1. Introduction
Bipolar disorder (BD) is reportedly the sixth leading cause of disability worldwide Reference Moreira, Van Meter, Genzlinger and Youngstrom[1]. It is a chronic psychiatric disease characterized by considerable mood instability, with periods of expansive mood alternating with periods of depressive mood. It causes severe behavioral, relational, social and familial problems [Reference García López, Ezquiaga, de Dios, Agud and Soler2, Reference Huxley and Baldessarini3].
It has already been established that patients with BD have fewer social interactions and more restricted social networks than healthy individuals Reference Bauwens, Pardoen, Staner, Dramaix and Mendlewicz[4]. The psychosocial disability resulting from BD is extensive, and encompasses multiple domains, including work and social interactions, independent living in the community, family adjustment, mortality, and quality of life Reference Sanchez-Moreno, Martinez-Aran, Tabars-Seisdedos, Torrent, Vieta and Ayuso-Mateos[5]. In a review conducted by MacQueen et al. Reference MacQueen, Young and Joffe[6], 30–60% patients with BD had detectable levels of social impairment, occurring in both occupational and social domains, whether or not they had interepisode symptoms. The factors that contribute to psychosocial impairment in BD may be interlinked, creating an effect of functional decline Reference Levy and Manove[7].
Among the most common clinical factors associated with impaired social functioning are episodes of depression Reference Rosa, Bonnn, Vzquez and Reinares[8] or subsyndromal depressive symptoms [Reference Lima, Czepielewski, Gama, Kapczinski and Rosa9, Reference Martino, Marengo, Igoa, Scpola, Ais and Perinot10]. These have been significantly associated with impaired work, family and social life Reference Rosa, Bonnn, Vzquez and Reinares[8]. By contrast, changes in the severity of mania or hypomania have not been consistently associated with variations in social functioning Reference Simon, Bauer, Ludman, Operskalski and Untzer[11].
Research on the functional outcome in BD has uncovered several factors besides mood symptoms that exacerbate psychosocial disability over the course of the illness, including genetics, illness severity, stress, anxiety, and cognitive impairment Reference Levy and Manove[7]. Some studies have found a specific relationship between poor functional outcomes in patients with BD and aspects of cognitive impairment [Reference Sanchez-Moreno, Martinez-Aran, Tabars-Seisdedos, Torrent, Vieta and Ayuso-Mateos5, Reference Burdick, Goldberg and Harrow12]. Cognitive performances (executive function, verbal learning and memory, attention, processing speed) have been associated with patients' level of functioning in both the short and long term [Reference Torres, DeFreitas, DeFreitas, Bond, Kunz and Honer13, Reference Martinez-Aran, Vieta, Colom, Torrent, Sanchez-Moreno and Reinares14]. In a longitudinal study, Burdick et al. Reference Burdick, Goldberg and Harrow[12] concluded that cognitive impairment should be treated as a different dimension from residual or persistent depressive features. They also advocated regular assessments of cognitive status as well as mood symptoms in future studies of functional outcome.
One aspect of cognition that is particularly worth exploring is social cognition. Social cognition is defined as the aspect of cognition that is dedicated to processing social information for adaptive functioning Reference Ochsner and Lieberman[15]. More specifically, it refers to an intricate set of higher-order neuropsychological domains that allow for adaptive behaviors in response to others Reference Amodio and Frith[16]. Four dimensions are usually included in this construct: theory of mind (ToM), emotion processing, social perception and social knowledge, and attribution bias Reference Green, Penn, Bentall and Carpenter[17]. In BD, impairments with medium effect sizes are observed in social cognition [Reference Bora, Bartholomeusz and Pantelis18, Reference Samamé, Martino and Strejilevich19]. Significant ToM dysfunctions, but with modest effect sizes, have been observed in BD, in both remitted and subsyndromal patients, with a greater deficit during acute episodes Reference Bora, Bartholomeusz and Pantelis[18].
There has been abundant research on social cognition in schizophrenia. These studies have revealed that patients exhibit a significant ToM impairment with large effect sizes [Reference Bora, Gken, Kayahan and Veznedaroglu20, Reference Sprong, Schothorst, Vos, Hox and van Engeland21]. This impairment remains significant regardless of the type of task used, and persists even during remission [Reference Bora, Gken, Kayahan and Veznedaroglu20, Reference Pousa, Duñó, Brébion, David, Ruiz and Obiols22, Reference Mehta, Thirthalli and Bhagyavathi23]. Various areas of social cognition (emotion perception, social perception, attributional style, ToM) have been identified as independent correlates of social functioning in schizophrenia Reference Couture, Penn and Roberts[24], and a causal relationship between social cognition deficits and social functioning has been already established in patients Reference Green, Horan and Lee[25]. By contrast, there is a surprising dearth of studies assessing the relationship between baseline social cognition and concurrent baseline social functioning in BD populations.
We set out to provide a comprehensive overview of the relationship between social functioning and social cognition in patients with BD. To the best of our knowledge, this was the first systematic review of the available literature on the subject. The aims were a) to gain an overview of the association between social cognition and functional outcome in BD, b) to explore if this association is present at the different clinical phases of BD, and c) to identify possible gaps within the present literature and directions for future research.
2. Materials and methods
2.1 Search strategy and selection criteria
We conducted a systematic review and data extraction of the published literature in accordance with Preferred Reporting Items for Systematic Reviews and Meta-analyse (PRISMA) guidelines Reference Moher, Liberati, Tetzlaff and Altman[26], to identify studies of the relationship between social cognition and social functioning in BD. Relevant articles were identified through literature searches in the MEDLINE/PubMed, EBSCOHost, Scopus and Google Scholar databases and, as the exploration of social cognition in bipolar disorder has been developed in the early 2000s, we restricted our search strategy to the period between January 2000 and October 2017. We used eight keywords (social cognition, theory of mind, mentalizing, emotion recognition, emotion processing, social perception, social knowledge, and attribution bias) for the social cognition component, and two keywords (social functioning, functional outcome, quality of life) for the functioning component; associated with the term bipolar. The reference lists of the articles we retrieved were also individually explored to look for other relevant reports. We personally contacted the authors of two articles in order to obtain publications that were not available through our university library.
