Introduction
System changes in Austrian primary health care
Since 2017, the Austrian primary health care (PHC) system has been undergoing a transformation, shifting from care provided mainly by individual general practitioners to the establishment of multiprofessional ‘primary health care units’ (PHCUs) (Primärversorgungsgesetz, 2023). In 2021, the European Commission funded €100 million to the Austrian ‘Attractiveness and Promotion of PHC’ project aimed at enhancing access to easily accessible health services and the establishment of more PHCUs (Austrian National Public Health Institute, 2022).
Thus, Austria has been following international good practice models by adopting multiprofessional approaches inspired by frameworks in Belgium and Slovenia, where care models emphasize collaboration between diverse health professionals to address complex patient needs (OECD, 2016). These models echo the principles of the Declaration of Alma-Ata, which highlight the importance of team-based, community-responsive care (Dussault et al., Reference Dussault, Kawar, Castro Lopes and Campbell2018).
End of 2024, Austria has 75 PHCUs, with 58 more planned by 2025 (Primary Care Platform, 2022). Austrian PHCUs are required to form multiprofessional teams, consisting of at least two general practitioners and one nurse, constituting the ‘core team’ (Primärversorgungsgesetz, 2023). Most PHCUs also meet earlier requirements, i.e., three general practitioners, nurses, and office assistants. In practice, of the 75 PHCUs today 56 PHCUs incorporate at least three additional professional groups (PGs) from the so-called ‘extended team’.
Austrian PHCUs exist in two formats: centres, where all professionals work in one location (currently 65 centres), and networks, where team members are spread across a defined region (currently 10 networks). The ‘extended team’ is formed based on the region’s needs, consisting of the following PGs in addition to the ‘core team’: dietitians, midwives, occupational therapists, physiotherapists, psychotherapists, social workers, and speech therapists. Pharmacies act as collaborating partners of PHCUs (Primary Care Platform, 2022). PGs such as biomedical scientists, orthoptists, medical training therapists, and radiographers aim to be integrated into Austrian PHCUs (Luxbacher, Reference Luxbacher2019; Jaksch, Reference Jaksch2020; Resch, Reference Resch2021; MTD-Austria, 2023; MTD-Austria, 2024; Rausch et al., Reference Rausch, Birklbauer, Federolf, Hecksteden, Hofmann, Niebauer, Reich, Rieder, Ruin, Scharhag, Seebacher, Treff, Tschan, Wessner, Würth and Müller2024).
Addressing non-communicable diseases through multiprofessional PHC
Transitioning towards a multiprofessional PHC system in Austria also addresses the increasing burden of non-communicable diseases (NCDs), which account for 74% of all deaths globally, ischaemic heart disease currently being the leading cause (WHO, 2023). By 2050, diabetes and chronic obstructive pulmonary disease (COPD) are projected to follow on second and third position (WHO, 2023; Institute for Health Metrics and Evaluation, 2024). Austrian data shows circulatory diseases (35%), cancer (23%), Alzheimer’s and other dementias (4.3%), diabetes (3.6%), and COPD (3.1%) as leading causes of death (OECD, 2023). By 2019, 38% of Austrians aged 15 and older reported chronic health problems (Gassner & Reinsperger, Reference Gassner and Reinsperger2021).
NCDs have become a critical healthcare challenge due to their socioeconomic costs. PHC plays an essential role in effectively preventing and managing NCDs through multiprofessional teams improving patient outcomes (Fowler et al., Reference Fowler, Garr, Mager and Stanley2020; Hu et al., Reference Hu, Tan, Nguyen, Wu, Bahadin and Nadkarni2023; Tandan et al., Reference Tandan, Dunlea, Cullen and Bury2024).
Interprofessional collaboration in PHC
IPC promotes amongst others patient-centred care, shared decision-making, and clearer role definitions (WHO, 2010; Ruebling et al., Reference Ruebling, Eggenberger, Frost, Gazenfried, Greer, Khalili, Ochs, Ronnebaum and Stein2023). Successful IPC is often driven by shared goals, such as improving addressed care quality and expanding professional roles and is facilitated by, e.g., shared tools and mutual recognition of each other’s roles (Rawlinson et al., Reference Rawlinson, Carron, Cohidon, Arditi, Hong, Pluye, Peytremann-Bridevaux and Gilles2021; Wei et al., Reference Wei, Horns, Sears, Huang, Smith and Wei2022). Evidence from other countries shows that well-functioning IPC improves patient outcomes and overall care quality in a time of complex patient needs in PHC (WHO, 2010; Carron et al., Reference Carron, Rawlinson, Arditi, Cohidon, Hong, Pluye, Gilles and Peytremann-Bridevaux2021; Tandan et al., Reference Tandan, Dunlea, Cullen and Bury2024).
