Introduction
Diabetes is endemic with an estimated worldwide incidence of 9⋅3 % in 2019 and is projected to reach 10⋅9 % by 2045. The Middle East and North Africa (MENA) region has the highest raw prevalence of diabetes (12⋅8 %) in 2019 and is further expected to rise to 15⋅7 % by 2045(1). Diabetes is increasingly being recognised to be one of the medical conditions that require biopsychosocial approaches as poor Quality of Life (QOL) is a common fallout among those affected.
The WHO defines QOL as an ‘individual's perception of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards and concerns’ [p. 1]. QOL is an extensive concept influenced by intricate multi-personal and environmental factors(2). A number of outcome-based measurements are in use to assess QOL in individuals with diabetes(Reference Rubin and Peyrot3). The progressive and debilitating nature of diabetes tends to adversely impact QOL. Studies reported significantly low QOL in individuals with diabetes(Reference Al-Maskari, Petrini and Al-Zakwani4–Reference Papelbaum, Lemos and Duchesne7). In a comparison study of Canadians, the Health-Related Quality of Life (HR-QOL) was significantly lower in people with diabetes than others(Reference Sikdar, Wang and MacDonald5). In an outpatient sample with type 2 diabetes (n 100), QOL was poorly perceived, as gauged by Problem Area of Diabetes scale (PAID)(Reference Papelbaum, Lemos and Duchesne7).
Diabetes is a refractory condition that requires multifaceted, lifelong self-management for which individualised nutrition therapy is a cornerstone, irrespective of medical management(8–Reference Davies, D'Alessio and Fradkin11). However, dietary management is a challenge for various reasons(10), though it positively impacts glycemic control and QOL when diabetes education interventions are provided(Reference Chrvala, Sherr and Lipman12–Reference Wolf, Conaway and Crowther14). Given the adverse impact of diabetes on QOL and the challenge of coping with day-to-day dietary management, assessing the effect of the latter on QOL would further guide the individualisation of patient care with respect to nutrition management. There is a dearth of such approaches assessing the trajectory of nutrition and QOL in the Eastern Mediterranean Region. An instrument known as Nutrition Quality of Life (NQOL) has been deemed to capture all domains representing the interface between nutrition and QOL(Reference Barr and Schumacher15,Reference Barr and Schumacher16) . NQOL specifically assesses food impact, self-image, psychological factors, social/interpersonal factors, physical functioning and self-efficacy that are not featured in other instruments designed to tap into QOL. While attempts have been made to quantify QOL among people with diabetes in Arabian Gulf countries, no studies were found that have specifically focused on NQOL. In non-Arabian countries, to date, only a few studies have been conducted on NQOL, of which two were on young healthy individuals. In one, the psychometric properties of NQOL were studied in relation to body mass index (BMI) and mindfulness(Reference Cochran17), while the other compared NQOL by socio-demographic characteristics of undergraduate students(Reference Pei Lin, Wan Putri Elena and Mohd Razif18). In a nursing home, NQOL significantly improved when elderly were given a liberalised diet plan for a period of 4 weeks moving from restricted diets(Reference Tanner19). In cancer patients, NQOL was significantly higher compared to others when provided with MNT(Reference McCarthy20).
In addition to QOL, diabetes is one of the multimorbidity conditions that, without adequate self-management, often leads to various psychosocial dysfunctions(Reference Bolton, Gillett, Bolton and Gillett21). The literature suggests that psychological burden is common in people with diabetes(Reference Stoop, Pouwer and Pop22) and within such background, there is a strong suggestion that there is an intimate link between diabetes and adverse moods such as depression and anxiety, or a mixture of them. One hypothesis suggests that affective disorders are likely to be precipitated by the onset of diabetes, but there is also a dissenting view(Reference Lustman and Clouse23,Reference Renn, Feliciano and Segal24) . Despite such a link, the recognition of mood disorders in people with diabetes has remained suboptimal because many studies have employed measures sensitive to psychological-cognitive symptoms rather than somatic-biological symptoms. The latter has been suggested to present the hallmark of affective disturbance in people with diabetes(Reference Nicolau, Simo and Conchillo25). Few studies that are sensitive to somatic-biological symptoms among people with diabetes have been conducted in the Eastern Mediterranean region, i.e. Arabian Gulf countries, using measures(Reference Sulaiman, Hamdan and Tamim26,Reference Bener, Al-Hamaq and Dafeeah27) . The existing studies from the Arabian Gulf consolidate the view that diverse populations around with diabetes do display psychological burden; hence, more studies are therefore warranted. The purpose of this study is to investigate the following research questions: (1) Are there any statistically significant differences in the distribution of participants with reference to levels of NQOL, affective functioning, glycemic control, measures of obesity and history of medical nutrition therapy (HMNT)? (2) Are there any significant associations between NQOL and affective functioning and between each with other variables (glycemic control, measures of obesity and HMNT)? (3) Are there any statistically significant associations between the levels of NQOL and affective functioning controlling for glycemic control, measures of obesity and HMNT?
