There are significant challenges to communication for families of paediatric patients hospitalised in intensive care units (ICU) surrounding goals of care. Communicating care plans must take into consideration variations in communication styles amidst a rotating set of inpatient providers’ and families’ preferences in receiving medical information. Reference Hallman and Bellury1,Reference Greenway, Rosenthal, Murtha, Kandil, Talento and Couloures2 Further, in this high-stress environment, complicated pathophysiology and uncertain outcomes can raise barriers to effective communication with parents. Reference Hallman and Bellury1–Reference Miller, Blume, Samsel, Elia, Brown and Morell4
The importance of documenting patient preferences has been reported on in paediatric palliative care and chronic disease literature. Reference Watson, Weaver, Jacobs and Lyon5–Reference White and Cooley8 However, the impact of formally assessing communication preferences to improve families’ hospital experience is unknown. Documenting communication preferences for the healthcare team may promote standardisation and consistency in communication styles in a variety of clinical settings including treatment plans, unanticipated complications, and prognostication. Attempts to ensure all families have an opportunity to consider and define their communication preferences may be useful, especially if providers have variable levels of skill and experience in this domain and rotate week to week. Further, the utilisation of a multi-language communication assessment tool in the ICU may improve communication between the medical team and families who speak languages other than English.
For parents of patients in the ICU requiring cardiac intensive care, we sought to describe respondents’ communication preferences using a Parental Communication Assessment (PCA) tool. We hypothesised that improved awareness of families’ communication preferences would improve communication between a patient’s family and the medical team and improve a family’s preparedness for their child’s clinical course during the hospitalisation, as measured through parents’ self-report.
Materials and methods
Study design and sample
This was a prospective, randomised unblinded study performed in the cardiac ICU (CVICU) of a tertiary free-standing children’s hospital in a university setting. Our institution’s 28-bed cardiac ICU cares for patients with surgical and medical congenital heart disease. Eligible participants included English- and Spanish-speaking parents of hospitalised patients < 18 years of age who were hospitalised in the ICU for three or more days. The survey was distributed to parents only.
We developed a novel tool, the PCA (Supplementary Table S1) with input from ICU and cardiology medical providers, palliative care, social work, and the Stanford Office of Patient and Family Education, which includes families of patients. The survey tool assesses
(1) communication preferences with parent and child regarding treatment goals and plans,
(2) communication preferences with parent and child regarding difficult decisions or setbacks,
(3) expectations and goals for the child’s hospitalisation,
(4) comfort with communicating with the medical team,
(5) how the CVICU can best support a family’s decision-making, and
(6) preferred language of communication.
A follow-up communication survey (Supplementary Table S2) was also developed to evaluate the parent’s satisfaction with communication in the ICU and was adapted from a previously standardised parent satisfaction survey, the pFS-ICU24. Reference Epstein, Unger and Ornelas9 This 24-question survey is a validated tool to evaluate family satisfaction with care in the paediatric intensive care setting. Reference Hummel, Presson, Millar, Larsen, Kadish and Olson10–Reference October, Hinds, Wang, Dizon, Cheng and Roter12 We took 18 of the 24 questions (the remaining 6 were not directly relevant to communication with parents) and added 3 additional questions related to suggestions for how to make care in the ICU better and general comments. The study information sheet, the PCA, and the follow-up survey were made available in English and Spanish. The consent of Spanish-speaking parents was obtained through an interpreter.
Participants were prospectively randomised to two groups: (1) the intervention group, which received the PCA, or (2) standard care. Results from the PCA were sent to the family’s social worker, who had an opportunity to communicate survey information to the medical team during weekly interdisciplinary rounds. Sending the results to the frontline provider was considered, but logistically challenging given the high provider turnover. All enrolled participants from both groups were given a follow-up survey after one week in the ICU or at the time of transfer out of the ICU, whichever came first. The follow-up survey evaluated the parent’s satisfaction with communication in the ICU, and demographic and disease characteristics were collected from the electronic medical records of participating paediatric patients. All data was collected and recorded in Research Electronic Data Capture, a secure web-based, Health Insurance Portability and Accountability Act-compliant software platform. Reference Harris, Taylor, Thielke, Payne, Gonzalez and Conde13,Reference Harris, Taylor and Minor14
The primary outcomes were (1) to assess the variation of communication preferences expressed by participants and to assess if (2) parent satisfaction regarding communication with their care team and (3) preparedness for difficult decisions or setbacks improved in the intervention group. Parent satisfaction with communication was assessed using two of the follow-up survey questions: “How well did CVICU staff provide you with explanations that you understood?” and “Did you feel included in the decision-making process?” Preparedness for hospitalisation was assessed using the question, “How prepared did you feel for difficult decisions or setbacks that arose during your child’s hospitalisation?” Exploratory sub-analyses were also performed to investigate differences between groups stratified by patient age, primary diagnosis, and length of hospitalisation.