However, challenges such as unclear roles and poor communication hinder IPC, and many healthcare professionals lack the structured training needed for delegation and conflict resolution (Rawlinson et al., Reference Rawlinson, Carron, Cohidon, Arditi, Hong, Pluye, Peytremann-Bridevaux and Gilles2021; Wei et al., Reference Wei, Horns, Sears, Huang, Smith and Wei2022). Additionally, leadership and team building are critical for fostering IPC in PHC (Brown et al., Reference Brown, Mulder, Clark, Belsito and Thorpe2020). Transversal skills, such as adaptive problem-solving, the openness to continuous learning, socio-cultural sensitivity, and digital literacy, are also becoming increasingly important for frontline health workers to address modern healthcare challenges (Maeda & Socha-Dietrich, Reference Maeda and Socha-Dietrich2021).
Internationally, training programmes using, e.g., elements of online distance learning and simulation-enhanced interprofessional education to clarify roles, encourage teamwork, and break down professional silos (Wilhelmsson et al., Reference Wilhelmsson, Pelling, Ludvigsson, Hammar, Dahlgren and Faresjö2009; Ansa et al., Reference Ansa, Zechariah, Gates, Johnson, Heboyan and De Leo2020; Simons, Goossensen & Nies, Reference Simons, Goossensen and Nies2022) are promising. Yet, they require ongoing evaluation to refine their effectiveness and long-term impact as well as supportive policies of educational institutions and health care providers to overcome IPC challenges (Ansa et al., Reference Ansa, Zechariah, Gates, Johnson, Heboyan and De Leo2020; Simons, Goossensen & Nies, Reference Simons, Goossensen and Nies2022).
Context and aim
This study is part of an Austrian university project focusing on designing a specific training programme for IPC in PHC. The respective Austrian Ministry already stated in 2014 that respective curricula should provide interprofessional modules developing knowledge on PGs and conveying tools for effective teamwork in PHC (Federal Ministry of Social Affairs, Health, Care and Consumer Protection, 2014), which thus far has not been implemented in the corresponding university region.
International literature on IPC success factors in PHC and on key elements of training programmes to prepare future professionals for IPC exist, but no study has investigated IPC in the emerging context of Austrian PHCUs. Understanding the possible national specificities from a professional perspective is crucial, as over 80% of the Austrian health care and social workforce are trained in Austria (Österreichische Ärztekammer, 2023; Pilwarsch et al., Reference Pilwarsch, Schichl-Zach, Gruböck, Mathis-Edenhofer, Wallner, Cartaxo and Gyimesi2024).
Therefore, this study aims to explore the perspectives of health care and social professionals on IPC in Austrian PHC and thereof deduct starting points for the development of a proprietary specific training programme. The results will contribute to an international understanding of how IPC in different healthcare systems is perceived by professionals and where there is potential for change.
Methods
A systematic rule-guided qualitative content analysis of 15 focus group interviews (FGI) with Austrian representatives from practice (especially PHCUs), educational institutions, and professional organizations was performed.
The participants were selected from those PGs already engaged in Austrian PHCUs and those expecting to be working there prospectively. This is pertinent for developing a future-oriented training programme. 15 PGs were included: biomedical scientists, dietitians, general practitioners, medical training therapists, midwives, nurses, occupational therapists, office assistants, orthoptists, pharmacists, physiotherapists, psychotherapists, radiographers, social workers, and speech therapists. Given the unequal representation of these PGs in Austrian PHC, mono-professional FGIs were performed. Hence, data pertaining to collective attitudes, ideologies, and beliefs could be gathered distinctive to each PG (Mayring, Reference Mayring2016).
Recruitment proceeded from September to December 2021. PHCUs in Salzburg were requested to designate one professional from each PG. As not all 15 PGs were represented in these PHCUs, PHCUs from surrounding federal states were invited to name participants. For PGs currently not represented in PHCUs, self-employed professionals were named by their professional association. All teaching institutions and professional associations in Salzburg (and surrounding federal states where necessary) were contacted to nominate one representative. The goal was to include at least one representative of a teaching institution or professional association and one active health care professional, preferably from an Austrian PHCU. If named individuals refused, the facilitators aided in the search for alternatives. Therefore, specific numbers of approached professionals and refusals cannot be provided. A maximum of eight participants for each FGI was determined (Krueger & Casey, Reference Krueger and Casey2015; Lamnek & Krell, Reference Lamnek and Krell2016). The only exclusion criteria was the inability to speak German.
Subsequently, 58 potential study participants were contacted via email for informed consent, explaining that they could withdraw from further data processing via email up to one week after participation in the FGI without providing reasons (no participant exercised this option). The study was approved by the institutional ethics committee of Salzburg University of Applied Sciences (R-2021-GUK-001).
