CLINICIAN’S CAPSULE
What is known about the topic?
Emergency physicians and trainees have high rates of stress and burnout.
What did this study ask?
How do reported stressors for emergency physicians and trainees differ between high and low resource settings?
What did this study find?
Trainees in the low resource setting reported higher stressors. Trainees reported higher levels of stressors than specialists in general.
Why does this study matter to clinicians?
High levels of reported stressors among trainees, and in low resource settings should be acknowledged and mitigated where possible.
INTRODUCTION
Occupational stress is a serious problem worldwide. The 2012 Global Workforce Study reported that four out of ten respondents were directly influenced by excessive pressure (stress) in the workplace. 1 Occupational stress accounted for 35% of all work-related illnesses in the United Kingdom (UK) during 2014 and 2015. 2 In Canada, occupational stress has an estimated financial cost of at least CDN$20 billion per year with one in four Canadian workers describing their work lives as highly stressful.Reference Anderssen 3 , Reference Crompton 4 Unfortunately, no direct comparative statistics are available for the South African setting. However, the World Health Organization (WHO) noted that in 2004, 50% of South African health care workers reported verbal abuse in the workplace that could be interpreted as evidence of occupational stress. 5
The WHO defines occupational stress as the response workers may demonstrate if presented with work demands and pressures that are not matched to their knowledge and abilities and challenges their ability to cope.Reference Leka, Griffiths and Cox 6 Both the WHO and UK Health and Safety Executive (HSE) acknowledge that all workers experience pressure at work on a daily basis by needing to perform continuously at their best. However, if workers experience excessive work-related pressure, without the opportunity to sufficiently recover, it may result in occupational stress. 7 , 8
Emergency medicine (EM) is regarded as one of the most stressful specialties in medicine.Reference Gallery, Whitley, Klonis, Anzinger and Revicki 9 - 14 Sustained high occupational stress levels can manifest in many negative outcomes including poor mental and physical health, decreased career longevity, and eventual burnout.Reference Leka, Griffiths and Cox 6 , Reference Gallery, Whitley, Klonis, Anzinger and Revicki 9 , Reference Burbeck, Coomber, Robinson and Todd 12 , Reference Arora, Asha, Chinnappa and Diwan 13 Recent surveys of doctors working in frontline medical specialties such as EM reported the highest prevalence of burnout.Reference Arora, Asha, Chinnappa and Diwan 13 , 14 In Cape Town, South Africa (SA), a recent study analyzed doctors working in frontline community hospitals and noted that the prevalence of burnout and depression were as high as 76% and 27%, respectively.Reference Rossouw, Seedat and Emsley 15
EM is a relatively young specialty with a paucity of qualified specialists worldwide. Low resource settings (severe mismatch between health care supply and demand), such as SA, are especially affected by an acute shortage of EM specialists. In 2014, SA had 92 EM specialists certified by the Health Professions Council of South Africa (HPCSA), serving a population of 54 million. 16 In contrast, EM in Canada has been a recognized specialty since 1982. In 2014, Canada had over 3000 EM physicians and EM physicians in training to serve a population of just over 35 million. 17
The 1999 Romanow Commission estimated that one EM physician was needed per 5000-patient emergency department (ED) visits per annum.Reference Affleck, Dodd and Drummond 18 This estimation translates to a requirement of 1000 EM physicians for the province of Ontario alone that far outstrips the number of currently practising EM physicians available.Reference Affleck, Dodd and Drummond 18 There is an overall severe shortfall of practising EM physicians for both Canada and SA, with the latter being much worse off.
Both the Canadian and South African public health care systems are based on similar social insurance principles for health care delivery. They offer a good comparative model to assess the impact of health care work-related stressors. The inclusion of both countries in the study was based on convenience, being representative of a low- and high-resourced setting, as well as the authors’ unique insights of both countries EM health systems. Disparities between the work stressors of both countries may be explained by the marked difference in EM physicians’ supply and demand and how the two EM systems are managed. Similarities may be because of the inherent stressors within the organization of the EM specialty itself and the nature of the work.
To bolster the number of EM specialists required to fill the severe shortfall, it is imperative to optimize the already stressful work environment by mitigating the occupational stressors currently experienced, thereby reducing the risk for any negative mental or physical effects to reduce attrition from an already under-resourced profession.
We aimed to test the hypothesis that well-resourced Canadian EM physicians experience lower levels of work stress than their relatively under-resourced South African counterparts.
