The development of psychoeducational family therapy in schizophrenia was inspired by the work on expressed emotion (EE) demonstrating that the course of illness depends to some extent on how the family members relate to and deal with the patient with first-episode psychosis (Reference Brown, Birley and WingBrown et al, 1972). A beneficial effect of psychoeducational family therapy on patients’ relapse rate is well documented, but it is unclear to what degree changes in the relatives’ knowledge, attitudes towards the patient and feelings of burden actually occur and contribute to this effect (Reference Barbato and D'AvanzoBarbato & D'Avanzo, 2000; Reference Pharoah, Mari and StrainerPharoah et al, 2000; Reference Pilling, Bebbington and KuipersPilling et al, 2002).
The OPUS trial is a randomised trial of integrated treatment v. standard treatment in first-episode psychosis (Reference Jorgensen, Nordentoft and AbelJorgensen et al, 2000). It has demonstrated several positive effects of integrated treatment compared with standard treatment: reduced levels of positive and negative symptoms, patients more satisfied with treatment, reduced number of in-patient days, and better continuity of treatment (Reference Thorup, Petersen and JeppesenThorup et al, 2005).
The present paper reports the 1-year outcome of key relatives’ subjective burden in the trial. The hypotheses were that integrated treatment in comparison with standard treatment would: (a) reduce subjective burden of illness; (b) increase satisfaction with treatment; (c) improve knowledge of schizophrenia; and (d) increase the conversion of high EE to low EE in key relatives.
METHOD
Inclusion of patients and randomisation
Patients with a first-episode of schizophrenia-spectrum disorder, aged 18–45 years, were included from all in- and out-patient mental health services in Copenhagen (Copenhagen Hospital Corporation) and Aarhus County from January 1998 until December 2000. A first episode of treated illness was operationalised as no exposure to antipsychotic medication exceeding 12 weeks of continuous medication. The details of inclusion criteria, recruitment and randomisation are described by Petersen et al (Reference Petersen, Nordentoft and Jeppesen2005, this issue).
Inclusion and assessment of key relatives
The researcher asked permission to interview the closest relative or friend of the patient. This key relative was contacted as soon as possible and asked to give written consent to be interviewed. When two close relatives were eligible, most often mother and father, both were invited to meet the assessor, and the one with closest contact to the patient was interviewed. The following hierarchy guided the choice of informant: (a) spouse; (b) parent; (c) child; (d) sibling or other relative; (e) friend or others. We did not demand a minimum level of contact between the relative and the patient. Researchers carried out the interview at the office or in the informants’ home at entry and after 1 year. The researcher was not masked to treatment.
Integrated treatment
Three newly established multidisciplinary teams working with low case-load (approximately ten patients for one team member) provided all the elements of the 2-year integrated treatment programme. The integrated treatment can be defined as a rich assertive community treatment model (Reference Stein and TestStein & Test, 1980) including protocols for medication, social skills training and psychoeducational family treatment. The psychosocial elements were adapted to meet the needs of patients during their first and second year of treated illness. Use of antipsychotics followed the guidelines from the Danish Psychiatric Society, which recommends a low-dose strategy for patients with first-episode psychosis and the use of second-generation drugs as first choice. Patients in need of social skills training were offered training at home or in a group format after assessment with the Disability Assessment Schedule (Reference Holmes, Shah and WingHolmes et al, 1982). The skills training focused on medication, coping with symptoms, conversation, problem-solving and conflict-solving skills (Reference Liberman, Mueser and WallaceLiberman et al, 1986).
Patients in contact with at least one key person were encouraged to take part in psychoeducational family treatment following McFarlane's manual for multi-family groups (Reference McFarlane, Lukens and LinkMcFarlane et al, 1995). The family treatment included: (a) three individual family meetings to create an alliance with the family and review the present crisis; (b) a survival skills workshop (Reference Anderson, Reiss and HogartyAnderson et al, 1986) with members of 4–6 families, given formal education about psychosis and its management, aetiology and prognosis through lectures and discussions; (c) 18 months’ treatment involving 1½ hours of therapy biweekly in a multi-family group with two therapists and 4–6 families, including patients. The multi-family groups focused on problem-solving and development of skills to cope with the illness.
