1. Introduction
Since December 2019, the world is facing the novel coronavirus disease 2019 (COVID-19). The rapid disease transmission, increasing influx of infected persons and subsequent fatalities has led to tremendous panic. An early investigation into the psychological response among the general population of China showed that 53.8% of participants rated the psychological impact of this outbreak as moderate or severe (Elbay et al., Reference Elbay, Kurtulmuş, Arpacıoğlu and Karadere2020). The disease is highly infectious, primarily spreads through respiratory droplets and contact routes (World Health Organization, 2020), and can rapidly lead to deterioration in health. Empirical clinical data shows that the overall case fatality rate is 2.3% (Zhong et al., Reference Zhong, Luo, Li, Zhang, Liu, Li and Li2020).
COVID-19 has challenged all nations in several dimensions, among which is the mental health of medical staff (Spoorthy et al., Reference Spoorthy, Pratapa and Mahant2020). Health care workers (HCWs) on the frontline are directly at risk of developing symptoms of psychological distress. The Centers for Disease Control and Prevention (CDC) warn HCWs about feelings of uncertainty, being overwhelmed, lacking motivation and having trouble sleeping or concentrating (Centers for Disease Control and Prevention, n.d.). The deluge of new cases, depletion of personal protection equipment, lack of definitive treatment, variable management guidelines, and inadequate social support, all contribute to the mental burden of HCWs. Fear of the contagion, infection of family and colleagues, and feelings of stigmatization lead to reluctance to work and high levels of stress, anxiety, and depression, among some of the psychological implications (Lai et al., Reference Lai, Ma, Wang, Cai, Hu, Wei, Wu, Du, Chen, Li, Tan, Kang, Yao, Huang, Wang, Wang, Liu and Hu2020).
2. Objectives
Pakistan has rarely addressed the mental health of its health care providers not withstanding this pandemic, with only one study on this subject (Sandesh et al., Reference Sandesh, Shahid, Dev, Mandhan, Shankar, Shaikh and Rizwan2020). Since Pakistan’s first case reported on 26 February, the total number of cases stands at 296,149 as of 31 August 2020 (Government of Pakistan, n.d.). This propagation in an already resource-poor country has placed tremendous physical and psychological pressure on its HCWs. Epidemiological data on the mental health consequences of COVID-19 and their screening, assessment, and management is lacking (Rana et al., Reference Rana, Mukhtar and Mukhtar2020). This is especially true for frontline workers of the Emergency Department (ED), which is a high-risk area being the first stop for suspected COVID-19 patients. A study on Chinese ED HCWs showed prevalence rates of depressive symptoms and post-traumatic stress disorder at 25.2% and 9.1%, respectively (Song et al., Reference Song, Fu, Liu, Luo, Wang, Zhoug, Yan and Lvn.d.). We aim to identify the prevalence, risk factors and sources of anxiety among ED HCWs in Pakistan during the COVID-19 pandemic. The insight our study provides may entice further research into the diagnosis, treatment and prevention of the psychological impact of this crisis on this vulnerable group.
3. Methods
This cross-sectional survey was conducted from 1 May 2020 to 20 May 2020 in the ED of Shifa International Hospital (SIH), Islamabad, Pakistan. Ours is a small ED which sees around 40,000 patients per annum. Purposive total population sampling was chosen for the entire census of HCWs (n = 109) providing patient care during the defined time frame. ED surveys have been conducted on a similar sample frame (Abraham et al., Reference Abraham, Thom, Greenslade, Wallis, Johnston, Carlström, Mills and Crilly2018; Basu et al., Reference Basu, Yap and Mason2016). Paper-based self-reporting questionnaires were distributed at the start of each work shift till all elements of the sample frame were included. The Institutional Review Board and Ethics Committee (IRB&EC) provided ethical approval for the study. All subjects were invited to participate on a voluntary basis and they provided informed consent prior to study commencement.