2.2 Inclusion and exclusion criteria
We only selected articles that were available in the English language. Their titles and abstracts were reviewed to determine whether they met the following additional methodological criteria: (1) BD I or BD II population; (2) at least one social cognition task and one functioning scale; and (3) search for a possible connection between social cognition and functioning in BD. As shown in Fig. 1, we initially identified 339 titles and abstracts, but only 20 studies met all the eligibility criteria and were thus included in our review.
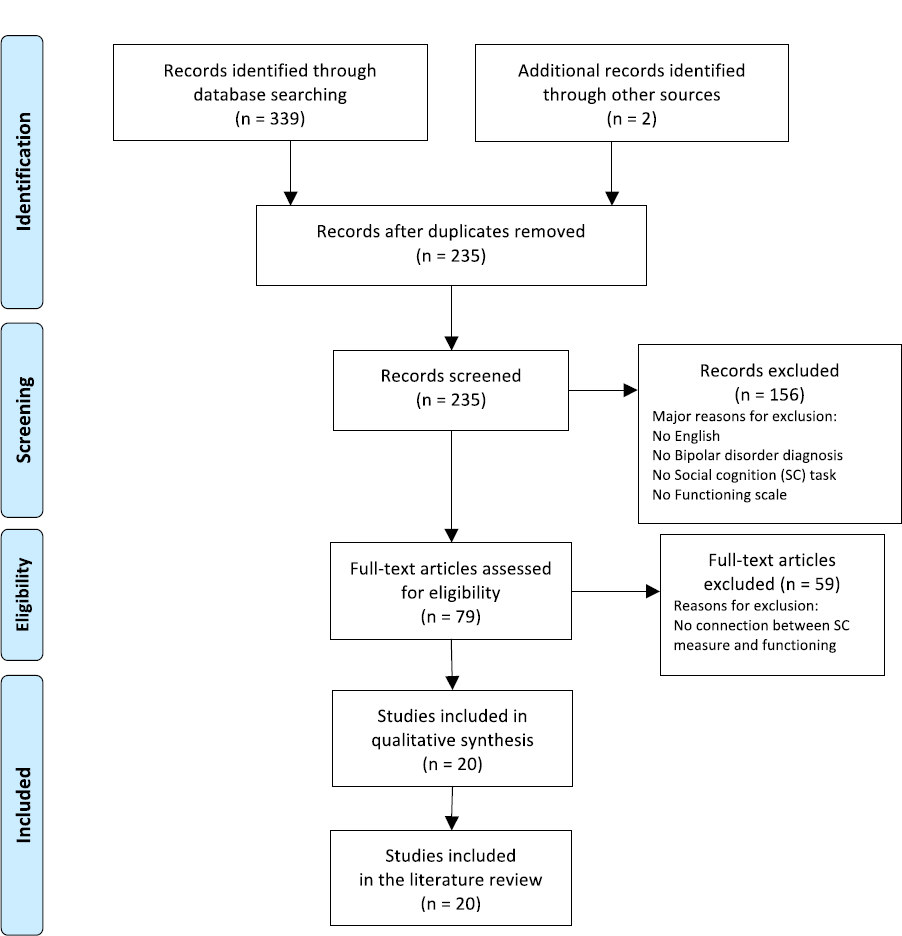
Fig 1. Flowchart of the literature search.
2.3 Data extraction
After duplicate publications were excluded, the first author (MV) screened all the remaining abstracts. In case of indistinctness, full texts were consulted. Two independent reviewers (MV, DRC) read the full text and all ineligible papers were excluded. Disagreements between the reviewers were discussed and resolved during consensus meetings. Information for each eligible study was extracted and tabulated. Extracted data included sample characteristics, method for assessing BD diagnosis, BD type, relevant measures, and main findings. The extraction process was completed independently by MV and checked by DRC.
2.4 Brief listing of the tasks and scales used
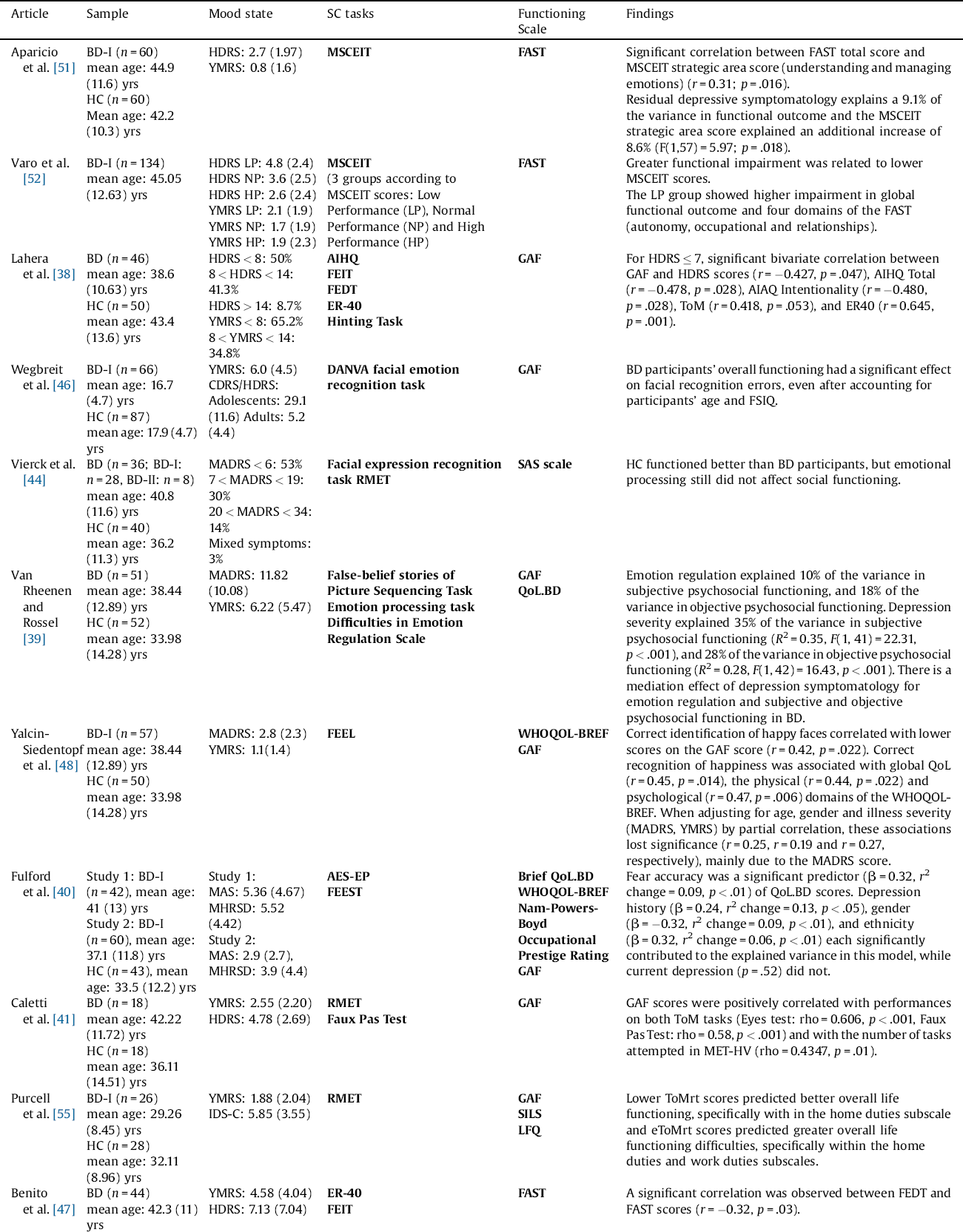
2.4.1 Social cognition tasks
The different tasks used in the studies we included are listed in Table 1. Facial emotion recognition was explored through sets of pictures of facial expressions that had to be labeled. The most commonly used ToM tasks were Reading the Mind in the Eyes Test (RMET; Reference Baron-Cohen, Wheelwright, Hill, Raste and Plumb[27]) and the Faux Pas Recognition Test Reference Baron-Cohen, O’Riordan, Jones, Stone and Plaisted[28]. In the RMET, individuals are instructed to look at a series of photographs of just the eye region of the face, and decide which word out of four best describes what the person in the photo is thinking or feeling. Faux pas recognition involves recognizing faux pas in a series of short stories. We also noted various versions of false-belief and intention tasks. Only two studies assessed attribution bias. Participants first had to complete a questionnaire describing various situations, after which they were asked to devise an explanation for why each situation had occurred. Social perception and social knowledge were not specifically assessed.
Table 1 Sociocognitive domains and tests.

2.4.2 Functional outcome scales
The most consistently used scales were the Global Assessment of Functioning (GAF; from DSM-IV-TR; Reference American Psychiatric Association[29]), the Functioning Assessment Short Test (FAST; Reference Rosa, Sanchez-Moreno, Martinez-Aran, Salamero, Torrent and Reinares[30]), and the Social Adjustment Scale Self-Report (SAS-SR; Reference Weissman and Bothwell[31]).