Standard treatment
Standard treatment consisted of the usual array of mental health services. The case-load of the staff in the community mental health centre varied between 1:20 and 1:30. Medication followed the same guidelines as integrated treatment. In a small proportion of cases, key relatives met with the consultant psychiatrist to be informed of the treatment or to give background information. A few relatives in the standard treatment group participated in workshops or groups for relatives.
Measures of outcome for key relatives
Burden of illness
Burden of illness was assessed with the Social Behaviour Assessment Schedule (SBAS; Reference Platt, Weyman and HirschPlatt et al, 1980). SBAS is a semistructured interview that consists of three dimensions: (a) disturbed behaviours; (b) change in social role performance; and (c) adverse effects on others. For each item, the ‘objective change’ in the life of the relative is scored separately from the distress or ‘subjective burden’ caused by that particular behaviour. Distress is used as a general description for any unpleasant emotional response including worry, feelings of sorrow, anger or loss, etc. The scale points are predefined and the ratings of distress are based on the relative's verbal answers to the standardised questions. The distress scale is: 0=no distress, 1=moderate distress, 2=severe distress. The interviewers were trained in the interview technique and coding using videotaped interviews, which were discussed in the group.
The SBAS has 35 items of relevance in all informant–patient relationships (Reference Mors, Sorensen and TherkildsenMors et al, 1992). These include 22 items on disturbed behaviours of patients, 5 items on social role performance and 8 items on adverse effects on the informant. For each dimension, the mean distress score was computed as the sum of scores divided by the number of applicable items.
Knowledge of schizophrenia
Knowledge of schizophrenia was measured by a multiple-choice questionnaire translated and modified from McGill et al (Reference McGill, Falloon and Boyd1983). We used 12 out of 14 questions covering the following aspects of the schizophrenia condition: diagnosis, symptomatology, aetiology, medication, management and course of illness. The relative was instructed to pick all the right answers. The total number of correct answers out of 33 possible was the knowledge score.
Relatives’ satisfaction with treatment
Relatives’ satisfaction with treatment was measured with eight questions adopted for relatives from the eight-item version of the Client Satisfaction Questionnaire (Reference Attkisson and ZwickAttkisson & Zwick, 1982) and rated on a four-point Likert scale. Examples of questions were: Do you feel that the professionals have been able to listen to and understand your relative? Do you feel that the needs of your ill relative were met? Are you generally satisfied with the treatment your ill relative has received? The range of satisfaction sum scores was 8–32. Higher scores represented a higher degree of satisfaction.
Expressed emotion
The Five-Minute Speech Sample (FMSS; Reference Magana, Goldstein and KarnoMagana et al, 1986) is an alternative, time-saving method for assessing expressed emotion (EE; criticism and emotional overinvolvement) from a 5-min tape recording of a relative who has been instructed to speak about his or her thoughts and feelings about the relative with psychosis and about how they get along together. A review of studies using the FMSS (Reference Wearden, Tarrier and BarrowcloughWearden et al, 2000) concluded that results correlate highly with the Camberwell Family Interview in terms of classification of families as high or low EE but tend to underrate the occurrence of high EE.
Statistical analysis
Data handling and analysis were carried out using the Statistical Package for the Social Sciences version 10.0 for Windows. All three mean distress scores, the knowledge score and the satisfaction summed score were approximately normally distributed. The difference between intervention groups in mean distress score on each dimension of subjective burden (disturbed behaviour, social role performance and adverse effects) and in knowledge score at follow-up was analysed by analysis of covariance with treatment allocation (intervention group) and the proper baseline entered as covariables. Student's t-test was used to analyse the difference between intervention groups in relatives’ general satisfaction with treatment. The proportion of relatives who converted from high EE to low EE was compared between intervention groups with the Mantel–Haenszel method, adjusting the change from high EE to low EE with change in the opposite direction from low EE to high EE. Categorical response data were analysed with the Pearson χ2 test. For continuous, non-normally distributed data we used the Mann–Whitney test to analyse group differences. Attrition of relatives at entry and at 1-year follow-up was analysed by logistic regression analyses. All tests were two-tailed at the 5% level of significance.
