Introduction
Maternal-infant bonding is one of the bedrocks of human relationships and an important predictor of child adjustment (Johnson, Reference Johnson2013). This early bond has been systematically shown to be negatively associated with maternal perinatal stress and postpartum depression and positively with social support (Afolabi et al., Reference Afolabi, Bunce, Lusher and Banbury2020; Balaji et al., Reference Balaji, Claussen, Smith, Visser, Morales and Perou2007; Crockenberg, Reference Crockenberg1981; Hopkins et al., Reference Hopkins, Miller, Butler, Gibson, Hedrick and Boyle2018; Jacobson & Frye, Reference Jacobson and Frye1991; Levitt et al., Reference Levitt, Weber and Clark1986; Yesilcinar et al., Reference Yesilcinar, Yavan, Karasahin and Yenen2017; Ziv & Cassidy, Reference Ziv and Cassidy2002), vaginal delivery (Sockol et al., Reference Sockol, Battle, Howard and Davis2014), and with factors promoting bonding such as breastfeeding (Johnson, Reference Johnson2013) and nulliparity (Barclay et al., Reference Barclay, Everitt, Rogan, Schmied and Wyllie1997; Harwood et al., Reference Harwood, McLean and Durkin2007; Lupton, Reference Lupton2000). As a result of COVID-19, changes in surroundings and living conditions may amplify maternal stress (Ostacoli et al., Reference Ostacoli, Cosma, Bevilacqua, Berchialla, Bovetti, Carosso, Malandrone, Carletto and Benedetto2020; Werchan et al., Reference Werchan, Hendrix, Ablow, Amstadter, Austin, Babineau, Anne Bogat, Cioffredi, Conradt, Crowell, Dumitriu, Fifer, Firestein, Gao, Gotlib, Graham, Gregory, Gustafsson, Havens, Howell, Humphreys, King, Kinser, Krans, Lenniger, Levendosky, Lonstein, Marcus, Monk, Moyer, Muzik, Nuttall, Potter, Salisbury, Shuffrey, Smith, Smith, Sullivan, Zhou, Thomason and Brito2022). Social distancing regulations were enforced in order to contain the spread of the virus, including distance limitations on mobility as well as limitations on gathering size, and hospital visitations were restricted. The availability of face-to-face assistance for postpartum mothers and infants was reduced, especially from older loved ones such as parents and grandparents, who were advised to stay home and avoid face-to-face social interactions. Many individuals had been staying at home on unpaid leave or working from home, which may be beneficial if both parents are able to be involved and supportive but may also be detrimental in the cases of a stressful relationship or even domestic violence (Kourti et al., Reference Kourti, Stavridou, Panagouli, Psaltopoulou, Spiliopoulou, Tsolia, Sergentanis and Tsitsika2023). Therefore, increased stress and reduced social support may have doubly hindered the development of positive maternal-infant bonds.
To control COVID-19 and ensure mothers’ and infants’ safety, governments and public health organizations advised that facilities should consider a temporary maternal-infant separation in different wards and under medical testing and supervision. If the separation was unwanted, social distancing measures and respiratory hygiene measures between mother and infant were enforced (Bartick, Reference Bartick2020). In Israel, as of March 2020, these changes included regulations limiting one companion per parturient and limitation of medical staff per COVID-19-suspected parturient (Ministry of Health, 2020). These guidelines, especially ones leading to mother-infant separation or distancing, might have prevented or impeded bonding behaviors such as breastfeeding, that may have disrupted the development of the early mother–child relationship (Gribble et al., Reference Gribble, Marinelli, Tomori and Gross2020). Health organizations around the world have issued several statements concerning the adverse outcomes of this policy for mother-infant’s relationships (Poon et al., Reference Poon, Yang, Kapur, Melamed, Dao, Divakar, McIntyre, Kihara, Ayres-de-Campos, Ferrazzi, Renzo and Hod2020, UNICEF, Reference UNICEF2020).
