Approximately 700 000 US military personnel were deployed to the Middle East during the 1991 Persian Gulf War. Unique aspects of that deployment included a relatively large proportion of reservists and National Guard units, exposure of deployed personnel to potentially harmful natural and manufactured environmental toxins (Presidential Advisory Committee on Gulf War Veterans' Illnesses, 1996) and relatively few casualties. Epidemiological studies have demonstrated greater psychological symptoms and disorders among these personnel compared with Gulf War-era veterans who were not deployed to the Persian Gulf region (Reference Perconte, Wilson and PontiusPerconte et al, 1993; Reference Sutker, Uddo and BraileySutker et al, 1993; Reference Southwick, Morgan and DarnellSouthwick et al, 1995; Iowa Persian Gulf Study Group, 1997; Reference Fukuda, Nisenbaum and StewartFukuda et al, 1998; Reference Proctor, Heeren and WhiteProctor et al, 1998; Reference Stuart and BlieseStuart & Bliese, 1998; Reference Ishoy, Suadicani and GuldagerIshoy et al, 1999; Reference Unwin, Blatchley and CokerUnwin et al, 1999; Reference Ismail, Kent and BrughaIsmail et al, 2002). The National Health Survey of Gulf War Era Veterans and Their Families (Reference Eisen, Kang and MurphyEisen et al, 2005) was designed to collect epidemiological data at several time points to assess the prevalence of medical and psychological conditions in both deployed and non-deployed veterans. Beginning in 1995, postal and telephone surveys were conducted of 15 000 deployed veterans and 15 000 non-deployed veterans. Those who had been deployed to the Gulf War reported more psychological symptoms, poorer functional impairment and poorer health-related quality of life compared with the non-deployed group (Reference Kang, Mahan and LeeKang et al, 2000). The study reported here evaluated a subset of these veterans using face-to-face psychological examinations conducted between 1998 and 2001. Based on retrospective report, we calculated the prevalence of mental disorders beginning during the deployment period, and their continued prevalence 10 years later.
METHOD
Study population and recruitment
Recruitment for the survey phase of the National Health Survey of Gulf War Era Veterans and Their Families performed in 1995 has been described elsewhere in detail (Reference Eisen, Kang and MurphyEisen et al, 2005). Briefly, the US Department of Defense's Defense Manpower Data Center identified the entire cohort of 693 826 deployed veterans and approximately half (800 680) of the non-deployed veterans who were in military service between September 1990 and May 1991. A total of 15 000 deployed and 15 000 non-deployed veterans were solicited to participate in the study. To ensure that female, reservist and National Guard personnel were adequately represented, a stratified random sampling method was applied to each group so that a fifth of each sample were women (3000), a third were reservists (5000) and approximately a quarter were members of the National Guard (4000).
For the examination phase of the study, a list of potential participants was created by random selection from the 11 441 deployed and 9476 non-deployed veterans who participated in the 1995 study, stratified by deployment status and region of last known residence at the time of the original survey (based on home telephone area code). Potential participants were assigned to the participating Veterans Affairs (VA) medical centre closest to their home. Participating medical centres were located in Albuquerque, Baltimore, Birmingham, Boston, Cincinnati, Hines (Chicago), Houston, Miami, Minneapolis, New Orleans, New York, Portland (Oregon), Richmond, Salt Lake City, San Diego and St Louis. Recruitment packages that included an introductory letter, a detailed explanation of the purpose and nature of the study, a letter of intent form and a pre-addressed stamped return envelope were mailed to the veterans. Because of lower participation among non-deployed veterans, an additional 799 were solicited to obtain examined groups of equal size.
Signed letters of intent were returned to the Hines VA Cooperative Studies Program Coordinating Center, which forwarded them to the participating VA medical centre to which the veteran was assigned. Site personnel then contacted the participant and scheduled the examination. Travel, hotel, per diem costs and an honorarium of $200 were provided by the research project. The protocol and consent form were approved by the Hines Cooperative Studies Program Human Rights Committee and the institutional review board at each individual site and at the Brockton Veterans Affairs Medical Center. Participants gave signed informed consent shortly before the start of the examination.
Mental health assessment
Mental health was assessed using two methods: structured clinical interviews, yielding mental disorder diagnoses; and paper-and-pencil, self-report measures of current symptoms. In the structured interviews, participants were asked about their lifetime experience of different symptoms, including the times when symptom constellations started and stopped. With these data, onset prevalence for disorders was calculated for the period ranging from 1 January 1991 to 30 July 1993, which encompasses the period from the beginning of the conflict to the date beyond which no further deployment to the Middle East occurred. Disorders with an onset during this period are referred to as Gulf War-era onset disorders. To assess the course of these mental disorders, prevalence rates were assessed for war-era onset disorders still present within 1 year of the current study, approximately 10 years after the resolution of the Gulf War. We also calculated the prevalence of disorders with onset prior to January 1991 and overall lifetime prevalence.
Mental disorders
Diagnoses of post-traumatic stress disorder (PTSD) were made with the Clinician Administered PTSD Scale (CAPS; Reference Blake, Weathers and NagyBlake et al, 1995), a structured interview yielding PTSD diagnoses according to DSM–IV criteria (American Psychiatric Association, 1994). Participants first indicated their exposure to stressful life events on a standard life events checklist; a follow-up interview then assessed whether these events met criterion A (exposure to a traumatic event). This assessment was not externally validated through record review. The participant was then asked to choose the two most stressful of the events reported. The symptom interview focused on the presence of any PTSD symptoms related to the two events, over the veteran's lifetime as well as in the past month. Symptoms were assessed regardless of whether the selected events met criterion A, but the disorder was only diagnosed if both criterion A and the symptom criteria were met. Participants could receive up to two diagnoses of PTSD associated with the two events; however, cases of PTSD in the time intervals discussed above were calculated per individual. We asked whether events were related to the Gulf War. In assessing the presence of war-era onset PTSD 10 years after the war, we assured that PTSD diagnoses were linked by event (e.g. if a person had war-era onset PTSD from event 1, we checked the duration of the PTSD related to event 1 to determine whether it was present 10 years later). The remaining DSM–IV Axis I psychiatric diagnoses were made using the Composite International Diagnostic Interview (CIDI; Reference Andrews and PetersAndrews & Peters, 1988), a computerised structured interview which yields diagnoses based on DSM–IV criteria. Diagnoses were then categorised according to the DSM–IV classification system.