Statistical analysis
Demographics and disease characteristics were recorded and compared to assess the sufficiency of randomisation. Differences between groups are reported with standard mean differences (SMDs), alongside the p-values from the χ2 tests. Standardised mean difference is a measure of effect size. The magnitude of effect is small if SMD = 0.2, medium if SMD = 0.5, and large if SMD = 0.8. Reference Cohen15 An intention-to-treat analysis was performed to compare the primary outcomes of the two randomised study groups using a Wilcoxon rank sum test with continuity correction. As a pilot study in the field, we considered our study as exploratory so that p < 0.05 was statistically significant for each of the primary outcomes. Sub-analysis was performed for the primary outcomes adjusted by age, primary diagnosis, and length of hospitalisation using ordinal logistic regression. Odds ratios, corresponding 95% confidence intervals, and p-values were reported from the models. All analyses were performed using R programming languages 16 (R version 4.2.2 (2022-10-31)).
Results
Respondent and patient characteristics
A total of 136 parents from February to December 2021 were eligible. Twenty-three declined, resulting in 113 participants (83% enrolment rate), of whom 56 (50%) were in the intervention group. Ten participants (9%) opted to receive study materials in Spanish (internal estimates are that 12–15% of our CVICU patient population is Spanish-speaking). Participant demographics are outlined in Table 1. There were no significant differences in patient characteristics between the intervention and control groups indicating adequate randomisation.
Table 1. Participant characteristics

Communication preferences
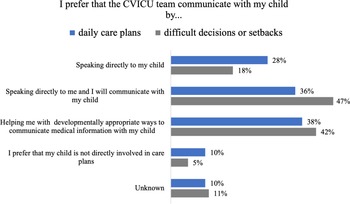
The communication preferences of the intervention group are represented in Supplementary Table S3. Most notably, most respondents reported that they prefer more detail-oriented communication in contrast to big-picture communication, and daily rounds were generally more preferred than weekly care conferences. When it came to the CVICU team communicating with their children, 29% of respondents preferred that the CVICU team communicate directly with their child about daily care plans, but only 18% wanted the team to directly communicate with the child regarding difficult decisions or setbacks. Most respondents understood the discussion on daily rounds and were comfortable discussing their child’s care with the medical team (64% and 68%, respectively). When asked how the medical team can best support the parent to make decisions about their child’s care, the majority (68%) selected “I prefer the medical team tell me the available options and their recommendation for what is best for my child.” Nearly 80% expected for their child to return home in the same or improved condition. Lastly, 86% reported that the survey was worthwhile for them to complete.