Considering the stressful changes in the conditions of delivery and postpartum period due to the COVID-19 pandemic, it is plausible that these may have an effect on maternal-infant bonding and attachment. Adaptation of infants to a pandemic mostly depends on the impact of illness and stress on their caretakers and the availability of these caretakers to provide infants with sufficient psychosocial needs (Murray, Reference Murray2010). Indeed, birth under the COVID-19 pandemic has been shown to be disruptive of maternal-infant bonding (Liu et al., Reference Liu, Hyun, Mittal and Erdei2021; Mayopoulos et al., Reference Mayopoulos, Ein-Dor, Dishy, Nandru, Chan, Hanley, Kaimal and Dekel2021). The consensus is that social support plays a crucial role in enhancing maternal well-being and serves as a protective factor for both maternal mental health and the bonding between mothers and infants(Hung & Chung, Reference Hung and Chung2001; Ohara et al., Reference Ohara, Okada, Aleksic, Morikawa, Kubota, Nakamura, Shiino, Yamauchi, Uno, Murase, Goto, Kanai, Masuda, Nakatochi, Ando and Ozaki2017). Social support encompasses both instrumental support and emotional support, with expectations often placed on mothers’ own mothers and partners to provide these forms of support (Negron et al., Reference Negron, Martin, Almog, Balbierz and Howell2013).
Despite these recommendations, little is known about the impact of specific COVID-19-related experiences among postpartum mothers, and possible mitigating factors. This study aimed to investigate the development of maternal-infant bonding in times of the COVID-19 pandemic, and its relation to stressful experience, including maternal exposure to, experience of, and fear of COVID-19. While nulliparity, mode of delivery, and bonding behaviors such as zero separation and breastfeeding have all been suggested as protective, our focus was on potential moderation by social support, which was compromised during the pandemic due to social distancing and lockdown regulations. Israel, characterized by a Jewish majority and a significant Arab minority, exhibited variations in the mental health of pregnant women during the pandemic. Research indicated that Arab pregnant women experienced higher levels of anxiety and distress in comparison to their Jewish counterparts. Consequently, being of Arab descent emerged as a potential risk factor for maternal mental health issues, which could be related to maternal-infant bonding (Taubman–Ben-Ari et al., Reference Taubman-Ben-Ari, Chasson, Abu Sharkia and Weiss2020). We hypothesized that typical and COVID-19-related risk factors, as well as typical protective factors, measured following birth would show negative and positive relationships, accordingly, to subsequent bonding. Moreover, we hypothesized that the relationship of COVID-19-related risk factors to bonding would be moderated by the protective effects of social support, so that higher social support would attenuate the negative relationship between COVID-19-related risk factors and bonding.
Methods
Participants and procedure
This was a longitudinal, multicenter study that was conducted at three university-affiliated medical centers in Israel: Hillel Yaffe Medical center (HYMC), Meir Medical Center (MMC) and Wolfson Medical Center (WMC). The study was conducted between March 10 and December 8 2020. The initial assessment, referred to as “Time 1” (T1), occurred approximately 10 weeks after childbirth, coinciding with the first lockdown period in Israel, and “Time 2” (T2) was conducted 6 months after childbirth and following the conclusion of the second lockdown period in Israel. The T1 survey included all detailed questionnaires listed, while the T2 survey included all questionnaires except for the demographic questionnaire.
Overall, 1,462 women delivered during the duration of the study at the three participating medical centers. During T1, 1,079 (74%) were contacted by phone. In total, 774 (53%) consented to answering the online questionnaires, and 429 (29%) answered over 70% of the questionnaires and were later re-approached in T2. Of them, 377 (87.9%) gave their consent, and 246 completed at least 70% of the T2 questionnaires and thus entered the analysis. Demographic and clinical information regarding the final sample can be found in Table 1.
Table 1. Sample demographics and study variables
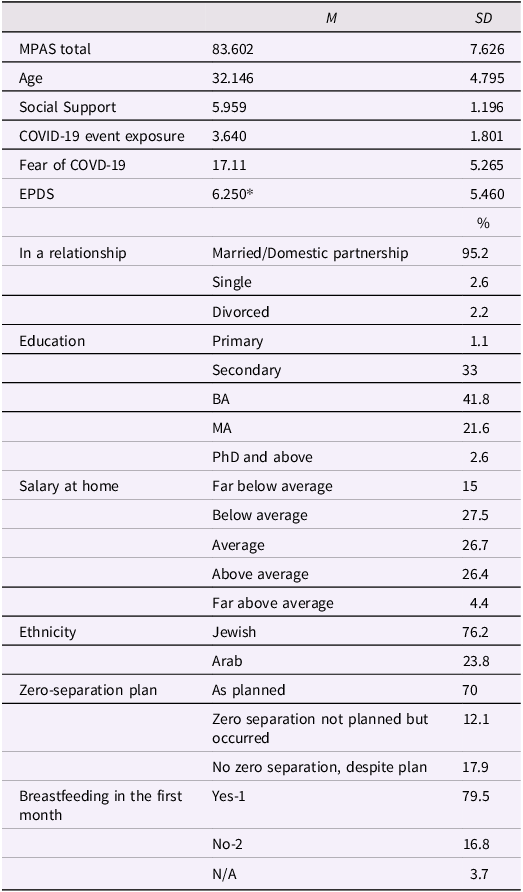
Note: COVID-19 = coronavirus disease 19; EPDS = Edinburgh Postpartum Depression Scale. *12.4% of the women scored ≥ 13, considered a likely depression diagnosis.
