Introduction
The percentage of deceased people needing palliative care (PC) in Europe ranges from 69% to 84% every year (Murtagh et al. Reference Murtagh, Bausewein and Verne2014). In Italy, this number is about 450,000–500,000 patients per year (Ministero della Salute 2019), and PC delivery is able to cover only 16%–19% of patients due to lower availability of services as compared to other countries (Longo et al. Reference Longo, Notarnicola and Rotolo2019; Ministero della Salute 2019).
PC was officially recognized by law in 2010, recognizing the needs of the population in terms of PC and chronic pain management and endorsing the citizen’s right not to suffer. Health services are provided in collaboration with private and/or nonprofit organizations on a free (or almost free) basis (Toth Reference Toth2014). Although the National Health Service (NHS) is available over the entire Italian territory, there have been reports of regional heterogeneity in the PC network (Ministero della Salute 2019).
At-home primary and specialized PC availability is insufficient (Ministero della Salute 2019; Scaccabarozzi et al. Reference Scaccabarozzi, Lovaglio and Limonta2019) although it allows patients and their families to live in their environment to maintain a good quality of life, and it also reduces the cost of care (Gomes et al. Reference Gomes, Calanzani and Gysels2013; Lattimore-Foot Reference Lattimore-Foot1996; Sanson‐Fisher et al. Reference Sanson‐Fisher, Girgis and Boyes2000; Sarmento et al. Reference Sarmento, Gysels and Higginson2017; Scaccabarozzi et al. Reference Scaccabarozzi, Lovaglio and Limonta2019). Timely, effective and personalized identification of the patients’ care needs should be a major goal of appropriate PC planning. Indeed, interventions that are not tailored to the actual needs of patients and caregivers risk to be useless or even damaging to the individual and to increase health costs due to a higher number of medical visits as well as emergency room and hospital utilization (Gilbertson-White et al. Reference Gilbertson-White, Aouizerat and Jahan2011). Clinical and sociodemographic characteristics have a primary role in determining care priorities of people affected by advanced diseases and showing multidimensional needs. In addition, sociocultural environment should be considered in the evaluation of patient needs and in the tailoring of an appropriate health-care pattern (Krikorian et al. Reference Krikorian, Limonero and Maté2012).
This observational retrospective study aims to describe geographical patterns in patients’ clinical conditions and demographic characteristics at the point of home PC inception and their relationship with care needs in the last month of life. In particular, the association between some clinical variables at the entry (age, Karnofsky Performance Score [KPS], symptoms, and therapies) and the intensity of care (number of physician and nurse home services) during the last 30 days of life has been analyzed among advanced cancer patients in Centre-North and Centre-South in Italy. Our main hypothesis was that the different sociodemographic conditions, structures, and processes for health-care delivery between the Centre-North and Centre-South of Italy would have impact on the delivery of PC, even with a universal health-care system.
Methods
Setting
The home PC program is provided by the National Tumor Assistance (ANT) Foundation (www.ant.it). It consists of a hospital-at-home approach in which a multidisciplinary team of physicians, nurses, and psychologists, all trained in PC, works around-the-clock 24 h/7 days a week to assist cancer patients. The service is available in 11 Italian regions where it is free for the patients and offered in agreement with the NHS (Casadio et al. Reference Casadio, Biasco and Abernethy2010).
Study design and patients
The observational retrospective study involved advanced cancer patients entered in the home PC program from January 1 to December 31 2020.
The analysis has been performed on patients with a care duration longer than 30 days and deceased at home within 31 August 2021. Since the primary outcome of the study was the number of health-care services given to patients at home during the last 30 days of life, alive patients or patients deceased at hospital or hospice or with a brief care (shorter than 30 days) have been excluded from the analysis.
