We would like to respond to the invited commentary by Blanco-Rojo(Reference Blanco-Rojo1) pertaining to our published findings on the improvement of Fe status indices following an 8-week vitamin D supplementation with Fe-fortified cereals in UK Fe-deficient women(Reference Fuzi and Mushtaq2). The key findings of our study supported the study hypothesis and suggest a role for vitamin D in Fe regulation. In particular, our study demonstrated a significant effect of vitamin D3 supplementation in improving the participants’ Fe status, indicated by the increase in Hb concentrations and haematocrit levels, despite the non-significant changes in hepcidin and ferritin concentrations. The commentary author correctly pointed out that low hepcidin concentration may have hindered the detection of a possible decrease. This is plausible, as the recruited participants for the study were Fe-deficient. Ganz et al. (Reference Ganz, Olbina and Girelli3) who developed and validated the first ELISA specific for hepcidin reported that serum hepcidin concentrations were undetectable in 18–19 Fe-deficient patients. Multiple clinical factors that may be present simultaneously have been shown to influence the concentration of circulating hepcidin(Reference Girelli, Nemeth and Swinkels4). A potential decrease may be insufficient to be observed due to the lack of sensitivity of the immunoassay used in the study which actually recognises all isoforms of hepcidin (–20, –22, –24 and –25). Hepcidin exists in various isoforms(Reference Hunter, Fulton and Ganz5), and hepcidin-25 has been distinctively identified to play a role in Fe regulation(Reference Lehtihet, Bonde and Beckman6) with unclear underlying mechanisms(Reference Qiao, Sugianto and Fung7,Reference Ross, Tran and Winters8) .
Focusing on the use of breakfast cereals in the study, Blanco-Rojo(Reference Blanco-Rojo1) inferred that the presence of phytic acid, Ca and casein in the milk, with the lack of ascorbic acid, might inhibit Fe absorption, which resulted in no statistically significant increase in ferritin concentrations, and this cannot be ruled out due to the nature of the phytate content of breakfast cereals in particular. However, depending on the conditions and chemical forms of Fe itself (haem or non-haem)(Reference McDowell9), the overall percentage of Fe absorption for an individual is reported to be classically low and ranges from as low as 5 % to as high as 35 %(Reference Abbaspour, Hurrell and Kelishadi10). Previous studies that used cereal-based meals also reported a wide range of Fe absorption, of between 0·56 and 18·8 %(Reference Layrisse, García-Casal and Solano11–Reference Ahmad Fuzi, Koller and Bruggraber16). The amount of phytates in ready-made cereal products varied from 0·05 to 3·29 %(Reference Reddy, Reddy and Shridhar17). A molar ratio of <1:1 for phytates and Fe in a meal was proposed to counteract the inhibition effect of phytates on the Fe absorption; however, it was shown that phytates can still interfere with Fe absorption at a ratio of as low as 0·2:1(Reference Hurrell, Reddy and Burri14). However, no means of measuring phytates was carried out in our study, which should be taken into account in future research in order to make a fair comparison in terms of the effect of phytates in the intervention food product on Fe absorption in general. Cereals and cereal products represent the highest percentage of food (38 %) that contributes to Fe intake among UK women based on the latest National Dietary Nutrition Survey(Reference Bates, Lennox and Prentice18), where high-fibre breakfast cereals represented 7 %. This explains why it was selected as means of providing dietary Fe to the participants in our study. The use of semi-skimmed milk in the study provides approximately 250 mg of Ca with no clear underlying mechanism on how Ca affects Fe uptake and bioavailability(Reference Lynch19). A dose-dependent effect of 40–600 mg of Ca in foods on Fe absorption was observed in one of the earliest studies by Hallberg et al. (Reference Hallberg, Rossander-Hulthèn and Brune20). In a recent study, Candia et al. (Reference Candia, Ríos-Castillo and Carrera-Gil21) investigated the effects of various Ca salts on non-haem Fe bioavailability in fasted women of childbearing age and found 800 mg of supplemental calcium citrate significantly decreased non-haem Fe bioavailability. Additionally, several studies have reported conflicting findings, due to factors such as variations in the forms of Ca; differing administration routes, including within foods in a single meal; complex meals; or as supplements, in addition to varied doses(Reference Hallberg, Rossander-Hulthèn and Brune20,Reference Monsen, Hallberg and Layrisse22–Reference Grinder-Pedersen, Bukhave and Jensen25) .