It is important to note that, during T1, lockdown regulations included considerable restrictions on freedom of movement, and shutdown of all non-essential services including medical services. COVID-19 regulations during childbirth included limiting one companion per mother, extensive protective equipment for all medical staff assisting the delivery, limitation of medical staff per COVID-19-suspected mother, facial mask-wearing by mothers during all physical contact with the infant, and consideration of an enforced zero-separation policy for infants and mothers, meaning that mothers and infants are advised to stay together at all times (Ministry of Health, 2020). From the beginning of May 2020 and after T1, the pandemic decreased, the lockdown was released, and schools reopened. For many people, life was “back to normal.” However, gradually the pandemic escalated until the second lockdown was initiated on September 18, 2020, for a period of three weeks. This lockdown was less strict, allowing considerable freedom of movement and with many services remaining open. The Institutional Review Board of each center approved the study (HYMC-20-0079, MMC-0169-20, WMC-143-20). Participants were recruited virtually, by a team of Hebrew and Arabic speaking physicians and medical students. Mothers who were under the age of 18 or who delivered earlier than 34 gestational weeks were excluded from the study. Informed consent was obtained both telephonically and electronically before data were collected from the participants. After consent, a text message was sent to each participant, containing a link to an online questionnaire in Hebrew or Arabic, according to the participant’s preference.
Measures
Demographic questionnaire
The demographic questionnaire included items such as age, gender, ethnicity, marital status, socioeconomic status, and level of education. Questions about zero-separation policy were added to this questionnaire as mothers were asked whether they experienced zero separation at the hospital following birth (meaning they stay together at all times) and whether they had planned for zero-separation pre-birth. The variable was coded ordinally according to hypotheses so that arrangements as planned was coded as having the highest value and zero separation despite planned separation was coded as the second-lowest value, with separation despite plans not to separate as the lowest value. Separation plans were changed in accordance with specific medical center COVID-19 policies. Moreover, obstetric and pregnancy history, course of labor and course of delivery data were all retrieved from the computerized perinatal databases of each medical center.
COVID-19 exposure
This 14-item questionnaire was compiled by authors (see in Supplement 1) in order to detect exposures to COVID-19-related life events, for example “I was in contact with someone who was infected by the Coronavirus.” Each participant was asked to indicate whether or not she experienced such an event. The number of events was then summed up (score 0–14).
Fear of COVID-19 scale (FVC-19S) (Ahorsu et al., Reference Ahorsu, Lin, Imani, Saffari, Griffiths and Pakpour2022)
The FCV-19s is a self-report validated scale for the assessment of fear of COVID-19. To note, this questionnaire was also validated for the Hebrew language (Tzur Bitan et al., Reference Tzur Bitan, Grossman-Giron, Bloch, Mayer, Shiffman and Mendlovic2020). The scale consists of seven items regarding the fear response to COVID-19, for example: “I am afraid of losing my life because of the coronavirus.” Participants are requested to rate on a five-point Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree), with a total score of 7–35, a higher total score indicating greater fear of COVID-19. The questionnaire has a good internal validity (alpha Cronbach 0.82) and in the current study the scale showed an internal consistency of 0.84.
Edinburgh postnatal depression scale (EPDS) (Murray & Cox, Reference Murray and Cox1990)
Postpartum depression symptoms were evaluated using the validated EPDS questionnaire. This questionnaire is composed of 10 items, scored by using a four-point Likert scale (0–3). In our sample, the internal consistency was found to be 0.87, in line with previous findings (Murray & Cox, Reference Murray and Cox1990).
Multidimensional scale of perceived social support (MSPSS) (Zimet et al., Reference Zimet, Dahlem, Zimet and Farley1998)
The 12-item MSPSS is a self-report scale for the assessment of subjective social support. The three subscales include support by family, friends, and significant others, and each subscale is represented by 4 items, for example: “There is a special person who is around when I am in need.” Participants are requested to respond using a seven-point Likert scale ranging from 1 (very strongly disagree) to 7 (very strongly agree), a higher total score indicating greater subjective social support. The questionnaire has good validity (alpha Cronbach 0.88) and in the current study the scale showed an internal consistency of 0.92.
