Almost all psychiatrists rely on neuroscience implicitly when it comes to prescribing drugs – one of our defining operational characteristics as a professional group in the mental health arena. Why else would you want to give a patient a receptor antagonist, or a reuptake inhibitor, if you didn't think their symptoms were somehow related to abnormal synaptic signalling between nerve cells? Yet there seems to be a deep-seated reluctance to embrace the theoretical and therapeutic potential of neuroscience for psychiatry, despite the danger, powerfully articulated by Craddock et al, Reference Craddock, Antebi, Attenburrow, Bailey, Carson and Cowen1 that the absence or attenuation of a secure scientific connection to the physical mechanisms of the body, specifically the brain, will cast psychiatry intellectually adrift from the core principles of medicine.
It would be particularly disappointing if this were to happen now. The connections between physical and mental health have never been clearer theoretically or more important therapeutically for patients, whether treated, for example, by psychiatrists with antipsychotic drugs that have unwanted metabolic effects or by physicians for somatic syndromes such as obesity that have prominent behavioural components. Moreover, we are just beginning to formulate integrated mind–brain models that incorporate both the genotype and its expression in hierarchical and complex phenotypes of the brain, and the bilaterally causal interactions between brain phenotypes and the physical and social environments. Owing to technological advances, such as high-throughput gene expression profiling and neuroimaging, we also now have unprecedented power to measure intermediate brain phenotypes clinically (Fig. 1).
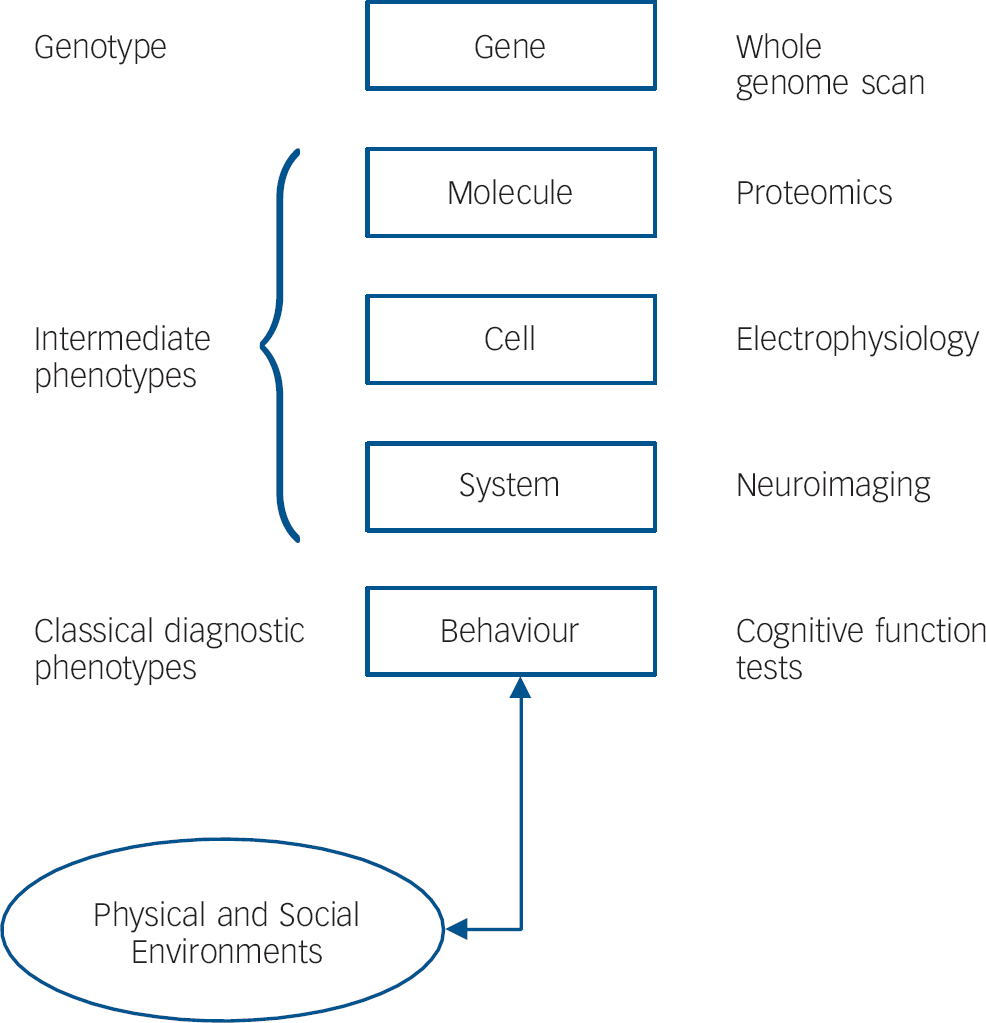
Fig. 1 Genotype, brain phenotypes, and environments. Genetic variation drives a hierarchy of complex brain phenotypes, culminating in behaviour, which mediates a bilaterally causal interaction with physical and social environments. All levels of this model are now accessible empirically in humans using appropriate investigational tools.