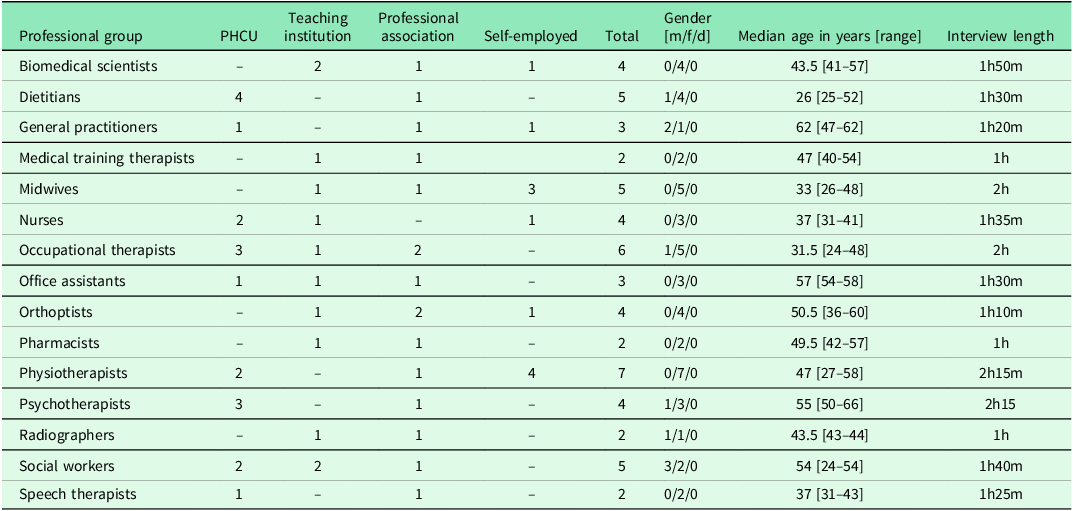
The sample’s actual composition (n = 58) is depicted in Table 1. Between two and seven professionals participated in each FGI. Most participants were women.
Table 1. Number of study participants representing a primary health care unit (PHCU), a teaching institution, their professional association or working self-employed
Data were collected between October 2021 and March 2022 through semi-standardized FGIs following this pre-established questioning route formulated in an open-ended manner and organized in a specific order in accordance with Mayring (Reference Mayring2016) and Krueger & Casey (Reference Krueger and Casey2015):
-
1) Introductory positioning question: How is your PG currently involved in Austrian PHC?
-
2) Main question on IPC: How do you experience the collaboration of your PG with other professions in PHC?
-
3) Main question on preparedness for IPC: How were you personally prepared for the collaboration with other health professionals and how are the current students prepared?
-
4) Concluding positioning question: How would you describe the ideal role of your profession in PHC?
All 15 FGIs were conducted online via Microsoft Teams. Although the lack of physical contact might affect interaction quality, online formats allowed for greater participation and bypassed pandemic restrictions. All 15 FGIs were moderated by the study’s first author (employed at a respective educational institution). Each FGI started with a brief explanation on the project, the goals of the FGI and the intended use of the data.
FGIs’ length ranged from 60 to 135 minutes (see Table 1). The video recordings were subsequently transcribed confidentially by the Austrian transcription service UniChamp GmbH.
Data were analysed between May and August 2022 using qualitative content analysis with inductive categorization according to Mayring (Reference Mayring2010) via QCAmap© Version 2022. The interviews were anonymized. The analysis solely considered the participant’s professional affiliation.
The data analysis started with the inductive development of a category system to systematically summarize the linguistic material. First, main categories were established, and subcategories were derived directly from the material using summarization techniques based on Mayring (Reference Mayring2016). To ensure rigour, transcriptions were analysed separately by two people. After a process of discussion and adjustment of discrepancies, the final category system was created and the material was analysed accordingly.
Findings
The qualitative content analysis led to two main and seven subcategories as shown in Figure 1.