Subjects and methods
This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects/patients were approved by the Central Research and Ethical Review and Approve Committee of the Ministry of Health (MH/DGP/R&S/PROPOSAL_APPROVED/4/2013) and the Regional Research and Ethics Committee of Governorate of Muscat (MH/DGHS/DPT/2/8/2013). Written informed consent was obtained from all subjects/patients.
Study sample
Oman has universal healthcare coverage for its nationals and its healthcare system is divided into primary, secondary and tertiary care. This prospective, non-controlled study was conducted in Primary Health Centers (PHCs) in the urban area Governorate of Muscat, divided into six districts (Muscat, Muttrah, Bowshar, A'Seeb, Al Amerat and Quriyat)(28), which had a total of twenty PHCs during the period of the study. The study included 1 % of the total number of patients registered with diabetes (N 14 909) in the Governorate in 2011(29) which translated to 149 participants. The sample size was constrained by the availability of financial resources. In addition, the consideration of factors (based on the authors’ field experience) such as the likelihood of the respondent's motivation to participate in the interview due to time factor and the respondent's unwillingness to talk about their personal matters affected the determination of sample size for the present study.
As an initial step, a stratified sampling process based on the number of patients involved in the PHCs was applied in selecting the centres. Centres with ≤100 cases in their diabetes registry were excluded from sampling. PHCs were then randomly chosen by a number draw from each district. An exception was the district of A'Seeb from which two centres were selected due to its population density and the increased number of PHCs in the area(28). The sample size from each selected health centre was calculated to be proportional to the number of diabetes cases recorded in its diabetes registry to match the overall sample size of the study (n 149). Only adult (19–65 years old), Omani Arabic-speaking individuals diagnosed with type 2 diabetes for ≥1 year were included. The study excluded non-Arabic-speaking Omani patients, persons <19 and >65 years old (the 65 years age limit was adapted to curb the number of illiterate individuals since the spread of education started in 1970 in Oman), persons on dialysis, pregnant females and persons having HbA1c values dated older than a year from the day of the interview. As a standard practice in PHCs, HbA1c is conducted on an annual basis for most of the patients.
Nutrition quality of life
The nutrition quality of life was gauged by the Nutrition Quality of Life (NQOL) questionnaire version 1.4. NQOL was developed by Barr and Schuacher to assess the impact of nutrition on QOL. This version of the NQOL consists of fifty items divided into six domains: food impact (nine items); self-image (six items); psychological factors (ten items); social/interpersonal factors (seven items); physical functioning (nine items); self-efficacy (nine items). All response options are on a five-point Likert scale (all of the time, most of the time, some of the time, little of the time and none of the time)(Reference Barr and Schumacher15,Reference Barr and Schumacher16) .
As an integral part of this study, NQOL was translated into Arabic. The translation was done following an established protocol(Reference Sartorius and Kuyken30). In brief, the translated questionnaire was back-translated and revised by a language specialist and a nutrition specialist and modifications were implemented to clarify and simplify meanings accordingly. The questionnaire was then piloted with ten adults, graduate students and staff. They independently reviewed the items for ease of reading and clarity of meaning. A discussion was then conducted with a sub-group of five out of the ten adults for clarity and possible phrasings and wordings of some words due to linguistic variation among people from different regions in Muscat. The item ‘my food-related condition has caused problem with sexual relations’ was excluded for its socio-cultural misalignment with local religious and cultural beliefs as indicated by the pilot group.