At such a time, could it possibly be that mainstream British psychiatry is retreating into a ‘neurophobic’ position? We can imagine three general recruiting slogans for the neurophobic cause, summarised and rebutted briefly below.
Physical models of mental functions or disorders are scientifically primitive
It is admittedly the case that the neuroscience of normal or abnormal cognition is far from complete; but the rate of technical and conceptual progress in neuroscience generally has been explosive over the past two decades. There have been major advances in understanding the genetic control of early brain development, the cellular substrates of memory and learning, and the relationships of mental states such as mood or attention to the configuration of large-scale brain functional networks. These theoretical developments have arisen in the context of major technical advances in our ability to measure cognitive function more exactly, to visualise the living human brain safely and in great detail, and to interrogate the human genome and related gene expression patterns both comprehensively and minutely.
The early impact of these fundamental developments on understanding of psychiatric disorders is clear to see. For example, when the first modern computed tomography studies of schizophrenia reported evidence of enlarged lateral ventricles in patients Reference Johnstone, Crow, Frith, Husband and Kreel2 the results were contested by some of the orthodox opinion leaders of the day Reference Hill3–Reference Marsden5 at least partly on the grounds that schizophrenia was, by definition, a ‘functional’ psychosis, meaning it could not possibly be associated with ‘organic’ abnormalities of brain structure. This false dichotomy has since lost its axiomatic status, thanks to a generation of computed tomography and magnetic resonance imaging studies which now collectively provide support for the multi-faceted model: that chronic schizophrenia is associated with grey matter volume deficits in an anatomically distributed network of cortical and subcortical regions; Reference Ellison-Wright, Glahn, Laird, Thelen and Bullmore6 that comparable though less severe deficits in network connectivity are often present in unaffected relatives or in patients pre-psychosis, indicating that they mediate genetic risk predisposing to emergence of psychosis; Reference Lawrie, McIntosh, Hall, Owens and Johnstone7 and that grey matter deficits in cortical regions tend to become more severe in patients following the first clinical episode of psychosis, Reference Salisbury, Kuroki, Kasai, Shenton and McCarley8 implying that there may be an important therapeutic opportunity to improve the long-term clinical prognosis of schizophrenia by minimising post-diagnosis progression of anatomical deficits in the cortex. In parallel to these insights, we have also accumulated much greater understanding of the critical importance of frontocortical activation and functional connectivity as brain markers for cognitive impairment in schizophrenia, Reference Stephan, Baldeweg and Friston9,Reference Tan, Callicott and Weinberger10 and changes in high-frequency (gamma and beta band) oscillations of frontal cortex have been linked persuasively to cellular abnormalities of cortical interneurons in schizophrenia. Reference Gonzalez-Burgos and Lewis11
This is just one example of neuroscience driving progress in understanding of psychiatric disease, from erroneous dogmatism to a gradually consolidating empiricism; other examples could be drawn from the fields of autism, mood disorders, obsessive–compulsive disorder, drug dependency, etc. In short, we are lucky enough to be living at the start of a golden age for neuroscientific discovery in relation to psychiatry and there has never been a better time for psychiatrists to pursue physical models of the mind and mental disorders.