Maternal postnatal attachment scale (MPAS) (Condon & Corkindale, Reference Condon and Corkindale1998)
The 19-item MPAS is a self-report scale for the assessment of mother-infant bonding, which was found to be among the most robust measures for postnatal maternal-infant bonding assessment (Wittkowski et al., Reference Wittkowski, Vatter, Muhinyi, Garrett and Henderson2020). The MPAS includes items such as ”Over the last two weeks I would describe my feelings for the baby as 1 (dislike) to 5 (intense affection)” ; “When I am caring for the baby, I get feelings of annoyance or irritation,” scored 1 (very frequently) to 5 (never); and “When I have to leave the baby I usually feel rather 1 (relieved) to 5 (sad).” All responses are recoded to represent a score of 1 (low bonding) to 5 (high bonding), a lower total score indicating a more problematic mother-infant bond. In the current sample alpha Cronbach was .788, similar to initial validation where it was .78.
Statistical analyses
Missing data patterns were analyzed using Little’s completely at random test for all variables used, and assumption of randomness was not disrupted. Sufficient complete data was obtained at both timepoints for reliable analysis of completer only data, as randomness precludes bias when using this strategy. Reported data in the current manuscript therefore includes original sample, for increased face validity and brevity, however when multiple imputations were employed this did not change results (for detailed account see Supplement 2).
Hierarchical regression analyses were conducted with demographics (household income, ethnicity, age, level of education and relationship status) included in the first step, factors typically associated with bonding and attachment (breastfeeding in the first days following delivery, parity, and mode of delivery as recorded in the hospital, zero -separation status at hospital as reported by mothers, MPSS score of social support) were included in the second step, and COVID-related factors (FVC-19S and instances of exposure to COVID-related stressors) were entered in the third step. In the fourth and final step, two-way interaction variables created from multiplication of fear of COVID, and impact of COVID, by social support, were entered, to test for possible moderation effects. Tests of multicollinearity using the most stringent threshold (VIF < 3) did not reveal social support to be redundant with any of the variables measured at T1. Dependent variables were overall MPAS scores During T2, 6 months after childbirth. In order to interpret interactions found to be significant, Hayes PROCESS1 package was employed to conduct Johnson-Neyman regions of significance analyses. Additionally, a median split of the moderator was employed, with group-mean centralized independent variables used to explore simple slopes for the relationship between the moderated dependent variable and the independent variable within the two split groups.
Results
All stepwise models significantly predicted later MPAS scores (see Table 2). Each step added significantly to the variance explained in subsequent MPAS scores, apart from the third step (COVID-19 related variables; see Table 3).
Table 2. Omnibus test for the regression model
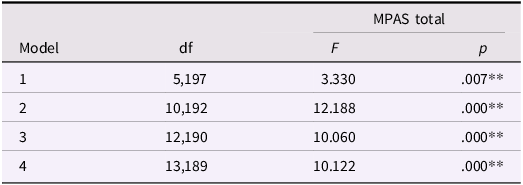
Note: COVID-19 = coronavirus disease 19; MPAS = Maternal postnatal attachment scale; MSPSS = Multidimensional Scale of Perceived Social Support. **Correlation is significant at the 0.01 level (2-tailed). *Correlation is significant at the 0.05 level (2-tailed).
Table 3. Stepwise change statistics for the regression

Note: **Correlation is significant at the 0.01 level (2-tailed). *Correlation is significant at the 0.05 level (2-tailed).
When more closely examining individual coefficients within the steps, several independent variables evinced differing patterns in their relationships with the dependent variables (for full statistical account see Table 4): Within the demographic variables, with all other variables held constant, higher education was associated with lower overall score on the MPAS. No other variables predicted MPAS scores.