The revised questionnaire was then tested on a convenient sample of nine patients with type 2 diabetes from two PHCs. Changes were adapted to simplify meanings for patients with low education levels, as emerged from this phase. In addition, the item ‘Liked the way my clothes fit’ was excluded as a result of criticism from patients that the item did not fall in line with what was considered to be culturally appropriate. In addition, the use of loose-fitting clothing among men and women is common in Oman. Thus, the final version of the adapted NQOL questionnaire consisted of forty-eight items. In the process, possible dialect synonyms and explanatory words were listed in case a need to clarify the meaning of phrases arose during the implementation.
Each item on NQOL was assessed on a scale of five points from 1 for ‘none of the time’ to 5 for ‘all of the time’ of the previous 2 weeks, with a minimum of 48 points and a maximum possible composite score of 240. For this study, NQOL scores were grouped into three levels: low (<75 %); moderate (75–89⋅9 %); high (≥90 %).
Affective functioning
The validated Arabic version of the Hospital Anxiety and Depression Scale (HADS) was used to screen for the presence of anxiety and depressive symptoms. The scale has fourteen screening items of which seven are for anxiety and the other seven items are for depression, assessed on a four-point Likert scale (0–3)(Reference El-Rufaie and Absood31). The current scoring of HADS was based on the threshold of ≤7 on each subscale. For those who scored ≤7 are labelled as ‘non-case’ as set by the previous researchers(Reference El-Rufaie and Absood31,Reference Zigmond and Snaith32) , while we labelled those scored >7 as ‘case-ness’. For brevity, this study collapsed three outcomes of HADS: HADS-Total (representing the sum score of the two subscales); HADS-Anxiety (denotes the sum of the items relevant to anxiety); HADS-Depression (denotes the sum of the items relevant to depression).
HbA1c, measures of obesity and history of medical nutrition therapy
The latest HbA1c values were abstracted from the medical records. As a standard practice, HbA1c investigation is only conducted once a year for most of the patients in PHC settings. Thus, only participating subjects with HbA1c dated within a year from the day of interviews were included. The WHO classification of glycemic control (HbA1c <7 %) was employed to denote adequate glycemic control(33).
Three anthropometric measurements were taken in the vital rooms on the same day of the interview: height (cm); weight (kg); waist circumference (cm). Height and weight were used to calculate the BMI index of weight-for-height (kg/m2) and the latter was used to assess central obesity. Both BMI and waist circumference are recommended indices of adiposity classification for different purposes such as assessing the status or the need for intervention. The WHO cut-off points for classifications of BMI (18⋅5–24⋅9 kg/m2 (normal), 25–29⋅9 kg/m2 (overweight) and ≥30 kg/m2 (obesity))(34) and sex-specific waist circumference (>102 cm for men and >88 cm for women) [p. 27](35) were applied.
MNT is recommended as a routine in the care for people with diabetes(36); thus, it was deemed essential to explore whether the patient-seeking consultation from primary health care in Oman had been exposed to MNT and if it had an impact on their NQOL. In this study, MNT operationalised to constitute History of Medical Nutrition Therapy (HMNT) was assessed by the number of times participants reported encounters with nutritionists/dietitians since the diagnosis of diabetes. Reported counts of HMNT were then categorised as ‘0’, 1–3 and >3 times. Socio-demographic data, including age, gender, employment status, marital status, income and educational level, were also sought.
Data collection
The present study was conducted in PHCs. In the stratified PHCs, patients showing up in the diabetes clinic for their follow-up were verbally invited to participate in the study. Patients who agreed to participate were asked to sign a consent form. Data were collected by three trained interviewers (nutritionist/dietitians). All interviewers were trained simultaneously on the tools. The interviewers were scrutinised for their consistency in dispensing the questionnaires. There was high concordance among them. Interviews were conducted either in the conference room of the PHC or in the waiting area depending on the participant's preference. Data were collected using online Google forms to minimise errors related to manual data entry. Data points on the electronic form were set as required to avoid any missing data. Seven identical electronic forms were created, one for each health centre to track the proportional number of patients specified for each centre and the progress of data collection.