Symptoms
Current psychiatric symptom severity was assessed using three scales. Higher scores on all three scales indicate greater symptoms. The PTSD Checklist (Reference Blanchard, Jones-Alexander and BuckleyBlanchard et al, 1996) was used to assess PTSD symptoms in the past month using 17 items rated on a scale of 1 to 5. We report the mean total score and the percentage of probable PTSD cases, defined by a total score of 50 or greater. The Beck Depression Inventory II (BDI–II; Reference Beck, Steer and BrownBeck et al, 1996) was used to assess depressive symptoms in the past 2 weeks using 21 items rated on a scale of 0 to 3. We report the mean total score and the percentage of cases in the following categories of depression severity: minimal (total score 0–13), mild (14–19), moderate (20–28) and severe (29–63). The Beck Anxiety Inventory (BAI; Reference Beck and SteerBeck & Steer, 1993) was used to assess anxious symptoms in the past week using 21 items rated on a scale of 0 to 3. We report the mean total score and the percentage of cases in the following categories of anxiety severity: minimal (total score 0–7), mild (8–15), moderate (16–25) and severe (26–63).
Quality of life
Healthcare quality of life
The 36-item Short Form Health Survey (SF–36; Reference McHorney, Ware and RaczekMcHorney et al, 1993; Reference Ware, Snow and KosinskiWare et al, 1993; Reference Kazis, Miller and ClarkKazis et al, 1998) was used to assess mental health-related quality of life in the 4 weeks preceding the evaluation. Items focused on current perception of health and normal daily functioning were rated on a Likert scale, and were summed into physical and mental component scores. Scores were standardised to a mean of 50 and standard deviation of 10; higher scores indicate better quality of life. We have previously reported on the physical component scores (Reference Eisen, Kang and MurphyEisen et al, 2005), and report on only the mental component in this paper.
General quality of life
The Quality of Life Inventory (QoLI; Reference FrischFrisch, 1994) was used to measure general life satisfaction. It enquires about 16 areas of life, which are rated by participants on importance to their overall happiness and satisfaction with the area. The 16 areas of life in the inventory are health, self-esteem, goals and values, money, work, play, learning, creativity, helping, love, friends, children, relatives, home, neighbourhood and community.
Combat exposure
The Combat Exposure Scale (CES; Reference Wolfe, Proctor and DavisWolfe et al, 1998) was expanded from the original version of the scale (Reference Gallops, Laufer, Yager, Egendorf, Kadushin and LauferGallops et al, 1981), which focuses on the presence and frequency of a range of war-zone stressors. Expanded items reflect war-zone events specific to service in the Gulf War, which in some cases extend beyond combat. Given that traditional combat in the Gulf War lasted only 5 days and did not involve all personnel, the expanded items inquire about less traditional war-zone events compared to the original items. The questionnaire was self-administered, and participants responded whether they experienced each event on the list. The responses are ‘no’ (rated 0), ‘once or twice’ (1) or ‘three or more times’ (2). The total score on all 33 items was used as a measure of war-zone stressor exposure.
Training and quality control
Research assistants received CIDI training from Dr L. N. Robins and her staff (Dr Robins is the author of the Diagnostic Interview Schedule on which the CIDI is based). Training in use of the CAPS was conducted by Dr Frank Weathers of the Brockton Psychometrics Laboratory, Brockton, Massachusetts, USA; one of the creators of the interview, and he co-rated 20 CAPS interviews for interrater reliability. One of the authors (R.T.) supervised ongoing ratings and overall quality through weekly calls and periodic reviews.
Statistical analyses
Sample size calculations and participant recruitment efforts for this project were based on the predicted prevalence of disease among veterans. The achieved sample size provided 80% power to detect prevalence differences of 2.0% for PTSD (assumed deployed veterans prevalence 2.8%, non-deployed veterans 0.8%), and a mean difference of 1.5 (s.d.=10) for the SF–36 mental component scores. Interrater reliability was assessed with intraclass correlations for CAPS continuous variables (frequency and intensity) for symptom clusters and individual symptoms and with kappa coefficients for PTSD diagnoses.
The sampling design is a stratified random sample with unequal probabilities of selection within combinations of the strata: deployment status, gender and duty type (active service v. reserve or National Guard). Therefore, population prevalence or mean estimates for all analyses were obtained using SUDAAN software developed for the analysis of complex survey data (SUDAAN release 9.0, Research Triangle Institute, North Carolina, USA). Sample weights used in SUDAAN were based on the probability of selection combined with the probability of response. For continuous outcomes, t-tests and linear regression models compared mean responses between groups. Logistic regression models were developed for dichotomous and ordinal polytomous outcomes. The covariates considered in the multiple regression models were age, gender, ethnicity (White v. other), years of education (less than 12 years v. 12 years or more), duty type (active v. reservist/National Guard), service branch (army/marine v. navy/air force) and rank (enlisted v. officer). Candidate covariates were deleted for particular models when they caused computational problems preventing model calculation. Odds ratios, 95% confidence intervals and P values are reported for dichotomous outcomes. Comparisons of categorical data and continuous data with adjustment for covariates were based on the Wald F-statistic. For continuous data without adjustments, P values were based on the two-sample t-test.