The GAF is used to assess patients’ overall functional status across psychological, social and occupational domains, via a single anchored measure. With a range extending from positive mental health to severe psychopathology, it is intended to be more of a generic scoring system than a diagnosis-specific one. It has the advantage of being simple to use Reference Aas[32].
Another well attested functioning assessment tool is the FAST Reference Rosa, Sanchez-Moreno, Martinez-Aran, Salamero, Torrent and Reinares[30], which was used in four of the 19 articles included in the review, either on its own or with the GAF. The FAST scale probes six functional domains: financial, interpersonal, leisure, autonomy, occupational and cognitive functioning. The six separate dimensional scores are summed to produce an overall functionality score.
The SAS-SR Reference Weissman and Bothwell[31] assesses a broad range of social domains, focusing on more specific subjects such as work/school role, social/leisure activities, relationship with extended family, marital role, parental role and membership of a family unit.
Similar scales, like the Life Functioning Questionnaire (LFQ; Reference Altshuler, Mintz and Leight[33]), Social and Occupational Functioning Assessment Scale (SOFAS; Reference Morosini, Magliano, Brambilla, Ugolini and Pioli[34]) and Bipolar Disorder Functioning Questionnaire Reference Aydemir, Eren, Savas, Kalkan Oguzhanoglu, Kocal and Devrimci Ozguven[35], were used in a number of the articles we included.
Both the Quality of Life in Bipolar Disorder (QoL.BD; Reference Michalak and Murray[36]) and the World Health Organization Quality of Life-BREF (WHOQOL-BREF; The WHOQOL Group; Reference Harper and Power[37]) are subjective self-report scales. The QoL.BD assesses 10 core domains (physical, sleep, mood, cognition, leisure, social, spirituality, finances, self-esteem, and independence and identity) and two optional domains (education and work). The WHOQOL-BREF consists of 26 items scored in four domains: physical, psychological, social relationships, and environment.
3. Results
In total, 20 studies yielded results on the relationship between social cognition and functional outcome in either euthymic or symptomatic patients with BD-I or BD-II. Nine studies were conducted in euthymic patients with BD. The 11 remaining studies included symptomatic, subsyndromal and euthymic patients. Only one study compared patients across different phases of the disease. Two studies compared patients with BD-I or BD-II. Table 2 summarizes the study designs and the main findings for social cognition and functional outcome in patients with BD.
Table 2 Overview of the studies included in reverse chronological order.