RESULTS
Representativeness of the sample with a relative included
The flow of relatives through the trial is shown in Fig. 1. In total 547 patients were included and allocated to integrated treatment or standard treatment. In the integrated treatment group, 185 (67.3%) out of 275 patients had a relative included, whereas in the standard treatment group only 140 (51.4%) out of 272 patients had a relative included. The reasons for non-participation of the key relative were: (a) the patient did not accept that their relative was contacted, because they did not want the relative to know about problems, or they wanted to protect the relative from dealing with problems; (b) the patient had no contact with his/her family or another key person; (c) the relative was too sick, lived too far away or was for other reasons unable to participate; (d) the key relative refused to participate.
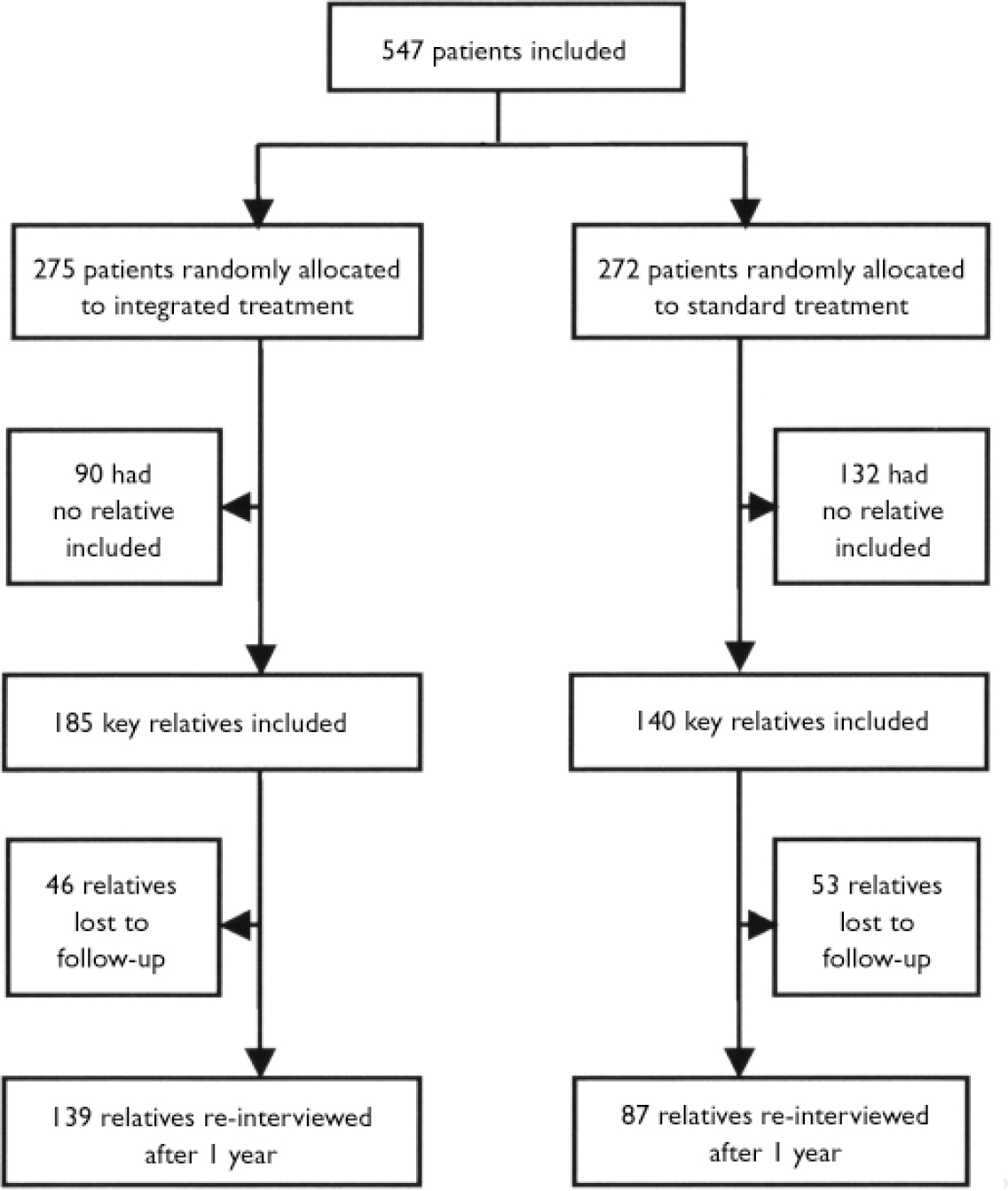
Fig. 1 Flow chart of key relatives in the OPUS trial.
