Attention-deficit hyperactivity disorder (ADHD) has widespread impact for affected children and their families. Despite the availability of, and an unequivocal role for, evidence-based treatments there is low use of specialist services and underdiagnosis (Reference Meltzer, Gatward and GoodmanMeltzer et al, 2000; National Institute for Clinical Excellence, 2000). Children with pervasive hyperactivity are at high risk of ADHD, other disorders and impaired social adjustment (Reference Taylor, Chadwick and HeptinstallTaylor et al, 1996). As general practitioners (GPs) have frequent contact with children, primary care attendance is an opportunity for detecting those with, or at risk of, disorders (Office of Population Censuses and Surveys et al, 1995). Given that there is under-treatment, at what levels of service use do access barriers exist and what influences access? By applying Goldberg & Huxley's (Reference Goldberg and Huxley1980) ‘pathways to care’ model to children with pervasive hyperactivity, we provide a quantitative description of the filters in the help-seeking pathway through primary care and investigate the relative contributions of child, parent and GP factors in determining service use.
METHOD
Setting
The outer London borough of Croydon was selected for the following reasons: over 80% of referrals to Child and Adolescent Mental Health Services (CAMHS) are from GPs, which gives a simplified version of possible referral routes; CAMHS is the only service responsible for diagnosing ADHD; and the borough has a socio-economic profile close to the national average but with wide variations within (Reference JarmanJarman, 1984). The study was approved by the South London and Maudsley National Health Service (NHS) Trust Ethics Committee.
Participants
Participants were children aged between 5 and 11 years identified from two sources. First, a community sample screened for pervasive hyperactivity, i.e. a score of 6 or above on the five ADHD items of both the parental and teacher-completed Strengths and Difficulties Questionnaire (SDQ; Reference GoodmanGoodman, 1997). The SDQ is discriminating in screening for non-referred cases in the community. The sampling frame for this community survey was children registered with a random sample of Croydon GP practices. Second, we identified children with a clinical diagnosis of ADHD who were either registered with the participating practices (but had not responded to the community survey) or had been referred by any Croydon GP to CAMHS in the previous year. This referred sample is important as only a small proportion of those with disorders in the community are known to specialist services (Reference Garralda and BaileyGarralda & Bailey, 1988; Reference Meltzer, Gatward and GoodmanMeltzer et al, 2000) and few referred cases were expected to be found in the community survey. The random sampling and response rate of the practices invited to participate mean that these practices should be representative of all Croydon practices, i.e. the clinic-identified cases should be similar to the community survey-identified referred cases.
Community survey
A random number table created by an independent statistician was used to invite 12 general practices (derived from a list of Croydon practices) to participate in the study. Ten practices agreed. Because of time constraints, five practices (18 GPs) were chosen randomly to be involved in the community survey. Parents of all 5-11-year-old Croydon residents registered with these practices (n=3218) were sent a letter and information sheet inviting them to participate in the study, the SDQ and a consent form. They were also asked for permission to approach them again for an interview. Permission to send an SDQ to the child's teacher and teachers' details were requested. For non-responders, one reminder was sent. For children who scored 6 or above on the ADHD questions of the parent SDQ, the headteacher of the school was approached. Subsequently, an SDQ was sent to the teacher; two reminders were sent to non-responding teachers.
Service use
The previous year was used to assess health service use (Reference Goldberg and HuxleyGoldberg & Huxley, 1980; Reference Meltzer, Gatward and GoodmanMeltzer et al, 2000). These contacts with the GP could be for any reason as most 7-12-year-olds with psychiatric disorders are presented to primary care with somatic complaints (Reference Garralda and BaileyGarralda & Bailey, 1986). Based on the pathways to care model (Reference Goldberg and HuxleyGoldberg & Huxley, 1980) the pervasive high-scorers were classified into four groups defined by their health service use in the previous year: (a) GP non-attenders (group 1; children who had not seen a GP in the previous year); (b) GP attenders — unrecognised (group 2; children who had seen a GP for any reason but were not regarded as having a mental health disorder); (c) GP — recognised but not referred (group 3; children who had seen a GP for any reason and were regarded as having a mental health disorder but were not referred to CAMHS); (d) CAMHS attenders — including clinic-diagnosed children who were either registered with the participating practices or were referred by any Croydon GP in the previous year (group 4).