RESULTS
Participant characteristics
Both the deployed and the non-deployed veteran groups were 78% male. The deployed group (mean age 38.9 years, s.d.=8.8) were nearly 2 years younger than the non-deployed group (40.7 years, s.d.=9.6; P<0.01), were more likely to be African–American, had lower levels of education and were less likely to be married compared with the non-deployed group. The groups did not differ in terms of the percentage still on active duty (deployed, 7.8%; non-deployed, 8.5%), mean income level, 1991 unit component breakdown or 1991 military branch. Those in the deployed group were less likely to be officers compared with the non-deployed group. Differences between the groups reflect true differences between the two cohorts (Reference Kang and BullmanKang & Bullman, 2001).
Participation rates
Of the 1996 deployed veterans who were solicited to participate, 53% (1061) were examined; of 2883 non-deployed veterans who were solicited to participate, 39% (1128) were examined. Despite intensive efforts, 12.8% of deployed veterans and 15.2% of non-deployed veterans were not located. In addition, 34.1% of locatable deployed veterans and 45.6% of non-deployed veterans either never returned their participation letter, or an examination could not be scheduled. Because of the lower participation rates by non-deployed veterans, more people in this category (n=799) were recruited to achieve the desired sample size of 1000 per group.
Participation bias
Historical military service data, obtained in 1991 for all solicited veterans from the US Department of Defense's Manpower Data Center, were used to evaluate participation bias on socio-demographic variables. We compared participants and non-participants in each group (deployed and non-deployed) and then used the Breslow–Day homogeneity of odds ratios test to assess the hypothesis that the odds ratios generated for the two groups were equal.
Participation bias for demographic characteristics is reported in more detail elsewhere (Reference Eisen, Kang and MurphyEisen et al, 2005). Briefly, we found that participants were nearly 2 years older than non-participants, and that White people, women, reservists and National Guard members were significantly more likely to participate. In addition, officers and army personnel were more likely to participate than non-officer and non-army personnel, although these differences were not uniformly significant. We also calculated participation bias for mental health characteristics available from the 1995 survey. Dichotomous data were available on smoking (‘Have you smoked in the past 12 months?’), drinking (‘Do you drink alcohol?’), depression (‘Have you experienced in the past year: difficulty getting to sleep; excessive sleepiness; awaken feeling tired; anxious, irritable, or upset; been depressed or blue; difficulty concentrating or reasoning, memory loss?' ‘Have you experienced in the past 6 months: unintended loss of more than 10 pounds, unintended gain of more than 10 pounds?’) and PTSD symptom severity (the PTSD Checklist). Participants did not differ from non-participants in each group on smoking, drinking, weight loss or PTSD symptom severity. Participants in each group more frequently reported the other mood symptoms; however, the degree of participation bias did not differ quantitatively between the groups. The only characteristic that yielded a statistically significant difference in the odds ratios generated by the two groups was 1995 active duty status (Reference Eisen, Kang and MurphyEisen et al, 2005). Overall, the degree of participation bias was independent of deployment status.
Reliability of CAPS
Interrater reliability was calculated for 32 continuous CAPS symptom variables (frequency and intensity ratings for symptom clusters B, C and D, and total symptoms, current and lifetime, for two events). Excellent interrater reliability was demonstrated by high (0.90 or higher) intraclass correlations for 31 of these variables and one moderately high (0.86) intraclass correlation (event 1 cluster C intensity). The kappa coefficient was 0.77 for the diagnosis of current PTSD and 0.79 for the diagnosis of lifetime PTSD, indicating good reliability.
Prevalence of all war-related mental disorders
The prevalence of any one Gulf War-era onset mental disorder (i.e. reported initial onset between 1 January 1991 and 30 July 1993) was significantly higher among the deployed veterans than among the non-deployed veterans (Table 1). The broader categories of mood disorders and anxiety disorders were also significantly more prevalent among the former group. Specific disorders within those categories that were significantly more prevalent among the deployed veterans compared with non-deployed veterans were major depression, PTSD, panic disorder and specific phobias. Of the deployed veterans with a PTSD onset in the war-era, in 93% of cases the PTSD was related to a Gulf War event. Two less common disorders also differed significantly between groups: pain disorder was significantly more common in the deployed veteran group, and brief psychotic disorder was significantly more common among the non-deployed veterans.