METHODS
Study design
We completed a cross-sectional electronic survey of EM physicians and trainees in Canada and SA. The study was approved by both the Health Research Ethics Committee at Stellenbosch University, South Africa (Ref: S14/07/146) and the Research Ethics Board of the Horizon Health Network, Saint John, NB, Canada (Ref: 2014–2033).
Study population and setting
The Canadian study population included all EM physicians and trainees that were registered with the Canadian Association of Emergency Physicians (CAEP). For SA, EM specialists who were registered with the HPCSA and EM specialist trainees who were registered with university academic EM specialty training programs were included in the study population. The study population excluded EM specialists and trainees who were practising outside of either SA or Canada.
Sampling
Between October and December 2014, emails were sent to all potential participants (the complete study population for both countries) inviting them to participate anonymously in the online survey. The invitational email had a link to the online platform for the survey. Three reminder emails were sent at regular one-month intervals to improve response rates.
Survey tool
The validated management standards indicator tool (MSIT) (available at: http://www.hse.gov.uk/stress/standards/pdfs/indicatortool.pdf ) was developed by the UK HSE as a validated a psychometrically sound measure of organizational performance against the HSE management standards and can provide a broad overview of occupational stressors within organizations.Reference Kerr, McHugh and McCrory 19 - Reference MacKay, Cousins, Kelly, Lee and McCaig 22
The UK HSE identified six key work stressors that, if not managed properly, are associated with poor health and well-being, lower productivity, and increased absences. The six domains are demands, role, support, change, control, and relationships (see Table 1).Reference Cousins, MacKay and Clarke 21
Table 1 The MSIT (HSE) survey tool
We assessed these six key risk factors among our study sample (survey respondents) by sending a 35-item Likert scale–based MSIT questionnaire to the study population in both countries. The MSIT survey answers were weighted from one (poor) to five (desirable) measuring subjectively how well the employer is performing in managing each of the six work-related stressors in relation to the management standards.Reference MacKay, Cousins, Kelly, Lee and McCaig 22
The survey also included demographic questions to assess occupational stressors in different categories (Table 2).
Table 2 Demographic data
Analysis
Continuous data were analyzed with IBM SPSS (v. 22 Statistical Package for the Social Science) software. The means and corresponding 95% confidence intervals (CI) were calculated for each of the demographic subsets and work stressor categories. The significance of differences in mean MSIT scores was compared with the independent samples t-test.
RESULTS
We received complete responses from 74 South African (50% response rate) and 430 Canadian (33% response rate) participants. Recruitment is further described in Figure 1. The two reasons that were identified and led to exclusions were incomplete surveys and participants not meeting the inclusion criteria.
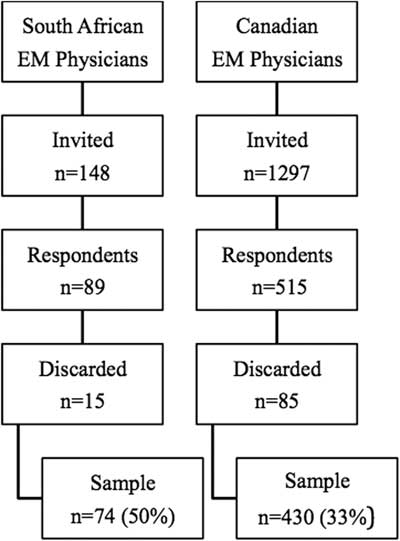
Figure 1 Recruitment flow diagram. EM=emergency medicine.
Groups were balanced for gender, other than in the Canadian trainees’ group, in which females represented the highest proportion (Table 2). Age distribution was similar for both trainee groups. The age distribution was younger for South African specialists than their Canadian peers, with the majority having practised for less than a decade. Eighteen percent of South African trainees indicated that they were considering leaving the EM profession in the next five years that contrasts strongly with the Canadian trainees. The lower potential for specialist attrition compares well between the two groups after allowing for age-related retirement.
