Attention-deficit hyperactivity disorder (ADHD) in childhood is characterised by inattention, impulsivity and hyperactivity, with onset before 7 years of age. There is a male preponderance, with a male:female ratio of 3:1. In adults (people over 18 years of age), the ratio is reported to be about equal.
The prevalence of ADHD in adults has not been systematically investigated, but estimates derived from the literature suggest that the disorder affects from 2% to 6% of adults. Estimates of the persistence of childhood symptoms into adulthood vary greatly, from 4% to 66% (Reference Barkley, Fischer and SmallishBarkley 2002; Reference Weiss and MurrayWeiss 2003).
Evolution of the diagnostic concept
The concept of ADHD has developed over the past 105 years and still continues to evolve. In 1902, Still described children with hyperactivity and poor attention skills as having ‘minimal brain dysfunction or damage’ (Reference Zwi and YorkZwi 2004). In 1930, the prevailing view was that ADHD was caused by gross brain damage. In 1937, Charles Bradley noted that 14 out of 30 children with behaviour problems showed a ‘spectacular change in behaviour during the first week of treatment with benzedrine’. He also reported the successful use of amfetamine in reducing hyperactivity in children (Reference Zwi and YorkZwi 2004). From that point, the view of ADHD as being caused by brain damage was no longer held to be sustainable given the absence of ‘actual brain lesions’.
During this period, psychoanalytical child psychiatrists conceptualised ADHD in the context of parenting and familial environments. In 1957, methylphenidate was introduced as a treatment for ADHD and within a decade the terms ‘hyperkinetic’ (as described by DSM–II; American Psychiatric Association 1968) and ‘hyperactive’ assumed greater popularity. DSM–III used the term ‘attention deficit disorder, with or without hyperactivity’ (American Psychiatric Association 1980). At this time, anti-medication campaigns gained considerable momentum and the whole field of ADHD diagnosis and treatment became the subject of debate and controversy.
The term ‘attention-deficit hyperactivity disorder’ first appeared in DSM–III–R (American Psychiatric Association 1987), and ‘impairment in the work place’ as a criterion was introduced. Following this, DSM–IV criteria (American Psychiatric Association 1994) for diagnosis of ADHD distinguished three subtypes that had not been previously studied in detail:
-
• adolescents with predominantly inattentive subtype (ADHD–I);
-
• adolescents with predominantly hyperactive and impulsive subtype (ADHD–HI);
-
• adolescents with the combined subtype (ADHD–C).
Aetiology
The aetiology and pathophysiology of ADHD remain in doubt, but substantial strides have been made in the past few decades. Given the neurocognitive and behavioural manifestations of the disorder, and the diagnostic requirement that onset be before the age of 7, aetiological factors applicable to childhood ADHD are applicable to the adult form as well. Various neurobiological factors have been identified that need to be studied further to understand their interaction with environmental factors. The Utah (Reference Ward, Wender and ReimherrWard 1993) and Reference Conners, Erhardt and SparrowConners (1999) criteria emphasise that adult ADHD is a continuation of childhood disorder.
Genetic findings
Genetic studies reveal a family history concordance rate of approximately 50% in first-degree relatives. Family and twin studies demonstrate a higher genetic concordance than has been established for any other psychiatric disorder (Reference Weiss and MurrayWeiss 2003). A family study by Reference Faraone and DoyleFaraone (2001) also supports the assertion that ADHD is hereditary.
Many studies have shown that ADHD in childhood is highly heritable, but inheritance is complex and likely to involve several genes acting together (Reference Zwi and YorkZwi 2004). Reference Goodman and StevensonGoodman & Stevenson (1989) found the heritability of hyperactivity to be as high as 64%. A twin study by Reference Sherman, Iacono and McGueSherman et al (1997) revealed that mothers' ratings showed a heritability of 91% for impulsivity/hyperactivity and 69% for inattention, and teachers' ratings yielded heritability of 69% for impulsivity and 39% for inattention.
The gene most strongly implicated in ADHD is the D4 dopamine receptor gene DRD4. The distribution of DRD4 mRNA in the brain suggests that it plays a role in cognitive and executive functions. These functions are implicated in the pathophysiology of ADHD (Reference Paterson, Sunohara and KennedyPaterson 1999).
