She was my last patient of a busy morning. Her morning call to our clinic – “my bleeding just won’t quit” – earned her the 11:40 a.m. slot, held open for patients with urgent matters. Her name was Susie.
As I would later learn, Susie was forty-six years old but hadn’t seen a nurse or doctor for seven years. She’d moved around from state to state a few times, been briefly employed in the service industry, but never stayed in one place long enough or earned enough to qualify for ongoing medical care. The last place she’d gone for care, a community health clinic in Colorado, had offered subsidized care, but funding issues had forced it to close.
Like many women, Susie never put Pap smear appointments high on her list. “I should go get a check-up,” she’d thought to herself. But such shoulds are rarely enough for patients like Susie to overcome daunting obstacles, including expensive medical fees, difficulty finding a clinic reasonably close to home, and perhaps most of all, the ability to trust a doctor with such an intimate procedure. Susie had been sexually assaulted. Women already feel vulnerable sitting on an exam table covered only by a sheet, knees spread apart for an internal pelvic examination – such vulnerability can be unimaginable for a woman who has experienced sexual violence.
Ideally, medical clinics offer patients a sense of safety, lessening their ambivalence about important exams. Our examination rooms in this clinic were small, equivalent to the interiors of Volkswagen vans. They held four-drawer, waist-high storage cabinets whose compartments hid pieces of equipment that could make women anxious, especially the metal speculums. Shaped like a duck’s bill, a speculum enables examiners to gently hold the vaginal walls in place for viewing the cervix – the vaginal opening to the uterus. The examination tables in our clinic were positioned to offer privacy, with the foot of the table farthest from the door. Fuzzy, colorful footies covering the stirrups where clients rested their feet provided extra padding and a sense of comfort.
Unfortunately, none of these factors made much difference in bringing Susie to our clinic – a woman from out of town, who, for a variety of reasons beyond her control, had waited too long to take advantage of the clinic’s preventative cancer care. It didn’t help that on that busy clinic day I’d had less opportunity to prepare for a patient like Susie. I’d only had time to read my medical assistant’s brief note, telling me that Susie had had “no medical care for seven years,” “irregular vaginal bleeding for three months,” and a “swollen right leg for six weeks.”
As I stood outside the exam room where Susie was waiting, my assistant approached me. “I did not want to write this on the chart,” she whispered, “but the room really smells.” I waited for more. “Susie told me she’s scared something is really wrong.”
When something is wrong, the patient is often the first to know.
The Moment Medical Training Rarely Prepares You For
As I cracked open the door to the exam room, the odor rushed out and overtook me. It was the smell of rottenness, the pungent smell of tissue dying. I knew that smell. As I listened to Susie’s story, I sensed the diagnosis even before doing the exam: cervical cancer.
The odor was not lost on Susie. She sat in a chair beside the exam table, her face red, her eyes toward the floor. It occurred to me that her shame was probably one reason she’d waited so long to go to a doctor, hoping her condition would improve before she had to have an embarrassing, traumatic examination, her vagina smelling of rottenness. But her condition did not improve. She told me she’d thought the smell came from bleeding for so long.
I asked Susie to tell me more about her leg swelling. Only swollen on the right. Gradually getting worse. No, no calf pain that might go with a blood clot but a generalized ache, especially at the end of the day. Maybe some back pain, worse, also, on the right side of the back.
As I listened, I carefully considered how to do this examination in the least distressing way. I was 99 percent sure I’d find a mass at the top of her vagina and that I’d want to take a biopsy to confirm what my heart and gut were so sure of already. Since Susie had been bleeding for so long, I’d also need to prepare for increased bleeding with the biopsy. Should the bleeding become heavy, I’d need to ask for help.
By now, Susie’s morning appointment had wound into early afternoon. I told her I’d need consent for the biopsies. Susie’s back stiffened, and she leaned forward in her chair. Her lips tightened, and I could see her brow knitting. As I got up to leave, I felt her anxiety. It had a presence, hanging thick in the air, mixing with the pungent odor.
Our clinic was on lunch hour, so I gathered up the necessary equipment by myself, and peeked into our medical provider room. My colleague, Samantha, was sitting there typing away. “Sammie, I’m about to do a biopsy on a woman, and I’m afraid she could bleed a lot. Can you please come in the room with me?” Sammie rose with a quick nod. As she opened the door to the room where Susie waited, we were again greeted by the odor. That odor. Sammie turned back to me with empathy and a knowing look in her eyes.
I introduced Sammie to Susie. While Susie lay on the exam table and I positioned her in the stirrups, Sammie held Susie’s hand and talked to her in her beautifully calming, Southern drawl. I placed the speculum in Susie’s vagina to see where the cervix sat. There it was, the source of the rotten flesh smell and some of Susie’s bleeding: a dark-brown, rough-edged growth in such stark contrast to the smooth, pink, healthy tissue surrounding it. Sammie and I made eye contact. With a subtle nod, I confirmed the diagnosis we’d both been expecting. I quickly obtained biopsies and applied silver nitrate to stop the bleeding from the missing tissue.