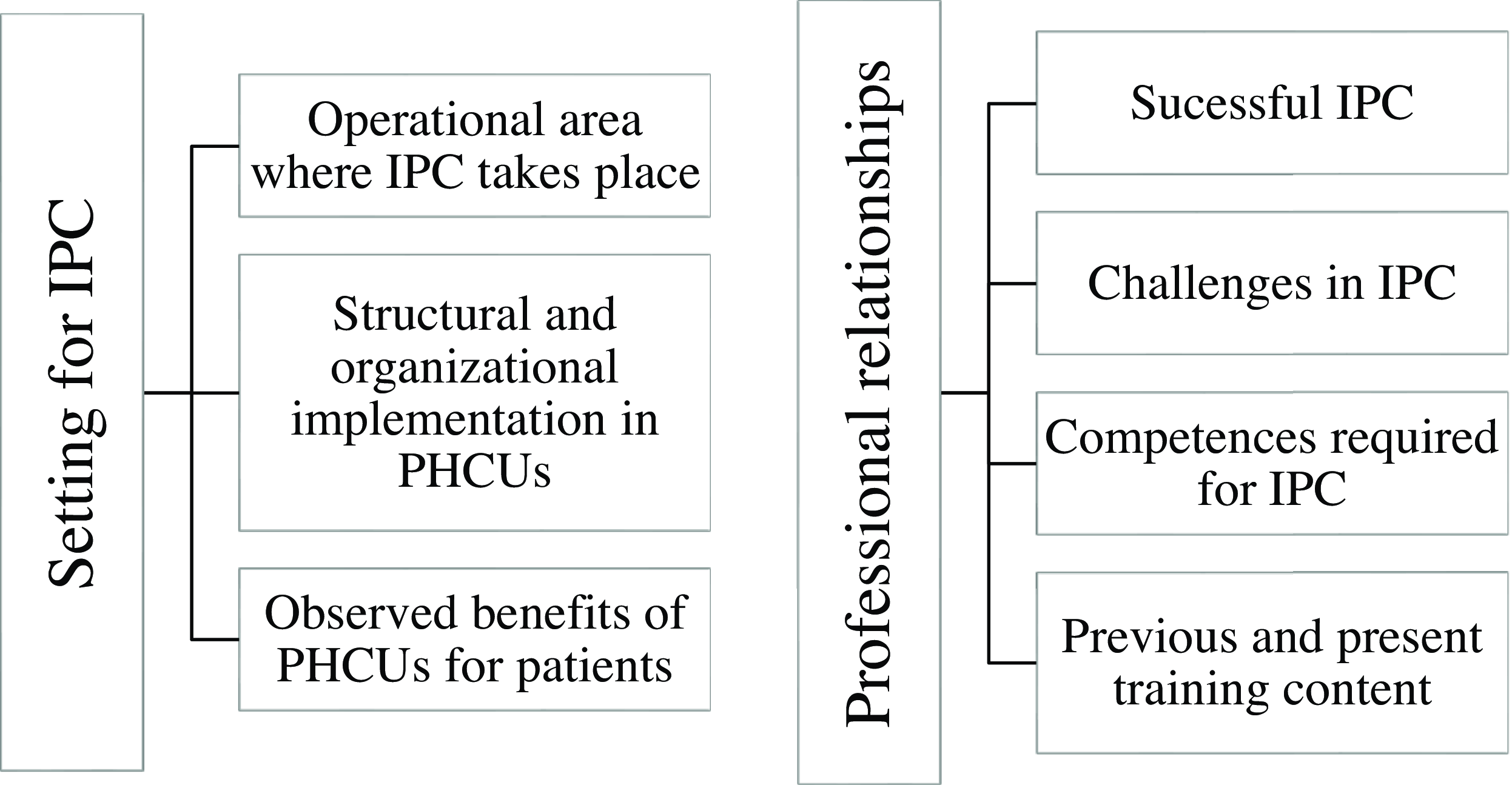
Figure 1. Category system with two main categories and seven subcategories (IPC: Interprofessional Collaboration).
Setting for IPC
This main category bundles the experience reports on three key themes (subcategories): the operational area where IPC takes place in PHC, the structural and organizational premises for this cooperation in PHCUs, and the observed benefits of PHCUs for patients.
Operational area where IPC takes place
This subcategory condenses participants’ elaborations on joint activities. Dietitians, medical training therapists, midwives, nurses, occupational therapists, and psychotherapists viewed preventative measures and patient education offered on an interprofessional basis as important activities in PHC in general and PHCUs specifically. Participants noted that patients better understand the specific operational area of each PG through this preventative work. IPC occurs during preventative work both within and outside the PHCU, including childcare units, private homes and schools. Health care and social experts collaborate to help patients, e.g., in adapting their homes to prevent falls. Nurses considered themselves the lynchpin, especially in disease management programmes, wound management, case and care management and holistic patient care:
‘(…) no matter what the patient’s concerns are, nursing is involved everywhere. (…) [in] case and care management, (…) wound care, (…) coordinating other health care providers, nurses are always in contact with the patient’. Nurse PHCU
A dietitian explained that the operational area in PHC differs from that in the acute sector, particularly in PHCUs. She noted that each day presents new challenges, with individual counselling and increasing tasks like visiting nursing homes. Unlike hospitals, PHCUs frequently experience interruptions due to team meetings and other organizational activities.
Biomedical scientists mentioned their PG is not yet visible in Austrian PHC, but they are eager to take over quality control responsibilities in PHC and PHCUs, especially in issuing reports and training, e.g., in blood sampling. They suggested the useful concept of a ‘movable lab’, where the laboratory comes to the patient instead of the other way around.
Structural and organizational implementation in PHCUs
This subcategory subsumes participants’ elaborations on particular structural and organizational manifestations in PHCUs that are essential for the implementation of IPC.
Patients’ first contact with a PHCU is typically with an office assistant, who directs them to the general practitioners. The interviewed general practitioners suggest that allowing patients to transition from the office assistant to the nurses for follow-up appointments could enhance regular care for chronically ill patients:
‘For me it is quite clear that there must be medical integration in PHC. (…) But I would like to start a nursing care department, where chronically ill multimorbid patients would have an appointment with a qualified nurse, where it is simply about weight, blood pressure, medication… The patients would have regular appointments and we would be called in, in case of a change or when problems occur’. General practitioner PHCU
Complex cases are discussed in PHCUs during weekly staff meetings. A coordinator and a joint calendar are of great importance:
‘We have a shared calendar as a PHC network. That means I see the appointments of the others and I can immediately make an appointment for my patient with another specialist, with the patient sitting opposite to me. (…) We have a coordinator who sort of brings us all together’. Psychotherapist PHCU
Observed benefits of PHCUs for patients
This subcategory encompasses participants’ observations regarding the advantages they perceive in PHCUs for patients.