In a logistic regression analysis of participation v. non-participation of a key relative at entry, all characteristics of patients (see Table 1), intervention group and centre were entered as explanatory variables. Participation of a relative was significantly positively associated with the following characteristics of the patient: allocation to integrated treatment, >11 years of schooling, living in parent's home, dual diagnosis with a harm or a dependence syndrome, and higher level of Global Assessment of Functioning (GAF) symptoms (best month in prior year), lower age, and Danish citizenship.
Table 1 Characteristics of patients with a relative included at entry
| n | Integrated treatment group | Standard treatment group | Significance | |
|---|---|---|---|---|
| Age, years: mean (s.d.) | 325 | 25.8 (6.0) | 25.9 (6.0) | 0.88 |
| Gender, males: n (%) | 325 | 101 (54.6) | 88 (62.9) | 0.14 |
| Danish citizenship, n (%) | 325 | 175 (94.6) | 136 (97.1) | 0.41 |
| Intimate relationship, n (%) | 323 | 44 (24.0) | 45 (32.1) | 0.11 |
| Marital status, n (%) | 324 | |||
| Never married | 157 (85.3) | 132 (94.3) | 0.03 | |
| Married | 14 (7.6) | 5 (3.6) | ||
| Divorced, widowed | 13 (7.1) | 3 (2.1) | ||
| School education, n (%) | 324 | |||
| 11, 12 or 13 years | 64 (34.6) | 42 (30.2) | 0.41 | |
| Vocational education, n (%) | 322 | |||
| None | 111 (60.7) | 74 (53.2) | 0.15 | |
| Little education | 27 (14.8) | 17 (12.2) | ||
| Short education, skilled | 35 (19.1) | 32 (23.0) | ||
| Longer education | 10 (5.5) | 16 (11.5) | ||
| DUP, weeks: median (IQR) | 262 | 38 (13-125) | 46 (14-172) | 0.57 |
| ICD—10 diagnosis, n (%) | 325 | |||
| Schizophrenia | 124 (67.0) | 90 (64.3) | 0.44 | |
| Schizotypia | 30 (16.2) | 17 (12.1) | ||
| Delusional disorder | 6 (3.2) | 6 (4.3) | ||
| Acute psychosis | 11 (5.9) | 15 (10.7) | ||
| Schizoaffective psychosis | 9 (4.9) | 10 (7.1) | ||
| Unspecified non-organic psychosis | 5 (2.7) | 2 (1.4) | ||
| Dependence syndrome, n (%) | 207 | |||
| Any psychoactive substance | 56 (30.3) | 39 (27.9) | 0.64 | |
| GAF: mean (s.d.) | ||||
| Symptoms, best month | 314 | 51.2 (16.8) | 53.9 (16.8) | 0.15 |
| Functioning, best month | 314 | 55.4 (16.2) | 59.0 (15.7) | 0.04 |
| Symptoms, last week | 321 | 32.3 (10.3) | 34.1 (11.7) | 0.16 |
| Functioning, last week | 321 | 40.8 (12.9) | 41.3 (14.0) | 0.76 |
Characteristics of the patients and key relatives by intervention group at entry
A total of 256 (79%) out of 325 included key relatives were females. A total of 236 (73%) out of 325 relatives were parents, the remainder were spouses (12%), siblings (9%), friends (5%), grandparents (2%) and children (0.6%). The mean age of the key relatives was 47 years. The median duration of illness, in the opinion of the key relative, was 2 years. On average, key relatives had been in face-to-face contact with their relative 18 days in the previous month. Although significantly more key relatives participated in the integrated treatment group compared with the standard treatment group, there were only three statistically significant differences between intervention groups in characteristics of patients and key relatives at entry (see Table 2). First, the mean level of distress due to the patient's behavioural disturbance was lower in the integrated treatment group compared with the standard treatment group at entry. Second, more patients in the standard treatment group compared with the integrated treatment group had never married. Third, there was a statistically significant difference in GAF functioning of the patient in the best month in the prior year; the integrated treatment group scoring worse, mean (s.d.)=55.4 (16.2) v. 59.0 (15.7), P=0.04.