The survey results (see Table 3 and Figure 2) indicate that the South African EM trainees (n=38) had the lowest scores (indicating highest stressors) on all measured stressor domains. Compared with Canadian trainee counterparts (n=35), South Africans trainees had significantly worse reported stressor domain scores for demands (2.2 [95% CI 2.1–2.3] v. 2.9 [95% CI 2.8–3.1], respectively; p<0.0001); role (3.6 [95% CI 3.4–3.7] v. 4.0 [95% CI 3.8–4.1], respectively; p<0.0001); manager support (2.9 [95% CI 2.7–3.1] v. 3.9 [95% CI 3.6–4.1], respectively; p<0.0001); peer support (3.3 [95% CI 3.1–3.5] v. 4.0 [3.8–4.2], respectively; p<0.0001); change (2.4 [95% CI 2.2–2.6] v. 3.2 [2.9–3.4], respectively; p<0.0001); control (2.6 [95% CI 2.4–2.7] v. 3.2 [3.0–3.4], respectively; p<0.0001); and relationships (3.3 [95% CI 3.1–3.5] v. 3.9 [3.6–4.1], respectively; p<0.0001). Comparing South African and Canadian specialists, there was one domain (control) in which Canadian specialists scored significantly worse than South African specialists (3.26 [95% CI [3.19–3.33] v. 3.51 [95% CI [3.30–3.72], respectively; p=0.038), whereas South African specialists had significantly worse scores on peer support (357 [95% CI 3.28–3.86] v. 3.86 [3.81–3.92], respectively; p=0.004); relationships (3.40 [95% CI 3.09–3.70] v. 3.73 [95% CI 3.66–3.79], respectively; p=0.004); and role (4.02 [95% CI 3.73–4.30] v. 4.22 [95% CI 4.17–4.27], respectively; p=0.033). South African trainees had significantly worse scores in work stressor levels for demands, change, control, and role domains, as compared with South African specialists. However, Canadian specialists had significantly worse scores related to experiencing work stressors from demands and manager support, as compared with Canadian trainees who had lower role domain scores (see Table 3).
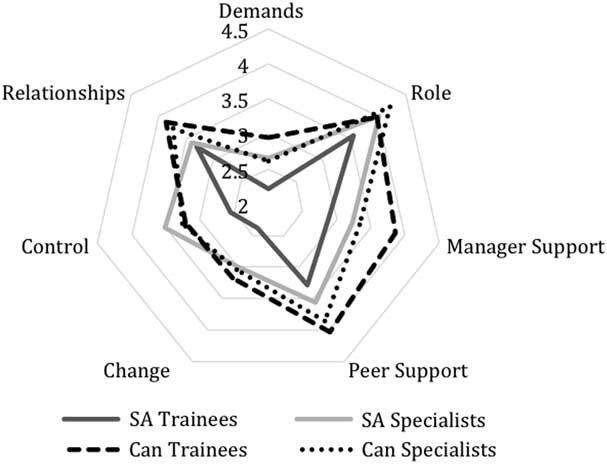
Figure 2 Key stressor comparisons among the four groups, by country and stage of career. *Lower values (closer to the centre) represent higher stressor scores. Can=Canadian; SA=South African.
Table 3 MSIT key stressor comparisons
CI=confidence interval; EM=emergency medicine.
*Lower values represent higher stressor levels
DISCUSSION
SA versus Canada
South African EM trainees were found to adversely experience all six MSIT stressor categories (demands, role, support, change, control, and relationships), as compared with their Canadian counterparts. The low resource setting in SA may be a significant factor contributing to the high level of work stressors measured among their EM trainees. The high demands stressor may be caused by the limited access to medical equipment and disposables that prevents the provision of optimal patient care. Furthermore, chronic staff shortages, undermining optimal shift rotational planning and crossover cover, often result in higher duty hours than previously anticipated with fewer EM physicians available to share ever-increasing clinical workloads. Change management was the second lowest score (high stressor) for South African trainees, whereas the biggest difference in work stressor scores between the trainee groups was the managerial support reported by South African trainees. The South African trainees’ low resource setting provides less flexibility in scheduling their work shifts that may have contributed to their higher work stressors. A 2009 study reported that patient care might be compromised by long physician hours, resulting in sleep deprivation, that, in turn, caused cognitive impairment, leading to an increased potential for medical errors to occur.Reference Ulmer, Wolman and Johns 23 Adverse conditions for residents have effects on their well-being and patient safety outcomes, although more recent studies have shown that flexibility in scheduling may still maintain learner health.Reference Ulmer, Wolman and Johns 24 , Reference Asch, Bilimoria and Desai 25
The Canadian trainees’ more favourable score for peer-support may be explained by strong representation, as well as a larger number of peers available for sharing the workload, resulting in more balanced clinical hours. Similar to the US,Reference Ulmer, Wolman and Johns 24 , Reference Asch, Bilimoria and Desai 25 the hours of service by residents in Canada has been regulated closely by residency programs to reduce occupational stress and sleep deprivation. Canadian EM trainees are supported by collective agreements in their respective provincial jurisdictions to limit unhealthy working conditions, unlike their South African counterparts.