Table 4. Stepwise coefficient statistics for the regression model
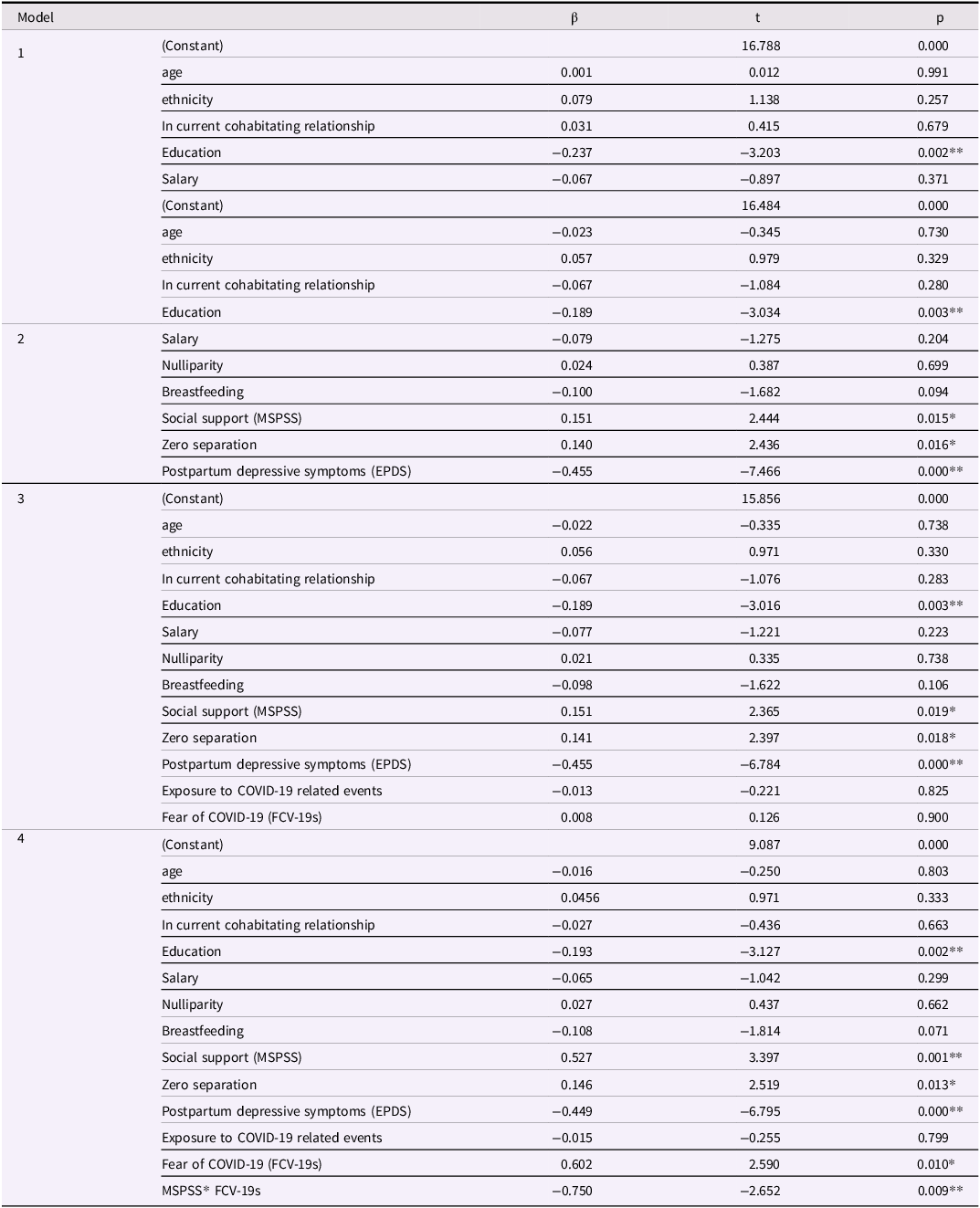
Note: COVID-19 = Coronavirus Disease 19. **Correlation is significant at the 0.01 level (2-tailed). *Correlation is significant at the 0.05 level (2-tailed).
Of the psychosocial independent variables, only zero separation, EPDS and MSPSS showed the expected association with MPAS scores when demographics and COVID-related variables were held constant (see steps 2 and 3, Table 4). Breastfeeding and parity were not significantly associated with MPAS within this model.
Of the COVID-related independent variables, mere exposure to COVID-related events was not associated with MPAS scores when other variables were held constant. FVC-19S was not significantly associated with the MPAS in the third step, but positively and significantly predicted MPAS in the fourth step, where moderation by social support was accounted for. Furthermore, it was found that none of the mothers had contracted COVID-19 in T1, and only five of the participants had contracted COVID-19 by T2. Infected mothers’ exclusion did not change the results and these women were included in analyses.
As moderation effect (MPAS interaction with Fear of COVID-19) was significant, a regions of significance analyses was conducted. This identified that the FVC-19S value at which the change in slope occurs is 5.9125, with 33.490% of the observed measurements falling below this threshold and 66.509% falling above it. Additionally, the relationship of FVC-19S with MPAS was examined in two groups: below-median and above-median MSPSS. Simple slopes for the relationships revealed that, for the group with below-median MSPSS scores (low support, N = 79), there was no significant relationship between FVC-19S at T1 and MPAS at T2 (r = .098, p = .303). However, for the group with above-median MSPSS scores (high support, N = 61), FVC-19S at T1 evinced a significant negative relationship with MPAS score at T2 (r = −.331, p = .000), accounting for the effect in the fourth step (see Fig. 1 for relationship plot).