Table 2 Characteristics of relatives by intervention group at entry
| n | Integrated treatment group | Standard treatment group | Significance | |
|---|---|---|---|---|
| Gender, females: n (%) | 325 | 145 (78.4) | 111 (79.3) | 0.84 |
| Age, years: mean (s.d.) | 325 | 46.6 (11.8) | 46.6 (11.8) | 0.96 |
| Relationship, n (%) | 325 | |||
| Parent | 130 (70.3) | 106 (75.7) | 0.55 | |
| Spouse | 27 (14.6) | 13 (9.3) | ||
| Child | 1 (0.5) | 1 (0.7) | ||
| Sibling | 19 (10.3) | 10 (7.1) | ||
| Grandparent | 3 (1.6) | 2 (1.4) | ||
| Friend | 5 (2.7) | 8 (5.7) | ||
| Duration of problems | 321 | |||
| DUI, months: median (IQR) | 24 (7-78) | 24 (10-108) | 0.38 | |
| Face-to-face contact | 325 | |||
| Days, last month: mean (s.d.) | 18.5 (11.2) | 18.0 (11.0) | 0.66 | |
| SBAS distress scores | 325 | |||
| Disturbed behaviour: mean (s.e.) | 1.02 (0.04) | 1.13 (0.04) | 0.05 | |
| Social role performance: mean (s.e.) | 0.59 (0.05) | 0.65 (0.05) | 0.45 | |
| Adverse effects: mean (s.e.) | 0.83 (0.05) | 0.87 (0.06) | 0.61 | |
| Knowledge score | 313 | |||
| Sum of correct answers: mean (s.d.) | 21.0 (6.2) | 21.1 (5.5) | 0.65 | |
| Expressed emotion, n (%) | 303 | |||
| Low EE | 108 (63.2) | 93 (70.5) | 0.90 | |
| Critical | 17 (9.9) | 4 (3.0) | ||
| Emotional overinvolvement | 39 (22.8) | 27 (20.5) | ||
| Critical+emotional overinvolvement | 7 (4.1) | 8 (6.1) |
Attrition during follow-up
Drop-out from re-interview at 1-year follow-up was investigated by a logistic regression analysis. All characteristics of the included patients and relatives, intervention group and centre were entered as explanatory variables. Participation of a key relative at 1-year follow-up was significantly positively associated with the following characteristics of the patient and relative: allocation to integrated treatment, patient having >11 years of schooling, Danish citizenship, and key relative being a parent.
Outcome of key relative
Burden of illness
There was a significant beneficial effect of integrated v. standard treatment on distress related to deficits in social role performance: regression coefficient β=–0.17 (95% CI –0.32 to –0.02), P=0.031, and a significant beneficial effect of integrated v. standard treatment on distress related to adverse effects of illness, β=–0.19 (95% CI –0.37 to –0.02), P=0.047. There was no difference between intervention groups in reduction of distress due to the patient's disturbed behaviour, β=–0.04 (95% CI –0.21 to 0.12); both groups improved significantly (see Figure 2).