Table 1 Prevalence of mental disorders with Gulf War-era onset
| Unadjusted | Adjusted 1 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Deployed % | Non-deployed % | P 2 | OR (95% CI) | P 2 | OR (95% CI) | |||||
| All anxiety disorders | 9.4 | 2.4 | <0.0001 | 4.17 (2.36–7.38) | <0.0001 | 4.43 (2.49–7.88) | ||||
| PTSD | 6.2 | 1.1 | <0.0001 | 5.70 (2.69–12.04) | <0.0001 | 5.78 (2.62–12.74) 3 | ||||
| Non-PTSD anxiety disorders | 4.3 | 1.4 | 0.004 | 3.17 (1.43–6.99) | 0.001 | 3.79 (1.80–7.99) | ||||
| Generalised anxiety disorder | 0.9 | 0.0 | NA | NA | NA | NA | ||||
| Agoraphobia without panic | 0.7 | 0.0 | NA | NA | NA | NA | ||||
| Panic disorder | 1.2 | 0.1 | 0.01 | 8.93 (1.58–50.31) | 0.006 | 10.53 (1.99–55.80) 3 | ||||
| Specific phobias | 1.9 | 0.8 | 0.12 | 2.32 (0.80–6.70) | 0.04 | 2.84 (1.08–7.48) | ||||
| Social phobia | 0.6 | 0.5 | 0.72 | 1.37 (0.24–7.93) | 0.57 | 1.61 (0.31–8.31) 4 | ||||
| Obsessive–compulsive disorder | 0.6 | 0.1 | 0.12 | 6.35 (0.64–63.41) | 0.07 | 8.90 (0.84–94.71) 5 | ||||
| Substance dependence | 7.9 | 4.8 | 0.04 | 1.71 (1.03–2.84) | 0.42 | 1.25 (0.73–2.16) 5 | ||||
| Nicotine dependence | 3.1 | 2.2 | 0.35 | 1.43 (0.68–3.01) | 0.88 | 1.06 (0.48–2.34) 5 | ||||
| Alcohol dependence | 4.3 | 3.0 | 0.24 | 1.48 (0.77–2.87) | 0.96 | 1.05 (0.51–2.16) | ||||
| Illicit substance dependence | 0.9 | 0.6 | 0.61 | 1.48 (0.33–6.66) | 0.81 | 1.20 (0.27–5.39) 6 | ||||
| Mood disorders | 7.5 | 4.1 | 0.02 | 1.89 (1.13–3.15) | 0.02 | 1.90 (1.09–3.32) | ||||
| Major depression | 7.1 | 4.1 | 0.03 | 1.78 (1.06–2.99) | 0.04 | 1.81 (1.03–3.19) | ||||
| Dysthymia | 0.04 | 0.0 | NA | NA | NA | NA | ||||
| Bipolar disorder | 0.36 | 0.0 | NA | NA | NA | NA | ||||
| Somatic disorders | 1.0 | 0.3 | 0.14 | 3.40 (0.66–17.50) | 0.12 | 4.12 (0.70–24.15) | ||||
| Somatisation disorder | 0.1 | 0.01 | 0.26 | 4.93 (0.31–78.34) | 0.18 | 5.03 (0.48–53.32) 7 | ||||
| Conversion disorder | 0.03 | 0.04 | 0.94 | 0.91 (0.06–14.46) | 0.94 | 0.91 (0.06–14.46) 8 | ||||
| Pain disorder | 0.9 | 0.01 | 0.0001 | 68.04 (8.04–575.54) | <0.0001 | 91.66 (10.52–798.21) | ||||
| Body dysmorphic disorder | 0.04 | 0.3 | 0.09 | 0.16 (0.02–1.37) | 0.14 | 0.17 (0.02–1.74) | ||||
| Psychotic disorders | 0.6 | 0.9 | 0.54 | 0.65 (0.17–2.55) | 0.39 | 0.54 (0.13–2.23) | ||||
| Schizophrenia | 0.3 | 0.0 | NA | NA | NA | NA | ||||
| Schizophreniform disorder | 0.0 | 0.0 | NA | NA | NA | NA | ||||
| Schizoaffective disorder | 0.0 | 0.0 | NA | NA | NA | NA | ||||
| Delusional disorder | 0.04 | 0.0 | NA | NA | NA | NA | ||||
| Brief psychotic reaction | 0.2 | 0.9 | 0.04 | 0.26 (0.07–0.96) | 0.04 | 0.23 (0.06–0.91) 9 | ||||
| Eating disorders | 0.03 | 0.0 | NA | NA | NA | NA | ||||
| Anorexia nervosa | 0.0 | 0.0 | NA | NA | NA | NA | ||||
| Bulimia nervosa | 0.03 | 0.0 | NA | NA | NA | NA | ||||
| One or more mental disorders 10 | 18.1 | 8.9 | <0.0001 | 2.28 (1.59–3.27) | 0.0001 | 2.12 (1.44–3.11) | ||||
NA, not applicable; PTSD, post-traumatic stress disorder
1. Adjusted for differences in age, gender, ethnicity (White v. other), years of education (less than 12 v. 12 or more), duty type (active v. reserve/guard), service branch (army/marine v. navy/air force) and rank (enlisted v. officer) unless otherwise noted
2. Critical value is 0.05
3. Model does not include adjustment for education
4. Model does not include adjustment for education or rank
5. Model does not include adjustment for rank
6. Model does not include adjustment for age or rank
7. Model does not include adjustment for age, gender, ethnicity, education or duty type
8. Model does not include any of the covariates listed above
9. Model does not include adjustment for education, duty type or service branch
10. Includes all diagnoses in the table except nicotine dependence
Prevalence of war-related mental disorders 10 years later
War-era onset disorders that were significantly more prevalent among deployed veterans than among non-deployed veterans and had a prevalence of at least 1% in both groups were examined for their continued presence in the year prior to the examination (i.e. if the disorder began during the war, was it currently active within 1 year of our examination, approximately 10 years later). In the case of recurrent episodes of major depression, there would have been an initial episode in the war-era and an episode in the year prior to the examination, however, the episodes might have come and gone in the intervening period. We combined non-PTSD anxiety disorders into one group to yield a larger event rate for further analyses. Using our whole sample, war-era onset major depression continued to be significantly more prevalent 10 years later in the deployed veterans group (3.2%) compared with the non-deployed group (0.8%, adjusted P=0.01) (Fig. 1). Comparing the odds ratios representing degree of remission, deployed veterans were 3.33 times more likely to be in an episode of depression 10 years later, whereas non-deployed veterans were significantly more likely to be in current remission (P=0.048). To determine whether severity of initial depression at the time of the war might have differed in the two groups, we examined the severity of depression (mild, moderate, severe) during that period and found that it did not differ between the two groups (P=0.89). We also examined the presence of comorbid psychiatric disorders with warera onset. There was a trend for deployed veterans with depression to be more likely to have a comorbid psychiatric disorder (45.6%) than non-deployed veterans with depression (25.8%, P=0.11) and the deployed group displayed a trend for having more anxiety disorders, including PTSD (P=0.07).