PHCUs provide access to continuous care from multiple PGs. Many PHCUs offer extended opening hours, ensuring that daily appointment slots are available:
‘(…) if a patient comes on Monday and needs an appointment quickly, then the office assistant finds an available slot. This is not possible in the private practice, with a waiting time of several weeks’. Physiotherapist PHCU
These observations highlight the perceived advantages of PHCUs from the professionals’ perspective. Disease management programmes, particularly for chronic diseases, are designed with the patient’s needs in mind. Participants emphasized that prevention and health promotion work in PHC and PHCUs enhance patients’ health literacy.
Moreover, easy access to various therapies, swift assistance, and convenient diagnostics and treatment near patients’ homes, even in rural areas, were consistently mentioned as benefits. IPC emerged as a significant theme in this context, with discussions frequently focusing on how IPC contributes to improving patient care and accessibility:
‘(…) there are straightforward access points and you’re really close on a personal level (…) I think that’s such a huge benefit for everyone involved, especially for the patients. (…) that we can simply offer this all in one place’. Psychotherapist PHCU
Professional relationships
This main category summarizes four key themes (subcategories): successful IPC, challenges in IPC, competencies required for IPC, and previous and present corresponding training content.
Statements about IPC in other settings apart from PHCUs were also included, especially from biomedical scientists, medical training therapists, orthoptists, pharmacists, and radiographers (PGs not yet part of Austrian PHCUs).
Successful IPC
This subcategory sums up participants’ elaborations on factors contributing to a successful IPC in practice.
A beneficial close collaboration between general practitioners, office assistants, and other PGs in PHC settings was reported by the study participants. Consciously positively experienced IPC leads to friction-less and fluent teamwork, as shown in three examples: (1) occupational therapists, physiotherapists and nurses in the context of fall prevention, (2) speech therapists, physiotherapists and dietitians, (3) social workers and nurses in case and care management. A nurse illustrated the advantage of collaborating with social workers: they ‘look at the whole thing from a different perspective. […] But they need us just as much as we need them. It’s a partnership’. Nurse PHCU .
Overlapping areas can also be organized as a pragmatic division of tasks, e.g., physiotherapists stating that occupational therapy focusses on the upper and physiotherapy on the lower extremities.
In general, overlapping areas of competency between different PGs were experienced positively: ‘There are of course overlapping areas, […] And that’s the exciting thing, that you solve it together’. General practitioner PHCU
One physiotherapist emphasized the importance of attitudes: ‘We always coordinate when we have patients together […] as long as I engage in interaction, I always receive good collaboration in return’. Physiotherapist PHCU
Weekly team meetings support a low-threshold, simple and uncomplicated collaboration:
‘For me the main thing is that we simply appreciate each other very much as a team (…). And when (…) there’s a need for a psychotherapist or a dietitian, then we immediately network. We also have a team meeting once a week, where we exchange ideas and discuss patients that we treat together’. Psychotherapist PHCU
General practitioners are seen as ‘bosses’, nevertheless flat hierarchies can be experienced:
‘There is an incredibly flat hierarchy. It is clear that the doctors are the bosses, but they admit when they don’t know something and ask us to come in with our “occupational therapy – perspective.” Or they go to the dietician and ask for their perspective’. Occupational therapist PHCU
Challenges in IPC
This subcategory summarizes participants’ views on issues that hinder successful IPC in practice.
Participants noted that role ambiguity in teams can hinder IPC. Biomedical scientists, dietitians, medical training therapists, midwives, occupational therapists, radiographers and speech therapists reported that the other health experts often lack awareness of their roles or do not fully recognize their expertise:
‘It is unfortunately not the case that other health professions fully understand the scope of occupational therapy; for example, many physiotherapists are unaware of it’. Occupational therapist PHCU
‘I don’t know if this is just the case in my area, but doctors often don’t know what speech therapy entails or when they should refer a patient, or what issues speech therapists actually treat’. Speech therapist PHCU
Some situations were also mentioned by midwives, physiotherapists and social workers, where IPC is not perceived at eye level:
‘I actually wanted to report that the relationship to other PGs is often something of a double-edged sword. I do indeed experience a hierarchy problem. In other words, doctors always have the last word. (…) It is often the case that social work is regarded as subordinate in the hierarchy. I find that problematic’. Social worker teaching institution
A shortage of time and unfavourable circumstances for networking or monitoring patients’ therapeutic progress was identified by dietitians, occupational therapists, orthoptists, and speech therapists. This presents a significant challenge for IPC in PHC, particularly in PHCUs.