Communication satisfaction
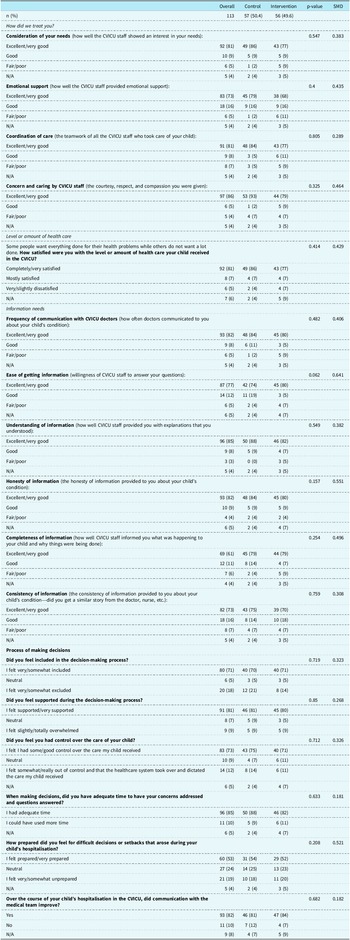
Parental satisfaction with communication with CVICU providers was overall high; greater than 70% of respondents reported “excellent” or “good,” and less than 5% reported “poor” for providers’ consideration of parents’ needs, emotional support, coordination of care, concern and caring, frequency of communication, ease of getting information, understandability of explanations, honesty, completeness, and consistency of information. Parents overall felt included and supported in the decision-making process (71% and 81%, respectively), they had control over their child’s care (74%), and they had adequate time to make well-informed decisions (85%). Eighty-two percent felt that communication with the medical team improved throughout the hospitalisation. Finally, while the majority (53%) felt prepared for difficult decisions or setbacks that arose throughout the hospitalisation, there was an important proportion that felt neutral (24%) or unprepared (19%). No significant differences were identified between the intervention group and control group for the primary outcomes. Ten participants (8.8%) participated using Spanish language materials. There were no significant differences between English- and Spanish-speaking participants regarding their communication preferences or their reported satisfaction with communication. As Spanish-speaking participants were only 9% of our cohort, we were inadequately powered to detect significant differences between language groups. Results of the follow-up survey can be seen in Table 2.
Table 2. Follow-up survey results

CVICU = cardiac ICU; SMD = standard mean difference.
Exploratory analysis
We performed additional exploratory analyses for questions that had a broader variation in responses to investigate possible differences between respondents who had a positive experience (e.g., “excellent” or “very good”) versus those who reported a less positive experience (e.g. “good,” “fair,” or “poor”). In other words, we evaluated for factors associated with positive versus negative responders, specifically looking at patient age, primary diagnosis, days in the hospital, and disposition. No factors that we evaluated trended towards or reached statistical significance.
Discussion
Like many medical settings, the ICU can represent a complex environment for families to navigate. Our anecdotal experience, supported in the literature, Reference Hallman and Bellury1,Reference Greenway, Rosenthal, Murtha, Kandil, Talento and Couloures2 is that many families have specific preferences about communication, especially related to critical decision-making, which the medical team often learns through personal experience. However, this takes time and can lead to miscommunications before such knowledge is gained.
Communication between the ICU team and parents of critically ill children is essential to ensure that families can make informed decisions and support their children. Barriers to communicating medical information in the inpatient setting are numerous and are exacerbated by complex physiology and critical illness. A review of the literature related to communication in paediatric ICUs by Hallman and Bellury cites poor communication as a factor leading to worse continuity of care, unnecessary care, and poor outcomes. Reference Hallman and Bellury1 This review references the paediatric Hospital Consumer Assessment of Healthcare Providers Systems survey and notes a study that found that communication can account for 25% of a hospital’s total score. Reference Hallman and Bellury1 In a study of parental perceptions of care in paediatric inpatient settings using another survey, the Picker Institute’s Pediatric Inpatient Survey, Co. et al. identified communication as the single most important factor to improve patient family satisfaction score. Reference Co, Ferris, Marino, Homer and Perrin17
Attempts to improve communication have thus evolved, and family-centred rounds have become the standard across many paediatric hospitals. The documented benefits are many, including improving patient and family satisfaction, communication, discharge planning, and patient safety. Reference Mittal18 While implementing a standard approach to communication can be useful, individual preferences may not be accounted for in a one-size-fits-all approach. Prior studies have qualitatively investigated aspects of family communication through small focus groups, Reference Greenway, Rosenthal, Murtha, Kandil, Talento and Couloures2 but none to our knowledge have directly asked families about their specific preferences for communication and integrated these preferences into the medical team workflow, despite a stated need in the literature. Reference Miller, Blume, Samsel, Elia, Brown and Morell4 In our study, we attempted to implement a standardised communication preferences assessment early in the child’s ICU hospitalisation. This assessment tool did not result in statistically significant improvements in parent participant’s satisfaction with care or communication as compared to parents who did not receive the communication assessment tool. However, the responses from parents about their communication preferences indicate that it is important for the medical team to attempt to inquire about and take into account a parent’s communication preferences, particularly when there are potential barriers to communication.