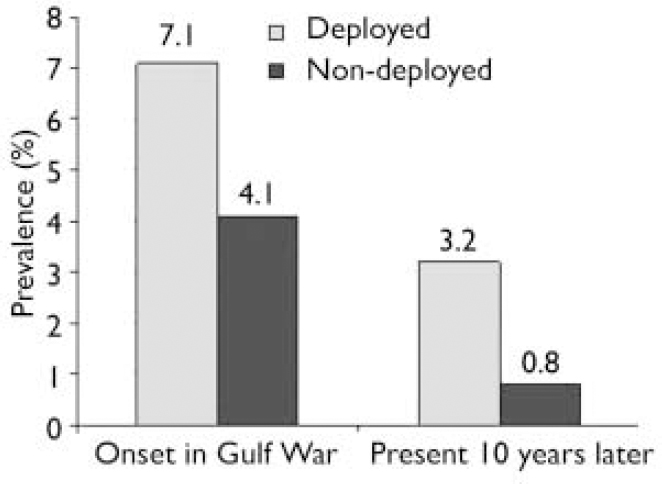
Fig. 1 Depression: prevalence of war-related major depression in the Gulf War period and 10 years later.
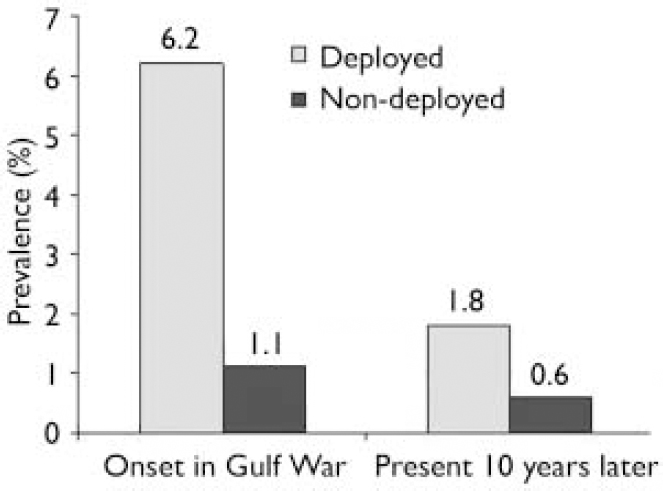
Fig. 2 Post-traumatic stress disorder:prevalence of war-related disorder in the Gulf War period and 10 years later.
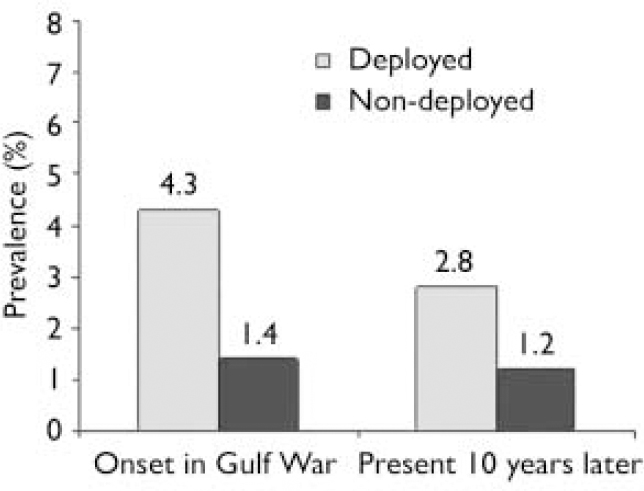
Fig. 3 Anxiety disorders: prevalence of war-related anxiety disorders (not post-traumatic stress disorder) in the Gulf War period and10 years later.
War-era PTSD prevalence did not differ statistically between deployed (1.8%) and non-deployed (0.6%) groups (adjusted P=0.12) 10 years later, although the rate among deployed veterans was three times higher than in the non-deployed group (Fig. 2). Remission rates did not differ significantly between the groups (P=0.14). Prevalence of war-era onset of non-PTSD anxiety disorders differed significantly between deployed veterans (2.8%) and non-deployed veterans (1.2%; adjusted P=0.01) 10 years later, with the rate among the deployed veterans being twice that among the non-deployed group (Fig. 3). There was no significant difference in degree of remission between the groups (P=0.36).
Use of medication for depression and anxiety
We examined medication use at the time of assessment in veterans having war-era onset mental disorders to determine whether those with remitted disorders were being successfully treated with medication. Of the 44 veterans (36 deployed, 8 non-deployed) with war-era onset depression who still met criteria within a year of our assessment, there was no significant difference in the percentage taking any antidepressant medication (deployed 17.1%, non-deployed 33.4%; P=0.43), although nearly twice the number of non-deployed veterans were taking medication. Of the 89 veterans with war-era onset depression whose depression had remitted, those who had been deployed (13.1%) were taking antidepressant medication at over twice the rate of non-deployed veterans (5.2%), but these rates were not statistically different (P=0.25). Overall, 14.9% of deployed veterans and 10.7% of non-deployed veterans with war-era onset depression took medication for depression at the time of their assessment. For those with any lifetime depression, 20.7% of those who were deployed and 14.2% of those who were not took medication for depression at the time of assessment.
Veterans diagnosed with PTSD and/or other anxiety disorders were examined for their use of both anti-anxiety and antidepressant medications, as both are commonly prescribed for anxiety disorders. We combined PTSD and other anxiety disorders for this analysis because the total sample size (n=135: PTSD only, n=73; other anxiety only, n=47; both, n=15) was similar to the sample size with warera onset depression (n=133) and we were concerned that by analysing PTSD (n=88) separately from other anxiety disorders (n=62) the cells would be too small for a meaningful analysis to be performed. Of the 78 veterans (deployed, n=61; non-deployed, n=17) with war-era onset anxiety disorders who still met criteria within 1 year of our assessment, a higher percentage of non-deployed (22.9%) than deployed (12.4%) veterans were taking medication for anxiety, but the rates were not statistically different (P=0.40). Of the 57 veterans with war-era onset anxiety whose disorders had remitted, significantly fewer deployed veterans (4.9%) took medication in comparison with non-deployed veterans (37.4%; P=0.02). Overall, 8.3% of deployed veterans and 26.6% of non-deployed veterans with war-era onset anxiety disorders were taking specific medication for anxiety at the time of assessment. For those with any lifetime anxiety disorder, 17.2% of deployed veterans and 15.4% of non-deployed veterans took medication for depression at the time of assessment. We conducted a Cochran–Mantel–Haenszel Test in SUDAAN using the entire cohort to examine if there was differential use of medication for anxiety in the two study groups. Among the deployed group there was no difference in medication usage between those with and without anxiety disorders, but among the non-deployed group those with anxiety disorders were 6.15 times more likely to take medications than those without an anxiety disorder (P=0.04).