Hence the filters are: primary care attendance; recognition of a mental health disorder by the GP; and referral to CAMHS. Children in groups 1 and 4 were identified from GP practice and CAMHS records, respectively. Children in groups 2 and 3 were classified by a GP completing a form (attached to case notes) for consultations. The GP was asked: ‘Do you think this child has a mental health disorder?’ GPs were blind to the SDQ scores. If the GP did not complete the form, a conservative assumption was made that the child was in group 2.
Sample size
For clinical relevance and service development, sample size calculation was based on a large effect size (0.8; based on univariate analysis). Based on power of 0.8 and α of 0.05, 26 children were required for each comparison group. As a subsample of children was obtained from the clinic, it was estimated that 3300 children needed to be screened in the community survey to yield 95 children with pervasive hyperactivity. This was based on expected parent and teacher response rates of 60% (Reference Garralda and BaileyGarralda & Bailey, 1986), the parent SDQ cut-off to include 20% of the population (Reference GoodmanGoodman, 1997) and the teacher SDQ cut-off to include 40% of the parent screen positive sample.
Measures
Parents of eligible children were interviewed at home. For children identified from the community survey the interviewer was blind to the child's group. Measures included: (a) The hyperactivity section of the Parental Account of Children's Symptoms (PACS; Reference Taylor, Sandberg and ThorleyTaylor et al, 1991), which is a reliable and valid standardised semi-structured interview. (b) A semi-structured interview to collect information on whether the parent had previously identified the behaviour as a presenting complaint to the GP or requested referral. (c) The previously completed parent SDQ informed about comorbidity and burden for others (Reference GoodmanGoodman, 1999). In addition to the previously-completed teacher SDQ, the parent was also asked to complete the teacher SDQ in relation to hyperactivity behaviours at school. This was done because parent perception of school-related concerns can influence service use. (d) As a measure of deprivation, the postcode was linked with Jarman underprivileged area (UPA) scores for census enumeration districts (Reference JarmanJarman, 1984). In addition, GPs were asked to complete a questionnaire examining their attitudes towards child mental health disorders and services.
Analysis
Based on a priori hypotheses about explanatory child and parent factors (see Tables 1 & 2), those who had passed each filter were compared with those who had not. At each filter, statistically significant (P < 0.05) predictors on univariate analyses were entered into a logistic regression analysis to provide adjusted odds ratio (OR) estimates.