Communication preferences
Parents in the intervention group reported a range of preferences related to communicating with the medical team. While some communication styles and methods were more preferred than others, there were no single communication preferences that dominated. More parents preferred detail-oriented than big-picture communication, but it is likely that a portion of parents prefer a combination of both, depending on the specific circumstances. More parents preferred daily updates, such as those that occur during family-centred rounds, rather than weekly care conferences. This is corroborated by other studies, such as by Zurca et al., which demonstrated that families of hospitalised paediatric ICU patients prefer meeting during rounds or at the bedside in contrast to formal family meetings. Reference Zurca, Wang, Cheng, Dizon and October19 Finally, an important portion of parents prefer to be the primary communicator to their child but recognise the challenges of communicating information in developmentally appropriate ways. In addition to the primary medical team, other members of the multidisciplinary team, such as social work, child life, and palliative care, can have an essential role in facilitating communication not just between medical teams and families but also within families.
Communication satisfaction
While there were no significant differences between the intervention and control groups, much can be learned from the responses of participants as a whole. A primary area of improvement may be to help parents prepare for setbacks. Our study identified a large portion of parents who felt neutral or unprepared for difficult decisions or setbacks, similar to the finding of Miller et al. that one-third of parents felt unprepared for decision-making, despite 88% feeling supported. Reference Miller, Blume, Samsel, Elia, Brown and Morell4 It is impossible to anticipate and discuss every possible complication, and it may be that no parent can be fully prepared for serious complications or the death of their child. However, evidence-based expectation setting and pre-emptive counselling regarding the possibility of complications may be important to consider. Blume et al. surveyed parents of children who had died from a cardiac diagnosis; parents reported that they realised their child had no realistic chance of survival a median of only two days prior to the child’s death, Reference Blume, Balkin and Aiyagari20 indicating that adequate and timely conversations about poor prognosis were either not had or were ineffective. For the medical team, identification of patients at high risk for acute decompensation and death may be especially important so that pre-emptive discussions can be initiated earlier in the patient’s course.
It is important to recognise that respondents consistently felt that much was done well by the ICU team in our study. Greater than 90% of all respondents felt supported with decision-making, and it is also notable that >90% of all respondents felt that communication with the ICU team improved. This is encouraging as it indicates that the team can learn parental communication preferences over time and therefore support them more effectively. Perhaps further implementation of communication assessment tools such as the one used in our study or improved strategies for integrating parents’ communication preferences into workflow may assist with accomplishing this important task early in patient care.
English- versus Spanish-speaking respondents
Racial and ethnic disparities exist within paediatrics for a range of populations and diseases. In paediatric cardiology specifically, there has been a documented survival advantage for white patients with congenital heart disease, Reference Chan, Pinto and Bratton21–Reference Nembhard, Salemi, Ethen, Fixler, DiMaggio and Canfield23 cardiac transplantation, Reference Morris, Kransdorf, Coleman and Colvin24,Reference Pietra, Kantor and Bartlett25 and cardiomyopathy and myocarditis Reference Olsen, Tjoeng, Friedland-Little and Chan26 in comparison to other races and ethnicities. While this disparity is multifactorial, a component of this disparity is related to communication and language barriers Reference Palau, Meier, Brinton, Hwang, Roosevelt and Parker27,Reference Stephen and Zoucha28 . Our patient racial distribution was similar to regional census numbers: 29 27% were charted as Latino/Hispanic, similar to the 2010 regional census of 23.5%. In practice, we found it challenging to recruit participants who preferred to participate in Spanish; 12–15% of our ICU’s patient population is estimated to be Spanish-speaking, but we were only able to recruit 9% to our study within our recruitment timeline. It is likely that the challenges to consenting and administering materials to Spanish-speaking participants were obstacles to successful recruiting, possibly in part related to the availability of interpreter services. In our CVICU at the time that this study was being conducted, in-person interpreters were available by appointment or on an as-needed basis, but they were a limited resource. Inadequate representation of Hispanic patients is unfortunately a common feature of medical research Reference Rodríguez-Lainz, McDonald, Penman-Aguilar and Barrett30,Reference Seltz, Zimmer, Ochoa-Nunez, Rustici, Bryant and Fox31 and ongoing steps to correct gaps in data for Hispanic populations must be pursued. Our Spanish-speaking sample was too small to make significant conclusions.