Prevalence of mental disorders prior to the war and lifetime prevalence
We examined whether major depression, PTSD and non-PTSD anxiety disorders with an onset prior to the Gulf War (before 1 January 1991) differed between groups. There was no significant difference for depression (deployed 5.9%, non-deployed 7.0%; P=0.97) or PTSD (deployed 3.9%, non-deployed 4.2%; P=0.60), but the deployed group had significantly more non-PTSD anxiety disorders (deployed 12.5%, non-deployed 9.2%; P=0.02). Having had any one mental disorder with an onset prior to the war did not differentiate the groups (deployed 25.9%, non-deployed 24.6%; P=0.13).
Lifetime prevalence of depression did not differ between the groups (deployed 21.3%, non-deployed 18.2%; P=0.22). Lifetime prevalence of PTSD (deployed 10.8%, non-deployed 6.7%, P=0.01), non-PTSD anxiety disorders (deployed 16.9%, non-deployed 11.0%, P=0.0003) and one or more mental disorders (deployed 43.6%, non-deployed 35.5%, P=0.01) were all significantly higher in the deployed group compared with non-deployed veterans.
Predictors of war-related mental disorders
Given that the deployed veterans group displayed a greater prevalence of Gulf War-era onset depression, PTSD and non-PTSD anxiety disorders compared with the non-deployed veterans, logistic regression was employed to examine predictors of these war-onset conditions. Simultaneous independent variables included deployment, pre-1991 onset of any one mental disorder (representing psychological vulnerability), combat (i.e. war-zone stressor) exposure, and demographic factors (age, gender, ethnicity, educational attainment in 1991, duty type, service branch and rank). For depression, pre-1991 mental disorder (P=0.009), war-zone stressor exposure (P=0.002) and gender (P=0.048) were significant. For PTSD, deployment was the only significant independent variable (P=0.03). For non-PTSD anxiety disorders, deployment (P=0.009), pre-1991 mental disorder (P=0.008), war-zone stressor exposure (P=0.0008), gender (P=0.0002) and duty type (P=0.0499) were all significant.
Self-report of symptoms and quality of life
Participants in the deployed veterans group self-reported more severe current symptoms of PTSD, depression and anxiety at the time of the assessment (Table 2), compared with the non-deployed group. Deployed veterans' mental component summary scores on the SF–36 were significantly lower than the non-deployed veterans' scores (50.0 v. 53.7), reflecting a more negative self-perception of mental health-related quality of life. Deployed veterans also reported lower levels of general life satisfaction on the QoLI than did non-deployed veterans, with 24.5% of the former group reporting below-average quality of life (v. 15.8%). When we examined groups on the 16 areas assessed in the QoLI, deployed veterans reported significantly less satisfaction with the following seven areas: health (P=0.0001), self-esteem (P=0.02), goals and values (P=0.04), play (P=0.01), learning (P=0.001), love (P=0.03) and children (P=0.049).
Table 2 Self-report measures of current mental health

| Unadjusted | Adjusted 1 | |||||
|---|---|---|---|---|---|---|
| Deployed 2 | Non-deployed 3 | P 4 | P 4 | |||
| SF–36 mental component scale score: mean (s.e.) | 48.7 (0.5) | 52.6 (0.3) | <0.0001 | <0.0001 | ||
| PTSD Checklist mean total score (s.e.) | 27.5 (0.6) | 22.8 (0.4) | <0.0001 | <0.0001 | ||
| PTSD Checklist score ≥50, % 5 | 9.8 | 2.7 | <0.0001 | <0.0001 | ||
| Beck Depression Inventory mean total score (s.e.) | 7.8 (0.4) | 4.7 (0.3) | <0.0001 | <0.0001 | ||
| Beck Depression Inventory, % | ||||||
| Minimal | 78.8 | 90.2 | <0.0001 | <0.0001 | ||
| Mild | 10.6 | 5.5 | ||||
| Moderate | 8.6 | 2.9 | ||||
| Severe | 2.0 | 1.4 | ||||
| Beck Anxiety Inventory mean total score (s.e.) | 4.8 (0.3) | 2.8 (0.2) | <0.0001 | <0.0001 | ||
| Beck Anxiety Inventory, % | ||||||
| Minimal | 80.6 | 89.9 | <0.0001 | <0.0001 | ||
| Mild | 10.5 | 7.2 | ||||
| Moderate | 5.4 | 1.0 | ||||
| Severe | 3.4 | 3.4 | ||||
| Quality of Life Inventory, % | ||||||
| Very low | 14.8 | 8.3 | 0.001 | 0.002 | ||
| Low | 9.7 | 7.5 | ||||
| Average | 54.2 | 58.8 | ||||
| High | 21.2 | 25.5 | ||||
PTSD, post-traumatic stress disorder; SF–36, Short Form Health Survey
1. Adjusted for differences in age, gender, ethnicity (White v. other), years of education (less than 12 v. 12 or more), duty type (active v. reserve/National Guard), service branch (army/marine v. navy/air force), and rank (enlisted v. officer)
2. Sample sizes ranged from 1051 to 1058
3. Sample sizes ranged from 1122 to 1126
4. Critical value is – 0.05
5. The odds ratios are 3.90 (95% CI 2.21–6.86) and 3.84 (95% CI 2.16–6.80) for the unadjusted and adjusted analyses respectively
DISCUSSION
Although there have been many studies showing greater psychological distress in Gulf War veterans, our review of the literature as well as a recent review by Stimpson et al (Reference Stimpson, Thomas and Weightman2003) found that the majority of studies assessed mental disorders with questionnaires rather than with structured interviews. In addition, many studies used selective samples. In a large, representative Australian sample of Gulf War veterans, Ikin et al (Reference Ikin, Sim and Creamer2004) used the CIDI and found that post-war anxiety, affective and substance use disorders remained elevated in deployed veterans compared with non-deployed veterans a decade after the war. Our study was unique in assessing a large, national sample of US Gulf War veterans using rigorous sampling methods and structured interviews for assessing the prevalence of mental disorders. We assumed that mental disorders with a Gulf War-era onset were related to that war, and we sought to determine whether the prevalence of these disorders a decade after the war differed among deployed v. non-deployed veterans.