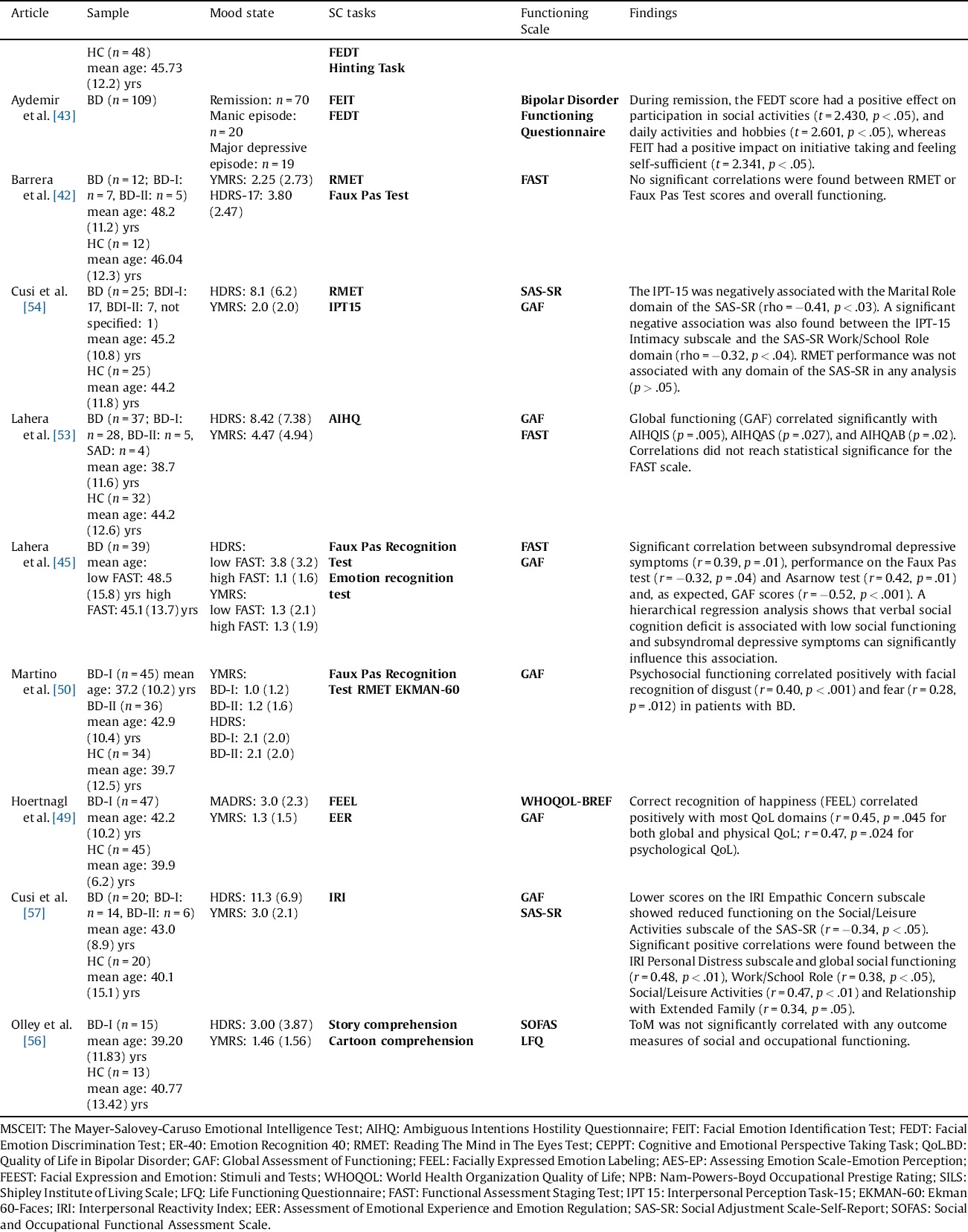
MSCEIT: The Mayer-Salovey-Caruso Emotional Intelligence Test; AIHQ: Ambiguous Intentions Hostility Questionnaire; FEIT: Facial Emotion Identification Test; FEDT: Facial Emotion Discrimination Test; ER-40: Emotion Recognition 40; RMET: Reading The Mind in The Eyes Test; CEPPT: Cognitive and Emotional Perspective Taking Task; QoL.BD: Quality of Life in Bipolar Disorder; GAF: Global Assessment of Functioning; FEEL: Facially Expressed Emotion Labeling; AES-EP: Assessing Emotion Scale-Emotion Perception; FEEST: Facial Expression and Emotion: Stimuli and Tests; WHOQOL: World Health Organization Quality of Life; NPB: Nam-Powers-Boyd Occupational Prestige Rating; SILS: Shipley Institute of Living Scale; LFQ: Life Functioning Questionnaire; FAST: Functional Assessment Staging Test; IPT 15: Interpersonal Perception Task-15; EKMAN-60: Ekman 60-Faces; IRI: Interpersonal Reactivity Index; EER: Assessment of Emotional Experience and Emotion Regulation; SAS-SR: Social Adjustment Scale-Self-Report; SOFAS: Social and Occupational Functional Assessment Scale.
3.1 Functioning and clinical variables
The GAF was the most used scale to assess functioning, as it was measured in 13 of the 19 articles included in the present review. The FAST, the QoL.BD and the WHOQOL-Bref were used in four articles. The SAS-SR was used as a measure of functionality in three of the 19 studies. The LFQ was used in two studies and the other measures (SOFAS, Bipolar Disorder Functioning Questionnaire) in one study each. As expected, functional outcome scores were significantly impaired in patients with BD, compared with healthy controls (HC) [Reference Lahera, Herrera, Reinares and Rullas38–Reference Caletti, Paoli, Fiorentini, Cigliobianco, Zugno and Serati41].
With regard to social functioning, we noted significantly poorer overall functioning among patients with BD than among HC [Reference Caletti, Paoli, Fiorentini, Cigliobianco, Zugno and Serati41, Reference Barrera, Vázquez, Tannenhaus, Lolich and Herbst42]. Mood symptoms seem to be the determining factor for social functioning during acute episodes Reference Aydemir, Akkaya, Uykur and Erol[43], with more severe mood symptoms being associated with poorer social functioning [Reference Lahera, Herrera, Reinares and Rullas38, Reference Van Rheenen and Rossell39, Reference Vierck and Joyce44, Reference Lahera, Ruiz-Murugarren, Iglesias, Ruiz-Bennasar, Herrera and Montes45]. Depressive symptomatology was associated with lower functional outcome across the domains of mood, cognition, leisure, sociability, spirituality, self-esteem, independence, identity, work and the overall score, as well as with GAF scores Reference Van Rheenen and Rossell[39].
Neither the GAF nor the QoL.BD overall scores correlated significantly with clinical variables like age, sex, age at illness onset or diagnosis, subsyndromal manic symptoms (Young Mania Rating Scale, YMRS), employment status or psychosis history [Reference Van Rheenen and Rossell39, Reference Fulford, Peckham, Johnson and Johnson40, Reference Lahera, Ruiz-Murugarren, Iglesias, Ruiz-Bennasar, Herrera and Montes45].