Neuroimaging
The striatum, frontal lobes and posterior peri-ventricular regions are thought to be important for controlling and directing what we attend to. As well as having complex connections with each other, these three areas have rich connections with cortical sensory systems and play a key role in attention by filtering out unnecessary information. In individuals with ADHD, the poor functioning of these gates revealed in neuroimaging studies will impede this process of selective attention.
One study (Reference Zametkin, Nordahl and GrossZametkin 1990) used positron emission tomography (PET) and single-photon emission computed tomography (SPECT) to assess blood flow and glucose metabolism in various parts of the brain of hyperactive adults who had had childhood ADHD. Affected individuals metabolised glucose at rates 8% lower than the control group on continuous performance tests of attention and vigilance to stimuli. This decrease in metabolic activity was most noticeable in the prefrontal and premotor regions of the brain. Another SPECT study, of children with ADHD, revealed decreased blood flow in the frontal lobes and the posterior periventricular region of the right hemisphere (Reference Lou, Henriksen and BruhnLou 1990). The caudate nuclei/striatum were the most consistent areas of underfunctioning. Administration of methylphenidate has been shown to cause redistribution of blood flow in the brain, allowing irrelevant messages to be filtered out, thus improving individuals' concentration (Reference Lou, Henriksen and BruhnLou 1989).
Other research has looked at the dopamine transporter, the main target of stimulant medications. A SPECT study of dopamine transporter density in adults with ADHD revealed density in the striatum to be elevated by about 70% (Reference Dougherty, Bonab and SpencerDougherty 1999).
Biochemical factors
A number of studies, postulating heterogeneous biochemical aetiologies for ADHD (Box 1), used dietary supplements (a mix of vitamins, minerals, phytonutrients, amino acids, essential fatty acids, phospholipids and probiotics) in attempts to redress these biochemical risk factors. Their findings support the effectiveness of food supplements in improving attention and self-control in children with ADHD and suggest that their efficacy equals that of methylphenidate (Reference Harding, Judah and GantHarding 2003). Hence, it was considered that children deficient in these substances, or in whom these were substantially decreased by other food additives, were predisposed to manifesting ADHD.
BOX 1 Biochemical risk factors for ADHD
-
• Food and additive allergies
-
• Heavy-metal and other environmental toxins
-
• Low-protein/high-carbohydrate diets
-
• Mineral imbalances
-
• Essential fatty acid and phospholipid deficiencies
-
• Amino acid deficiencies
-
• Thyroid disorders
-
• Vitamin B deficiencies
Studies suggest that children with ADHD have lower levels of essential fatty acids (omega-3 and omega-6) (Reference RichardsonRichardson 2006). It is speculated that replacement of essential fatty acids through food or supplements may help to decrease the behaviours and symptoms of ADHD.
A study conducted at the Children's Hospital, Boston, USA, indicated that prenatal exposure to phenylalanine is associated with a higher likelihood of subsequent hyperactive or impulsive symptoms, and postnatal exposure is associated with a higher likelihood of inattentive symptoms (Reference Antshell and WaisbrenAntshell 2003). The study concluded that toxicity is dose dependent.
An open study (Reference Mousain-Bosc, Roche and RapinMousain-Bosc 2004) concluded that hyperexcitable children have low intra-erythrocytic magnesium (ERC-Mg) levels with normal serum magnesium values, and that magnesium/vitamin B6 supplementation restored normal ERC-Mg levels and improved the children's abnormal behaviour.
Environmental factors
Environmental risk factors fall into three broad categories (Reference Asherson, Kuntsi and TaylorAsherson 2005) (Box 2):
-
• prenatal/perinatal risks
-
• parental and family risk
-
• acquired neurobiological risks.
BOX 2 Environmental factors associated with ADHD
-
• Prenatal and/or perinatal risks (e.g. prematurity, low birth weight, exposure to toxins)
-
• Parental and family factors (e.g. child neglect, inconsistent parenting, high expressed emotion, family conflict, early institutional rearing)
-
• Acquired neurobiological risks (e.g. head trauma)
These factors play a role in the persistence of the disorder, the development of comorbid disorders and the outcome of the individual. There is a lack of solid evidence for the cause-and-effect association. However, it would be possible for researchers and clinicians to investigate specific environmental factors that interact with biogenetic vulnerabilities.
Clinical manifestations in adults
Some symptoms of childhood ADHD persist more than others into the adult form. Research suggests that up to 66% of children will continue to have clinically significant symptoms in adulthood (Reference Barkley, Fischer and SmallishBarkley 2002).