Considering the recognized sociodemographic differences between Italian regions located in the Centre-North and the Centre-South (Toth Reference Toth2014), we split patients in 2 geographical clusters: Centre-North (Lombardy, Veneto, Emilia-Romagna, Tuscany, Umbria, and Marche) and Centre-South (Lazio, Campania, Puglia, and Basilicata). (Toth, Reference Toth2014).
All the clinical and demographic data of ANT patients and the health-care services provided by ANT physicians and nurses are collected on an electronic record form exploiting Cloud technology created by Vitaever® SaaS (Nethical S.r.l., Bologna Italy) (www.vitaever.com).
Data related to patients entering in ANT home PC program during the year 2020 have been extracted by the Vitaever® database in an Excel format.
Outcomes
The primary outcome of the study was the number of health-care services given to patients at home during the last 30 days of life (Hagarty et al. Reference Hagarty, Bush and Talarico2020). The health services were considered as follows: the total number and content of the activities performed by physician and nurse, physician alone, or nurse alone. The type services consist of complex clinical activities, simple clinical activities, and other activities (caregiver and family training, conversation with family and/or general practitioner, drug provision, death registration, etc.). The list of the complex and simple services provided by physicians and nurses is shown in Supplementary Table S1.
Variables considered in the analysis were as follows:
• demographic data (sex and age);
• days from the entry in home PC to death (survival);
• primary site of disease (recorded according the International Classification of Diseases [9th revision] (Ministero del lavoro della salute e delle politiche sociali 2007) and then classified as gastrointestinal, respiratory tract, genitourinary, breast, nervous system, hematological, and others);
• clinical data at the entry (KPS, pain [Numerical Rating Scale, NRS from 0 to 10], dyspnea [absent, moderate, and severe], delirium [absent, moderate, and severe], cachexia [absent, moderate, and severe], vomit [absent, nausea, and vomit], bowel function [regular, diarrhea, or constipation or irregular function], asthenia [absent, moderate, and severe], anxiety [absent, moderate, and severe]). These symptoms were collected on the Vitaever® electronic record at each visit and represent a simplified version of the paper medical records, which includes the Edmonton Symptom Assessment System and other relevant parameters (i.e. bowel function and delirium);
• therapies at the entry: infusion therapy, no cancer therapy, and therapy for advanced cancer.
Statistical analysis
Clinical and demographic characteristics of patients at the entry in home PC have been presented as follows: sex, oncological therapy, tumor primary site, and symptoms were shown as frequency, and the comparison between Centre-North and Centre-South has been analyzed by Chi-square test; age, KPS, and pain have been presented as mean ± SD, and the comparison between Centre-North and Centre-South has been analyzed by Mann–Whitney U test; survival (days from the entry in PC to death) has been presented as mean (95% CI) and the comparison between Centre-North and Centre-South has been evaluated by Cox regression adjusted for age and gender with Centre-North as reference group.
The bivariate correlation between demographic data, performance status, symptoms, and health-care services (total, performed by physician and by nurse) during the last month of life have been analyzed by Spearman’s Rank correlation. The association between the health-care services (total, performed by physician and by nurse, and dependent variables) and demographic data, performance status (KPS), symptoms, therapies at the entry (independent variables) was explored by General Linear Models (GLM).
The comparisons between complex, simple, and other activities (total, by physician and nurse) during the patient last month of life in Centre-North and Centre-South were analyzed by Mann–Whitney U Test. p-values were adjusted by the Benjamini–Hochberg correction for multiple testing. The significance threshold was set at 0.05.
The statistical analyses were executed by SPSS 27.0 for windows (SPSS Inc., Chicago, IL, USA).
Results
A total of 4971 cancer patients entered in at-home PC program during 2020. The selection of patients for the analysis of the health-care services in the last month of life is shown in Figure 1. Patients still alive at 3 August 2021 (n = 1383), who received care for <30 days (n = 1386), deceased in hospice or in hospital (n = 462), and with missing data (n = 19) have been excluded.

Fig. 1. Selection of ANT cancer patients for the analysis of the health-care services in the last month of life.