Physical models of mental functions or disorders are too reductionistic
Reductionist is a word that can be used in two rather different senses in neuroscience and psychiatry. The first, scientific sense, is related to levels of explanation and the classical reductionist model of early 19th century physics, which over-optimistically anticipated that the macroscopic world could be entirely understood and predicted on the basis of complete knowledge about the microscopic behaviour of each atom. An analogous expectation for psychiatry might be phrased as the ambition that we will one day be able to reduce the appearance or content of mental symptoms to the status of a few key molecules (e.g. genes or transmitters).
For every twisted thought a twisted molecule? Scientifically this seems most unlikely to be a realistic destination. What we know about the genetics of psychiatric disorders, for example, does not suggest that we will find one or a few genes of major effect that can provide a classically reductionist explanation for why a particular individual develops, say, bipolar symptoms. It is much more likely that we will need to develop more complex accounts, involving the interactions between multiple genes each of minor effect, post-translational and epigenetic factors, and the differential impact of environmental stressors depending on individual genetic susceptibility. We will ultimately need to account not only for how the behavioural phenotype emerges from the genotype but also how neural systems are plastically adaptive to environmental factors, including interpersonal and social relationships which are themselves largely constructed by behaviour (Fig. 1). The scientific insights of real value in defining such models will be those which can make complementary and mutually informative connections between different levels of description. We do not feel that there is an ultimate level of description or that it should be the aim of neurobiological psychiatry to deem one level of description paramount.
The key word is complex. At every level of biological description, from the genome through molecular, cellular and system levels of the phenome, we can expect to find that it will generally not be the case that one agent at a lower (micro) level of description causes one effect at a higher (macro) level of description. It is much more likely that higher level behaviour emerges from the non-linear interactions between multiple agents organised as a system or network at a lower level. For example, the cellular effects of glutamate transmission will depend on a signalling network of about 100 post-synaptic proteins and the emergence of most cognitive and emotional processes will depend on large-scale neurocognitive networks of functionally connected brain regions. We can aspire to an integrated hierarchical phenotype of psychiatric disorders that extends from genes to behaviours, but it will not be classically reductionistic in form; it will be couched in the language of systems biology and modern complexity theory.
The clinical sense in which we might apprehensively talk about reductionism is in relation to our professional interactions with patients and the importance of their personal experience of mental illness. If we were to be transformed overnight into a cadre of high-tech, integrative neuroscientists, using brain scans and gene expression profiles to make diagnoses, wouldn't this somehow detach us from our patients, impoverish our engagement with them, and leave them better understood objectively perhaps, but more isolated subjectively?
We suspect that for many psychiatrists, and other mental health professionals, some such rather soulless vision of how brain science might transform clinical practice is close to the heart of their objection to the biological agenda. We appreciate that it is a principled objection, based on an admirable determination to respect the uniquely personal ramifications of mental illness, but, to our minds at least, it is not a compelling argument for neurophobia. One of the things that patients and their families want most from psychiatrists is a better, indeed expert, understanding of their predicament: an explanation for why they have become ill; a reliable prediction of how much they can expect to improve and over what timescale; and a personalised rationale for any proposed treatment. Currently, we often lack good answers to a lot of these questions because we are operating in a pseudo-physician mode, for example prescribing drugs on the basis of vague talk about possible transmitter imbalance without knowing anything, typically, about the physical state of the brain in which said imbalance is supposed to reside. Our capacity to provide meaningful and precise explanations for patients will increase to the extent that we can refine and implement physical models of mental disorder. Moreover, just as empathy, understanding, respect and consideration may be regarded as attributes of any good physician – regardless of specialisation – there is no reason to diminish their importance in psychiatry or to predict that they will be undermined by the more secure neurobiological understanding of mental disorder that we anticipate.