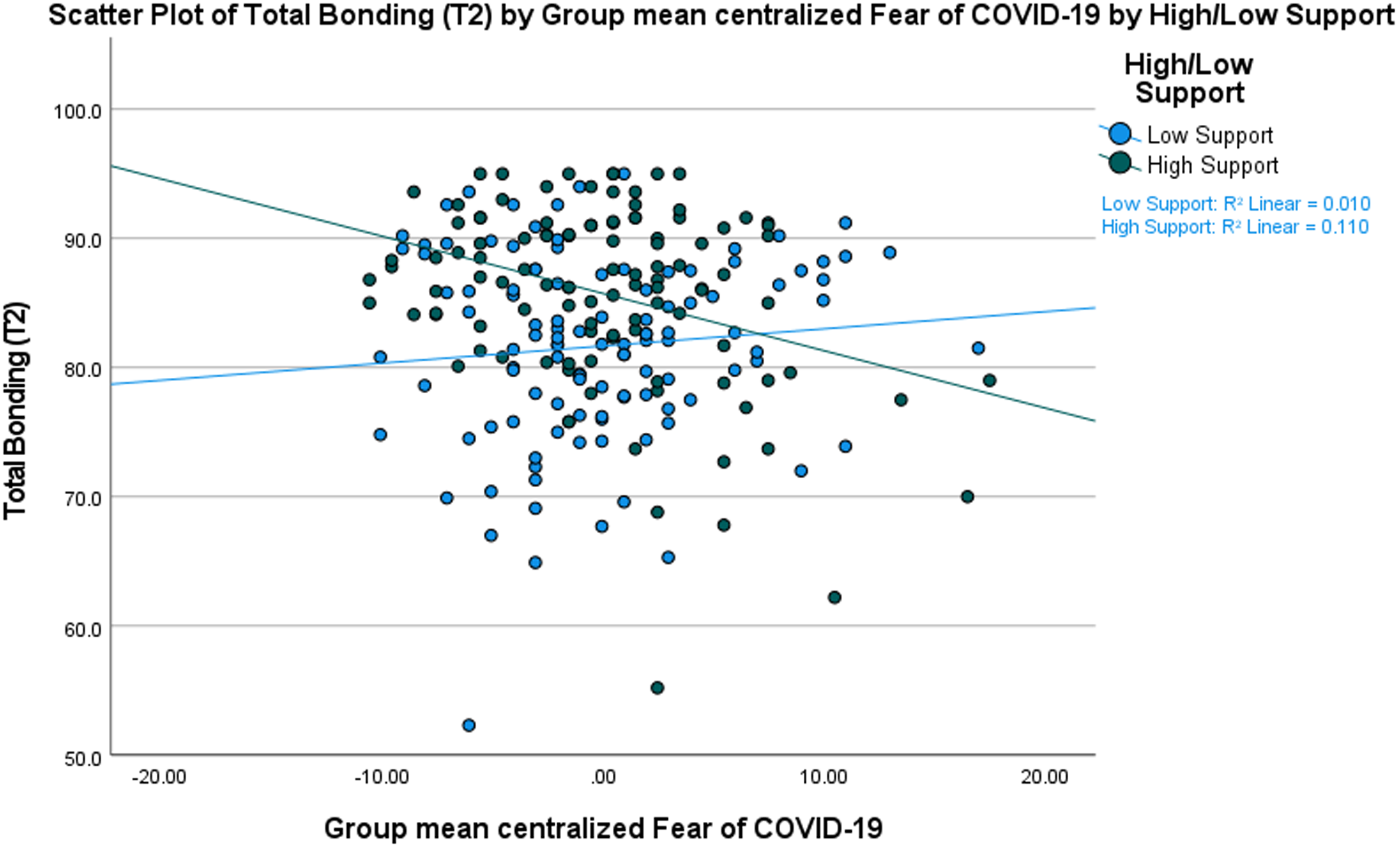
Figure 1. Relationship between fear of COVID-19 and bonding by level of support.
*Note: COVID = coronavirus disease; high/Low support groups determined by scoring above or below median on the social support scale. T2 = Time 2 (approximately six months later than measures of dependent and moderating variables).
In order to verify reliability of results, all analyses were repeated with T1 MPAS as dependent variable. The results were replicated (see Supplement 3).