A total of 1721 patients (919 assisted in Centre-North of Italy and 802 in Centre-South) were considered for the analysis. Clinical and demographic characteristics as well as symptoms at admission and survival are shown in Table 1. Patients admitted in Centre-South were younger and showed a lower KPS as compared to Centre-North patients (p < 0.001 for both comparisons). A lower percentage of Centre-South patients was still receiving cancer treatment at admission (p < 0.001). Pain at admission was significantly lower in Centre-North (p < 0.001). The frequencies of asthenia, nausea or vomit, cachexia, anxiety, dyspnea, delirium, and irregular bowel function at admission were significantly minor in Centre-North (p ≤ 0.001 for each comparison). The survival of patients assisted in Centre-South was shorter (p = 0.010).
Table 1. Clinical and demographic characteristics of patients entering in home PC in Centre-North and Centre-South
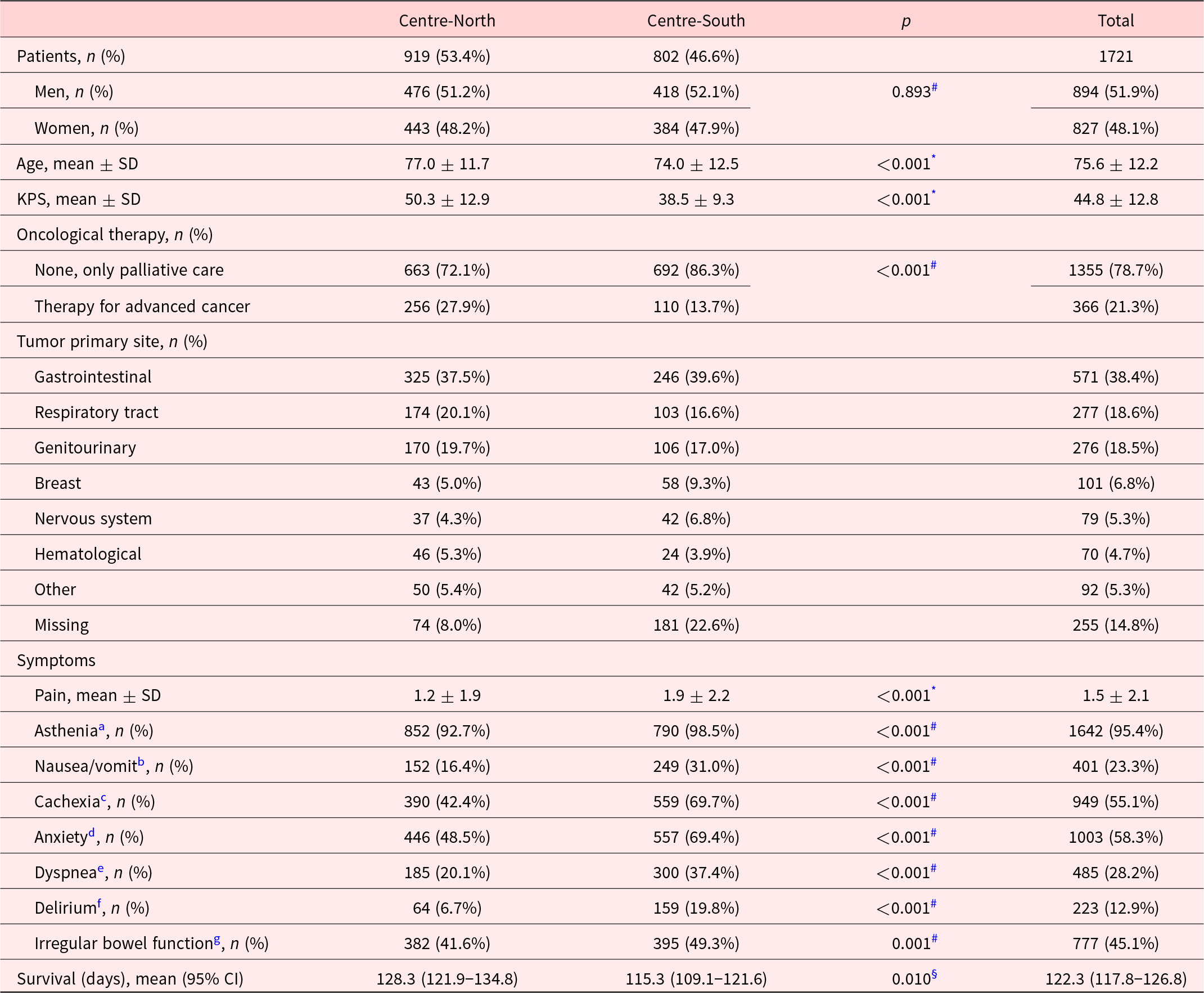
Comparisons between patients entering in home PC in Centre-North and Centre-South have been analyzed by
# Chi-squared test,
* Mann–Whitney U test, and
§ Cox regression adjusted for age and gender.