Table 1 Attendance filter

| Non-attenders | Attenders | Odds ratio (95% CI)1 | |
|---|---|---|---|
| Demographic measures | n=29 | n=81 | |
| Gender (male) | 22 (76%) | 65 (80%) | |
| Age | 8.77 (1.75) | 8.15 (1.80) | |
| Jarman UPA score | 2.16 (12.10) | 0.97 (13.75) | |
| Predictor measures (range) | |||
| Emotional (SDQ) (0-10) | 2.69 (2.19) | 3.60 (2.69) | 1.17 (0.98-1.41) |
| Conduct (SDQ) (0-10) | 3.21 (2.13) | 3.36 (2.22) | 1.02 (0.84-1.25) |
| Interview measures | n=23 | n=70 | |
| Hyperactivity (PACS) (0-3) | 0.96 (0.68) | 1.29 (0.64) | 2.15 (0.91-5.10) |
| Parent regards the behaviour as a problem (PACS) (0-2) | 0.91 (0.73) | 1.34 (0.74) | 2.11 (1.11-4.03) |
| Parent perception of school-rated burden (SDQ) (0-3) | 0.95 (0.90) | 1.19 (0.90) | 1.34 (0.76-2.36) |
Table 2 Recognition filter
| Unrecognised (group 2) | Recognised (groups 3 & 4) | Odds ratio (95% CI)1 | |
|---|---|---|---|
| Demographic measures | n=58 | n=40 | |
| Gender (male) | 46 (79%) | 33 (83%) | |
| Age | 8.26 (1.72) | 7.66 (1.74) | |
| Jarman UPA score | 0.96 (13.62) | 3.19 (13.16) | |
| Predictor measures (range) | |||
| Emotional (SDQ) (0-10) | 3.40 (2.57) | 3.8 (2.55) | 1.10 (0.93-1.30) |
| Conduct (SDQ) (0-10) | 2.79 (1.94) | 5.08 (2.28) | 1.68 (1.30-2.18) |
| Interview measures | n=50 | n=37 | |
| Hyperactivity (PACS) (0-3) | 1.18 (0.62) | 1.73 (0.67) | 3.51 (1.66-7.45) |
| Ineffectiveness of parental management strategies (PACS) (0-7) | 1.82 (0.66) | 2.24 (0.86) | 2.07 (1.09-3.93) |
| Parent identified behaviour as presenting complaint | 13 (26%) | 33 (89%) | 25.37 (7.34-87.74) |
| Parent requested referral | 3 (6%) | 25 (68%) | 38.91 (9.02-167.76) |
RESULTS
Figure 1 shows participant recruitment. Selection bias in parental response is unlikely as 21% of responders were high-scorers (the SDQ cut-off score identifies 20% of the population; Reference GoodmanGoodman, 1997). Further evidence that selection bias is unlikely is that the proportions of those scoring above cut-off for emotional and conduct symptoms were 22% and 23%, respectively (expected 20%). As response status was associated with child age and Jarman UPA scores, these were included as covariates in the logistic regression models. A total of 127 eligible children were identified. In terms of information available for analyses, parent and teacher SDQs were available for all 127 children and interview information for 110 children. There were no differences between those interviewed and not interviewed in terms of the child's GP attendance or recognition status, gender, age, SDQ hyperactivity scores and household Jarman UPA score.
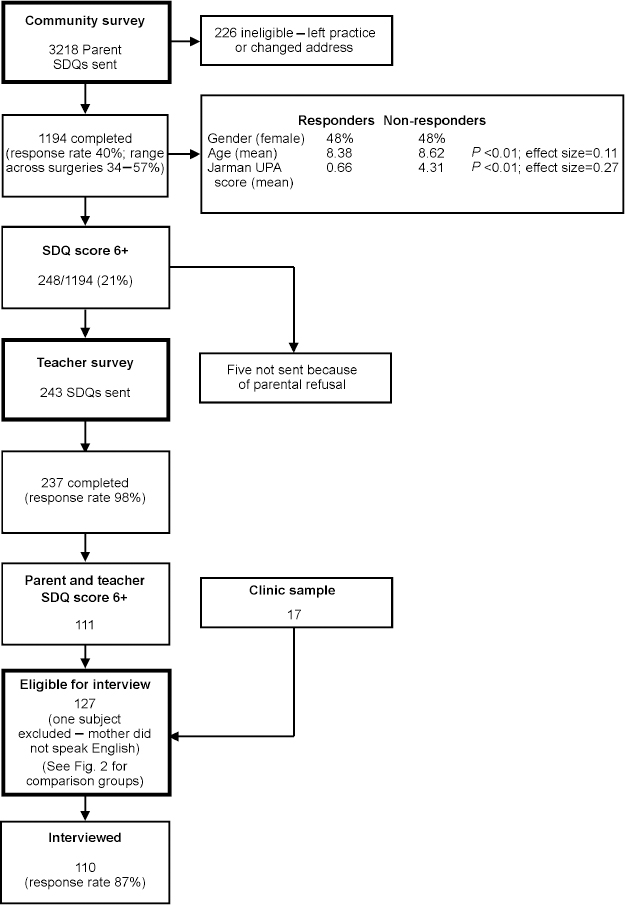
Fig. 1 Flow chart illustrating participant recruitment.