3.1. Materials
Our questionnaire consisted of 25 questions divided in three sections. The first section queried about demographic and occupational characteristics. The next section of questions answered as “yes” or “no”, pertained to specific sources of stress for HCWs while caring for COVID-19 patients: availability of personal protective equipment, their own physical and mental health, safety of their families, lack of social support and childcare, and feelings of incompetence and stress affecting work performance. These questions were derived from the prevailing concerns for HCWs (Shanafelt et al., Reference Shanafelt, Ripp and Trockel2020). Cai et al. used similar questions (Cai et al., Reference Cai, Tu, Ma, Chen, Fu, Jiang and Zhuang2020). The third section measured the anxiety symptoms among HCWs during the pandemic using the Generalized Anxiety Scale-7 (GAD-7) (Spitzer et al., Reference Spitzer, Kroenke, Williams and Löwe2006). GAD-7 is a validated, seven-item, self-reporting, screening questionnaire that assesses participants’ mental health status during the previous 2 weeks (Williams, Reference Williams2014). Each item is scored from 0 to 3 based on severity of symptoms experienced. The scores are then totaled from 0 to 21 with 5, 10 and 15 as cut-off points for mild, moderate and severe anxiety symptoms, respectively (Williams, Reference Williams2014). GAD-7 has been widely used during the SARS-CoV-2 pandemic to evaluate the prevalence of anxiety symptoms among HCWs across the globe (Centers for Disease Control and Prevention, n.d.; Gupta et al., Reference Gupta, Mehra, Niraula, Kafle, Deo, Singh, Sahoo and Grover2020; Wilson et al., Reference Wilson, Raj, Rao, Ghiya, Nedungalaparambil, Mundra and Mathew2020).
3.2. Statistical analyses