a Patients with moderate or severe asthenia.
b Patients with nausea or vomit.
c Patients with moderate or severe cachexia.
d Patients with moderate or severe anxiety.
e Patients with moderate or severe dyspnea.
f Patients with severe or moderate delirium.
g Patients with diarrhea, constipation, or irregular bowel function.
The association between demographics, KPS, symptoms, therapies at the entry, and total health-care service delivered (calculated as the sum of all the activities performed by physician and nurse during the last month of life) are shown in Table 2. Bivariate analysis highlights that age and KPS at admission were negatively correlated with the number of services during the last month of life. Pain, asthenia, nausea/vomit, cachexia, and anxiety at admission were positively correlated with number of health-care services during the last month of life.
Table 2. Bivariate correlation and General Linear Model showing the relationship between demographic data, performance status (KPS), symptoms, therapies at the entry and the total of the health-care services performed by physician and nurse during the last month of life

Bivariate correlation was analyzed by Spearman’s Rank correlation, ρ is the Spearman correlation coefficient, p-values of the correlation analysis were adjusted by the Benjamini–Hochberg correction for multiple testing. For the General Linear Model, the independent variable was the total number of the health-care services by physician and nurse, and among the independent variables, the following categorical variables have been considered:
a Men(ref) vs. women.
b Regular bowel function (ref) vs. diarrhea or constipation or irregular function.
c No infusion therapy (ref) vs. infusion therapy.
d No oncological therapy (only palliative care) (ref) vs. therapy for advanced cancer.
e Centre-North (ref) vs. Centre-South.
The severity of dyspnea and delirium were not significantly correlated with health-care services; hence, these symptoms were not included in the GLM. The GLM confirmed the independent association between age, asthenia and health-care services in the end of life (negative association for age and contrast estimate = −0.209; positive association for asthenia and contrast estimate = 3.045). Moreover, infusion therapy and cancer treatment at admission were associated with a higher frequency of health-care services in the end of life (infusion therapy and contrast estimates = 9.285; therapy for advanced cancer and contrast estimates = 2.294). The geographical area was not significantly associated with the total number of health services.
The association between demographic data, KPS, symptoms, therapies at the entry, and the health-care services provided by physician during the last month of life is shown in Table 3. Age and KPS at the entry were negatively correlated with the number of physician services during the last month of life; pain, asthenia, and nausea/vomit at the entry were positively correlated with number of physician activities during the last month of life. The GLM confirmed the significant association between age (contrast estimate = −0.097), pain (contrast estimate = 0.422), and health-care physician services in the end of life. Infusion therapy and cancer treatment at admission were associated with a higher number of physician care services in the end of life (infusion therapy and contrast estimates = 2.621; therapy for advanced cancer and contrast estimates = 2.297). The geographical area was significantly associated with the health-care services by physician: the home care in Centre-South was associated with a lower frequency of physician activities in the last month of life referred to Centre-North (contrast estimate = −4.433).