Limitations
As this was designed as a quality improvement initiative, multiple iterations and improvements were required. Despite these modifications, the PCA has inherent limitations. It was developed out of a need for a better assessment of parental communication preferences; as no other relevant survey tool was available, the PCA was developed specifically for the purposes of this study. It was not validated prior to its use in this study. While multiple stakeholders, including patient and family representatives, provided input in the survey development phase, some responses indicated that aspects of the survey tool were difficult to understand. Additionally, developing an effective and standardised implementation strategy was challenging; completed PCAs were sent to the individual family’s social worker, who then communicated information from the survey to the medical team during weekly interdisciplinary rounds. However, this was variably implemented, and without a convenient and efficient place to document communication preferences in the electronic medical record, this information was likely inadequately integrated into clinical care. Additionally, as discussed above, participants who speak languages other than English were inadequately represented in this study. Finally, as this was a survey-based single-centre study, conclusions and generalizability are limited.
Conclusions
To our knowledge, this is the first assessment tool that evaluates individual parents’ preferences regarding communication of treatment plans and decision-making for paediatric patients in the ICU receiving cardiac intensive care. Parents of patients reported a wide range of preferences related to communication with the medical team (Figures 1 and 2) and important gaps in communication with and support of parents in the ICU were identified. Although there were no significant differences in communication satisfaction for the intervention group compared to controls, nuanced and individualised assessments of parents’ communication preferences are needed, and future studies and quality improvement work that address this are essential. Specifically, the development of multi-lingual standardised assessment tools should be pursued and applied to paediatric patients in intensive as well as acute care settings. Improved methods for delivering this information to providers and retaining the information in efficient and accessible ways should be considered. Examples range from low-tech communication support tools such as utilising the whiteboard in the patient room for questions for the medical team Reference Sehgal, Green, Vidyarthi, Blegen and Wachter32 to higher-tech ones, like utilising the electronic medical record to document and carry forward patient and parent preferences. Reference Holt, Spanbauer and Cusatis33 Finally, steps must be taken to identify and address the additional barriers that parents who are racial and ethnic minorities or who speak languages other than English experience when it comes to communication. While surveys that assess communication preferences are one way to collect this information, other modalities of eliciting and communicating patients’ and parents’ preferences should also continue to be explored. Attempts to standardise processes are important, and thus our study attempted to develop a standardised process for documenting communication preferences. However, the human connection that is so fundamental to the art of medicine cannot be supplanted by surveys. For the parents of a critically ill child, a timely, honest, and caring discussion with their medical team remains an essential and irreplaceable component of their child’s medical care.

Figure 1. Parent preferences for CVICU team communication with parents regarding daily care plans versus difficult decisions or setbacks. Respondents were asked to select every option that aligned with their preferences. CVICU = cardiac ICU.

Figure 2. Parent preferences for CVICU team communication with paediatric patient for daily care plans versus difficult decisions or setbacks. Respondents were asked to select every option that aligned with their preferences. Percentage reported excludes respondents who answered, “not applicable.” CVICU = cardiac ICU.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S104795112402506X.
Acknowledgements
Thank you to the Lucile Packard Children’s Hospital Social Work Team and Stanford Office of Patient and Family Education for their contributions in helping to develop the PCA.
Author contribution
Katherine Hansen conceptualised and designed the study, designed the data collection instruments, coordinated and supervised data collection, collected data, carried out the analysis, drafted the initial manuscript, and reviewed and revised the manuscript. Meghna D. Patel, Harvey Cohen, and Andrew Y. Shin conceptualised and designed the study, contributed to the development of study materials, and reviewed and revised the manuscript. Erin Jenkins, Aihua Zhu, Shawna Collins, and Kimberly Williams obtained consents, collected data, and reviewed and revised the manuscript. Beth Kaufman and Loren D. Sacks contributed to the development of study materials and reviewed and revised the manuscript. Ariadna Garcia and Yingjie Weng provided statistical support and reviewed and revised the manuscript.
Financial support
None.
Competing interests
None.
Ethical standard
This study was approved by the Stanford University Institutional Review Board.
Consent to participate
Consent to participate was obtained from all participants.
Consent for publication
All authors approved the final manuscript as submitted and agreed to be accountable for all aspects of the work.