Statistical analyses
Statistical analysis was conducted using Statistical Package for the Social Science (SPSS). Demographic data were analysed by frequencies and percentages. The distribution of the continuous variables was assessed before analyses using the Jarque–Bera Lagrange multiplier (J-B LM) test that indicated that all the continuous variables were not normally distributed(Reference Jarque and Bera37). Cronbach's alpha (with 95 % CI) was applied to assess the size of the internal reliability of the NQOL and HADS. The Pearson's product moment correlation coefficient was used to measure the relationships between the NQOL and HADS as all the concerned variables are continues in nature. A non-parametric statistical test (i.e. the χ 2 test of independence) on two- and three-way contingency tables was conducted to check the association between groups of variables of interests (i.e. NQOL and HADS with other variables (HADS-Total, anxiety, depression, gender, HbA1c, BMI, waist circumference, HMNT, etc.)). The χ 2 test of independence determines the statistical significance of the association between variables but not the extent of such relationships. Therefore, Cramér's V coefficient (also known as Cramér's phi) which uses χ 2 statistic was calculated to examine the strength of the relationship between variables. The value of the Cramér's V coefficient (CV) ranges from 0 to 1. A priori P < 0⋅05 was considered significant.
Results
Both scales, NQOL and HADS, had high levels of internal consistency, as determined by a Cronbach's alpha of 0⋅880 (95 % CI 0⋅85, 0⋅91) and 0⋅863 (95 % CI 0⋅83, 0⋅89), respectively.
Characteristics of the study participants
The characteristics and the distribution of the study participants are presented in Tables 1 and 2. With mostly females and low-income individuals, a large proportion of the study sample is classified as overweight (38⋅9 %) and obese (46⋅3 %). Most of the participants had central obesity (75⋅8 %) and poor glycemic control (71⋅1 %) as noted by HbA1c ≥ 7.
Table 1. Socio-economic profile of Omani patients with type 2 diabetes seeking care in primary health centres in Muscat

OMR (Omani Rial). 1 OMR ≈ USD 2⋅59 (pegged).
Table 2. Distribution of the participants with type 2 diabetes by the study variables and χ 2 test results
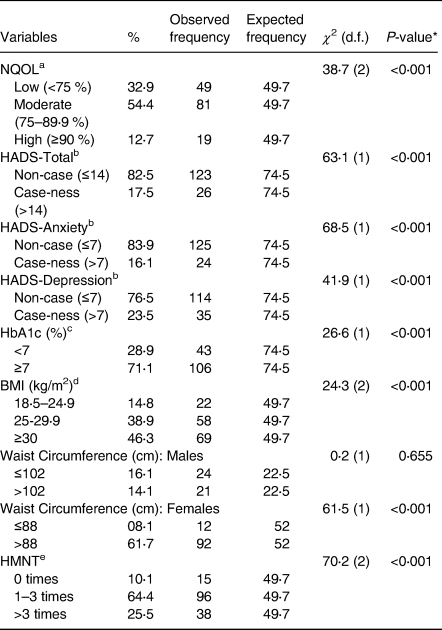
d.f., degree of freedom.
a Nutrition Quality of Life (NQOL).
b Hospital Anxiety and Depression Scale (HADS)-Total based on the sum of all subscales of HADS (i.e. HADS-Anxiety and HADS-Depression).
c HbA1c refers to glycated haemoglobin.
d Body mass index (BMI) weight-for-height (kg/m2).
e History of Medical Nutrition Therapy (HMNT) represents the number of times subjects reported to have received MNT.
* P-value < 0⋅05 indicates statistical significance at the 5 % level.
A significant difference in the distribution of participants among the three levels of NQOL, χ 2 (2) 38⋅71, P < 0⋅001, was observed in all variables but waist circumference in males. Much of the sample had reported having 1–3 encounters with a dietitian (Table 2).
NQOL and HADS associations
The relationship between NQOL and HADS was found to be negative and significant. Significant positive correlations were found between HADS score and its subscales, anxiety (r 0⋅885, P < 0⋅001) and depression (r 0⋅871, P < 0⋅001) (Table 3). Results of the two-way χ 2 test of independence are presented in Table 4. There was a significant association between levels of NQOL with levels of HADS-Total (χ 2 (2) = 38⋅2, P < 0⋅001), anxiety (χ 2 (2) = 38⋅7, P < 0⋅001) and depression (χ 2 (2) = 22⋅3, P < 0⋅001), with associations from highly to moderately strong(Reference Cohen38), Cramér's V (CV) = 0⋅51, 0⋅51 and 0⋅39, respectively.