‘It is usually difficult to talk together. Because it is often the case that when you work your colleague is not there’. Speech therapist PHCU
Difficulties can arise in overlapping areas, e.g., between medical training therapists and physiotherapists or between midwifery and nurses:
‘I sometimes experience some difficulties with nurses who do breastfeeding and lactation training. They are normally very much appreciated (…) but there are also nurses who are active in the postpartum period. Not just breastfeeding counselling, but simply offering postpartum care. And that is simply a midwife’s job’. Midwife self-employed
Competences required for IPC
This subcategory aggregates participants’ elaborations on personal competences that are required for IPC.
Participants emphasized the need to understand each PG’s strengths, recognize boundaries, and clarify roles, believing that a strong professional identity enhances IPC, especially in the flat hierarchy of PHC: ‘For me, collaboration only works when I know what the other person can do. And I know where my limits are. That means, whenever I notice that this could also be in the area of the other person, who could support or knows more than me, then I ask for their advice’. Orthoptist self-employed
Additionally, several other competences emerged as vital for effective IPC. One participant emphasized that ‘coordination is very important; it’s about coordinating with all PGs’. Office assistants PHCU
Moreover, the ability to communicate effectively within the team is crucial. A participant pointed out that, ‘(…) social communication skills are essential. In a primary care team, everyone must find their place’. Occupational therapist PHCU This reflects the necessity for team members to understand their own roles and how they interact with one another.
Furthermore, participants stressed the importance of being open to learning from others. One participant articulated that there must be ‘(…) a process within us to learn to let go of certain things and truly utilize the competencies of other PGs’. General practitioner PHCU This mindset encourages flexibility and the effective use of diverse skills within the team.
Overall, networking abilities and social skills are essential for working in PHC. Participants emphasized the need for flexibility in scheduling common time with colleagues and the willingness to give and receive constructive criticism, highlighting the collaborative spirit in PHC settings.
Previous and present training content
This subcategory includes participants’ insights on past and present training content for IPC, specifically in PHC.
When asked about their preparedness for IPC in PHC, participants had varying responses, even within the same PG. Dietitians, midwives, occupational therapists, and psychotherapists reported minimal preparation during training but gained IPC experience through internships and courses like ‘casework’, where students from all health and social sciences programmes collaborated on cases. Occupational therapists, however, admitted that it ‘made up a very small proportion’. Occupational therapy PHCU
Summing up, study participants wished for a different and extended preparation for IPC in PHC in the areas of cooperation, communication and interdisciplinary connection:
‘What I think that should be integrated into the training, especially with regard to PHC, is that one learns about interdisciplinary collaboration and, above all, what the other PGs are allowed to do’. Biomedical analytics teaching institution
Discussion
This study qualitatively explored the perspectives of 15 PGs from the health care and social sector on IPC in Austrian PHC. The participants from the 15 mono-professional FGIs gave insights to the current respective setting for IPC of their PG as well as to their perceived professional relationships. Thereof, starting points for the development of specific educational and training content were deducted.
Setting for IPC
The representation of the PGs included in this study varies in Austrian PHC and specifically in PHCUs.
Those PGs already part of the PHCUs report various interprofessional activities across the therapeutic and patient support spectrum. This mirrors countries like the United States and Israel where PHC teams provide prevention work (Fowler et al., Reference Fowler, Garr, Mager and Stanley2020) and home visits (Williams et al., Reference Williams, Brooks-Russell, McManus, Yost, Olds and Tung2021) on an interprofessional basis.
The professionals describe that their everyday working life in a PHCU differs significantly from other work contexts, both in structural processes and in patient-related activities. Working in PHCUs poses unique working circumstances compared to other health and social sectors (Virtanen et al., Reference Virtanen, Oksanen, Kivimäki, Virtanen, Pentti and Vahtera2008; Kalandyk et al., Reference Kalandyk, Penar-Zadarko and Krajewska-Kułak2016; Ashley et al., Reference Ashley, Halcomb, Brown and Peters2018; Burgmann et al., Reference Burgmann, Huter, Mayerl, Paier-Abuzahra and Siebenhofer2021). These specific circumstances also impact collaborative practices and are part of various IPC models and dimensions (Canadian Interprofessional Health Collaborative, 2010; van Dongen et al., Reference van Dongen, Lenzen, van Bokhoven, Daniëls, van der Weijden and Beurskens2016; Interprofessional Education Collaborative, 2016; Sangaleti et al., Reference Sangaleti, Schveitzer, Peduzzi, Zoboli and Soares2017; Seaton et al., Reference Seaton, Jones, Johnston and Francis2020).
Although not the study’s focus, the professionals repeatedly noted the benefits of PHCUs for patients, aligning with previous research focusing on the patient perspective of PHCUs in different countries (Derriennic et al., Reference Derriennic, Barais, Le Goff, Fernandez, Le Borne and e Reste2021; Rawlinson et al., Reference Rawlinson, Carron, Cohidon, Arditi, Hong, Pluye, Peytremann-Bridevaux and Gilles2021; Wang et al., Reference Wang, Zhang, Loban and Wei2023; Sathyananda et al., Reference Sathyananda, Krumeich, Manjunath, Rijk and Schayck2024).