Hyperactivity
If hyperactivity continues into adult life, its form differs from that in childhood. The symptom of ‘nervousness’ is often reported (Reference MillerMiller 2002). Individuals may describe feelings of discomfort that are relieved only with physical activity. There may be physical or verbal overactivity. Individuals may find it very difficult to rest, moving about excessively, squirming or fidgeting. Individuals who are hyperactive often talk excessively, either interrupting others or monopolising conversation and not letting others express their views. Their disruptive behaviour often creates great problems in social, family and occupational situations.
Impulsivity
The negative consequences of impulsivity may be far reaching and may be seen across the entire spectrum of functioning. This may be linked with poor psychosocial outcome. A tendency to constantly interrupt often undermines the quality of social interaction. Problems may arise as a result of aggressive driving, impulsive and injudicious spending, or starting multiple projects without carrying them through to completion. A pattern of pleasure-seeking behaviours and limited capacity to plan or assess their consequences is noted. Often their actions result in forensic sequelae.
Inattention
Adults with inattention often fail to pay close attention to detail, make careless mistakes, fail to listen when spoken to directly or do not follow instructions. There may be subjective or non-specific reports of difficulties in the performance of daily tasks and in concentrating on watching television or reading. This often results in significant educational, occupational and interpersonal problems.
Psychosocial and occupational problems
Intellectual disabilities often persist, such as problems with spelling, reading and arithmetic. Confusion of right and left may occur along with reversal of numbers and letters.
Disorganisation or irritability may have detrimental effects on relationships, which can become strained and dysfunctional, and may suffer because of impulsivity, temper, failure to listen to partners and poor prioritisation. This is further compounded if the obstinacy, bossiness and stubbornness often described in children persists into adulthood. Communication becomes difficult. Adults with ADHD tend not to take part in the conversation of others and interpret poorly (Reference ElliottElliott 2002).
Adults may cite their primary concern as procrastination, lack of motivation, or mood lability (Reference Weiss and MurrayWeiss 2003). The inability to control frustration and poor academic performance despite average or above average IQ are found in adult ADHD (Reference ElliottElliott 2002). Adults often describe very reactive mood: fluctuations may occur without any identifiable triggers, although some individuals are particularly vulnerable to the effects of sudden changes of environment. Mood fluctuations can last anywhere between a few hours and a few days (Reference WenderWender 2000).
Differential diagnosis
Many of these symptoms occur in various psychiatric disorders; it is important therefore to systematically assess each symptom to rule out organic disorders (Reference WenderWender 2000). Individuals with ‘undiagnosed’ ADHD manifest significantly greater functional and psychosocial impairment than those screening negative for the disorder, suggesting that ADHD poses a serious burden to adults even when clinically unrecognised (Reference Able, Johnston and AdlerAble 2007). Failure to gain promotions at work or frequent dismissals because of impaired work performance may result.
Comorbidity
Comorbidity is common, with estimates as high as 80%. The rate of comorbidity with personality disorders is 10–20% and with antisocial behaviour 18–28% (Reference BarkleyBarkley 1998). Hyperactive children are at a greater risk for antisocial activities and arrests by the time they reach young adulthood. These are most often for illegal drug possession, use and sale (Reference Barkley, Fischer and SmallishBarkley 2004). In a prospective case–control study of hyperactive boys with conduct problems and healthy boys, Reference Satterfield and SchellSatterfield & Schell (1997) concluded that the risk of becoming an adult offender is associated with conduct problems in childhood and serious antisocial behaviour in adolescence. Hyperactive children who do not have conduct problems are not at increased risk for criminality later in life.
The comorbidity for alcohol misuse is 32–52%; for other types of substance misuse, including marijuana and cocaine, it is 8–32% (Reference Goldstein and EllisonGoldstein 2002: p. 47).
Dysthymia in particular is common in adults with ADHD. The National Comorbidity Survey Replication Study found that among individuals diagnosed with depression, bipolar disorder or anxiety disorders, the rates of ADHD were 32%, 21.2% and 9.5% respectively (Reference Kessler, Adler and BarkleyKessler 2006).
Impulsivity in ADHD is associated with psychiatric comorbidity and may present both directly and indirectly with forensic sequelae. When there is forensic involvement, the need for specialists and experts becomes even greater in order to deal with the many levels of psychopathology, emotional and behavioural dysfunction and sociopathic traits, and responding appropriately to treatment and court recommendations.