All study variables were coded numerically, including the degree of anxiety. The following analyses were carried out using SPSS 26.0 (IBM Corp): descriptive analyses, summarized as frequency (percentage); nonparametric tests to identify the differences in categorical variables between groups, as the data did not conform to normality; multivariate ordinal regression to identify the association between demographic and occupational variables as independent risk factors for the development of anxiety according to severity presented as odds ratios (ORs) and 95% CIs, after adjustment for confounders, including age, gender, marital status, designation, years of experience and work placement. P-value ≤0.05 was statistically significant.
4. Results
A total of 109 questionnaires were collected, of which 107 were valid. Two responses were excluded because of incomplete data. The response rate was 98%.
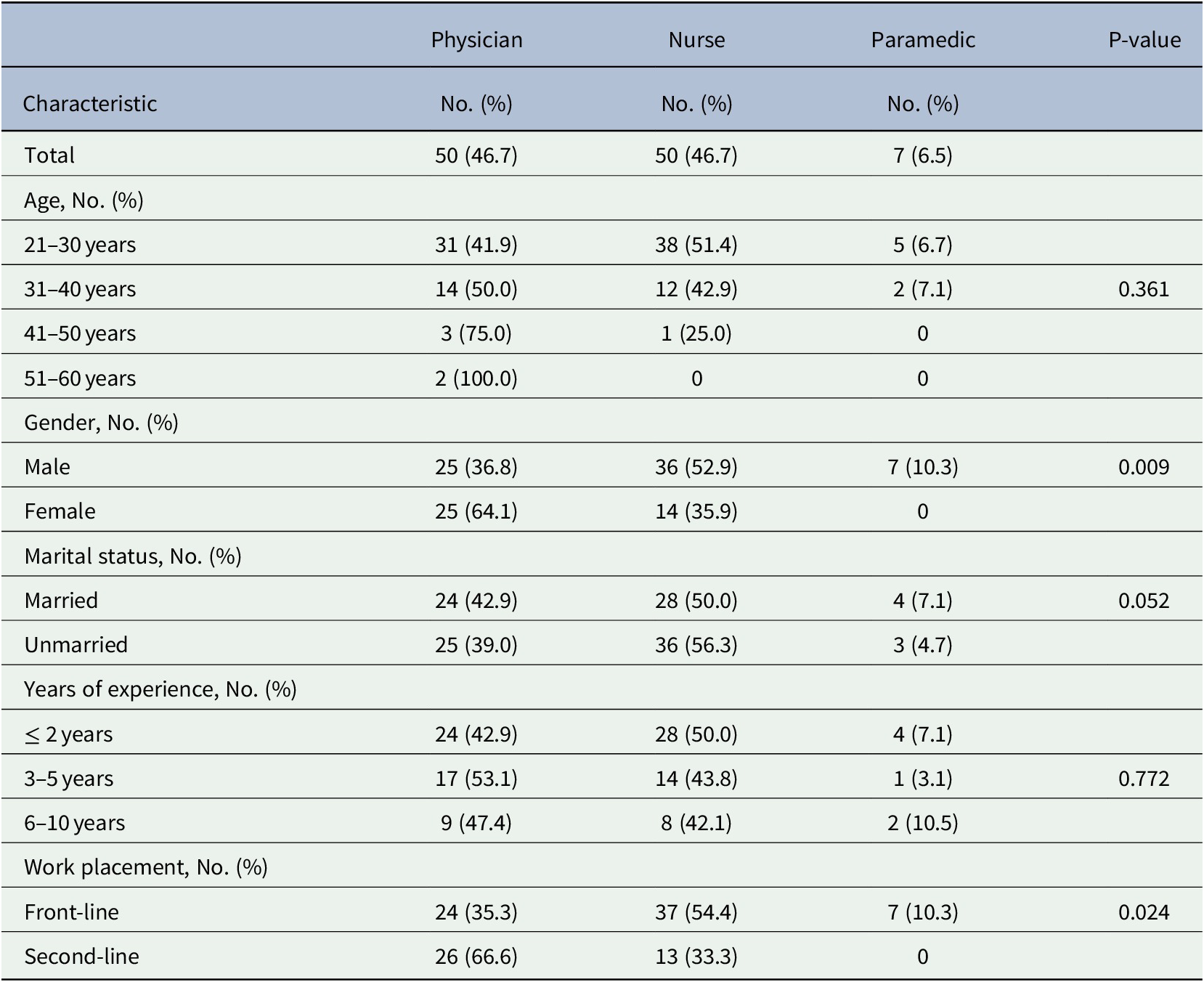
The demographic and occupational characteristics of all the participants are presented (Table 1). Male: female ratio of nurses and paramedical staff was greater as compared to almost equal numbers among physicians; more nurses and paramedical staff had worked as front-liners. These differences were statistically significant (Table 1).
Table 1. Demographic and occupational characteristics of participants
4.1. Comparison of severity of anxiety between groups
The severity of anxiety was compared across all groups (Table 2). Half the participants experienced anxiety, most had mild symptoms. Six (5.6%) healthcare workers reported severe anxiety, average GAD-7 score of 16.50 (±0.50); all were nurses and frontline workers. Nurses’ mean score was 10.28 (±4.39), classified as moderate anxiety symptoms, whereas physicians’ average score was 9.18 (± 4.90), classified as mild symptoms. This difference was statistically significant (P = 0.001). The younger age group 21–30 years scored an average of 10.03 (±4.40), compared to 31–40 years and 41–50 years mean scores of 9.55 (±5.10) and 5.75 (±5.50) respectively; the difference was statistically significant (P = 0.035). Frontline workers’ mean score was 9.80 (±4.50) compared to second-line workers’ score of 9.30 (±4.90), which was statistically significant (P = 0.001). The variables of gender, marital status and years of experience, were not significant when compared with the severity of anxiety.