Table 3. Correlations between nutrition quality of life and hospital anxiety and depression scale, and with other variables

NA, not applicable.
a Nutrition Quality of life (NQOL).
b Hospital Anxiety and Depression Scale (HADS).
c HbA1c refers to glycated haemoglobin.
d Body mass index (BMI) weight-for-height (kg/m2).
e History of Medical Nutrition Therapy (HMNT).
* P-value < 0⋅05 indicates the statistical significance of the associated coefficient at the 5 % level.
Table 4. The association between nutrition quality of life and affective functioning and with other variables
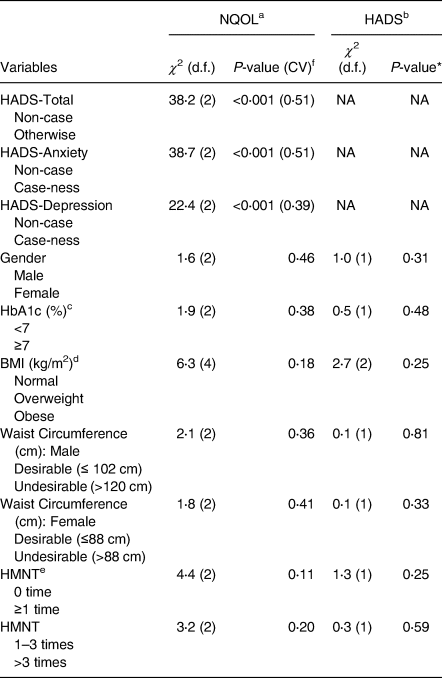
d.f., degree of freedom; NA, not applicable.
a Nutrition Quality of life (NQOL).
b Hospital Anxiety and Depression Scale (HADS).
c HbA1c refers to glycated haemoglobin.
d Body mass index (BMI) weight-for-height (kg/m2).
e History of Medical Nutrition Therapy (HMNT).
f Cramér's V coefficient (CV) estimate is in the parentheses. Reported only for statistically significant (at least at the 5 % level) cases.
* P-value < 0⋅05 indicates statistical significance at the 5 % level.
The results of the three-way χ 2 test of independence are presented in Table 5. It is evident that in participants with HbA1c ≥7 %, there are significant associations between NQOL with all measures of HADS: HADS-Total, χ 2 (2) = 19⋅42, P < 0⋅001; HADS-Anxiety, χ 2 (2) = 27⋅62, P < 0⋅001; HADS-Depression, χ 2 (2) = 8⋅85, P 0⋅01. The associations were high to moderately strong(Reference Cohen38), Cramér's V (CV) = 0⋅43, 0⋅51 and 0⋅29, respectively. Significant associations (P < 0⋅001) are observed in all χ 2 testes that meet the assumption of test, BMI ≥ 25 kg/m2, undesirable waist circumference, HMNT ≥ 1 and one to three times of HNMT.
Table 5. The association between nutrition quality of life and the hospital anxiety depression scale and other variables

d.f., degree of freedom; NA, not applicable.
a Nutrition Quality of life (NQOL).
b Hospital Anxiety and Depression Scale (HADS).
c Cramér's V coefficient (CV) estimate is in the parentheses. Reported only for statistically significant (at least at the 5 % level) cases.
d HbA1c refers to glycated haemoglobin.
e Body mass index (BMI) weight-for-height (kg/m2).
f Aggregated waist circumference groups (Desirable: ≤102 cm (male) and ≤88 cm (female); Undesirable: >102 cm (male) and >88 cm (female)).
g History of Medical Nutrition Therapy (HMNT).
* P-value < 0⋅05 indicates statistical significance at the 5 % level.
Discussion
With our sample of type 2 diabetes, NQOL and HADS showed high internal reliability (α = 0⋅88 and α = 0⋅86, respectively) with tight ranges of 95 % CI signifying the size of reliability(Reference Iacobucci and Duhachek39). Both alpha levels are higher than the satisfactory minimum reliability (α = 0⋅7) suggested by Nunnally and Bernstein(Reference Nunnally and Bernstein40). Also, the reliability of the NQOL (48-item) in our sample is higher than those reported on the 50-item NQOL surveys of American (α = 0⋅74)(Reference Cochran17) and Malay (α = 0⋅217–0⋅908; n 241) undergraduate students(Reference Pei Lin, Wan Putri Elena and Mohd Razif18). Although the NQOL scale is intended to gauge nutrition-related quality of life of individuals receiving MNT(Reference Barr and Schumacher15,Reference Barr and Schumacher16) such as those in our sample, studies on NQOL and MNT(Reference McCarthy20,Reference Wampler41,Reference Hunt, Wilson and Pope42) did not report psychometric properties of the instrument.