Table 3. Bivariate correlation and General Linear Model showing the relationship between demographic data, performance status, symptoms, and oncological therapy at the entry and the health-care services performed by physician during the last month of life
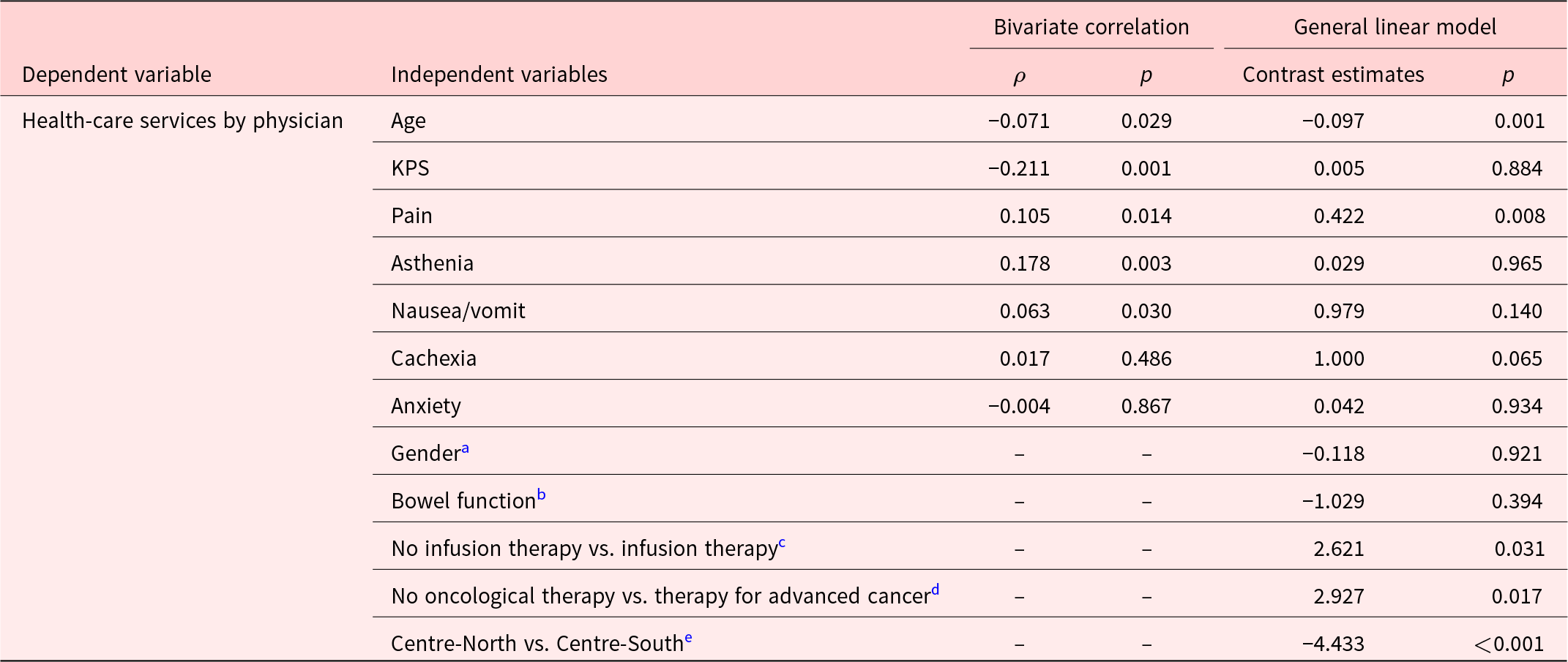
Bivariate correlation was analyzed by Spearman’s Rank correlation, ρ is the Spearman correlation coefficient, p-values of the correlation analysis were adjusted by the Benjamini–Hochberg correction for multiple testing. For the General Linear Model, the independent variable was the number of the health-care services by nurse, and among the independent variables, the following categorical variables have been considered:
a Men (ref) vs. women.
b Regular bowel function (ref) vs. diarrhea or constipation or irregular function.
c No infusion therapy (ref) vs. infusion therapy.
d No oncological therapy (only palliative care) (ref) vs. therapy for advanced cancer.
e Centre-North (ref) vs. Centre-South.