3.2 Functioning and emotion processing
Overall, patients with BD displayed significantly impaired recognition, identification and discrimination of facial emotions, compared with HC [Reference Vierck and Joyce44–Reference Benito, Lahera, Herrera, Muncharaz, Benito and Fernandez-Liria47]. They performed particularly poorly on happiness and disgust recognition [Reference Yalcin-Siedentopf, Hoertnagl, Biedermann, Baumgartner, Deisenhammer and Hausmann48, Reference Hoertnagl, Muehlbacher, Biedermann, Yalcin, Baumgartner and Schwitzer49].
Twelve of thirteen studies reported a connection between functional outcome and emotion processing (i.e., identification of specific emotions, emotion regulation) in euthymic and symptomatic patients. For example, the GAF score correlated positively with the recognition of facial expressions of disgust, fear and happiness in patients with BD [Reference Yalcin-Siedentopf, Hoertnagl, Biedermann, Baumgartner, Deisenhammer and Hausmann48, Reference Martino, Strejilevich, Fassi, Marengo and Igoa50]. Emotion discrimination impairment was significantly correlated with a lower FAST score, showing that deficits in facial emotion discrimination have a negative impact on participation in social activities, as well as on daily activities and hobbies Reference Benito, Lahera, Herrera, Muncharaz, Benito and Fernandez-Liria[47]. In one of the studies, intentionality bias and emotion recognition together explained around 50% of the variance in the GAF score Reference Van Rheenen and Rossell[39]. Deficits in tasks assessing the understanding and management of emotions (MSCEIT strategic area) were also related to a greater social functioning impairment, particularly for the autonomy, occupational and relationships FAST domains [Reference Aparicio, Santos, Jimenez-Lopez, Bagney, Rodriguez-Jimenez and Sanchez-Morla51, Reference Varo, Jimenez, Sole, Bonnin, Torrent and Valls52]. Correct recognition of expressions of happiness was associated with better scores on the physical and psychological dimensions of the WHOQOL-BREF [Reference Yalcin-Siedentopf, Hoertnagl, Biedermann, Baumgartner, Deisenhammer and Hausmann48, Reference Hoertnagl, Muehlbacher, Biedermann, Yalcin, Baumgartner and Schwitzer49]. The ability to identify fear was correlated with higher quality of life ratings, even after accounting for demographic factors and current mood symptoms. The same results were found for self-reported emotion perception after controlling for executive function and demographic factors. This effect, however, was only relevant to wellbeing-not to occupational prestige Reference Fulford, Peckham, Johnson and Johnson[40]. Subjective wellbeing scores were significantly related to lower current depressive symptoms and higher emotion perception scores Reference Fulford, Peckham, Johnson and Johnson[40].
The influence of mood symptomatology on the link between emotion processing and functional outcome was unclear. When depressive symptomatology was included in the statistical analysis (partial correlations or regression analysis), six studies found an effect of depressive symptoms [Reference Lahera, Herrera, Reinares and Rullas38, Reference Van Rheenen and Rossell39, Reference Lahera, Ruiz-Murugarren, Iglesias, Ruiz-Bennasar, Herrera and Montes45, Reference Yalcin-Siedentopf, Hoertnagl, Biedermann, Baumgartner, Deisenhammer and Hausmann48, Reference Aparicio, Santos, Jimenez-Lopez, Bagney, Rodriguez-Jimenez and Sanchez-Morla51, Reference Lahera, Benito, González-Barroso, Guardiola, Herrera and Muchada53]. The correlation between emotion recognition and GAF scores lost significance, mainly owing to the MADRS score Reference Yalcin-Siedentopf, Hoertnagl, Biedermann, Baumgartner, Deisenhammer and Hausmann[48]. Van Rheenen and Rossell Reference Van Rheenen and Rossell[39] found a mediation effect of depression symptomatology on emotion regulation, as well as on subjective and objective psychosocial functioning. However, three studies did not report any effect of depressive symptoms [Reference Fulford, Peckham, Johnson and Johnson40, Reference Benito, Lahera, Herrera, Muncharaz, Benito and Fernandez-Liria47, Reference Martino, Strejilevich, Fassi, Marengo and Igoa50]. In Fulford’s study, fear recognition was a significant predictor of QoL.BD scores. Depression history and sex each significantly contributed to the explained variance, whereas current depression did not.
Only one study directly compared the emotion recognition and discrimination performances of patients with BD across different phases of the disease. This showed that during mood remission, accurate emotion discrimination had a positive effect on participation in social and daily activities and hobbies, while correct emotion identification had a positive impact on taking initiatives and feeling self-sufficient Reference Aydemir, Akkaya, Uykur and Erol[43]. In both depressive and manic episodes, no significant correlation was found between Facial Emotion Identification Test (FEIT) and Facial Emotion Discrimination Test (FEDT) scores and domains of social functioning Reference Aydemir, Akkaya, Uykur and Erol[43].
3.3 Functioning and theory of mind
In the studies we included, the most consistently used task was the RMET, with discrepant results for accuracy in participants with BD compared with controls. Lower scores were reported by some of these studies (54), but most of them failed to reach significance [Reference Caletti, Paoli, Fiorentini, Cigliobianco, Zugno and Serati41, Reference Barrera, Vázquez, Tannenhaus, Lolich and Herbst42, Reference Vierck and Joyce44, Reference Martino, Strejilevich, Fassi, Marengo and Igoa50]. Similarly, some (but not all) RMET task results correlated positively with functioning [Reference Caletti, Paoli, Fiorentini, Cigliobianco, Zugno and Serati41, Reference Purcell, Phillips and Gruber55]. In Caletti et al. Reference Caletti, Paoli, Fiorentini, Cigliobianco, Zugno and Serati[41], GAF scores were positively correlated with performances on the RMET task. In Purcell et al. Reference Purcell, Phillips and Gruber[55], an exploratory analysis revealed that lower RMET response times predicted greater overall life functioning difficulties within the home duties and work duties subscales for the BD group. However, the other studies failed to find a positive correlation between RMET scores and functioning. No significant correlations were found between RMET and either overall functioning or any of the six functional dimensions assessed by the FAST scale in Barrera et al.’s study Reference Barrera, Vázquez, Tannenhaus, Lolich and Herbst[42]. Nor was RMET performance associated with any domain of the SAS-SR in any of the analyses Reference Cusi, Macqueen and McKinnon[54]. The RMET did not contribute to variance beyond neurocognitive impairments, and no other significant associations were found between social functioning and measures of social cognition Reference Martino, Strejilevich, Fassi, Marengo and Igoa[50].