Reference Weiss, Hechtman and PerlmanWeiss and colleagues (1979) reported that during adolescence and young adulthood, individuals with ADHD were more likely to be involved in traffic accidents as drivers than their unaffected peers. They were also more likely to incur damage to their vehicle. Reasons for this include excessive unmodulated anger, aggression and risk-taking behaviour (Reference Deffenbacher, Lynch and FilettiDeffenbacher 2003), infrequent use of seat belts, greater use of alcohol and drugs, affiliation with peers who tolerate and support drug use, lack of parental monitoring, stress and persistent behavioural or emotional difficulties (Reference Shope, Waller and RaghunathanShope 2001). Disorganisation, emotional disturbances, stress intolerance and disorders such as dyslexia, dyscalculia and dysgraphia are common in ADHD.
Diagnostic assessment
Assessment of adults is similar to that of children (Box 3). The clinician must assess current (in the past 6 months) and childhood (before 7 years of age) symptoms in accordance with standard diagnostic criteria (Box 4 shows an assessment based on DSM–IV). Adults may have difficulty in accurately recalling childhood symptoms, therefore obtaining a childhood history is an essential component of the assessment: self-report rating scales and gathering information from school records/reports as objective evidence of childhood onset is necessary. It is useful to obtain information from parents or siblings, aided by the use of standardised rating scales. Cultural factors should be borne in mind when diagnosing the disorder. Adult ADHD is a clinical diagnosis, and the clinician-administered interview remains the cornerstone of diagnostic evaluation (Reference Adler and CohenAdler 2004).
BOX 3 Steps in the diagnosis of ADHD in adults
-
1 Clinical interview to assess current ADHD symptoms (within the past 6 months)
-
2 Assess functional impairments at work, home and in relationships
-
3 Developmental history and childhood history of ADHD symptoms
-
4 Rule out other psychiatric disorders or establish comorbid conditions
-
5 Family history of mental health problems (e.g. ADHD, obsessive–compulsive disorder, tics, learning difficulties, attention/concentration difficulties)
-
6 Complete physical examination (rule out head trauma, seizures, substance misuse, hormonal problems)
-
7 Rule out ongoing social stressors as generators of symptoms that mimic ADHD
-
8 Neuropsychological assessments (e.g. attention, memory, intellectual functioning and academic achievement)
(Adapted from Reference Weiss and MurrayWeiss 2003)
BOX 4 Assessment and diagnosis of ADHD in adults
Ask the patient to indicate how often, on a 4-point scale (0, never or not at all; 1, sometimes or somewhat; 2, often or pretty much; 3, very often or very much), he or she has experienced the following symptoms in the past 6 months and whether they have persisted for at least 6 months.
Assessment
-
a Inattention
-
• Does not pay close attention to what he or she is doing and makes careless mistakes
-
• Has trouble paying attention to tasks
-
• Has trouble following verbal instructions
-
• Starts things but does not finish them
-
• Has trouble getting organised
-
• Tries to avoid doing things that require a lot of concentration
-
• Misplaces things
-
• Is easily distracted by other things going on
-
• Is forgetful
-
-
b Hyperactivity–impulsivity
-
• Fidgets with hands or feet
-
• Has trouble sitting still
-
• Feels restless and jittery
-
• Has trouble doing things quietly
-
• Is a person who is ‘on the go’
-
• Talks too much
-
• Acts before thinking things through
-
• Gets frustrated when having to wait for things
-
• Interrupts other people's conversations
-
Diagnosis
All of the following criteria must be met for a diagnosis of ADHD:
-
1 six or more of the symptoms of either (a) or (b) above are rated as ‘often or pretty much’ or ‘very often or very much’ and have persisted for at least 6 months (for adults over 50, only three or more symptoms rated ‘often’ or ‘very often’ are required)
-
2 some symptoms of inattention or hyperactivity–impulsivity that caused impairment were present in childhood
-
3 impairment from the symptoms is present in two or more settings (e.g., at work, at school, at home, during leisure activities, when driving a car)
-
4 there is clinically significant impairment in social, academic or occupational functioning
-
5 the symptoms do not occur exclusively during the course of a pervasive developmental disorder, schizophrenia or other psychotic disorder and are not better accounted for by another psychiatric disorder
(After Reference Weiss and MurrayWeiss 2003, with permission)
As ADHD is highly familial, it is essential to look for a family psychiatric history of the disorder: first-degree relatives might have difficulty with tics, drug use and criminal behaviours.