Blanco-Rojo(Reference Blanco-Rojo1) suggested that the food fortification vehicles used in previous studies may have contributed to low Fe absorption in the first place, but the limited number of recent Fe fortification studies carried out in various settings have reported discrepancies in the improvement of Fe status biomarkers (Table 1). There was no significant increase in the daily Fe intake in our study; however, the intake was 1·7-fold higher at baseline, relative to typical Fe intake of adult women reported in the National Dietary Nutrition Survey, which accounted to approximately 116 % of the UK reference nutrient intake. We agree that future randomised controlled trials should consider the importance of addressing the use of food products that taken into account the bioavailability of both Fe and vitamin D. Findings from such studies have the potential to provide an alternative or adjunct route to manage Fe deficiency, as opposed to the therapeutic oral Fe therapy that can lead to poor adherence due to the adverse gastrointestinal events.
Table 1. Recent iron fortification studies using cereal and cereal-based products
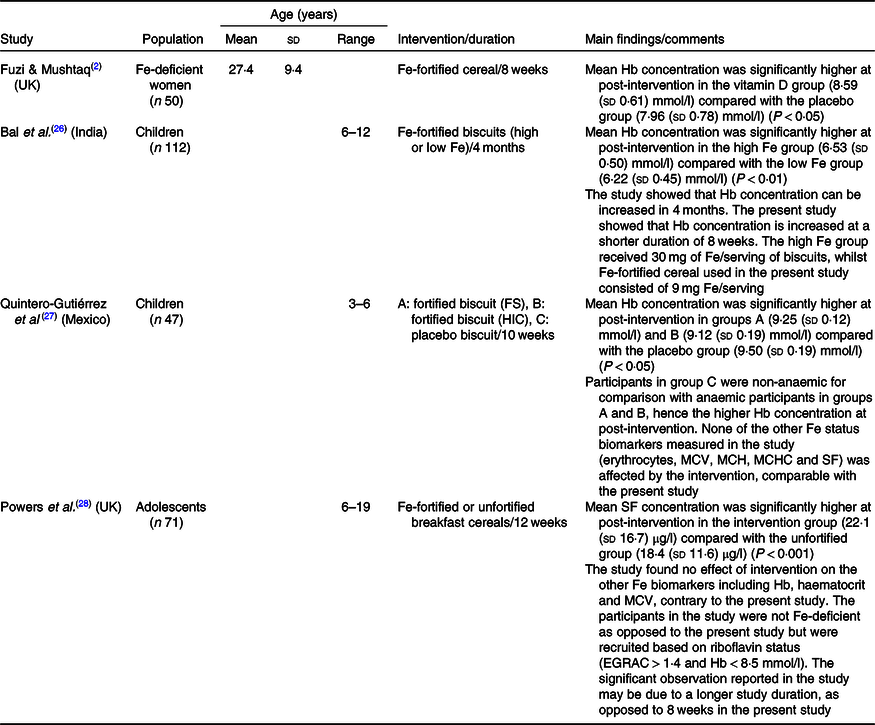
FS, ferrous sulphate; HIC, haem Fe concentrate; MCV, mean corpuscular volume; MCH, mean corpuscular Hb; MCHC, mean corpuscular Hb concentration; SF, serum ferritin; EGRAC, erythrocyte glutathione reductase activation coefficient.
Acknowledgements
The present research received no specific grant from any funding agency, commercial or not-for-profit sectors.
The authors declare that there are no conflicts of interest.



