notable differences between ICU and non-ICU staff regarding their experiences with the CATH TAG. Non-ICU staff appeared to have a positive experience and regarded it as more useful and effective than ICU staff. In the non-ICU setting, staff reported in both the survey and focus group that the CATH TAG was easy to use and to implement into clinical care.
We assessed our study for pragmatism, using the PRagmatic-Explanatory Continuum Indicator (PRECIS-2) tool.Reference Loudon, Treweek, Sullivan, Donnan, Thorpe and Zwarenstein10 This tool could be implemented into hospital care relatively easily, especially if it were incorporated into a urinary catheter bag. When we designed the study, we were interested to know whether the device would engage patients in catheter care, particularly when the device flashed red. There did not appear to be much patient involvement or ownership with the CATH TAG, perhaps because the device was largely unnoticed by participants. No negative comments were made by patients or reported to the researchers via the survey or focus group.
We did not identify a reduction in bacteriuria in our study. However, bacteriuria was a secondary outcome, and a larger sample size would be needed for a definitive conclusion. The need to preserve antibiotic effectiveness is an important healthcare issue.Reference Trautner, Grigoryan and Petersen11 Avoiding treatment of asymptomatic bacteriuria should reduce the risk of developing antibiotic resistance.Reference Gross and Patel12 Thus, strategies that reduce catheter use, and therefore bacteriuria, may be of value and could be included as part of a wider strategy to reduce CAUTIs and antimicrobial resistance.
The cluster randomized design has the advantage of addressing many potential confounders because wards (clusters) act as their own control. A Hawthorne effect may have occurred as a result of study awareness and impending rollout. To reduce this potential bias, educational events and training on the use of the CATH TAG were staggered, were focused on the use of the device only and were delivered to wards individually in the week prior to implementation of the intervention. Our study was limited to a single hospital.
We undertook a pragmatic clinical trial and identified the potential benefits of using an electronic reminder system at the point of care to reduce catheterization duration and hence CAUTI risk. Although our overall results were negative, we identified a potential reduction in catheterization duration in the non-ICU setting. These results, coupled with largely positive survey and focus group feedback from nursing staff, suggest that the CATH TAG may be a useful device to aid prompt removal of urinary catheters in the non-ICU hospital setting.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/ice.2019.31.
Author ORCIDs
Brett G. Mitchell, 0000-0003-4220-8291
Acknowledgments
The authors acknowledge the support of the participating hospital and specifically the infection prevention and control team. Senver, the company that owns CATH TAG and who was awarded the Accelerating Commercialisation grant played no role in the study design, conduct, collection, or analysis of data.
Financial support
This study was supported by an Accelerating Commercialisation grant from the Australian Commonwealth Government.
Conflicts of interest
All authors report no conflicts of interest relevant to this article.