Table 2. Severity categories of anxiety in total cohort and subgroups

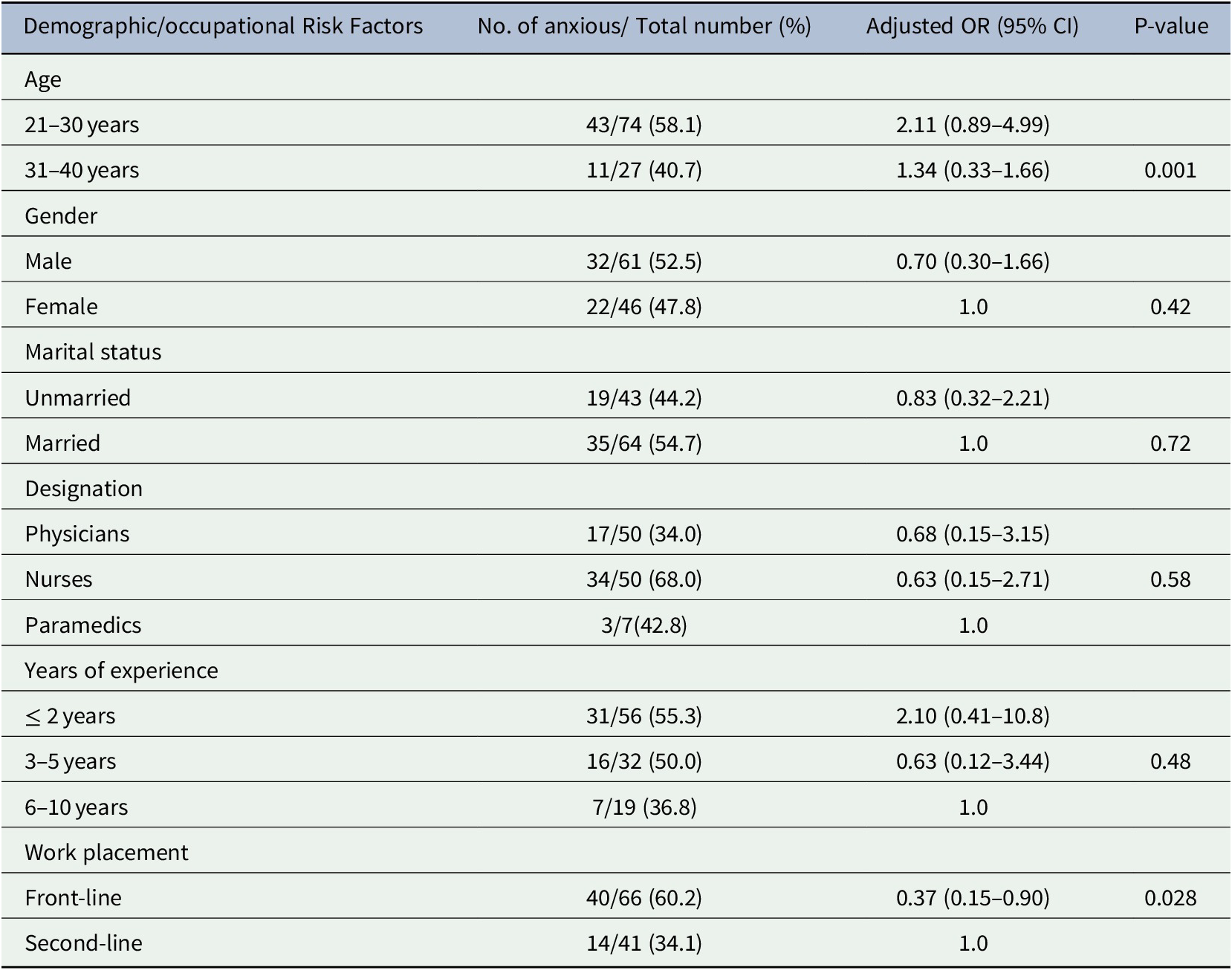
4.2. Risk factors for the development of anxiety
The association between the demographic and occupational characteristics of participants and the development of anxiety symptoms showed the youngest age group (21–30 years) and frontline workers were at greatest risk of having anxiety (P = 0.001, OR 2.11, 95% CI 0.89–4.99 and P = 0.028, OR 1.34, 95% CI 0.33–1.66, respectively). There was no association demonstrated between anxiety symptoms and the other study variables including gender, marital status, designation and years of experience. (Table 3).