After removing the speculum, I conducted a bimanual examination on Susie’s pelvic structures, as well as the bones lining her pelvis. Using two fingers, I felt a hard, irregular mass occupying the upper region of Susie’s vagina. Placing one hand on her abdomen, I could feel the mass extending to the bones bordering the pelvis on the right side. I knew her tumor had likely spread beyond her cervix and her vagina. It had also cut off the lymph channels draining liquid out of the leg, which explained the swelling. As I finished the exam, Sammie fixed Susie with her warm gaze and told her how happy we were that she had come to see us that day.
The Deadliness of Delaying Care
I left the room as Susie dressed and took a few moments to close my eyes and breathe deeply to compose what I would say. Frankly, I needed to collect my thoughts by clearing the smell from my nostrils and the image of that irregular, oozing, dark mass. I returned to the room. “Susie, I did find a growth at the top of your vagina,” I told her. “We won’t know for sure until the biopsies return, but I’m worried it may be cancer, and that it may have spread outside your cervix.” I stopped. I tried to allow my words to sink in. We sat together in silence. She started to weep. I passed her tissues and reached out to grab her hand. She would not remember most of what I was saying, but I hoped she’d remember my touch.
“Susie, there is treatment for this.” Again, I paused, waiting for her to wipe her tears and return my gaze. “I have some excellent partners who specialize in caring for women who have cancer of the cervix. We will get you help.” I was thinking that her treatment would mean chemotherapy and radiation, and that because the cancer had spread outside her cervix, her chances for a cure were lower, but still reasonable. When I share such a frightening diagnosis, patients usually ask for information or help, but some can’t speak at all because I have confirmed their worst fear, the fear of facing what their instincts already know. This fear can keep people out of doctors’ offices altogether. Now that Susie had come to see me, I wanted to do everything I could to keep her coming back and get the treatment that could save her life.
After getting Susie’s contact information, I walked her to the waiting area. “I will call you tomorrow to see how you are doing or if you have more questions,” I told her. “You do not have to go through this alone.”
It was now 1:15 p.m., and afternoon clinic was starting. I slumped onto a stool in a quiet room for a few minutes. I’d encountered something heartbreaking, but sacred. I’d entered a space with Susie where time stopped and everything that came before fell away. I felt complicit, somehow, in Susie’s suffering. By uttering the word cancer, I’d rewarded a patient for finally seeking care by confirming her worst fear. Tears ran down my cheeks, thinking about Susie, how much her life had changed in the last hour. Did she hear any of the hope I tried to offer?
When she came to the clinic that morning, Susie had reached a crisis point in her health. As I confirmed her fear that “something was really wrong,” I, too, echoed those words to myself. Yes, something is really wrong. Another patient had received a devastating, possibly terminal diagnosis for a disease I knew to be preventable.
The fact that science had recently deemed her disease preventable offered few reassurances for Susie. She came to a clinic in a country with sophisticated health care systems and resources, and she still ended up with advanced cervical cancer.
No Country Is Immune to the Ravages of Cervical Cancer
Susie’s story starts to unpack the uncomfortable truth. Even in the United States, where we can offer vaccines that prevent cervical cancer and tests that can screen and treat for the first possible signs, women face obstacles to lifesaving care. They suffer far more than they should. It’s not enough to offer tests, treatments, or vaccines if we are also not addressing the accessibility, financial, and emotional issues that prevent women from using them. In other words, cervical cancer is only as preventable as a country’s willingness to provide prevention services and to ensure persons with cervixes avail themselves of them. Without the conscientious efforts of caring, committed individuals, health care systems, governments, and global alliances – particularly in the wealthiest nations – the science of prevention simply isn’t enough to stop women from dying.
To prevent cervical cancer, we must understand not only how to prevent it, but also what gets in the way of preventing it. Part One of this book addresses the scope of this cancer and its economic and social costs. Part Two examines the science of cervical cancer – what causes it, how to prevent it, how to treat it once it occurs, and how being infected with human immunodeficiency virus (HIV) affects cervical cancer’s behavior. Part Three delves into the crucial question: What are the social, economic, political, and cultural issues that continue to make this cancer so difficult to stop? Finally, Part Four introduces those devoted to solving the problem of cervical cancer, and how their efforts can inspire us to work alongside them. As it will soon become clear, truly making cervical cancer preventable requires a herculean effort. To meet this goal – that no person with a cervix suffers again from cervical cancer – all of us will need to play a part.
Cervical cancer, of course, is not about numbers or obstacles; it is about people. As such, I have made a point of weaving in the stories of women affected by cervical cancer. Their stories show, in a way that facts and figures can’t, just how difficult a journey with cervical cancer can be.