GAF scores were positively correlated with performances on faux pas tasks in Caletti et al. Reference Caletti, Paoli, Fiorentini, Cigliobianco, Zugno and Serati[41], and Lahera et al. Reference Lahera, Ruiz-Murugarren, Iglesias, Ruiz-Bennasar, Herrera and Montes[45]. In Lahera et al. Reference Lahera, Ruiz-Murugarren, Iglesias, Ruiz-Bennasar, Herrera and Montes[45], patients with a low FAST score performed significantly more poorly on the faux pas test, and this result was not confounded by either education level or attention deficit. It should, however, be noted that subsyndromal depressive symptoms can significantly influence this association Reference Lahera, Benito, González-Barroso, Guardiola, Herrera and Muchada[53]. No association between scores on the faux pas task and social functioning was found by Martino et al. Reference Martino, Strejilevich, Fassi, Marengo and Igoa[50] or Barrera et al. Reference Barrera, Vázquez, Tannenhaus, Lolich and Herbst[42].
Scores on the Hinting Task, ToM story task, and ToM and non-ToM cartoon tasks were not significantly correlated with functioning [Reference Lahera, Herrera, Reinares and Rullas38, Reference Benito, Lahera, Herrera, Muncharaz, Benito and Fernandez-Liria47, Reference Olley, Malhi, Bachelor, Cahill, Mitchell and Berk56].
In summary, an association between functioning and ToM was only found in three of the 12 studies that assessed it. Only Lahera et al.’s Reference Lahera, Herrera, Reinares and Rullas[38] study found that the association between a verbal social cognition deficit and low social functioning was significantly influenced by subsyndromal depressive symptoms.
3.4 Functioning and other social cognition tasks
Patients with BD were found to have significantly impaired attributional style in both of the studies that used the Ambiguous Intentions Hostility Questionnaire (AIHQ), scoring significantly higher on the AIHQ-Anger Bias and the AIHQ-Intentionality Bias subscales [Reference Lahera, Herrera, Reinares and Rullas38, Reference Lahera, Ruiz-Murugarren, Iglesias, Ruiz-Bennasar, Herrera and Montes45]. Patients with subthreshold depressive symptoms had higher anger bias and aggression bias scores [Reference Lahera, Herrera, Reinares and Rullas38, Reference Lahera, Benito, González-Barroso, Guardiola, Herrera and Muchada53]. Lahera et al. Reference Lahera, Herrera, Reinares and Rullas[38] found that hostile intent attribution and blame attribution was related to depressive symptoms Reference Lahera, Herrera, Reinares and Rullas[38]. A correlation between social functioning and attributional style was found in both studies. GAF correlated negatively with intentionality [Reference Lahera, Herrera, Reinares and Rullas38, Reference Lahera, Benito, González-Barroso, Guardiola, Herrera and Muchada53], anger, and aggression biases Reference Lahera, Benito, González-Barroso, Guardiola, Herrera and Muchada[53]. Functioning also correlated significantly with attributional style and attributional bias Reference Lahera, Benito, González-Barroso, Guardiola, Herrera and Muchada[53]. Among euthymic patients, significant bivariate correlations were found between the GAF, Hamilton Depression Rating Scale (HDRS), AIHQ Total and AIHQ-Intentionality scores. A regression analysis in a subsample of patients with subsyndromal depressive symptoms showed that the HDRS score and hostility bias were both strongly associated with social functioning Reference Lahera, Herrera, Reinares and Rullas[38].
Exploration of the empathy dimension showed that patients with BD scored lower on the Perspective Taking subscale and higher on the Personal Distress subscale than HC. There were significant positive correlations between the Interpersonal Reactivity Index (IRI) Personal Distress subscale, global social functioning, and the Work/School Role, Social/Leisure Activities, and Relationship with Extended Family domains of the SAS-SR. Moreover, individuals who scored lower on the IRI Empathic Concern subscale also showed reduced functioning in the Social/Leisure Activities domain of the SAS-SR Reference Cusi, Macqueen and McKinnon[57].
A study focusing on social perception found that the BD group performed significantly more poorly than the HC group, suggesting that individuals with BD make impaired judgments about everyday social situations. The Interpersonal Perception Task (IPT-15) Kinship subscale was negatively correlated with the Marital Role domain of the SAS-SR. A significant negative association was also found between the IPT-15 Intimacy subscale and the SAS-SR Work/School Role domain. Moreover, the BD group scored lower than controls on the IPT-15 Kinship and Competition subscales. No significant group differences were found for the IPT-15 Intimacy, Status, and Deception subscales Reference Cusi, Macqueen and McKinnon[54].
4. Discussion
The present literature review was conducted to collate the data available on interactions between functional outcome and social cognition in BD. In the 20 available studies, five social cognitive domains were considered: ToM (both emotional and cognitive), emotion processing, attributional bias, empathy, and social perception. Overall, significant correlations were found between all the social cognitive domains and social functioning.