As in the present study, the NQOL cut-off scores are set arbitrarily due to limited research in the field. In this study, NQOL score ≥90 % was deemed high and <75 % was deemed low. In cancer patients, a score of ≥76 % is set as acceptable(Reference McCarthy20) based on a dichotomous NQOL scale (agree, disagree) while we used a 5-point Likert scale. Other studies reported means of NQOL. On a 47-item NQOL survey, a mean score of 66 % ± 10 is reported for post-gastric bypass surgery individuals (n 72)(Reference Hunt, Wilson and Pope42), while a higher mean score (145⋅8 ± 23⋅1) is reported in college students (n 182)(Reference Cochran17) using a 50-item NQOL survey; however, students form a special population. Wampler only included five items of the NQOL survey from two constructs (social/interpersonal and psychological)(Reference Wampler41), and hence, it is not comparable to our findings. Differences in the number of items and the cut-off points of NQOL are evident among studies and comparison should be considered with caution.
Various measures have been employed to tap into mood symptoms of people with diabetes. It is increasingly being recognised that questionnaires soliciting somatic-biological symptoms rather than those soliciting psychological-cognitive symptoms are more likely to capture phenotypical presentation of mood disturbance in people with diabetes(Reference Nicolau, Simo and Conchillo25). Studies have suggested that HADS is more equipped to tap into somatic-biological symptoms since it was initially described for use among people with medical conditions rather than psychiatric disorders(Reference Nicolau, Simo and Conchillo25). When correlated, both the aggregated and segregated HADS scores were correlated negatively and significantly with NQOL. To our knowledge, this is the first study that explores the variation of NQOL and mood symptoms.
A 17⋅5 % of our patients endorsed themselves to be having mood symptoms (HADS-Total) which outshines the 9⋅3 % reported in a large (n 245 404 of which 2 % had diabetes) multination study by WHO(Reference Moussavi, Chatterji and Verdes43). Also, a lower prevalence of both anxiety (9 %) and depression (20⋅9 %) was found in individuals with type 1 and type 2 diabetes in Italy(Reference Trento, Raballo and Trevisan44) compared with current 16⋅1 and 23⋅5 % endorsing case-ness on the subscales HADS-Anxiety and HADS-Depression, respectively. The incidence of anxiety in this sample is proximal to that found (15⋅6 %) in a large multi-racial (n 20 142) American study on the coexistence of anxiety and diabetes conducted based on the PHQ-8 scale(Reference Li, Barker and Ford45).
Differences in the prevalence of mood symptoms are seen in studies from the same region as well. Depression in our sample with diabetes is higher than that of a diverse large sample (8⋅1 %; n 2005) attending PHCs in Muscat Governorate as assess by PHQ-9(Reference Al-Salmani, Juma and Al-Noobi46). On the other hand, our prevalence appears to echo that reported in subjects with diabetes in Jordan where mood symptoms, based on the PHQ-8 scale, amounted to 19⋅7 % (n 649)(Reference Al-Amer, Sobeh and Zayed47). On the other hand, the prevalence of mood symptoms in our study is considered high compared to that (12⋅5 %) from the United Arab Emirates (UAE) for subjects with diabetes from PHC (n 347), based on the Kessler Psychological Distress Scale (K6)(Reference Sulaiman, Hamdan and Tamim26). In contrast, the prevalence in this study is lower than that reported in Qatar where anxiety was prevalent among 73 % and depression among 52⋅5 % in people with diabetes (n 889), assessed by the Depression, Anxiety and Stress Scale (DASS-21)(Reference Bener, Al-Hamaq and Dafeeah27).