The association between demographic data, KPS, symptoms, therapies at the entry, and the health-care services provided by nurse during the last month of life is shown in Table 4. Age was negatively correlated with the number of nurse services during the last month of life; pain, nausea/vomit, and cachexia at the entry were positively correlated with number of nurse activities during the last month of life. The GLM confirmed the significant association between age (contrast estimate = −0.097), asthenia (contrast estimate = 2.686), anxiety (contrast estimate = 1.515), and health-care nurse services in the end of life. Furthermore, infusion therapy and cancer treatment at admission were associated with a higher number of nurse care services in the end of life (infusion therapy and contrast estimates = 2.621; therapy for advanced cancer and contrast estimates = 2.297). The geographical area was significantly associated with the health-care services by nurse: the home care in Centre-South was associated with a higher frequency of nurse activities during the last month of life referred to Centre-North (contrast estimate = −4.433).
Table 4. Bivariate correlation and General Linear Model showing the relationship between demographic data, performance status, symptoms, and oncological therapy at the entry and the health-care services performed by nurse during the last month of life

Bivariate correlation was analyzed by Spearman’s Rank correlation, ρ is the Spearman correlation coefficient, p-values of the correlation analysis were adjusted by the Benjamini–Hochberg correction for multiple testing. For the General Linear Model, the independent variable was the number of the health-care services by nurse, and among the independent variables, the following categorical variables have been considered:
a Men (ref) vs. women.
b Regular bowel function (ref) vs. diarrhea or constipation or irregular function.
c No infusion therapy (ref) vs. infusion therapy.
d No oncological therapy (only palliative care) (ref) vs. therapy for advanced cancer.
e Centre-North (ref) vs. Centre-South.
The mean number of health-care services per patient provided by physicians and nurses in Centre-North and Centre-South during the last month of life are shown in Table 5. No significant differences were observed considering the sum of the physician and nurse complex clinical activities and other services between the geographical areas. Simple clinical activities were marginally more numerous in Centre-South compared to Centre-North (p = 0.049). Splitting services provided by physicians and nurses, significant differences were observed between geographical areas. Complex and simple clinical activities as well as other activities performed by physicians were more frequent in Centre-North (p = 0.011, p = 0.022, and p = 0.033, respectively), while complex and simple clinical activities as well as other activities performed by nurses were more frequent in Centre-South (p = 0.006, p = 0.017, and p = 0.028, respectively).
Table 5. Complex clinical activities, simple clinical activities, and other activities (total, by physician and nurse) given during the last month of life to patients assisted by ANT in Centre-North and Centre-South

Data are shown as mean of the number of activities per patient in Centre-North and Centre-South. Comparisons between clinical activities given to patients assisted in Centre-North and Centre-South were analyzed by Mann–Whitney U Test. p-values were adjusted by the Benjamini–Hochberg correction for multiple testing.
Discussion
The present study highlighted a different home PC point of inception for patients assisted in Centre-North compared to Centre-South Italy. Patients assisted in Northern Italy had a better performance score, and they were more frequently still in oncological therapy for advanced cancer at the activation of home PC respect to Centre-South. Moreover, Centre-South patients showed higher pain level, more frequently moderate or severe symptoms, and a reduced survival in home PC. Despite the fact that NHS is available over the entire national territory, these results indicate important regional differences characterized by an earlier home PC activation in Centre-North than in Centre-South Italy. This situation seems to reflect a broader gap between North and South in health-care services (Toth Reference Toth2014). The NHS was established in 1978 in Italy in order to provide free health services to all citizens, but the progressive regionalization and the decentralization process led to disparities in the delivery of health-care services near the end of life. In particular, in Southern Italy, more resources have been invested in hospital care, while the Northern regions have enhanced the community and local care (Toth Reference Toth2014).