Discussion
This study aimed to explore how demographic factors, psychosocial elements, and experiences related to COVID-19 are linked to maternal-infant bonding. Additionally, our goal was to assess the role of social support as a protective factor mitigating the potentially adverse effects of COVID-19 on subsequent maternal-infant bonding. Our hypotheses posited that both conventional risk factors, including those associated with COVID-19, and standard protective factors measured post-birth would exhibit negative and positive correlations, respectively, with subsequent maternal-infant bonding. Additionally, we postulated that mothers with social support would experience a safeguarding effect on maternal-infant bonding, mitigating the impact of risk factors specific to COVID-19.
Regarding common risk and protective factors, and in line with the literature, a higher maternal educational level was found to be related to a less positive maternal-infant bonding, (Figueiredo et al., Reference Figueiredo, Tendais and Dias2014), and there was no difference in overall mother-infant attachment between Jewish and Arab mothers (Zreik et al., Reference Zreik, Oppenheim and Sagi-Schwartz2017). Also consistent with the literature, perceived maternal social support was related to higher maternal-infant bonding (Johnson, Reference Johnson2013) and postpartum depression symptoms was related to reduced maternal-infant bonding (Lehnig et al., Reference Lehnig, Nagl, Stepan, Wagner and Kersting2019). Breastfeeding was not found to be associated with maternal-infant bonding, which adds to the mixed findings regarding this relationship (Britton et al., Reference Britton, Britton and Gronwaldt2006; Else-Quest, Reference Else-Quest2003) as was the case for parity (Lehnig et al., Reference Lehnig, Nagl, Stepan, Wagner and Kersting2019).
COVID-19 and maternal-infant bonding
Just as COVID-19 changed many aspects of mothers’ birth plan (Gildner & Thayer, Reference Gildner and Thayer2020) it was found, as expected, that the changes in zero-separation plans predicted reduced mother-infant bonding, especially if separation was unwillingly enforced. This is aligned with the literature, in which birth plan changes during COVID-19 had a negative effect on maternal mental health (Liu et al., Reference Liu, Koire, Erdei and Mittal2022).
We found that the mere exposure to COVID-19-related events was not significantly related to maternal-infant bonding. This is aligned with previous studies in which exposure to traumatic life events such as war or natural disasters, was not related to maternal-fetal bonding (Punamäki et al., Reference Punamäki, Isosävi, Qouta, Kuittinen and Diab2017) or infant temperament (Tees et al., Reference Tees, Harville, Xiong, Buekens, Pridjian and Elkind-Hirsch2010).
The fear of COVID-19, in isolation, was not identified as a factor linked to maternal-infant bonding. However, when considering the interaction with social support, this interplay was found to be statistically significant and only partially fit our hypothesis; Mothers with higher levels of social support exhibited lower levels of maternal-infant bonding when experiencing heightened fear of COVID-19. One plausible explanation for this correlation is that social support may be associated with anxiety, as individuals with anxiety often seek increased social support as a coping mechanism. Consequently, it is conceivable that mothers reporting high social support may also be more prone to anxiety, and the interaction between heightened anxiety and fear of COVID-19 could better explain these findings than the direct influence of social support alone. It’s also important to consider that, although social support has generally been identified as a protective factor for maternal-infant bonding in prior studies, the dynamics change during a global pandemic. In a situation where, human interaction serves as the primary vector of infection, socializing becomes a potential health risk and, consequently, a potential stressor. While not all items of the scale used to assess social support require physical contact, some allude to it. In alignment with this, our study revealed that social support might function as a risk factor for maternal-infant bonding, particularly for mothers who harbored fears of COVID-19 infection. The pandemic introduces a unique social context, necessitating a nuanced examination of the relationship between maternal-infant bonding and social support, considering the novel factors brought about by the global health crisis.
The analyses showed that the relationship between bonding, support and fear was already apparent in T1, which is unsurprising considering the high stability of maternal-infant bonding (Capelli et al., Reference Capelli, Anceresi, Grumi and Provenzi2023), and suggests that these relationships are established early in the mother-infant relationship, exerting a lasting impact, and possibly mediating later bonding. Consequently, the results underscore the significance of early intervention, as the identified patterns suggest that addressing these factors early in the mother-infant relationship can be particularly crucial.