A complete physical examination to rule out neurological and hormonal problems is also an important part of the assessment. Neuropsychological tests contribute to the clinician's overall impression, although none have good sensitivity and specificity for diagnostic purposes. Psychoeducational testing is beneficial if the clinician suspects an intellectual disability (Reference Weiss and MurrayWeiss 2003).
The Adult Self-Report Inventory–4 (ASRI–4) and the Adult Inventory–4 (for informants) are screening tools designed to assist clinicians with the assessment of comorbid conditions and differential diagnoses (Reference Weiss and MurrayWeiss 2003). Other common scales are listed in Table 1.
Although there is ongoing debate about the validity of the adult condition and the specificity of the available diagnostic criteria, DSM–IV (American Psychiatric Association 1994) and ICD–10 (World Health Organization 1992) criteria are the best available diagnostic guides.
Management
A judicious mix of pharmacological (Table 2), neuropsychological and environmental interventions is likely to provide optimal improvements in adult ADHD.
Pharmacological interventions
Pharmacological treatments proven to be efficacious in children appear to benefit adults. Children with untreated ADHD growing into adults suffer from lifelong work and relationship problems, confounded by comorbid conditions such as low self-esteem and mood disorders.
First-line treatment
The first line of treatment is with stimulant agents such as methylphenidate or amfetamine salts. Methylphenidate dosing requires careful titration from lowest possible dose to achieve best control of symptoms. Extended-release methylphenidate tablets should not be crushed, divided or chewed. Dexamfetamine can be started at a dose of 10 mg/day, and increased by 10 mg/day weekly up to a maximum of 45 mg/day. About two-thirds of adults with ADHD who are given these medications show significant improvement in their symptoms (Reference Gadow and WeissGadow 2001).
Atomoxetine was the first non-stimulant medication approved by the US Food and Drug Administration (FDA) for the treatment of ADHD in both adults and children. Randomised placebo-controlled studies have showed atomoxetine to be effective in the treatment of adult ADHD (Reference Michelson, Adler and SpencerMichelson 2003). It is a highly specific nor-adrenaline reuptake inhibitor with minimal affinity for serotonin and dopamine transporters and neuronal receptors.
Second-line treatment
Second-line treatment includes imipramine, clonidine and, occasionally, moclobemide. In view of the hypotonic side-effects of clonidine, a study conducted in Italy (Reference NiederhoferNiederhofer 2004) looked at tianeptine as an alternative. Tianeptine has a longer excretion half-life, decreased sedative effects and more selective binding profile. This preliminary study concluded that tianeptine might be more effective and beneficial for ADHD, reducing hyperactive behaviours and improving attention with minimal side-effects.
Other pharmacological treatments
The most recent FDA-approved product for the treatment of ADHD is the methylphenidate transdermal system (MTS) patch. In a large-scale phase 3 study, clinician, teacher and parent ratings of ADHD symptoms showed the patch to be superior to placebo (Reference Melmed, Arnold and BurnsideMelmed 2006). It was safe and well tolerated: adverse effects were similar to what would be expected for oral methylphenidate.
Lisdexamfetamine (LDX) is a novel amfetamine prodrug in which an amino acid is covalently bound to the amfetamine molecule. This bond can only be broken through enzymatic processes in the gastrointestinal tract, and the compound is biologically inert if used via any other route of administration. This means that this compound may possess lower misuse potential via intranasal or intravenous routes, or if the compound is smoked. Lisdexamfetamine gained FDA approval in 2007.