We found that the prevalence of warera onset of mental disorders was significantly higher among deployed compared with non-deployed veterans; in particular, deployed veterans exhibited an increased prevalence of depression, PTSD and non-PTSD anxiety disorders, all of which had a prevalence over 1% in both groups. Ten years later, these cases of depression and non-PTSD anxiety disorders remained significantly more prevalent among deployed compared with non-deployed veterans. Post-traumatic stress disorder was over three times more prevalent among deployed veterans. As evidenced by these continued mental disorders as well as self-reported current symptoms of emotional distress, deployed veterans experienced more psychological distress and mental disorders than the non-deployed veterans both during deployment or immediately after the Gulf War, as well as 10 years later. Our results also indicate that deployment had multiple adverse effects on quality of life (health-related and non-health-related) 10 years later. However, whereas deployed veterans reported statistically significantly lower scores on the SF–36 mental component summary compared with the non-deployed group, the mean group difference of 3.9 fell short of the 4.0 group difference typically used with this measure as an index of clinical significance (Reference Wyrwich, Tierney and WolinskyWyrwich et al, 1999). Likewise, mean totals on the symptom scales did not reach the clinically impaired range, although deployed veterans were more likely to be in clinically impaired categories on these scales than non-deployed veterans.
Limitations
Our determination of the onset of mental disorders during the Gulf War era was based on the participants' retrospective report, and their recall might have been biased by their symptoms and later experiences. We did not externally validate self-report of exposure to trauma (criterion A1). As suggested by Frueh et al (Reference Frueh, Elhai and Grubaugh2005), self-report of combat trauma in veterans may be exaggerated. However, our epidemiological sample is more similar to that of Dohrenwend et al (Reference Dohrenwend, Turner and Turse2006) than the treatment-seeking sample of Frueh. Dohrenwend found that self-report of combat exposure correlated highly with record-based evidence of combat exposure. Our use of ‘state of the art’ assessment of criterion A2 helps ensure the validity of our ratings for the presence of criterion A. Although we demonstrated a lack of participation bias for demographic characteristics and selected queries regarding mood, we did not examine mental disorder diagnoses during the postal and telephone survey portions of our study. Therefore, whether increased mental disorders in the deployed group possibly reflected increased participation among deployed veterans compared with non-deployed veterans is addressed only indirectly through consideration of distress symptoms.
Causes of war-related psychological distress
The increase in psychological dysfunction in the deployed veterans could be due to multiple factors. We examined the contribution of deployment status, pre-war psychological vulnerability, combat exposure and demographic variables on disorders with Gulf War-era onsets. Only deployment predicted war-era onset of PTSD, and deployment also predicted war-era onsets of non-PTSD anxiety disorders. The war-era onsets of non-PTSD anxiety and depressive disorders were also associated with the presence of pre-war psychological vulnerability, higher levels of combat exposure and female gender.
Exposure to traumatic events is a well-recognised hazard of war, and an acknowledged precipitant of psychiatric morbidity (Goldberg et al, Reference Goldberg, Eisen and True1990a ,Reference Goldberg, True and Eisen b ; Reference Kulka, Schlenger and FairbankKulka et al, 1990) and post-war syndromes (Reference Hyams, Wignall and RosewellHyams et al, 1996). However, because exposure to trauma does not uniformly lead to psychiatric morbidity (Reference GreenGreen, 1994; Reference Kessler, Sennega and BrometKessler et al, 1995) or increased symptom complaints (Reference Eisen, Goldberg and TrueEisen et al, 1991), individual vulnerability (Reference Kulka, Schlenger and FairbankKulka et al, 1990; Reference True, Rice and EisenTrue et al, 1993; Reference Kessler, Sennega and BrometKessler et al, 1995; Reference Bromet, Sonnega and KesslerBromet et al, 1998; Reference Roy, Koslowe and KroenkeRoy et al, 1998; Reference Shalev, Freedman and PeriShalev et al, 1998; Reference Yehuda, Bierer and SchmeidlerYehuda et al, 2000) is likely to be an important contributory factor. Consistent with prior research documenting that traumatic stress exposure is associated with disorders such as depression in addition to PTSD (Reference Shalev, Freedman and PeriShalev et al, 1998), psychopathology in our cohort that began during the Gulf War era was not specific to PTSD but encompassed anxiety disorders more generally and depression. The development of these other disorders among deployed veterans might reflect the adverse psychological consequences of exposure to non-traumatic stressors associated with Gulf War participation, such as unexpected career and family disruption related to the rapid activation of an all-volunteer force with significant reservist and National Guard representation, uncertainty regarding anticipated chemical and biological warfare, or other deployment stressors (Reference Nash, Figley and NashNash, 2007). Our findings suggest that pre-existing mental disorders represent an individual vulnerability factor for the development of mental disorders during war deployment.