Limitations and implications
The current study benefits from being a longitudinal study, which allows results to reflect the pandemic’s long-lasting effect. This was also a multicenter study, which allowed a diverse population in terms of ethnicity, religion and socioeconomic status. Some of the maternal reports on demographics, obstetric and delivery data were cross-validated against their medical records, therefore this data can be considered as more accurate. Nevertheless, our study is not free of limitations. Most of the data was collected by self-report, therefore social desirability must be considered as a limitation of this study. Moreover, a substantial number of women did not answer the phone call for recruitment, creating a self-selection recruitment bias. We can assume that mothers who chose to participate in this study had the time and mental capacity to do so, while those who chose not to participate may have been suffering from possible socioeconomic or other difficulties. This is in line with the literature, as approaching postpartum mothers often results in low participation, especially in high-risk populations (Beasley et al., Reference Beasley, Ciciolla, Jespersen, Chiaf, Schmidt, Shreffler, Breslin, Bakhireva, Sanjuan, Stephen, Coles, Chambers, Kable, Leeman, Singer, Zellner, Morris and Croff2020; Lawton et al., Reference Lawton, Snowdon, Morrow, Norman, Denison and Hallowell2016). Due to our active recruitment process, this presents a smaller bias than studies recruiting through social media (Berthelot et al., Reference Berthelot, Lemieux, Garon-Bissonnette, Drouin-Maziade, Martel and Maziade2020; Lebel et al., Reference Lebel, MacKinnon, Bagshawe, Tomfohr-Madsen and Giesbrecht2020) and yet the current sample cannot be considered as a representative sample due to response bias. Finally, while the experience of contracting COVID-19 was included in the events reported by participants, it was a rare occurrence. To our knowledge, none had contracted the virus by T1, and between T1 and T2, only five women had contracted the virus. These women did not pose outliers, and their removal from the sample did not change the results of the analyses. Nevertheless, due to the limited number of cases, specific conclusions regarding the impact of COVID-19 infection on the tested model cannot be confidently drawn.
The current study’s results present important information concerning maternal-infant bonding during a global pandemic. The prevention of planned zero-separation was identified as a negative predictor of maternal-infant bonding. This implies that the epidemiological advantages of such a policy should be carefully balanced against the potential risks of disrupted bonding (Kim et al., Reference Kim, Feldman, Mayes, Eicher, Thompson, Leckman and Swain2011; Ranson & Urichuk, Reference Ranson and Urichuk2008). However, it’s crucial to note that the operationalization of the zero-separation variable in our study limited a comprehensive assessment of whether, for certain mothers, the absence of zero separation – whether it deviated from the initial plan or not – had varying effects.
These findings are valuable for both healthcare professionals and policy makers, as well as mothers’ families and loved ones. Particular attention should be directed at addressing the specific maternal stressor experienced by mothers, and providing adequate support accordingly, as per the mother’ needs and preferences. Thus, even though social support has been shown to be a positive factor for maternal-infant bonding, human interaction during such times makes this association more complex. In light of these results, healthcare professionals should still encourage social support for mothers in the postpartum period, engage in the best practices for mitigating potential postpartum depression, but also provide public health psychoeducation in order to try and minimize the fear of the pandemicgative impact of support for fearful mothers by examining non-anxiety provoking manner of support. Furthermore, if fear of social engagement is apparent, healthcare professionals and mothers’ loved ones should consider providing suitable maternal support through means of lesser physical contact, such as telephone or online connection. Finally, women with heightened fear of infection may face an increased risk of disruptions in bonding with their infants, necessitating closer follow-up and support. Considering that fear of infection is a potential component of additional peripartum mental disturbances like postpartum anxiety and OCD (Brockington et al., Reference Brockington, Macdonald and Wainscott2006; Field, Reference Field2018), which can further contribute to disrupted bonding (Tietz et al., Reference Tietz, Zietlow and Reck2014), it is essential to explore the interaction between such fear and social support in predicting subsequent bonding. This investigation should extend beyond the context of the pandemic to encompass a broader understanding of these dynamics in various peripartum mental health scenarios, particularly for mothers giving birth in times of stress, such as national or community emergencies. Future research endeavors should prioritize a deeper exploration of the characteristics of maternal fear of infection and its specific role in mediating or moderating the relationship between social support and bonding. Furthermore, there is a need for longitudinal studies that examine changes in maternal-infant bonding over time as the pandemic evolves. This longitudinal perspective can offer a nuanced understanding of the dynamic interplay between maternal well-being, social support, and the evolving circumstances of the pandemic. Additionally, these findings emphasize the need to investigate how other fears that may limit the buffering effects of typical resilience promoting factors: for example, fears regarding safety that may hinder health promoting behaviors and help seeking.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0954579424000853.
Author contribution
R. Gabbay-Benziv and L. Helpman are equally contributed to this work.
Funding statement
Dr Helpman’s work partly supported by Binational Science Foundation.
Competing interests
None.








