To the Editor—Hand hygiene improvement is a critical part of effective infection prevention and control (IPC) and therefore constitutes a priority for patient and healthcare worker (HCW) safety. However, hand hygiene compliance in healthcare settings remains suboptimal globally. Reference Lotfinejad, Peters, Tartari, Fankhauser-Rodriguez, Pires and Pittet1 The World Health Organization (WHO) recommends a Multimodal Hand Hygiene Improvement Strategy (MMIS) that includes 5 elements: (1) system change, (2) training and education, (3) monitoring and feedback, (4) reminders in the workplace and communications, and (5) safety climate and culture change. Reference Allegranzi, Gayet-Ageron and Damani2
Systematic reviews have shown an interrelation between safety culture, IPC processes, and the reduction of healthcare-associated infections. Reference Hessels and Larson3,Reference van Buijtene and Foster4 Improving the organizational safety climate has been associated with enhanced hand hygiene compliance and improved patient outcomes, including HAI reduction, particularly vancomycin-resistant enterococci, Staphylococcus aureus, and central-line–associated bloodstream infections.
When the Hand Hygiene Self-Assessment Framework is used to assess the implementation of the WHO MMIS in healthcare facilities worldwide, the Institutional Safety Climate element repeatedly scored the lowest, Reference De, Tartari and Tomczyk5 suggesting that progress in improving safety climate has been slower compared with the 4 other elements of the MMIS. Therefore, we must focus on safety climate and culture change to ensure further and sustainable hand hygiene improvement.
Safety climate, safety culture, and organizational culture are often used interchangeably, but their concepts are distinct. Organizational culture refers to the deeply embedded norms, values, beliefs, and assumptions shared by members within an organization. Safety culture considers leadership and HCW attitudes and values related to the perception of risk and safety. Safety climate is a subset of the overall organizational climate that comprises employee perceptions about the extent to which the organization values safety for patients, HCWs, and the environment.
The institutional safety climate, as part of the hand hygiene MMIS, refers to the environment and perceptions of patient safety issues in a healthcare facility. Hand hygiene improvement is given high priority and is valued at all levels of the organization, including the perception and belief that resources must be provided to ensure hand hygiene, particularly at the point of care. In summary, when a health facility’s “quality and safety climate or culture” values hand hygiene and IPC, both patients and HCWs feel protected and supported.
Prioritizing clean hands at the point of care means using the right agent and the right technique at the right time. People at all levels, including those in healthcare facilities, should focus on the importance of hand hygiene to achieve and promote the appropriate behaviors and attitudes that ultimately save lives.
Considering the importance of this element and given the limited progress in hand hygiene in the last 20 years, World Hand Hygiene Day on May 5, 2022, will promote institutional safety climate and culture change as priorities for hand hygiene improvement. The slogan for this campaign is “Unite for safety—Clean your hands.” To achieve unity for safety, the WHO calls upon all key stakeholders to participate actively (Table 1).
Table 1. World Hand Hygiene Day on May 5, 2022: WHO SAVE LIVES: Clean Your Hands Campaign Calls to Action
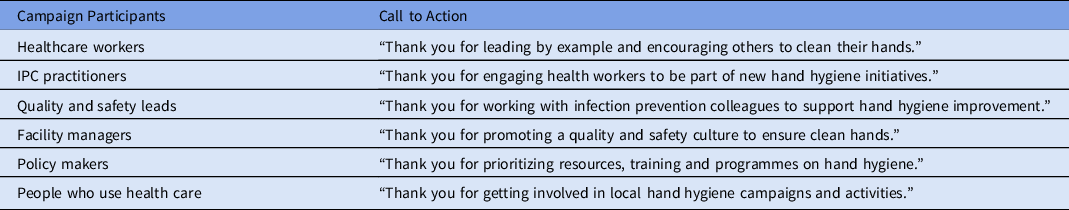
Note. IPC, infection prevention and control.
Further information is available on the webpage WHO SAVE LIVES: Clean Your Hands campaign and World Hand Hygiene Day 2022 (https://www.who.int/campaigns/world-hand-hygiene-day/2022), including an advocacy tool kit offering guidance on the campaign’s objectives, key messages, and how to get involved.
Healthcare facilities can use the Hand Hygiene Self-Assessment Framework to track progress in hand hygiene implementation, including safety climate and culture change, to evaluate improvement over time. This tool can also be used to develop an action plan to ensure long-term sustainability. To ensure that hand-hygiene best practices are prioritized at all levels, several elements are required to create and support an environment that raises awareness about patient safety and quality of care: (1) a team dedicated to the promotion and implementation of hand hygiene in the facility, (2) leadership commitment and active participation, (3) promotional activities, (4) champions and role models, (5) engagement of patients and patient organizations, and (6) institutional targets, accountability, and reporting. Additionally, self-efficacy and individual accountability should be supported in the organization, and role models and champions should be cultivated at every level.
We call on the international community to get involved in World Hand Hygiene Day 2022 (https://www.who.int/campaigns/world-hand-hygiene-day/2022) and to work together to accelerate progress in hand hygiene across health services. Reaffirm your commitment—unite. Talk about hand hygiene and work together to achieve sustainable progress in hand hygiene to improve quality and provide safer care. “Unite for safety—Clean your hands!”
Acknowledgments
The authors alone are responsible for the views expressed in this article; it does not necessarily represent the views, decisions, or policies of the institutions with which they are affiliated.
Financial support
This article was supported by the World Health Organization (WHO) and the Infection Control Program (SPCI) of the University of Geneva Hospitals and Faculty of Medicine, Geneva, Switzerland. Hand hygiene research activities at the SPCI are also supported by the Swiss National Science Foundation (grant no. 32003B_163262).
Conflicts of interest
All authors report no conflicts of interest relevant to this article.