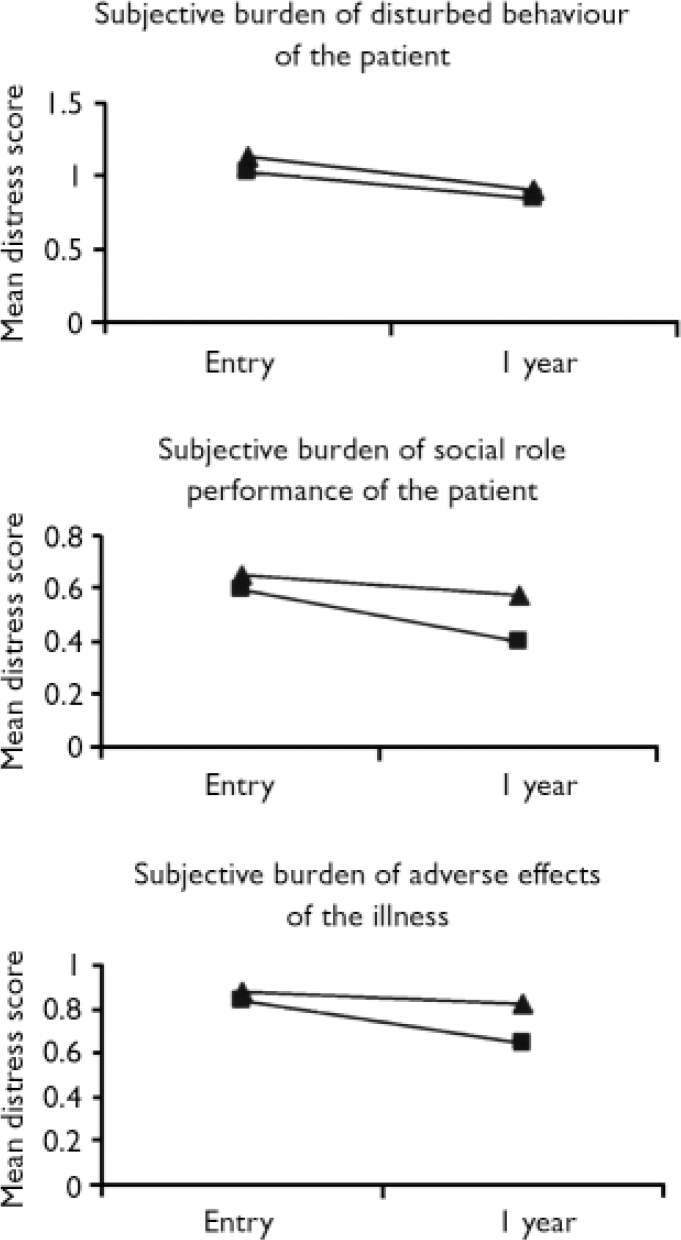
Fig. 2 Mean distress scores on the Social Behaviour Assessment Schedule by intervention group (integrated treatment, ![]() standard treatment,
standard treatment, ![]() ).
).
Expressed emotion
The proportion of key relatives changing from high EE to low EE was 63.2% in the integrated treatment group compared with 59.1% in the standard treatment group. The proportion of key relatives changing from low EE to high EE was 18.7% in the integrated treatment group compared with 12.5% in the standard treatment group. The net reduction in EE was the same in both intervention groups, see Table 3 (the net reduction in EE was compared with the Mantel–Haenszel method (OR=0.84; 95% CI 0.40–1.76; P=0.79)). There were no differences between intervention groups in the proportion of relatives being emotionally overinvolved, critical, or both at follow-up.
Table 3 Conversion from high expressed emotion to low expressed emotion and from low expressed emotion to high expressed emotion
| Entry | Follow-up | Integrated treatment (n=113) n (%) | Standard treatment (n=70) n (%) |
|---|---|---|---|
| Low EE | Low EE | 61 (81.3) | 42 (87.5) |
| High EE | 14 (18.7) | 6 (12.5) | |
| High EE | High EE | 14 (36.8) | 9 (40.9) |
| Low EE | 24 (63.2) | 13 (59.1) |
Knowledge of schizophrenia
There was no effect of integrated v. standard treatment on improvement in knowledge score, β=0.9 (95% CI –0.5 to 2.3), P=0.2. On average, the integrated treatment group had gained three and the standard treatment group had gained two more correct answers at 1-year follow-up.
General satisfaction with treatment
The mean satisfaction summed score was significantly higher in the integrated treatment group compared with the standard treatment group at follow-up. The mean difference was 3.4 (95% CI 2.1–4.7), P<0.001. The difference can be illustrated as follows: relatives in the integrated treatment group felt very satisfied, whereas relatives in the standard treatment group felt only somewhat satisfied on almost half of the questions.
Programme fidelity
Despite the effort to engage at least one family member in the treatment, only 127 (68.6%) out of 185 key relatives allocated to the integrated treatment group received one or more sessions of family therapy within the first year. A total of 94 (50.8%) began multi-family group therapy, and 79 (42.7%) had six or more sessions of multi-family group sessions. In contrast, only 27 (19.3%) out of 140 key relatives allocated to standard treatment received one or more family meetings within the first year. Only five (3.6%) had six or more family sessions including meetings in a relative's group or self-help group.