Figure 2 shows the comparison groups for analysis. Of the 110 children identified from the community survey, 10 (9%) were recognised but unreferred primary care attenders and 13 (12%) were CAMHS attenders. However, 8 of these 10 recognised children had been referred to CAMHS before the interview took place. Hence, for analysis, the recognised (group 3) and referred (group 4) groups were combined to form a single recognised group.
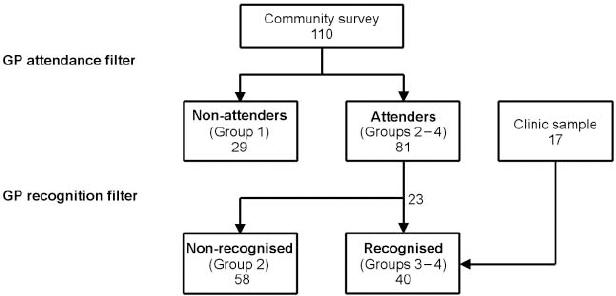
Fig. 2 Comparison groups.
Attendance filter
Most (74%) children with pervasive hyperactivity identified from the community survey had seen their GP in the previous year. Table 1 shows that the only significant predictor of primary care attendance was parental perception of the behaviour as problematic (P < 0.05). Child factors (severity of hyperactivity or comorbidity) did not predict attendance.
Recognition filter
GPs recognised the presence of a mental health disorder in 23 of the 81 (28%) primary care attenders. Table 2 shows that GP recognition was associated with all the a priori hypotheses except emotional symptoms comorbidity. After controlling for all these statistically significant predictor variables, the logistic regression found only two factors that predicted recognition: parental request for referral (OR 20.83, 95% CI 3.05-142.08; P < 0.01); and conduct problems comorbidity (OR 1.48, 95% CI 1.04-2.12; P < 0.05).
GP questionnaire
A total of 16 (89%) questionnaires were completed. All 16 GPs agreed with the statement: ‘If a parent requests referral to specialist services for one of these disorders I tend to refer.’ In comparing their views about the management of ADHD and emotional disorders, GPs were less likely to agree that children with ADHD can be managed solely in primary care (on a Likert scale ranging from 0 (strongly agree) to 4 (strongly disagree); means 3.13 v. 3.44; paired sample t-test, t=2.6, d.f. 15, P < 0.05).
DISCUSSION
Specific factors distinguish between different levels of service use in relation to pervasive hyperactivity. The decision to attend primary care was associated with parent, but not child, factors. In contrast, recognition of disorder in primary care was related to both child and parent factors. Child factors can be more important in physician identification than in the parental decision about which children to bring to primary care. The barriers to service use were at all levels except the referral filter. Non-recognition of disorder by the GP was the main barrier to accessing specialist services. This recognition filter is particularly important in understanding the pathway to care as following recognition, most children with pervasive hyperactivity were referred to CAMHS. This contrasts with adult mental health disorders where the referral filter was found to be relatively impermeable (Reference Goldberg and HuxleyGoldberg & Huxley, 1992).
Parental perception of problems is known to be associated with service use (Reference Woodward, Boyle and OffordWoodward et al, 1988; Reference Verhulst and van der EndeVerhulst & van der Ende, 1997). We found that parental perception of hyperactivity symptoms as a problem predicted primary care attendance for any reason. The presenting complaint is likely to be physical rather than about the behaviour (Reference Garralda and BaileyGarralda & Bailey, 1986). It could be that parental concern about being blamed for the child's problems contributes to a reluctance to identify the behaviour as a presenting complaint. Despite increased awareness about ADHD, the diagnosis remains controversial and GPs and parents often have contrasting views (Reference Klasen and GoodmanKlasen & Goodman, 2000).