The differences between the South African and Canadian specialists may reflect the developing nature of the specialty in SA with peers being disparate and the role being less well defined and perhaps, partly as a consequence of relationships at work, being more pressured than for Canadian specialists. However, Canadian specialists reported more difficulty with control over their work that was perhaps not an anticipated finding.
The Canadian EM trainees scored similarly to a UK-based study by Basu et al. that also used MSIT. Both EM specialist groups performed less well except on the domains of change and control. However, the UK study used a much smaller group of EM physicians with more diverse experience levels.Reference Basu, Yap and Mason 26
EM trainees versus specialists
The scores for South African EM trainees indicated higher stressors for demands, change, control, and role domains, in comparison with South African specialists. This may be explained by trainees working more and less sociable (shifts v. on call from home) clinical hours, as compared with specialists. Trainees have less management representation concerning daily operational decisions and future planning of the specialty itself that may have contributed to their higher control domain stressor results. Additionally, the specialty is still developing in SA, and the role of the trainee continues to evolve.
Canadian EM trainees had higher stressor scores for the role domain in comparison with Canadian EM specialists. This could potentially be attributed to trainees still exploring and defining their role within the EM specialty during their formative years.
Canadian specialists had less favourable stressor scores for demands and manager support, as compared with their trainees. The EM specialty is unique in that it requires specialists to be a clinical manager and liaison among patients, other specialties, and hospital management. This new managerial role is novel to most newly qualified EM specialists and requires substantive work experience and non-clinical management skills.
LIMITATIONS
The cross-sectional study design that was used could not provide work stressor severity and domain changes over time in relation to the EM physicians’ career progression. The relatively low response rate (33%) of the Canadian cohort may have skewed the results because of responder bias. Although the number of South African respondents was low (n=89), their higher responder rate (60%) was more representative of the study population. The impact of possible responder bias was limited by sending regular reminders to improve the responder rates in both surveys. Non-responder bias may also have influenced the study results. Specialists and trainees in both countries feeling aggrieved because of severe stress and were more likely to respond to the survey, resulting in an overestimation of the measured stressors. The South African responses were skewed toward Cape Town, as compared with the rest of the country, that was especially noted in the trainee group. This may be attributed to the primary investigator working in the Western Cape Province training group. However, Cape Town trains more than 60% of the national EM physicians.
Despite the internal limitations of the study, it was clear that work stressors were pervasive across both EM platforms irrespective of setting. The survey found that South African EM trainees were exposed to the highest levels of work stressors across all measured stressor indicators, as compared with South African specialists and their Canadian peers. However, the other three groups also demonstrated significant differences in their perception of work stressors, across different stressor indicators. This highlights some areas in which efforts could be focused to improve working and training conditions. Future qualitative research could help to explore underlying themes for the differences in the reporting of work stressor indicators among the respective four groups. This study has added further strength to the argument that a search for solutions to mitigate the effect of highly perceived work stressors is required. A Canadian study previously demonstrated that task-oriented coping (taking direct action to alter the situation itself) was associated with a decreased risk of burnout, while emotion-oriented coping (managing one’s emotional responses to a situation) was associated with an increased risk of burnout.Reference Howlett, Doody and Murray 27 Our study provides useful data upon which stressor domains to focus management action while considering the challenges faced in EM.
The consequences of failing to act may contribute to mental health problems and possible attrition from the profession that would be concerning, given the existing shortage of EM physicians in both countries. The creation of an optimal work environment for all health care workers, in which work stressors are recognized as a potential threat and avoided or managed effectively, is needed.
CONCLUSIONS
Reported occupational stressors were found to be less favourable among EM trainees in SA. The more favourably reported occupational stressors among Canadian EM specialists and trainees may be explained by its higher resourced setting (facilities, equipment, consumables, and staff), as compared with SA, and perhaps by the fact that the specialty is more established in Canada and, therefore, has better regulation of the work environment for physicians.
Competing interests: None declared.