Table 3. Analysis of demographic and occupational factors associated with developing anxiety
4.3. Sources of stress
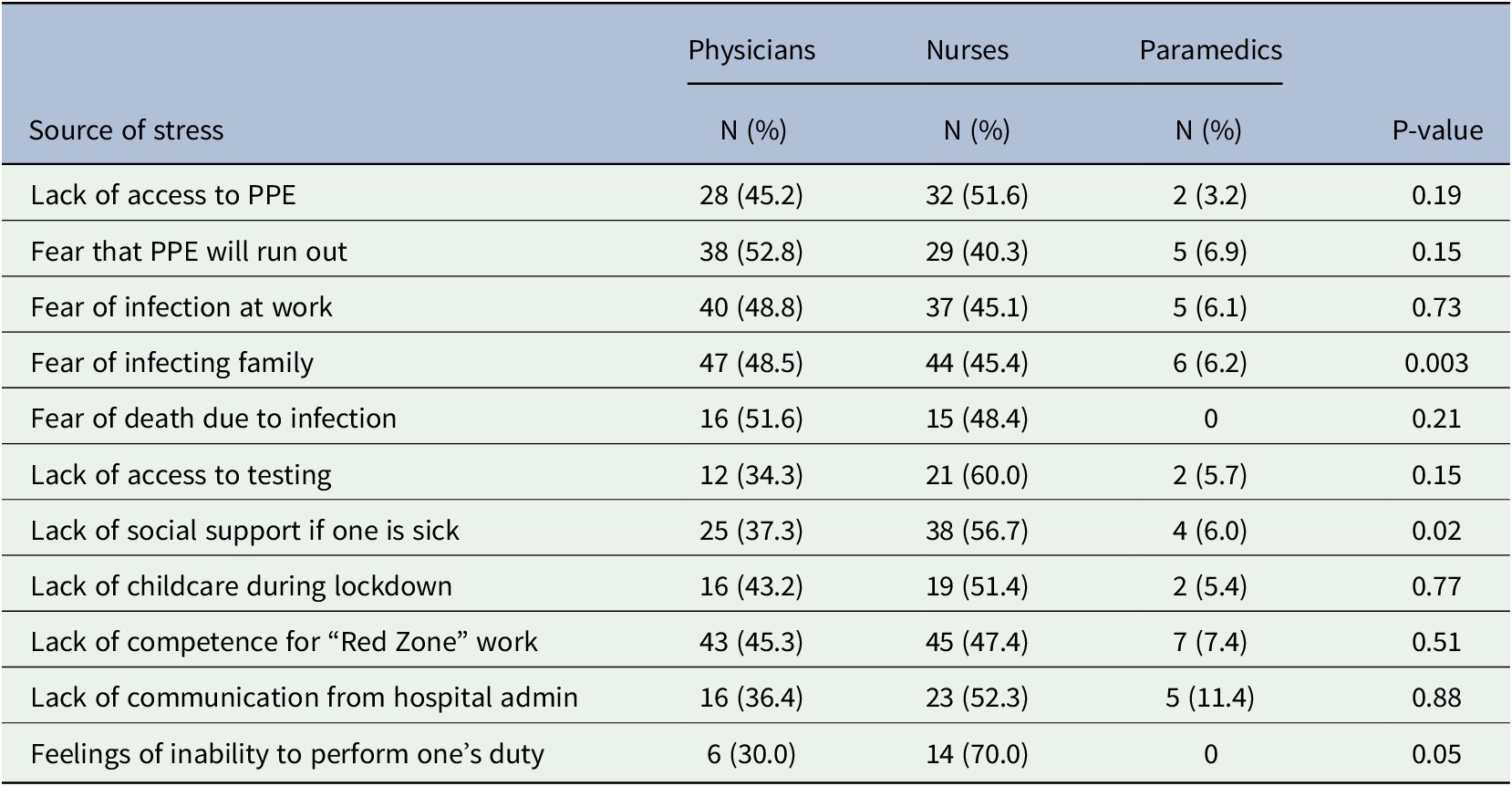
Significant sources of stress among HCWs were the fear of carrying the infection home (P = 0.003), lack of social support when the HCW were themselves unwell (P = 0.02) and feelings of inadequate performance at work (P = 0.05) (Table 4).