Previous research has also found that clinical severity (Reference Woodward, Dowdney and TaylorWoodward et al, 1997; Reference Garralda and BaileyGarralda & Bailey, 1988) and parental request for referral (Reference Bailey and GarraldaBailey & Garralda, 1989) are associated with referral status. Our findings suggest that these factors operate by facilitating recognition of disorder by the GP. As recognition was associated with comorbidity GPs seem to be correctly identifying those that are most likely to have a disorder. However, parental request for referral was the strongest determinant of recognition making parents the main gatekeepers for access to specialist services but also indicating that GPs are responsive to parental concern. GPs acknowledged that, for child mental health disorders, they support parental referral requests. GPs are also more likely to refer children with ADHD to CAMHS than children with emotional disorders. Compared to previous findings, we found twice as many parents of the recognised group regarded themselves as requesting referral (Reference Bailey and GarraldaBailey & Garralda, 1989). Over the past decade, therefore, parents could be playing an increasingly active role in consultations and have greater confidence in asking for a referral to specialist services. Of course, our findings are restricted to hyperactivity, about which parents might be particularly knowledgeable and more likely to request referral than for other disorders.
Methodological issues
We found that it is feasible to use the ‘pathways to care’ model for studying access to children's services. The study is original in that it uses a large-scale community screen and applies this model to conceptualise the selection processes involved in the help-seeking, recognition and referral of children at risk of a disorder. The use of multiple ascertainment methods to identify referred children was justified as very few (13 out of 1194) of the community survey-identified sample were referred.
In terms of response status in the community survey, the small effect sizes of the differences in age and Jarman scores suggest the possibility of selection bias. However, the Jarman score is a proxy measure and cannot necessarily be attributed to individual households. Moreover, the distributions of SDQ sub-scale scores and gender of respondents were as expected. Overall, 9% of respondents had pervasive hyperactivity, which is similar to the expected proportion (Reference Taylor, Sandberg and ThorleyTaylor et al, 1991; Reference SandbergSandberg, 1996). The response rate was also similar to the single reminder rate in a recent national primary care survey (NHS Executive, 1999). The request to contact schools could have affected the response rate; one-fifth of responders were expected to refuse permission (Reference Zahner, Pawelkiewicz and DeFrancescoZahner et al, 1992). It is also likely that the proportion of incorrect addresses or children no longer registered with practices was underestimated; rates of up to 46% have been found in GP samples (Reference Pope and CroftPope & Croft, 1996; Reference Shaw, Creed and TomensonShaw et al, 1999).
The sample size precluded examination of interactions between the potential explanatory variables. As the investigation focused on pervasive hyperactivity in 5-11-year-olds, the findings might not generalise to other age groups or disorders. However, the study's setting and the use of a random sample of GP practices give the findings national relevance. Objective health service use information was obtained from clinical records, which minimises recall bias. Although our findings about parental referral request are subject to recall bias, these perceptions were confirmed by the GP's report. Parental perceptions of previous consultations are important as they influence future service use. It is unlikely that recognition status was misclassified where GPs had not completed the recognition forms as most recognised children were also referred, and so would have been identified from clinic records.
The final methodological issue relates to three possible concerns about the inclusion of the clinic-identified sample in the assessment of the recognition filter: there is a possibility of selection bias if the practices referring the 17 clinic-identified cases were different from the five practices studied; they are all diagnosed with ADHD whereas the rest of the sample is at high risk by virtue of high SDQ scores; and there is a potential tautology of analysing the issue of parent requesting referral because these cases have already been referred. These concerns are addressed in turn. The use of random sampling to recruit practices and the high response rate of participation in invited practices mean that the clinic-identified cases should be representative of the community survey-identified cases. Eight of the clinic-identified cases were children registered with participating practices whose parents did not respond to the community survey. Thirteen of the community survey-identified sample were also under the care of CAMHS. Although the clinic-identified cases were selected because they had a clinical diagnosis of ADHD, severity of hyperactivity symptoms did not distinguish recognition status when other factors were controlled for. Finally, the ‘parent requesting referral’ variable examines whether a parent has, in the past, requested referral and whether this alters the outcome (i.e. recognition). By comparing a referred and unreferred group, possible alternative explanations could be that parents of unreferred children did request referral and this was turned down by the GP, or that referrals occurred at the GP's (not the parents') suggestion.