Regarding home PC network, numerous geographical disparities are still evident, although in the last decade, there has been a gradual consolidation in the provision of PC on the Italian territory (Ministero della Salute 2019; Scaccabarozzi et al. Reference Scaccabarozzi, Amodio and Riva2020). We can hypothesize that fewer available resources can influence the later activation of PC in Southern regions. In fact, the gap in covering the need of PC persists between Centre-Northern and Centre-Southern Italy, where the 4 regions that still fail to provide the level of PC indicated by national standards are located (Fortino et al. Reference Fortino, Tamburo De Bella and Catania2022; Longo et al. Reference Longo, Notarnicola and Rotolo2019).
In addition, sociocultural differences may play a role: larger families, richer social networking, and greater adherence to religious values seem to favor home PC setting, but the scarcity of health-care resources could foster informal patient management, keeping the practice of a later PC activation (Biasco and Surbone Reference Biasco and Surbone2009). A study on 1,289 Italian informal caregiver about actual and preferred place of death of cancer patients (Beccaro Reference Beccaro2006) described Southern regions as more anchored to values such as religiosity and greater centrality of the family and community. This culture, associated with the persistence of a paternalistic approach in medical care, might lower the result in significantly lower number of patients informed about diagnosis and prognosis in Southern Italy. Cultural and religious values unevenly distributed across the Italian territory may lead to difficulties in determining appropriate policy and practice standards regarding end of life and PC, requiring that local policy makers identified PC models adaptable to the specific needs of the patients (Biasco and Baider Reference Biasco and Baider2011). The model of PC should evolve to assist a growing number of patients during the different phases of illness adapting to the increase of elderly population and to the innovation of cancer therapies (Hui et al. Reference Hui, Dev and Bruera2015).
Patients entering in home PC in Centre-North were older at the admission and showed a longer survival. Unhealthy lifestyle risk factors and detrimental habits (obesity, sedentary attitude, and exposure to secondhand smoke) are still more diffused in Southern Italy (Fondazione AIOM 2020; Laura and Lidia Reference Iannucci and Gargiulo2021). These factors may in part explain the younger age for cancer onset in Southern Italy. Moreover, in Italy, a marked heterogeneity remains in secondary prevention services: that is, still strongly delayed in South, where, for instance, the accesses to screening for the early detection of women’s cancers as well as colorectal tumor are considerably less overspread and exploited (Fondazione AIOM 2020; Laura and Lidia Reference Iannucci and Gargiulo2021). Indeed, the retard in cancer diagnosis together with a later admission in home PC program, proven by their worst clinical condition at the entry, shortened the survival of patients assisted in Centre-South. Younger patients seemed to need a more intensive and demanding care in end of life. Previous studies showed that patient age predicted the intensity of service use for home-based physician and nurse visits, with a decrease in intensity as age increased (Cai et al. Reference Cai, Guerriere and Zhao2017; Kirkova et al. Reference Kirkova, Walsh and Rybicki2010). These findings may be in part explained by former data showing that younger cancer patients tend to manifest greater suffering and emotional distress in advanced stages of disease (Kirkova et al. Reference Kirkova, Walsh and Rybicki2010; Krikorian et al. Reference Krikorian, Limonero and Maté2012; Pandey et al. Reference Pandey, Lam and Cheung2021). Moreover, dealing with the end of life of younger patients can represent a higher burden of stress for the family. A recent paper reported that family caregivers with severe distress significantly more often cared for younger patients (≤60 years) entering in specialist inpatient PC (Oechsle et al. Reference Oechsle, Ullrich and Marx2019). An inverse relationship between advanced age and the likelihood of high patient complexity has been observed in PC (Carrasco-Zafra et al. Reference Carrasco-Zafra, Gómez-García and Ocaña-Riola2020), and this finding has been explained by the greater acceptance and adaptation of older patients and their family environment to the situation of terminal illness. Patient’s age may also influence interpretation of situations by the PC professionals. Younger patients could elicit a nonacceptance feeling for a life limiting illness, a higher likelihood of identification by PC staff (Hodiamont et al. Reference Hodiamont, Jünger and Leidl2019), and consequently, a greater apprehension/compassion/attention of PC professionals toward them, increasing the number of physician and nurse visits in the end of life.