The ability to identify emotion in other people is critical to social functioning. The majority of the studies revealed a link between social functioning and emotion processing (recognition, discrimination, regulation) in euthymic and symptomatic patients with BD. In the case of facial emotion recognition, three emotions (happiness, fear and disgust) were found to be significantly correlated with functional impairment in BD. Happiness was the emotion least subject to errors in emotion recognition Reference Hoertnagl, Muehlbacher, Biedermann, Yalcin, Baumgartner and Schwitzer[49]. Among patients with schizophrenia, the ability to recognize emotions has been shown to have no direct effect on social interaction in real life Reference Janssens, Lataster, Simons, Oorschot, Lardinois and van Os[58], but patients who erroneously report recognizing relatively high levels of happiness function better socially and have less severe symptoms Reference Cohen, Nienow, Dinzeo and Docherty[59]. Fear recognition was also associated with impaired social functioning in two studies [Reference Fulford, Peckham, Johnson and Johnson40, Reference Martino, Strejilevich, Fassi, Marengo and Igoa50]. Regarding the third emotion, our review revealed that difficulty recognizing the disgust emotion is related to poorer social functioning in the BD population. Similarly, in the schizophrenia literature, the recognition of disgust is significantly associated with functioning. A positive correlation was found in one study between correct recognition of disgust and patients social and professional functioning Reference Hofer, Benecke, Edlinger, Huber, Kemmler and Rettenbacher[60]. There are functional domains for which correct recognition of disgust may be particularly important, such as social and professional interactions. Recognizing it may allow patients to adapt their responses, and may lead them to move toward more socially accepted behaviors Reference Hofer, Benecke, Edlinger, Huber, Kemmler and Rettenbacher[60]. Emotion regulation, and managing and understanding emotions were also correlated with social functioning [Reference Aparicio, Santos, Jimenez-Lopez, Bagney, Rodriguez-Jimenez and Sanchez-Morla51, Reference Varo, Jimenez, Sole, Bonnin, Torrent and Valls52, Reference Van Rheenen and Rossell61]. Emotion regulation was associated with subjective and objective psychosocial functioning, while understanding and managing emotions was associated with the autonomy, occupational and relationship domains. Even though emotion processing explains part of the variance of social functioning, this relationship between emotion processing and functional outcomes seemed to be modulated by depressive symptoms [Reference Lahera, Herrera, Reinares and Rullas38, Reference Lahera, Ruiz-Murugarren, Iglesias, Ruiz-Bennasar, Herrera and Montes45, Reference Yalcin-Siedentopf, Hoertnagl, Biedermann, Baumgartner, Deisenhammer and Hausmann48, Reference Aparicio, Santos, Jimenez-Lopez, Bagney, Rodriguez-Jimenez and Sanchez-Morla51, Reference Lahera, Benito, González-Barroso, Guardiola, Herrera and Muchada53, Reference Van Rheenen and Rossell61]. More than half the studies included patients who either had subsyndromal symptoms or were in a depressive state. When depressive symptomatology was included in the statistical analysis (correlation or regression analysis), the association between emotion processing and social functioning became weaker. Van Rheenen and Rossell Reference Van Rheenen and Rossell[39] demonstrated a mediation effect of depression symptomatology on emotion regulation and subjective and objective psychosocial functioning in BD. It should be noted that in the majority of studies, patients had more subyndromal depressive symptoms than depressive states. The link between psychosocial disabilities and the severity of affective symptoms has already been reported in the literature [Reference Kauer-Sant’Anna, Kapczinski, Andreazza, Bond, Lam and Young62–Reference Rosa, Reinares, Franco, Comes, Torrent and Snchez-Moreno64]. Not only depressive episodes, but also subsyndromal levels, have been shown to be strongly associated with poor social functioning. For example, Simon et al. Reference Simon, Bauer, Ludman, Operskalski and Untzer[11] found that even subtle changes in the severity of depression were associated with statistically significant changes in functional impairment and disability. As suggested by Van Rheneen et al.’s analysis, mood symptoms may be a mediator between emotion processing and social functioning. On the other hand, poor social functioning during depression might also be mediated by the domains proposed by Pulcu and Elliott Reference Pulcu and Elliott[65], including emotion processing. Their hypothesis is that emotion processing and social perception, motivation and reward value processing and social decision making constitute the fundamental sequential stages of social interactions Reference Pulcu and Elliott[65]. In this hypothesis, emotion processing exploration should be included in experimental tasks, integrated with the other domains, for a higher ecological validity and a better understanding of social functioning variability. However, three studies did not find any effect of depressive symptoms [Reference Fulford, Peckham, Johnson and Johnson40, Reference Benito, Lahera, Herrera, Muncharaz, Benito and Fernandez-Liria47, Reference Martino, Strejilevich, Fassi, Marengo and Igoa50]. Only one study directly compared the emotion recognition and discrimination performances of patients with BD across the different phases of the disease. This showed that during mood remission, accurate emotion discrimination has a positive effect on participation in social and daily activities and hobbies, while correct emotion identification has a positive impact on taking initiatives and feeling self-sufficient Reference Aydemir, Akkaya, Uykur and Erol[43]. In both depressive and manic episodes, no significant correlation was found between emotion processing and the domains of social functioning Reference Aydemir, Akkaya, Uykur and Erol[43]. Although the majority of studies highlighted an effect of depressive symptoms on the link between social cognition and social functioning, several studies failed to find one. Further research using a methodology similar to that featured in Aydemir et al.’s study is needed to clarify this aspect.
For ToM, results were more discrepant, with only three of the 12 relevant studies finding a significant relationship between ToM scores (RMET and the Faux Pas test) and functional impairment. Two of these studies found an association between ToM scores and functional outcomes, as assessed by the GAF. The third study reported an association with the social functional domains of home duties and work duties. The one study to assess the impact of clinical symptomatology found an influence of subsyndromal depressive symptomatology on the relationship between verbal social cognition and social functioning. Both the RMET, a mental-state decoding task, and the Faux Pas test are regarded as affective ToM tests Reference Shamay-Tsoory, Shur, Barcai-Goodman, Medlovich, Harari and Levkovitz[66]. They revealed affective ToM impairments that significantly correlated with poorer functioning in BD. The other ToM tasks probe reasoning on cognitive mental states. One plausible explanation for the weaker correlation between cognitive ToM and functioning lies in the crucial differences between affective and cognitive ToM tasks. These constructs are theoretically distinct, in that the former involves noticing something about what another person is experiencing (e.g., recognizing possible emotions in others), while the latter involves forming ideas about others intentions and goals Reference Phalen, Dimaggio, Popolo and Lysaker[67]. Shamay-Tsoory et al. Reference Shamay-Tsoory and Aharon-Peretz[68] suggested that affective and cognitive ToM have different neural bases. Until recently, no definite conclusions could be drawn about ToM impairments in BD, as results were sometimes contradictory. However, in a recently published meta-analysis, Bora et al. Reference Bora, Bartholomeusz and Pantelis[18] found that patients with BD exhibited significant impairment on all ToM tasks, regardless of which ToM domain was being evaluated (affective/cognitive or verbal/visual). The ToM deficit was present regardless of mood state, but was significantly more severe during acute episodes. A recent study focusing on the connection between persecutory delusions and impaired functioning in schizophrenia hypothesized that causality is reversed, and an impoverished social life leads to poorer ToM rather than vice versa Reference Phalen, Dimaggio, Popolo and Lysaker[67]. This could also apply to BD, given that we did not found a strong causal relation. In addition, based on the presence of partial correlations within the results, we can hypothesize that antipsychotic medication may influence the association between ToM performance and social functioning in patients with BD. The effect of antipsychotics on ToM performance has already been considered, but with inconclusive results [Reference Kucharska-Pietura and Mortimer69–Reference Sergi, Green, Widmark, Reist, Erhart and Braff71]. ToM measures may also be too limited and possibly not sufficiently specific to reveal links with functional impairment among patients with BD.