The participants from all those professions that are not yet involved in PHCUs in Austria expressed that they would like to be involved in this setting, in accordance with official statements of the national professional associations (Jaksch, Reference Jaksch2020; MTD-Austria, 2023; MTD-Austria, 2024; Rausch et al., Reference Rausch, Birklbauer, Federolf, Hecksteden, Hofmann, Niebauer, Reich, Rieder, Ruin, Scharhag, Seebacher, Treff, Tschan, Wessner, Würth and Müller2024).
The following specific role models were mentioned:
In Denmark, the integration of biomedical scientists in PHC settings includes tasks such as conducting tests and providing diagnostic support, sometimes through mobile laboratory buses equipped to bring services closer to patients (OECD, 2017; Healthcare Denmark, 2023). In Norway they are also directly involved in PHC: they advise health care providers on the right choice of methods, equipment and parameters in clinical laboratory diagnostics during laboratory visits, but also via telephone and email (Luxbacher, Reference Luxbacher2019).
Orthoptists also expressed the wish of being a part of PHC and PHCUs specifically, working preventively in eye care teams like those in the United Kingdom (Resch, Reference Resch2021). Primary eye health care teams could drastically reduce the burden on ophthalmologists and improve access and care quality (Patel, Reference Patel2021).
For radiography and medical training therapy, no specific role models were discussed. Nonetheless, radiographers, for instance, perform essential imaging for diagnosis and treatment, including history-taking and quality control. Integrating them into PHCUs could enable on-site or mobile imaging, reducing patient transport needs and improving access for those with mobility limitations (Jaksch, Reference Jaksch2020) Direct access to imaging in PHC may facilitate earlier diagnosis of cancer and other conditions. Limited evidence suggests that such access from primary care shortens imaging wait times and enhances both patient and general practitioner satisfaction (Black et al., Reference Black, Lyratzopoulos, Vincent, Fulop and Nicholson2023).
Recently, a study protocol was published to evaluate how integrating medical training therapists into the primary care team can improve patient uptake and adherence to physical activity, especially among those with NCDs (Wattanapisit et al., Reference Wattanapisit, Hemarachatanon, Somrak, Manunyanon, Wattanapisit, Amornsriwatanakul, Katewongsa, Sangkaew, Vichitkunakorn, Lee, Ramdzan, Salim, Ng and Stoutenberg2024).
Furthermore, PGs already included in PHCUs, i.e., midwives and nurses expressed a desire to expand their roles, aligning with their national professional associations’ statements (Österreichisches Hebammengremium, 2023; Meistler, Reference Meistler2024). Midwives work in seven of the 50 PHCUs in Austria (Primary Care Platform, 2022) and feel their role is too limited, advocating for stronger representation in PHCUs for the benefit of women and families. Continuity of care by a midwife has been shown to increase women’s satisfaction from antenatal until postpartum care (Della Forster et al., Reference Della Forster, McLachlan, Davey, Biro, Farrell and Gold2016), leading to positive health outcomes for women and newborns (Sandall et al., Reference Sandall, Fernandez Turienzo, Devane, Soltani, Gillespie, Gates, Jones, Shennan and Rayment-Jones2024).
Participants noted that nursing roles in Austrian PHC are evolving, as corroborated by national legislative developments (Parlament Österreich, 2024). Although already seen as crucial in the functioning of a PHCU, the wish to develop ‘nurse-led clinics’ was expressed in the nurses’ FGI and the one with general practitioners. This could lead to a higher quality of life and less stress, especially for chronically ill patients, e.g., for those with cancer (Molassiotis et al., Reference Molassiotis, Liu and Kwok2021).
These reported trends align with international developments, where PGs seek to expand their competencies in response to increasing demands for high-quality healthcare. Extending the scope of practice for allied health professionals can be a cost-effective strategy to enhance patient outcomes and meet the needs of an ageing population in PHC (Saxon, Gray & Oprescu, Reference Saxon, Gray and Oprescu2014; Leong et al., Reference Leong, Teoh, Fun and Lee2021).
Professional relationships
During the 15 FGIs, several aspects were listed that could sustain and facilitate IPC in PHC, corroborated by literature (Canadian Interprofessional Health Collaborative, 2010; Morgan et al., Reference Morgan, Pullon and McKinlay2015; Pullon et al., Reference Pullon, Morgan, Macdonald, McKinlay and Gray2016; Luxbacher, Reference Luxbacher2019; Brown et al., Reference Brown, Mulder, Clark, Belsito and Thorpe2021; Rawlinson et al., Reference Rawlinson, Carron, Cohidon, Arditi, Hong, Pluye, Peytremann-Bridevaux and Gilles2021; Seaton et al., Reference Seaton, Jones, Johnston and Francis2021; Wei et al. Reference Wei, Horns, Sears, Huang, Smith and Wei2022): respect, sense of belonging, time for networking, communication and sharing, shared space and channels of communication, role clarity, appreciation and knowledge of respective professional roles; leadership that promotes teamwork and orientation towards the relationship with patients.