Although I refer to these stories as “women’s stories,” the term “women” in reference to cervical cancer can be misleading. Cervical cancer happens to persons with cervixes, some of whom may not identify as women. While I often refer to cervical cancer as a “woman’s disease” – partly for ease of understanding – it’s critical to recognize all genders born with female reproductive organs. Trans men or those born “female” who identify as gay, queer, or nonbinary can be doubly disadvantaged when it comes to seeking cancer care, since they are more likely to face discrimination in any medical environment. They are understandably less likely to pursue a procedure as intimate or uncomfortable as cervical cancer screening. I will talk more about the challenges these individuals face. But for the purposes of this book, the term “women” stands for the cervical cancer prevention needs of all persons with cervixes. I hope readers will offer me grace as I try to navigate an issue that I care about very deeply.
In looking at medical approaches to cervical cancer and global disease spread, I have separated the world into two income-level categories. The World Bank divides countries’ gross national incomes into four groups. For the purposes of this book, I have lumped together the top two groups, deeming “higher-income” what the World Bank calls “upper-middle- and high-income” countries and “lower-income” for the “lower-middle- and low-income” countries (Figure 1.1). I’ve created these two designations partly for ease of argument, but also to show the contrasting abilities for governments to fund health care and delivery systems for their citizens, which includes services for preventing and treating cervical cancer.
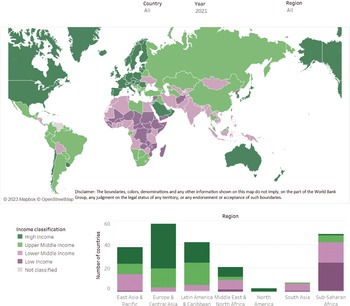
Figure 1.1 World Bank classifications of income levels by country
No Matter a Country’s Wealth – Inequity Is Everywhere
In lower-income countries, the cost of comprehensive cervical cancer prevention and treatment services poses a significant problem; health care budgets in lower-income countries can be less than $100 USD per person per year.1 With so little to spend on citizens’ health, governments must make cervical cancer a priority and direct sufficient resources toward it. These efforts can be stymied not only by financial barriers but also by cultural and social barriers to prevention.
Marginalized communities in higher-income countries face many of the same challenges as lower-income countries, even while wealthy countries spend much more on health care. Underneath the sight line in higher-income countries are women whose poverty level creates a different health care reality – one that is not reflected by the country’s World Bank higher-income-level designation. Because society doesn’t deem women with low incomes a priority, they suffer from a lack of ready access to the services many of their fellow citizens take for granted. In addition to struggling with personal finances, marginalized women can face – or may solely face – barriers that include stigma, lack of awareness, or specific religious or cultural taboos. While women in lower-income countries typically face far more significant barriers, women in higher-income countries can be affected in a similar way, discouraging them from seeking preventative health care: a “wealthy country problem” that runs counter to many people’s expectations.
Despite scarcely resourced countries assuming the burden of disease, these “pockets of inequity” in the developed world explain why this book divides its attention between cancer prevention obstacles in lower-income and higher-income countries. It’s astonishing to see such discrepancies in medical care within the same country, and even within smaller geographic regions. Shockingly, U.S. women’s diminished access to cervical cancer prevention services can parallel women’s experience in parts of Africa: the inability to travel the distance needed to a clinic, the costs that keep care out of reach, or a striking lack of treatment or follow-up care providers, the latter of which causes women with vastly different income levels to compete for the same prevention resources. These are the kinds of factors that make a preventable disease so deadly. Existing social structures suggest a cancer can only be made preventable for those lucky enough to live in the right place and with the money to pay for preventative care.
Because cervical cancer is a global problem, this book features research on cervical cancer prevention across a variety of countries, just as it includes women with access to a diverse range of resources. The book examines obstacles to cervical cancer elimination across diverse geographic locations – countries found in all four hemispheres, some of them densely populated or, conversely, with more sheep than people. I’ve looked at various economic settings, from countries offering the highest level of medical care to those with scant clinics or hospitals. Of course, I’m most familiar with the U.S. health system where I’ve based my medical practice. Because the United States offers its citizens a unique, mixed model of private- and public-funded health care, I’ve compared it with how well women are served in other higher-income countries relying on a publicly funded system, such as the United Kingdom, Canada, and Australia. And while publicly funded health care appears to offer a reliable supply of cervical cancer prevention services, women isolated by geography, finances, or social status aren’t necessarily able to take advantage of them.
For women like Susie and Maria, to whom I could offer few words of hope, I hope for this: that by exploring and acknowledging the underlying issues allowing for the continued spread of cervical cancer in both lower- and higher-income countries, we might find a way to erase a disease that continues to rage across the globe; in our failure to help these two women, that we can and will spare others a similar fate.