Table 4. Sources of stress perceived by HCWs during the pandemic
5. Discussion
Anxiety is a natural response to stress. Stress is a normal body reaction to any changes that occur. The SARS-CoV-2 pandemic has abruptly and drastically changed the lives of people of all nations across the world. While HCWs of all types are caring for large surges of COVID-19 patients, it is essential to maintain their numbers while maximizing their abilities to perform to their full potential (Shanafelt et al., Reference Shanafelt, Ripp and Trockel2020). To this end, our study attempted to evaluate the prevalence, severity, sources and risk factors of anxiety symptoms that endanger the psychological health of HCWs. This was meant as a screening to identify requirements for professional referral and subsequent intervention. Studies on the mental health of HCWs in previous disease pandemics are well-document, yet there are marked differences compared with the current situation (Xiao et al., Reference Xiao, Zhu, Fu, Hu, Li and Xiao2020). The subject of the ongoing psychological impact on HCWs during the COVID-19 pandemic has gained interest in many hard hit countries such as the U.S., China, Iran, India and Italy (Centers for Disease Control and Prevention, n.d.; Gupta et al., Reference Gupta, Mehra, Niraula, Kafle, Deo, Singh, Sahoo and Grover2020; Kaveh et al., Reference Kaveh, Davari-tanha, Varaei, Shirali, Shokouhi, Nazemi, Ghajarzadeh, Feizabad and Ashraf2020; Pearman et al., Reference Pearman, Hughes, Smith and Neupert2020; Rossi et al., Reference Rossi, Socci, Pacitti, Di Lorenzo, Di Marco, Siracusano and Rossi2020; Song et al., Reference Song, Fu, Liu, Luo, Wang, Zhoug, Yan and Lvn.d.; Wilson et al., Reference Wilson, Raj, Rao, Ghiya, Nedungalaparambil, Mundra and Mathew2020; Xiao et al., Reference Xiao, Zhu, Fu, Hu, Li and Xiao2020).
We chose the ED as the setting for our study. EDs across the globe have borne the brunt of managing COVID-19 patients; however the psychological impact on this particular subgroup of HCWs has yet to be studied. We included all elements directly involved in patient care, including paramedical staffs who are technical assistants to aide physicians and nurses with surgical procedures in the ED. An enormous challenge in this crisis has been the restructure of the work flow of hospitals to accommodate the influx of patients while containing the cross-transmission of disease. In our ED, a separate negative pressure isolation area has been dedicated for suspected/confirmed COVID-19 cases, named the “Red Zone”, where staff was randomly rotated at regular intervals. Those who had worked in the “Red Zone” were considered as front-line workers, while those who had not were considered as second-line. Most of our participants had worked in the “Red Zone”.
Nearly half of our participants reported symptoms of anxiety, but mild symptoms accounted for a larger proportion of disturbances; only 5.6% reported severe symptoms. Among Chinese HCWs, anxiety symptoms ranged from 11.4–50% (Centers for Disease Control and Prevention, n.d.; Song et al., Reference Song, Fu, Liu, Luo, Wang, Zhoug, Yan and Lvn.d.; Zhu et al., Reference Zhu, Sun, Zhang, Wang, Fan, Yang, Li and Xiao2020). Similar to our observation, studies from Iran and India demonstrated that the majority of HCWs had minimal to mild anxiety symptoms (Kaveh et al., Reference Kaveh, Davari-tanha, Varaei, Shirali, Shokouhi, Nazemi, Ghajarzadeh, Feizabad and Ashraf2020; Wilson et al., Reference Wilson, Raj, Rao, Ghiya, Nedungalaparambil, Mundra and Mathew2020). Younger age and working at the frontline were found to be independent risk factors for developing severe anxiety symptoms. Lai et al. from China also observed the latter (Lai et al., Reference Lai, Ma, Wang, Cai, Hu, Wei, Wu, Du, Chen, Li, Tan, Kang, Yao, Huang, Wang, Wang, Liu and Hu2020). Other countries have seen higher anxiety levels in younger HCWs (< 40 years of age), who were more likely to be female, which was not observed in our participants (Badahdah et al., Reference Badahdah, Khamis and Mahyijari2020; Kaveh et al., Reference Kaveh, Davari-tanha, Varaei, Shirali, Shokouhi, Nazemi, Ghajarzadeh, Feizabad and Ashraf2020). We also identified significant sources of distress according to occupational designation. Our results are similar to those of a meta-analysis exploring the factors related to HCWs’ psychological difficulties, which found that infection of colleagues or family members, protective measures, and medical violence were among the main concerns of HCWs in COVID-19 affected areas (Pappa et al., Reference Pappa, Ntella, Giannakas, Giannakoulis, Papoutsi and Katsaounoun.d.). Similar results were observed by Cai et al. (Reference Cai, Tu, Ma, Chen, Fu, Jiang and Zhuang2020). Surprisingly, lack of personal protective equipment was not a significant source of anxiety in our cohort. This may arise as a concern in other settings or a different time frame.