The participants in this study have a high average HbA1c (8⋅3 % ± 2) and the most (71 %) have poor glycemic control, and such a trend is commonly reported among people with diabetes in both developed and developing nations(Reference Emeka, Mukalaf and Helal48–Reference Ali, Bullard and Imperatore50). The American Diabetes Association (ADA) noted that poor glycemic control is common in nearly 50 % of people with diabetes(10). The current sample with diabetes has increased measures of adiposity which echoes the general trend in Oman where the prevalence of overweight and obesity ranges from 46 %(Reference Moursi51) to 65⋅5 %(52). With such high proportions of adiposity, weight management interventions are warranted for patients with type 2 diabetes in PHC to ameliorate HbA1c and blood lipids to curb diabetes complications(Reference Wolf, Conaway and Crowther14).
Although most participants (89⋅9 %) received at least one encounter of MNT with a dietitian with the majority (64⋅4 %) reporting 1–3 encounters, yet the majority have high measures of adiposity and poor glycemic control. More encounters with dietitians and evaluation of MNT services appear necessary to boost MNT for diabetes management in PHCs. Based on the Evidence Analyses Library (EAL), at least 3–6 encounters of MNT during the first 6 months of diagnosis are recommended(53). For many, determining what and how much to eat are challenging while implementing diabetes management plans and there is not a ‘one-size-fits-all’ eating pattern. Thus, the ADA recommends that people with diabetes be actively and collaboratively engaged in the development of individualised eating plans(10). Also, attention is due to provide literacy-appropriate MNT approaches, since the vast majority of the participants in our study did not obtain formal education and were of low income, in order to improve diabetes control in low-income groups(Reference Rosal, Ockene and Restrepo54).
Since there are no studies that have investigated NQOL in people with diabetes, findings of this study are compared to both, findings on NQOL as available and studies on QOL in people with diabetes. A negative correlation between NQOL and affective functioning (HADS-Total) (r −0⋅59; P < 0⋅001) was expected. As diabetes management requires dietary changes that are challenging to those affected(10), depression and anxiety could precipitate as a result and/or vice versa. This relationship guides us to conclude that NQOL is a practical tool to assess the impact of diabetes on NQOL and guide the direction of MNT in PHCs. In establishing criteria-related validity, NQOL was positively correlated with both, perceived health status as assessed by the Short-Form Health Survey (SF-36) (r 0⋅57; P < 0⋅001) and mindfulness (r 0⋅46; P < 0⋅001) based on Mindful Attention Awareness Scale (MAAS) among healthy students(Reference Cochran17). Also, similar correlations are reported between various scales of QOL and depression and anxiety among people with diabetes. QOL, based on the PAID scale, correlated with depressive symptoms based on the BDI scale (r 0⋅503; P < 0⋅001) in patients (n 100) with type 2 diabetes(Reference Papelbaum, Lemos and Duchesne7). Paschalides et al. reported significant correlations between QOL and anxiety and depression, using the SF-36 for health-related QOL and WBQ scale for anxiety and depression in adult outpatients with type 2 diabetes (n 184)(Reference Paschalides, Wearden and Dunkerley55).
Lifelong dietary management is a cornerstone for diabetes management and it has a positive effect on glycemic control(Reference Al-Sinani, Min and Ghebremeskel56–Reference Esposito, Maiorino and Ceriello59) and QOL(Reference Chrvala, Sherr and Lipman12,Reference Lemon, Lacey and Lohse13) . However, no significant correlation was found between NQOL and HbA1c in the present study, which could partly be attributed to the disproportionally large number of patients had HbA1c ≥7 % and less than the recommended encounters of MNT. It is also possible that NQOL is designed to measure nutritional habits in the last 2 weeks, while the HbA1c values in this study were within a year from the day of the interview. Thus, variable findings could be revealed using recent HbA1c readings. Others also did not find significant correlations between HbA1c and QOL(Reference Papelbaum, Lemos and Duchesne7) or depression and anxiety(Reference Paschalides, Wearden and Dunkerley55) though low depression scores, using HADS, were significantly associated with good glycemic control (P < 0⋅01) in a large sample (n 1456) of Irish people with diabetes(Reference Collins, Corcoran and Perry60). Such a difference could be attributed to the multifold difference in sample sizes, demographic differences and analyses approach.