Patients showing more difficult-to-control symptoms as well as a low functional score at the entry in the home PC program needed more health-care services. These patients appeared to retain its complexity until the end of life. In particular, poorly controlled pain upon admission was associated with a higher intensity of home physician clinical activities in the end of life. Moreover, infusion therapy upon admission and receiving cancer treatment were predictors of more intense care at the end of life and could be interpreted as aspects increasing the patient complexity. These results highlighted the importance of the accurate identification of highly complex situation at the beginning of home PC program for the early provision of appropriate treatments and tailored interventions (Carrasco-Zafra et al. Reference Carrasco-Zafra, Gómez-García and Ocaña-Riola2020).
Although home PC during the last month of life was managed with a similar number and pattern of health-care services, the distribution of physician and nurse workloads slightly diverged according to geographical area: physicians provided more numerous services in Centre-North, while nurses delivered a higher number of activities in Centre-South. These differences could be related to regional organizational model. There are currently few studies about organizational models in home PC. A recent Canadian study described a home PC model finding that physicians visits during the end of life may improve home deaths and reduce emergency visits and acute hospital admissions compared to provincial normative data (Webber et al. Reference Webber, Valiulis and Tanuseputro2021). It might be interesting to correlate organizational differences in home PC with emergency visits and acute hospital admission in a future study.
The findings of the present paper highlight the importance of considering the complexity of patients’ home care due to the multidimensional nature of their PC needs. Even in a country where a NHS should deliver free, comprehensive and equal health services to all citizens, the provision of at-home PC can differ according to the local organizational model. The sociocultural context has to be carefully evaluated together with the clinical condition of the patient population for a successful at-home PC service delivery.
Finally, this study identifies major regional variation in the process of care. There is a need to better characterize the association between those differences and the patient and family experience, as well as the impact of such differences on the well being of clinicians delivering care under such different environments. Our findings justify these future studies.
Despite many strengths, this study presents some limitations: no social-economics, no accesses to hospital and caregiver data, and no standardized assessment of patient complexity at the admission are available. Hospital and hospice deaths were not considered for analysis. This might add a selection bias to our findings. Future research should investigate the distribution of death location in both geographical areas.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S1478951523000032.
Acknowledgments
The authors gratefully thank Prof. Federico Toth, University of Bologna, for the precious suggestions about the health-care regionalization in Italy.
Author contributions
Biasco Guido and Bruera Eduardo share senior authorship. O.R.: conceptualization, data curation, methodology, formal analysis, writing – original draft, and writing – review and editing. V.S.: conceptualization, project administration, writing – original draft, and writing – review and editing. P.F.: software, data curation, and methodology. P.R.: resources, project administration, and supervision. B.G.: conceptualization, methodology, project administration, supervision, writing – original draft, and writing – review and editing. B.E.: conceptualization, methodology, project administration, supervision, writing – original draft, and writing – review and editing.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interest
The authors declare that they have no conflicts of interest. The authors received no financial support for the research, authorship, and/or publication of this article.
Ethical approval
This retrospective observational study was conducted in full accordance with the Declaration of Helsinki and the Good Clinical Practice, and the study protocol have been approved by Ethical Committee of Area Vasta Emilia Centro (Bologna, Italy) (729-2021-OSS-AUSLBO – 21131; ID 2866) and authorized by a General Direction’s administrative act.