On the other hand, participants reported that colleagues often don’t fully understand their roles, which can lead to undervaluing their expertise. Additionally, hierarchical dynamics, particularly with doctors’ authority, can limit equal collaboration and undermine contributions from other PGs. Lack of role clarity, limited specific training, and hierarchical issues have all been identified as barriers to effective IPC in PHC (Rawlinson et al., Reference Rawlinson, Carron, Cohidon, Arditi, Hong, Pluye, Peytremann-Bridevaux and Gilles2021; Wei et al., Reference Wei, Horns, Sears, Huang, Smith and Wei2022).
As the study participants do not feel optimally prepared for IPC in PHC and PHCUs specifically, almost all interviewed PGs expressed the desire of specifically designed training content, concentrating on these topics: the unique structure of Austrian PHCUs, the roles of all involved PGs, and conflict management. From systemic and organizational viewpoints the development of a proprietary specific training programmes should consider that (a) access should be possible for all PGs regardless of their level of academic training, (b) the programme should work both as a module within the primary professional training and as continued training; (c) a modular design would reflect the different prerequisites and interests of the participants, as well as their time possibilities, and (d) in view of the limited time resources of the participants (both in the scenario of training and further education), the programme should convey the content as efficiently and effectively as possible.
Research highlights that successful IPC relies on high-level IPC education, which fosters IPC-competent practitioners through interprofessional curriculum components and hands-on learning experiences (Robben et al., Reference Robben, Perry, van Nieuwenhuijzen, van Achterberg, Rikkert and Schers2012; Guraya & Barr, Reference Guraya and Barr2018; Simons, Goossensen & Nies, Reference Simons, Goossensen and Nies2022; Wei et al., Reference Wei, Horns, Sears, Huang, Smith and Wei2022; Ruebling et al., Reference Ruebling, Eggenberger, Frost, Gazenfried, Greer, Khalili, Ochs, Ronnebaum and Stein2023). Additionally, building a resilient and adaptable health workforce requires developing transversal skills, such as person-centred communication, interprofessional teamwork, adaptive problem-solving, and digital proficiency, to effectively meet the complex demands of modern healthcare (Maeda & Socha-Dietrich, Reference Maeda and Socha-Dietrich2021).
Strengths and limitations
This study is the first to qualitatively examine IPC in Austrian PHC. A key strength is the integration of perspectives from professionals working in PHCUs, educational institutions and professional associations. It also included voices from PGs involved in PHC but not yet active within PHCUs, offering a holistic and forward-looking perspective on PHC.
However, there were some limitations. No direct observation methods were used, which are valuable for analysing IPC (Morgan et al., Reference Morgan, Pullon and McKinlay2015; Seaton et al., Reference Seaton, Jones, Johnston and Francis2021). Not all FGIs included participants from all relevant settings, and the number of participants varied, leading to somewhat different discussion dynamics. Since the FGIs were conducted in a mono-professional setting, comparisons between PGs were only possible during the data analysis.
Despite these limitations, the study provides valuable qualitative insights for future quantitative research on IPC in Austrian PHC, specifically in the developing PHCU setting, and for developing targeted training programmes. Further research should also evaluate patients’ experiences with the IPC in Austrian PHCUs, as this perspective was not directly surveyed in this study.
Conclusion
This study showed that Austrian health care and social professionals aim to get more involved in PHC and PHCUs specifically. While they see opportunities, they also recognize challenges for their PGs. However, they feel unprepared for the effective IPC. Specific training is desired focusing on the unique requirements of Austrian PHCUs to enhance the beneficial collaboration between multiple PGs in the increasingly important setting. The overarching goal is to provide optimal healthcare for patients and a supportive working environment for professionals.
Moving forward, a representative quantitative study should be conducted in Austria to validate the qualitative results and weigh the key factors for successful IPC, highlighting any differences among PGs.
The findings of this study are applicable not only to Austria but contribute to an international understanding of IPC. However, a detailed comparison between different countries is challenging due to significant variations in healthcare system structures and regulations.
Data availability statement
The data in the original language underlying this article will be shared on reasonable request to the corresponding author.
Acknowledgements
We express our gratitude to all our interview partners for their time and valuable input. We thank G.J. Oostingh and A. Schuster for the critical proofreading of our manuscript.
Funding statement
This study was funded by an institutional grant of the Salzburg University of Applied Sciences (grant number 7088-015).
Competing interests
The authors declare none.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional guidelines on human experimentation, in our case the Institutional Ethics Committee of the Salzburg University of Applied Sciences and with the Helsinki Declaration of 1975, as revised in 2008. Written informed consent was obtained from all subjects.