The moderate to large(Reference Cohen38) significant associations between levels NQOL and HADS (Total, anxiety and depression) are in line with the significant negative correlation between NQOL and affective functioning (HADS) in our patients, and as reported by others between QOL and anxiety and depression(Reference Papelbaum, Lemos and Duchesne7,Reference Paschalides, Wearden and Dunkerley55) . No significant associations were found between NQOL and other variables in this sample, while healthy Malay female students exhibited a general tendency for higher NQOL than males(Reference Pei Lin, Wan Putri Elena and Mohd Razif18), and provision of MNT positively influenced NQOL in cancer patients (n 12)(Reference McCarthy20) and nursing home residents (n 30)(Reference Tanner19), and QOL in adults with type 2 diabetes(Reference Lemon, Lacey and Lohse13,Reference Wolf, Conaway and Crowther14) . The present study used reported a history of encounters of MNT which could be negatively influenced by recall bias and the low level of education among the majority (>72 %) of the sample. With that, it is imperative to investigate the quality and approaches of MNT practices in diabetes clinics in PHCs in Muscat to gain a better insight on their impact on the recipients of the services. As for HADS, no significant associations were observed with other variables, while different studies reported that depression is significantly higher in females(Reference Al-Amer, Sobeh and Zayed47,Reference Yekta, Pourali and Yavarian61,Reference Yu, Y-Hua and Hong62) .
In the three-way analyses, poor glycemic control, BMI ≥ 25 kg/m2, and central obesity are contributing factors to the significant association between NQOL and affective functioning in our sample and are also linked to affective functioning in relation to diabetes elsewhere(Reference Papelbaum, Lemos and Duchesne7,Reference Katon, Von Korff and Ciechanowski63) . In addition, the contribution of the history of MNT to the significant association between NQOL and affective functioning is also in line with the positive associations reported in intervention studies between MNT and QOL(Reference Lemon, Lacey and Lohse13,Reference Wolf, Conaway and Crowther14) , significant positive interactions between QOL and affective functioning(Reference Al-Maskari, Petrini and Al-Zakwani4,Reference Hall, Rodin and Vallis64) and the significant interactions among QOL, depressive symptoms and glycemic control(Reference Papelbaum, Lemos and Duchesne7) in persons with diabetes. With such findings and as noted earlier a significant negative correlation (r −0⋅59, P < 0⋅1) is in place in our sample, MNT appears important to enhance the NQOL that in turn would reflect on reduced levels of anxiety and depression.
Conclusions and recommendations
Overall, there is a large negative correlation between NQOL and affective functioning. With categorical testing, the two variables also exhibited large association. When controlled for other variables, the association between them persisted though the effect size was marginally decreased due to sample size. Examination of the sensitivity of the outcome variable (NQOL) to potential predictor variables using logistic regression techniques should also be a useful addition to the present research. The incidence of anxiety and depression is higher than in other studies and is coupled with high rates of poor measures of obesity and HbA1c. Hence, preventative actions tackling anxiety and depression and lifestyle modification interventions should be considered in people with diabetes at PHC services in Oman. The Arabic NQOL survey (available on request) exhibited large internal reliability and further studies are recommended to validate the measure among other Arabian populations since it is a new tool and had not been widely established.
Limitations
There are some shortcomings in the study to be acknowledged. The study is based on a small sample from one region of the country. Thus, any attempt to generalise the findings should be made with caution. During translation to Arabic, two of the items on the NQOL 1.4 were deemed as being unadaptable to socio-cultural norms in Oman. Such omission would ostensibly compromise the present findings compared to those that have employed the full version of NQOL version 1.4. Finally, the study relied on existing data of HbA1c as permitted by the standard practice in PHCs. Hence, the correlation between NQOL and HAD with HbA1c might be different if HbA1c readings were standardised.
Acknowledgements
The authors thank all the staff in the PHCs for sharing their space with us and to giving us access to the medical records to obtain HbA1c readings.
This work was partially supported by the Sultan Qaboos University internal grant (IG/AGR/2010/09). Sultan Qaboos University had no role in the design, analysis or writing of this article.
Al Toobi acquired analysed the data and drafted the manuscript. Al Subhi conceived and designed the study, acquired and coded the data, drafted and critically revised the manuscript. Bose analysed the data, interpreted the results and revised the manuscript. Al-Adawi drafted and critically revised the manuscript. All authors approved of the version to be published. Al Subhi is accountable for all aspects of the work.
There are no conflicts of interest.