At least two additional non-stimulants are in development (Reference KollinsKollins 2007). Phase 1 studies of an extended-release formulation of guanfacine (GXR) in healthy adults have found it to be safe and well tolerated at daily doses of 1–4 mg (Reference Swearingen, Pennick and ShojaeiSwearingen 2006). As rebound hypertension following treatment cessation could occur, an abrupt cessation study was conducted with healthy young adults. In this study GXR was either tapered down or discontinued abruptly. No significant differences in electrocardiogram parameters of rebound hypertension were found between the two groups (Reference Kisicki, Fiske and SchecknerKisicki 2006). With respect to clinical efficacy, a phase 3 study conducted in children and adolescents reported that once-daily GXR doses of 2, 3 and 4 mg significantly reduced scores at endpoint on the Attention-Deficit/Hyperactivity Disorder Rating Scale IV compared with placebo (Reference Biederman, Melmed and PatelBiederman 2008). These effects were observed for both hyperactive/impulsive and inattentive symptoms. The patients tolerated the drug well, with 16.2% of the 258 individuals taking GXR discontinuing because of adverse events. Mild to moderate somnolence, sedation or fatigue were among the most common events and tended to be transient. Taken together, these studies suggest that GXR is a promising non-stimulant alternative for treatment of ADHD. Currently GXR is under review by the FDA.
Nicotinic agonists, another class of non-stimulant compound currently under investigation, have shown promising results with no clinically significant adverse effects (Reference Wilens, Verlinden and AdlerWilens 2006).
Neuropsychological interventions
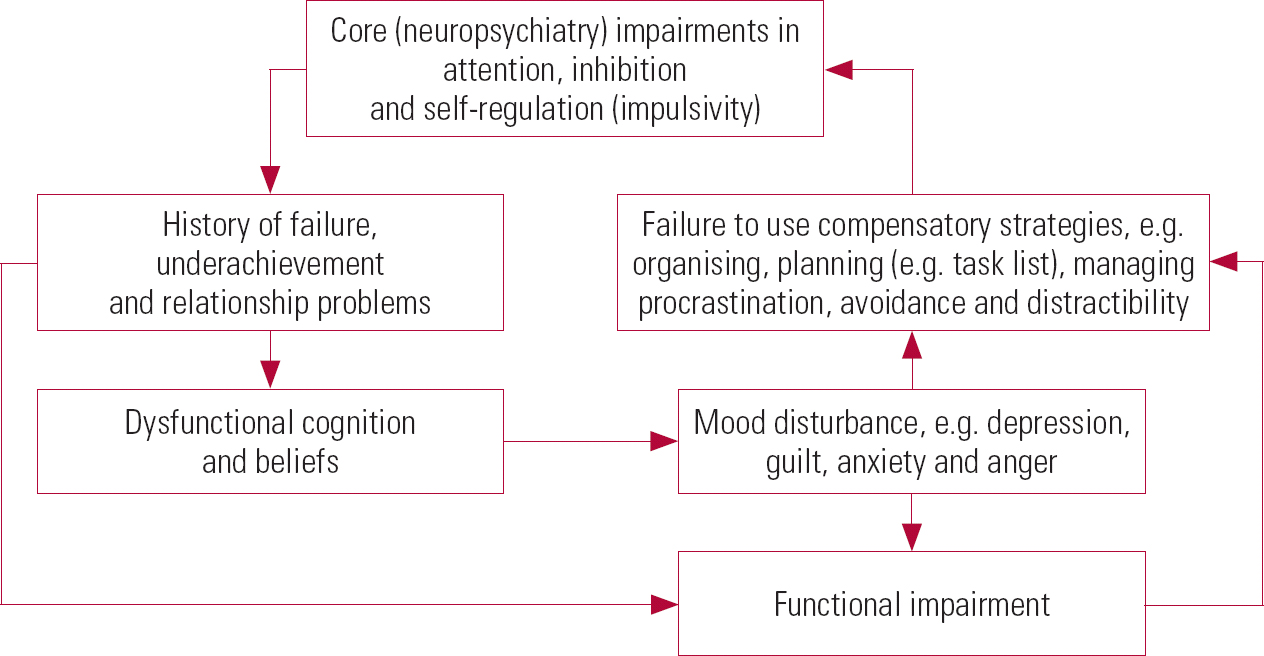
Cognitive approaches to understanding ADHD emphasise the role of dysfunctional cognitive responses to work or academic demands (Fig. 1). Chronic patterns of procrastination and disorganisation are hypothesised to be strengthened by negative cognition. Cognitive–behavioural therapy for ADHD conceptualises treatment in terms of three core modules (Reference Hallowell and NadeauHallowell 1995; Reference Nadeau and NadeauNadeau 1995; Reference Murphy, Barkley and MurphyMurphy 1998; Reference McDermott and BrownMcDermott 2000) and several optional modules (Box 5).