COVID-19 has adversely affected healthcare systems, created public health challenges and unnerved health service providers world-wide. Recognizing the most vulnerable HCWs, working in high-risk areas such as the ED, it is essential to provide them with support for coping with the emerging situation. Our hospital designed mental health facilities for HCWs specific to this crisis in the form of informative webinars and group sessions, as well mandatory screening sessions by professionals. Those suffering from severe symptoms were offered one-on-one sessions while maintaining their confidentiality. Timely assessment and provision of appropriate resources by the relevant healthcare authorities to combat, as well as prevent these disturbances is greatly needed, especially as the end of the pandemic is as yet, out of sight.
Our study has several limitations. Our scope was limited to screening for anxiety symptoms and identifying stressors. The actual prevalence of clinically diagnosed anxiety may vary. Stressors will vary individually and according to the prevailing situation, not all can be covered. The results of our study cannot be generalized to all HCWs working in EDs locally or internationally unless similar studies are undertaken in their settings on a larger sample of randomized subjects. Although our response rate was high and we used a validated screening tool, response bias is a possibility. Since it was a cross-sectional observation, longitudinal follow-up is lacking. This is required to assess the long-term effects of such crises on HCWs, providing future avenues of research. Furthermore, the mental health condition of HCWs themselves infected with COVID-19 is also a subject to be explored.
6. Conclusion
Our study aimed to identify the presence of anxiety symptoms and sources of distress among HCWs of an ED in Pakistan during the SARS-CoV-2 pandemic. We found the degree of anxiety symptoms to be mild; young nursing staff who had direct contact with infected patients were more affected. Significant sources of stress included fear of infecting family, lack of social support when the HCW were themselves unwell and feelings of inadequate work performance. Provision of appropriate measures to alleviate as well as prevent anxiety in HCWs is the need of the hour.
Acknowledgment
The authors sincerely appreciate the participation in this study of all the medical staff who are fighting against COVID-19.
Financial support
None to declare.
Conflict of interest
None to declare.
Data availability statement
The data that support the findings of this study are openly available in Pubmed Central at. http:// https://www.ncbi.nlm.nih.gov/pmc/, reference numbers 1, 3–7, 9–25;
World Health Organization at https://apps.who.int/iris/bitstream/handle/10665/331616/WHO-2019-nCoV-Sci_Brief-Transmission_modes-2020.2-eng.pdf, reference number 2;
The official website of the Government of Pakistan at http://covid.gov.pk/stats/pakistan, reference number 7.
Author contributions
-
a. N. Haroon: concept and design, drafting of manuscript.
-
b. S. S. Owais: data acquisition, analysis, interpretation, takes responsibility for data integrity and accuracy; drafting of manuscript
-
c. A. S. Khan: critical appraisal; administrative support
-
d. J. Amin: data acquisition, technical support
Disclaimer
This is an original work. All references have been clearly cited. This manuscript has not been published, nor is it under consideration for publication elsewhere.






Comments
Comments to the Author: 1. page 4, line 40. The decimal place of mean and SD should be uniform.
2. All decimal place of P value should be three.
3. page 5, line 4. The P value cannot be equal and smaller than 0.001 at the same time.
4. page 5, line 4. the 95%CI contains 1 with the p value smaller than 0.001. But how is that possible? There must be something wrong. The researchers should check them statistical outcome again.
5. All tables should be three-line tables.