No significant association was found between manic symptomatology itself and either social functioning or social cognition. This lack of an association may be due to methodological limitations. For a start, in the studies included in this review, very few patients had hypomanic or manic symptoms, making comparisons difficult. The majority of social functioning scales are self-report measures. At a clinical level, we can assume that most social functioning scales require patients to have sufficient insight to notice and report their functioning impairments, and this insight is frequently lacking during manic states. Moreover, these scales may not be appropriate for individuals with BD who are experiencing manic episodes. They essentially assess the lack of social interactions and social activities, rather than excessive behaviors. Similarly, the social cognition tasks used are perhaps not the most appropriate. The majority of social cognition tasks used in the literature was designed to assess these processes in individuals with schizophrenia or autism, who have significant impairments in this domain. Like social functioning scales, social cognition tasks are more sensitive to the lack of affective and cognitive inferences. Studies seem to show that social cognitive impairments are less severe in BD than in schizophrenia Reference Bora and Pantelis[72]. These tasks possibly fail to highlight the social cognitive difficulties of patients in manic states, even though they influence functional outcomes.
Some of the limitations of our review are inherent to the review procedure, such as the heterogeneity of the BD samples across the different studies or the heterogeneity of the social cognition tasks they used. In the 20 studies we included, 23 different social cognition tasks were used (12 tasks for emotion processing, eight for ToM). The types of scales used to assess social functioning also constitute a methodological limitation. Most studies used the GAF or the FAST. The GAF score is a measure of general functioning more than a measure of social functioning. When the FAST scale was used, subdimensions were not always analyzed. Some aspects of social cognition may be more closely related to certain aspects of social functioning, as suggested by the results of Aydemir et al., who used a more comprehensive social functioning scale. More exhaustive scales are needed to address multiple aspects of function (e.g., SAS, work performance). The schizophrenia literature focuses on a more specific link between social cognition and social functioning Reference Couture, Penn and Roberts[24]. It is important to understand the specificity of the associations between social cognition and social function versus other domains of function. The heterogeneity of results may also come from the mood dimension, as we included studies regardless of mood state. It would be interesting to conduct a further review that separately assessed manic, depressive and euthymic patients. In order to conduct such a review, more studies are needed, especially on the manic phase. In addition, studies of the link between social functioning and social cognition are needed to compare patients with different subtypes of BD (BD-I, BD-II, rapid-cycling). Two studies included in this review found no differences between BD-I and BD-II on social cognition tasks, but did not carry out separate analyses for the link with social functioning [Reference Benito, Lahera, Herrera, Muncharaz, Benito and Fernandez-Liria47, Reference Martino, Strejilevich, Fassi, Marengo and Igoa50]. A recent meta-analysis of Bora Reference Bora[73] tried to distinguish different clinical subgroups of BD (type I vs. II and history of psychosis) to explore neurocognitive features and found only subtle and not distinctive differences between groups. Most of the cognitive heterogeneity in BD cannot be explained by the proposed subtypes of BD Reference Bora[73] and more studies are needed to adequately distinguish pertinent subgroups. The small number and the cross-sectional design of the studies we included may also restrict the generalizability of our review. Even so, the number of studies included is in line with the literature on these topics in BD Reference Duarte, Becerra and Cruise[74]. Little is known in the literature about the effects of psychotropic drugs on social cognition, and additional information would be of interest Reference Kucharska-Pietura and Mortimer[69]. Moreover, since the available literature points to the potential relevance of attentional and executive functioning to emotion processing in patients with BD Reference Martino, Strejilevich, Fassi, Marengo and Igoa[50], the generalized use of a uniform neuropsychological battery, such as the International Society for Bipolar Disorders-Battery for Assessment of Neurocognition (ISBD-BANC) Reference Yatham, Torres, Malhi, Frangou, Glahn and Bearden[75] could be particularly useful for acquiring an overall cognitive perspective. Finally, despite the evidence that social cognition is a determinant of daily functioning in BD, many of the relevant studies only carried out correlational analyses. Unfortunately, the results of such studies do not provide any information about the directionality of relationships, and explanatory models of associations remain heterogeneous and need to be developed Reference Martinez-Dominguez, Penades, Segura, Gonzalez-Rodriguez and Catalan[76].
5. Conclusions
Our review suggests that impaired functioning in the BD population is associated with social cognition deficits, especially in the domain of emotion processing. ToM results in the literature are more discrepant, reflecting the heterogeneity of the tasks and, possibly, of the processes involved. The involvement of mood state also deserves to be analyzed further, as depressive symptoms may mediate or moderate the relationship we found between social cognition and functioning. Further studies should be conducted in this specific area to understand the role of social cognition in social functioning and, possibly, to improve quality of life through social cognition training Reference Tas, Brown, Cubukcuoglu, Aydemir, Danaci and Brne[77].
Disclosure
The authors declare that they have no conflicts of interest affecting this article.
This research received no specific grant from any funding agency, in either the commercial or not-for-profit sectors.
Acknowledgements
The authors thank all the people who took part in this study and Elizabeth Portier for reviewing the English style.






Comments
No Comments have been published for this article.