BOX 5 Cognitive–behavioural therapy for ADHD
First module
This provides training and structure for enhanced organisational and planning skills. The first three sessions involve learning new skills and the fourth session is for review and consolidation. The module also includes training in problem-solving skills.
Second module
This targets distractibility.
Third module
Targets the elimination of dysfunctional thoughts that increase negative affect and that enhance avoidance of work-related topics.
Optional modules
Application of skills to cope with procrastination, anger, communication and relationship problems.
Marital/individual counselling and self-help groups are often valuable adjuncts to pharmacotherapy and skills training.
Further research on these strategies in the context of well-controlled trials is an essential step for helping to reduce disability and distress among individuals with ADHD.
Environmental interventions
Changes in physical setting can improve individuals' learning and functioning. People with ADHD cannot ignore unimportant sounds and sights, so reducing these distractions as much as possible improves attention and concentration. Environmental manipulations similar to those recommended for improving attention and concentration in children with ADHD can also help adults with the disorder. These include rehearsed listening strategies, interactive learning, more structured life at home and office, regular bedtimes, calm activities and adequate sleep (Reference Goldstein and EllisonGoldstein 2002). Supervision, behaviour modification, family intervention and support possibly help to alleviate the symptoms of impulsivity and hyperactivity.
MCQs
-
1 Executive functioning in ADHD can be evaluated using the:
-
a Brown Attention Deficit Disorder Scale
-
b Conners' Adult ADHD Rating Scale
-
c Adult ADHD Self-Report Scale
-
d the Wender–Reimherr Adult Attention-Deficit Disorder Scale
-
e Copeland Symptom Checklist for Attention Deficit Disorders – Adult Version.
-
-
2 An area not known to underfunction in ADHD is the:
-
a frontal lobes
-
b striatum
-
c posterior periventricular region
-
d caudate nuclei
-
e occipital lobes.
-
-
3 Which of the following statements is false?
-
a prenatal phenylalanine exposure is associated with hyperactive symptoms in children
-
b phenylalanine toxicity is dose dependent
-
c postnatal phenylalanine exposure is associated with inattentive symptoms in children
-
d impulsivity is associated with absence of phenylalanine exposure
-
e children with ADHD and a history of conduct problems are at increased risk of becoming adult offenders.
-
-
4 The following comorbidities are found in ADHD except:
-
a post-traumatic stress disorder
-
b alcohol and substance misuse
-
c personality disorders
-
d dysthymia
-
e depression and anxiety.
-
-
5 The first FDA-approved non-stimulant medication for ADHD in both adults and children was:
-
a guanfacine
-
b atomoxetine
-
c methylphenidate
-
d dexamfetamine
-
e nicotinic agonists.
-
MCQ answers
| 1 | 2 | 3 | 4 | 5 | |||||
|---|---|---|---|---|---|---|---|---|---|
| a | t | a | f | a | f | a | t | a | f |
| b | f | b | f | b | f | b | f | b | t |
| c | f | c | f | c | f | c | f | c | f |
| d | f | d | f | d | t | d | f | d | f |
| e | f | e | t | e | f | e | f | e | f |
TABLE 1 Screening tools for assessing ADHD
| Rating scale | Indication |
|---|---|
| Brown Attention Deficit Disorder Scale (Reference BrownBrown 1996) | Self-report questionnaire. Explores the executive functioning aspects of cognition that are associated with ADHD |
| Conners Adult ADHD Rating Scales (CAARS) (Reference Conners, Erhardt and SparrowConners 1999) | Two formats are included for self-report ratings and observer ratings. Both the self-report and observer forms provide multimodal assessments of the same behaviours and problems |
| The Wender–Reimherr Adult Attention Deficit Disorder Scale (WRAADS) (Reference Wender, Reimherr and WoodWender 1981) | To measure the severity of the target symptoms of adults with ADHD using the Utah criteria |
| Copeland Symptom Checklist for Attention Deficit Disorders – Adult Version (Reference CopelandCopeland 1991) | To assess whether an adult has characteristic ADHD symptoms, to what degree, and which areas of functioning are most seriously affected |
| Adult ADHD Self-Report Scale (ASRS) (Reference Adler, Spencer and FaraoneAdler 2006) | Self-screening tool to identify adults who might have ADHD |
TABLE 2 Common pharmacological treatments for ADHD
| Medication | Formulations | Starting daily dosage | Target daily dosage |
|---|---|---|---|
| Methylphenidate | 5, 10, 20 mg tablets; 20 mg slow-release tablets | 5–10 mg, 3–4 times daily | 40–60 mg |
| Controlled-release tablets: 18, 36 mg tablets | 18 mg, once daily in the morning | 36–54 mg | |
| Clonidine | 25, 100, 150 μg | 25 μg | 150–300 μg |
| Pemoline | 18.75, 37.5, 75 mg tablets; 37.5 mg chewable tablets | 37.5 mg | 75 mg |
| Atomoxetine | 10, 18, 25, 40, 60 mg capsules | 0.5mg/kg | 1.4 mg/kg |
| Dexamfetamine | 5, 10, 15 mg slow-release capsules; 5 mg per 5 ml (elixir) | 5–10 mg, 2–3 times daily | 20–45 mg |
| Methamfetamine | 5 mg tablets; 5, 10, 15 mg long-acting tablets | 5–10 mg | 20–45 mg |
| Mixture of amfetamine and dexamfetamine | 5, 10, 20 mg tablets | 5–10 mg | 20–45 mg |
| Imipramine | 10, 25, 50 mg tablets | 10–25mg | 100–150 mg |
| Nortriptyline | 10, 25, 50, 75 mg capsules | 10–25mg | 75–100 mg |
| Bupropion | 75, 100 mg tablets | 37.5 mg, twice daily | 150–300 mg |
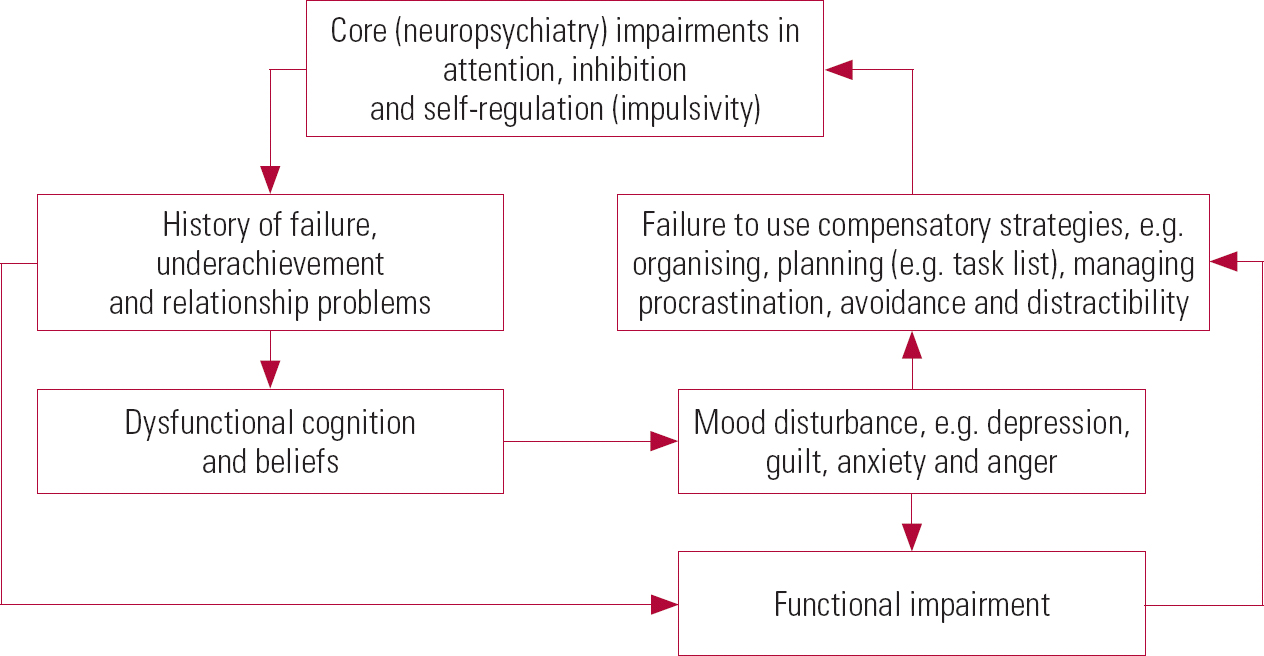
FIG 1 A cognitive–behavioural model of impairment in adult ADHD (after Reference Safren, Sprich and ChulvickSafren 2004, with permission).




eLetters
No eLetters have been published for this article.