Nor should the advance of neuroscience in psychiatry be assumed, as it sometimes is, to threaten the value of psychotherapy. Let us not forget, psychoanalysis was invented by a neuroscientist and its subsequent evolution and diversification has yielded many important insights into mental, interpersonal, developmental and therapeutic processes. In our view, a neuro-Freudian synthesis is theoretically conceivable, even probable, over the next 10 years or so. It is already the case that key concepts under study, such as inhibition, implicit motivation and latent or unconscious processing, overlap strongly in terminology and conceptualisation, with psychoanalytic constructs. In future, we are likely to see more neuroscientific evidence for changes in brain organisation caused by maternal deprivation, childhood abuse or other classical psychoanalytic traumas. We can also expect to see more clinical trials combining cognitive–behavioural therapy with short-term drug treatments in a synergistic approach to post-traumatic stress, addictive and memory disorders.
Physical models haven't made any difference to clinical practice in psychiatry
It can seem as if there is a yawning gap between the rhetoric of scanners and micro-arrays and the reality of psychiatric practice in the UK, where there is currently agreed to be no clear role for neuroimaging, biomarkers or genetic testing. But it has always taken time – 20 years or more – for major scientific developments to translate into changes in clinical practice. Medicine is a conservative profession. Healthcare is a regulated, legislated, potentially expensive service and the hard-nosed economic debates concerning real-life implementation of neuroscientifically progressive treatments in psychiatry will be protracted. Nobody should think it's going to be easy just because it's inevitable.
It will take several decades of effort, by generational waves of committed, talented clinicians and scientists, to deliver the therapeutic potential of a psychiatry that is fully informed by the brain and its extraordinary capacity to interact with the environment. Under these circumstances, neurophobia is not a position our generation can afford to take. It is not in the best interests of our patients. It neglects a rare opportunity to advance Reil's seminal vision of psychiatrists as physicians of the mind. It seems intellectually timid at a time when we should be bold. And in any case, we suspect that, whatever our mainstream position in this country at this time, on a global scale neurophobia is historically doomed.
We will do much better by actively seeking to make Reil's psychiatry real, for the benefit of our patients and to the credit of our profession, than by retreating or perseverating in the face of the great opportunity (and challenge) presented by contemporary neuroscience. We suggest that the Royal College of Psychiatrists might usefully consider initiatives for strategic action (see below) to support the future growth of a brain-based medicine of the mind and its psychiatric practitioners.
Proposals for strategic action
-
(1) Review and enhance the neuroscientific curriculum for the MRCPsych examination. We do not need to know the anatomy of the cranial nerves; we should know more about cognitive testing, neurobiological sequelae of early-life social deprivation and psychopharmacology.
-
(2) Influence evolution of the MBBS psychiatry curriculum and examination to include more basic and cognitive neuroscience and its applications to understanding and treatment of disorders; perhaps commission new teaching materials to support national changes in the MBBS curriculum.
-
(3) Initiate a strategic review of neuroscience and psychiatry, the scientific, therapeutic and professional implications, to be conducted in partnership with cognate groups from the Royal College of Physicians and other professional groups with the goal of integration not fragmentation.
-
(4) Ensure that the role of brain biology does not become a forgotten element within design of mental health services by specialist mental health National Health Service trusts.
-
(5) Enhance our efforts collectively to communicate the neuroscientific basis of mental disorders to patients, their families and the general public. Ignorance of the physical basis of any disease (epilepsy, leprosy, tuberculosis) has generally led to social stigmatisation of patients with the disease. Greater knowledge of the physical basis of mental illness should have a destigmatising benefit for our patients; but to have such a transforming attitude on entrenched social attitudes towards mental illness, the new medicine of the mind will need to be communicated more effectively and to a wider public than it has been to date.




eLetters
No eLetters have been published for this article.