Implications
How does this description of the selection processes that operate in practice match with desirable criteria for referral? Not all of the at-risk children studied have ADHD or require referral to CAMHS. As GPs were asked to recognise the presence of disorder rather than ‘high-risk’ children, GP non-recognition might not be problematic — GPs could be correctly identifying those children that do not have a disorder. They would not be expected to refer children who are simply high risk but do not meet criteria for disorder. However, it is concerning that GPs might not recognise children who have ADHD if the parent is unaware or reticent about the possibility of requesting referral.
As most of these high-risk children attend primary care there is an opportunity for early identification of those with a disorder. It is known that nearly a quarter of 7-12-year-olds attending primary care have psychiatric disorders (Reference Garralda and BaileyGarralda & Bailey, 1986) and that GPs are the main referrers to CAMHS (Audit Commission, 1999). Appropriate GP recognition of the disorder and referral to CAMHS are important elements of the pathway to care. Effective treatment is available for ADHD; the subsequent reduction in long-term morbidity and prevention of the development of complications could be cost-effective. Given recent guidance emphasising the importance of severity of hyperactivity in determining need for treatment (National Institute for Clinical Excellence, 2000), we should develop means of ensuring that the severity of hyperactive behaviour plays a stronger role in decisions about referral and treatment. For example, screening measures in primary care could be developed to identify those who would benefit from referral.
A National Service Framework for Children is being created to tackle inequalities and access problems (Department of Health, 2001). Hence epidemiological studies that investigate the barriers to accessing services are of clinical and political importance (Reference Costello, Burns and AngoldCostello et al, 1993). This study's identification of barriers to help-seeking suggests pathway changes that could reduce inequities in access to services. Parental request for referral and thus parental recognition of hyperactive behaviour as problematic play a crucial part in accessing specialist services. We also found that a quarter of our sample had not attempted primary care in the previous year and could be a hard-to-reach group. Alternative means of accessing specialist services need to be developed for these children. There is an argument for developing health education services to help parents recognise the disorder and for facilitating direct referrals to CAMHS by parents or teachers — in effect allowing them to bypass GPs. However, improving access highlights the need for adequately resourced CAMHS. Only 12% of our community-identified sample were in contact with CAMHS; a potential increase in referrals could overwhelm hard-pressed services. Nationally, only 30% of those with the more severe hyperkinetic disorder are being treated (National Institute for Clinical Excellence, 2000).
Following on from this investigation of child and parent factors, work is required on two levels to improve our understanding about factors that influence access to care. First, at the individual level, predictors of parental recognition of problems should be investigated. This could involve a two-stage process, e.g. school concerns can initiate parental worries or help-seeking behaviour. Second, a hierarchical model only involving primary care is likely to be an oversimplification of the real world. The multiple and parallel referral tracks to CAMHS that currently exist (e.g. from paediatricians, social services, education and self-referrals) need to be quantified and evaluated.
CLINICAL IMPLICATIONS
-
• As most children at risk of attention-deficit hyperactivity disorder (ADHD) do attend primary care, this suggests that recognition of the disorder by general practitioners (GPs) is feasible.
-
• In contrast to adult mental health disorders, following GP recognition of the disorder, most children with pervasive hyperactivity are referred to Child and Adolescent Mental Health Services (CAMHS).
-
• For children at risk of ADHD, parents are the main gatekeepers for access to specialist services, the GP's role appears to be responsive.
LIMITATIONS
-
• Low response rate to, and possibility of selection bias in, the community survey.
-
• Findings relate to pervasive hyperactivity in 5-11-year-olds and may not generalise to other disorders or age groups.
-
• A hierarchical model through primary care might be an oversimplification of the multiple and parallel referral tracks to CAMHS.
Acknowledgements
We thank all the participating families and schools, the GPs and the staff at the participating practices and Croydon CAMHS and Emma Cainey and Sheila Figueirado for help with data collection.







eLetters
No eLetters have been published for this article.