The classic way in which wars are thought to influence psychological well-being are the effects of exposure to combat-related traumatic stressors on the development of PTSD. Our interest in the more general effects of deployment across mental disorders led us to focus on onset during the interval of deployment rather than specific exposures to war-zone stressors. Thus, the war-era onset of PTSD cases does not overlap completely with traditional combat-related PTSD. Moreover, we did not externally validate self-report of combat experiences, which might have resulted in some overestimation of actual experiences (Reference Dohrenwend, Turner and TurseDohrenwend et al, 2006; Reference Frueh, Elhai and GrubaughFrueh et al, 2005), nor did we capture combat-related PTSD cases with an onset later than 30 July 1993, which might have resulted in underestimation of PTSD cases. Nevertheless, our data demonstrate that deployment to the Gulf War did contribute to a greater onset of major depression, PTSD and other anxiety disorders, with some persisting problems in these veterans 10 years later. Perhaps a broader conceptualisation of the relationship between war deployment and psychological functioning than the link between combat stress and PTSD would better represent health consequences for our combat veterans. This expanded view might also help to explain how the experience of combat deployment could contribute to a reduced quality of life a decade after the war.
Hobfoll's stress model of conservation of resources (Reference HobfollHobfoll, 1989) provides one perspective on the multiple impacts of stress. This model posits that individuals, when confronted with stress, try to minimise their net loss of resources. Stress involves a loss or potential loss of resources, including object resources (e.g. a home), conditions (e.g. a marriage, a state of peace), personal characteristics (e.g. an optimistic view of the world) and energies (e.g. time). Deployment is a condition involving loss of resources regardless of whether combat trauma was experienced. Coping itself depletes resources that may or may not offset the original loss of resources, and ‘loss spirals’ may develop when people have limited resources to offset an initial loss, or when coping reduces available resources needed to fend off future losses. For example, in relation to our findings, war stress (traumatic or non-traumatic) involves a loss of resources. Someone with optimistic tendencies has a resource to help buffer the loss of other resources related to war stress. In contrast, someone with pessimistic tendencies may require additional resources to offset their pessimism and insure protection against the development of additional depressive symptoms. For either person, energy spent on offsetting the loss of resources due to deployment may take away from investment in various domains ensuring enhanced quality of life.
Medication use
We examined the likelihood of remission of war-era onset disorders in deployed v. non-deployed veterans. Depression was less likely to remit among deployed than non-deployed veterans, although the levels of antidepressant use in the two groups were similar. To explore possible explanations of these differential remission rates, we compared the study groups on the severity of the depression during the Gulf War era, as well as on the presence of comorbid war-era mental disorders. The severity of depression in the two groups did not differ. Depressed deployed veterans were twice as likely as depressed non-deployed veterans to have comorbid war-era onset mental disorders. The presence of these comorbid disorders could explain the reduced likelihood of remission of depression in the deployed veterans group. Trivedi et al (Reference Trivedi, Rush and Wisniewski2006) identified predictors of remission in out-patients with major depressive disorder. Participants who were White, female, employed, or had higher levels of education or income had higher remission rates for depression, whereas longer index episodes, more concurrent psychiatric disorders, more general medical disorders and lower baseline function and quality of life were associated with lower remission rates. Thus, increased comorbidity and lower levels of education among our deployed veterans could have contributed to lower remission rates of depression. Parker et al (Reference Parker, Wilhelm and Mitchell2000) examined 12-month outcome in 182 persons with major depression. Non-recovery at 12 months was predicted most consistently by higher baseline levels of anxiety and depression; high trait anxiety and a lifetime anxiety disorder; disordered personality function; and self-reported exposure to acute and enduring stressors at baseline assessment. The more complicated clinical presentation of multiple comorbidities associated with exposure to war stressors in our deployed veterans group might have contributed to their continued depression compared with the non-deployed group.
Anxiety disorders were equally likely to remit in the two groups, but non-deployed veterans with anxiety in remission were more likely to be taking medication than deployed veterans in remission. Indeed, in the entire cohort, non-deployed veterans with anxiety disorders were more likely to take medication for these disorders than deployed veterans with anxiety disorders. The reason for this treatment disparity is unclear and we do not know whether the deployed veterans were less likely to be prescribed medication for anxiety disorders or were less likely to take anti-anxiety medication compared with the non-deployed group.
Implications of the study
The prevalence of Gulf War-era depression, anxiety – and even PTSD to some extent – abates with time. The prevalence of all these conditions decreased among both our study groups 10 years after the Gulf War compared with the rates that were found in immediate proximity to the war. Continued depression in deployed veterans appears partially resistant to remission despite comparable levels of medication use in the two groups; however, anxiety disorders might possibly remit further in deployed veterans with greater use of medications. The presence of comorbid psychiatric disorders may make it less likely that depression will remit. We do not know the extent to which the groups might or might not have differed in their use of psychological treatments for these conditions, but the findings point to the need for adequate follow-up mental healthcare for veterans with persistent mental illnesses following major military operational deployments.
Acknowledgements
We acknowledge the support of the Cooperative Studies Program of the Department of Veterans Affairs Office of Research and Development and the work of the investigators, nurse coordinators and research assistants at the 16 participating Veterans Affairs Medical Centers (VAMC); the staff at the Hines Cooperative Studies Program Coordinating Center, Hines, Illinois, and the staff at the Cooperative Studies Program, Department of Veterans Affairs Central Office, Washington, DC; the members of the executive committee and the Data and Safety Monitoring Board; and the study project manager (Tammy Nydam, MA, Hines VAMC) and coordinators (Joyce Hunter, RN, MSN, St Louis VAMC; Leila Jackson, DrPH, VA Central Office).
We acknowledge the staff at the Brockton Psychometrics Laboratory, Brockton, Massachusetts: Lisa James and Zachary Warren, research assistants; Michael Lyons, PhD, Frank Weathers, PhD, and Marie Walbridge, PhD, consultants. Finally, we thank the participating veterans and their families for their time and effort.








eLetters
No eLetters have been published for this article.