DISCUSSION
Methodology
There are several important limitations to the internal validity of the trial: (a) high and skewed attrition of key relatives at entry and at follow-up; (b) lack of masking; (c) lack of interrater reliability assessments; and (d) lack of validation of the psychometric instruments in Denmark.
Despite skewed attrition of relatives from baseline interview, there were only three statistically significant differences between intervention groups at entry. Only one of these might have clinical significance, i.e. relatives in the integrated group felt less burdened by the patient's behavioural disturbance at entry. This could be an effect of the first single-family sessions with integrated treatment relatives beginning before the point of assessment. Characteristics of patients by intervention group at entry showed several tendencies towards higher levels of symptoms and disability in the integrated treatment group compared with the standard treatment group. Thus, an eventual selection bias was more likely to work against the integrated treatment group. The study may be biased due to skewed attrition during follow-up, which is inborn when comparing treatments where one is designed to increase adherence of the patient and the relative to treatment. Lack of masking is a serious limitation of the study. Although the investigators themselves may believe they were not influenced by knowledge of therapy, others wishing to interpret trial results have a right to be sceptical. Researchers at each centre were trained in how to score SBAS and EE together, and EE ratings were consensus ratings among researchers in the centre. However, the interrater reliabilities across the two centres were not assessed. None of the psychometric scales were validated in Denmark. High EE attitudes were likely to be underestimated due to: (a) use of FMSS instead of the CFI; (b) assessment of one key relative instead of the entire household. Thus, there is a risk of misclassification.
The trial tested the hypotheses that the integrated treatment in comparison with standard treatment would: (a) reduce subjective burden of illness; (b) increase satisfaction with treatment; (c) improve knowledge of schizophrenia; and (d) increase the conversion of high EE to low EE in key relatives.
Findings supported the first and the second hypotheses, but not the third and the fourth hypotheses.
Only half the key relatives in the integrated treatment group had more than six sessions of family treatment. Specific measures of the process of psychoeducational family treatment, i.e. expressed emotion and knowledge of illness, showed no effect of intervention group. Despite these negative findings, integrated treatment compared with standard treatment proved effective in reducing the key relative's distress on two out of three domains: distress related to deficits in social performance of the ill family member and distress related to adverse effects of illness. The very high overall satisfaction with treatment among integrated treatment relatives is noticeable in view of their limited former experience with psychiatric treatment.
In summary, results generalise to mothers and other close relatives of Danish young adults coping with a first-episode of schizophrenia-spectrum disorder. Characteristics of the ill family members, like dual diagnosis, 11 or more years of schooling, living with a key relative or high levels of face-to-face contact predicted better adherence to the protocol and thereby to the psychoeducational family treatment.
Most studies of family interventions in schizophrenia are subjected to attrition of the same size and character as in our study (Reference Barrowclough, Tarrier and LewisBarrowclough et al, 1999). The attrition limits the generalisability of findings. On the other hand, it emphasises the problems of adherence to family treatment models, which are also seen in those with first-episode psychosis.
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
▪ Integrated treatment including psychoeducational multi-family groups reduced family burden of illness and improved satisfaction with treatment in first-episode psychosis.
-
▪ High expressed emotion (EE) attitudes were infrequent and unstable with no differential effect of intervention.
-
▪ The likelihood of engagement of key relatives in the treatment of first-episode psychosis is negatively associated with patients’ being older, having less schooling, worse functioning prior to the psychotic breakdown and belonging to a minority ethnic group.
LIMITATIONS
-
▪ High attrition of key relatives is seen in most studies of family interventions in schizophrenia, the present study is no exception.
-
▪ The research assessors were not masked to treatment allocation.
-
▪ The applied method for assessment of EE is likely to underestimate the presence of high EE attitudes among the key relatives.
Acknowledgements
The OPUS study was funded by grants from the Danish Ministry of Health (jr.nr. 96-0770-71), the Danish Medical Research Council (jr.nr. 9601612 and 9900734), and Copenhagen Hospital Corporation and Aarhus County.








eLetters
No eLetters have been published for this article.