People with borderline personality disorder experience considerable instability in their emotions and relationships with others, and this can lead to frequent crises and acts of self-harm. 1 Self-harm is the strongest predictor of completed suicide Reference Cooper, Kapur, Webb, Lawlor, Guthrie and Mackway-Jones2 and, as such, the consequences of people with borderline personality disorder not receiving appropriate interventions during times of crises are potentially lethal. Despite this, relatively little research has examined the management of acute crises for people with borderline personality disorder. Reference Borschmann, Henderson, Hogg, Phillips and Moran3 A joint crisis plan (JCP) is a written document containing a mental health service user's treatment preferences for the management of future crises. Reference Henderson, Swanson, Szmukler, Thornicroft and Zinkler4 The service user develops the JCP in collaboration with their treating clinician at a meeting that is facilitated by an independent mental health practitioner. Although the main aim of a JCP is to enhance the service user's empowerment regarding their own care, other benefits, such as reduced levels of mental health service use, reduced levels of perceived coercion and enhanced therapeutic alliance, may also be achieved. Reference Henderson, Swanson, Szmukler, Thornicroft and Zinkler4 Previous research has found JCPs to be an effective way of reducing coercive treatment for people with psychosis. Reference Henderson, Flood, Leese, Thornicroft, Sutherby and Szmukler5 However, there have been no published randomised controlled trials (RCTs) investigating the impact of personalised crisis plans for people with borderline personality disorder. Reference Borschmann, Henderson, Hogg, Phillips and Moran3 We conducted a pilot RCT, the aims of which were to investigate (a) the feasibility of recruiting and retaining a sample of community-dwelling adults with borderline personality disorder to a trial of JCPs and (b) the potential efficacy and cost-effectiveness of using a JCP on the self-harming behaviour of participants.
Method
Trial design and participants
We undertook a parallel group, single blind, treatment as usual (TAU)-controlled, randomised trial of participants with borderline personality disorder. We specifically wanted to recruit participants who experienced crises and engaged in self-harming behaviour. Follow-up was considered at 6-months post-randomisation. We recruited a sample of adults accessing community mental health teams (CMHTs) in south east London, UK. Inclusion criteria were:
-
(a) aged 18 years or older;
-
(b) meeting diagnostic criteria for borderline personality disorder (according to DSM-IV-TR criteria 6 and measured using the Structured Clinical Interview for DSM-IV (SCID-II) - Borderline Personality Disorder subsection); Reference First, Spitzer, Gibbon and Williams7
-
(c) had self-harmed in the previous 12 months (defined as at least one act with a non-fatal outcome in which the individual had initiated a behaviour (such as self-cutting), or ingested a toxic substance or object, with the intention of causing harm to themselves); Reference Madge, Hewitt, Hawton, De Wilde, Corcoran and Fekete8
-
(d) under the ongoing care of a CMHT;
-
(e) able to provide written informed consent.
Exclusion criteria were:
-
(a) currently an in-patient;
-
(b) primary diagnosis of a psychotic illness;
-
(c) unable to read or write in English;
-
(d) unable to provide written informed consent.
All potential participants were in the first instance identified and approached by their care coordinator, who informed them about the trial. After they had expressed an interest in participating, a member of the research team met with the participant to explain the trial further and obtain written informed consent.
Ethics and governance approvals
Data collection protocols were approved by the South London Research Ethics Committee (ref: 09/H0803/113) and the trial was registered with the International Standard Randomised Controlled Trial registry (ISRCTN12440268) prior to the commencement of data collection. Reference Moran, Borschmann, Flach, Barrett, Byford and Hogg9 All participants provided written informed consent prior to entering the trial, including allowing members of the research team to access their electronic records. Progress of the trial, adherence to protocol and participant safety were overseen by a trial steering committee (chaired by Professor Mike Crawford, Imperial College London).
Randomisation and masking
After consent and baseline assessment, randomisation was conducted at the level of the individual and was stratified by alcohol use (as measured by scores on the Alcohol Use Disorders Identification Test (AUDIT); Reference Saunders, Aasland, Babor, de la Fuente and Grant10 low <8; medium 8-15; high >15) and depression (as measured by scores on the Hospital Anxiety and Depression Scale (HADS) Reference Zigmund and Snaith11 depression subscale; low <8, medium 8-10, high >10), both of which have been shown to be predictive of future self-harm. Reference Kapur, Cooper, King-Hele, Webb, Lawlor and Rodway12,Reference Colman, Newman, Schopflocher, Bland and Dyck13 Randomisation was managed electronically by the Clinical Trials Unit at the King's College London Institute of Psychiatry, UK. The nature of the intervention meant that neither participants nor staff members could be masked to allocation; however, all follow-up data were collected by a research worker who was masked to treatment allocation and all data analyses were conducted by a statistician who was also masked to treatment allocation. The extent to which masking was achieved in the collection of outcome data was assessed at the end of the trial.
Intervention and control arms
Joint crisis plan
Participants randomised to the JCP + TAU condition were provided with a blank template of a JCP that included a list of topics to be considered for inclusion in the participant's JCP. Topics included ‘Positive things I can do in a crisis’, ‘Specific refusals regarding treatment during a crisis’, ‘Practical help in a crisis’ and ‘Useful telephone numbers’. A fictional JCP is displayed in online supplement DS1. Approximately 1 week later, a JCP planning meeting between the participant and their care coordinator was arranged (and facilitated) by R.B. Other key workers, advocates, friends or family members were also invited at the discretion of the participant. The aim of this meeting was to have a facilitated, informed discussion about the most appropriate information to be included in the participant's JCP. Meetings lasted approximately 60 min and the final information included in the JCP was of the participant's choosing and was entered in the participant's own wording. Within 24 h of the meeting, a typed version of the JCP was distributed to all individuals specified by the participant. With the participant's permission (56.1% of participants consented), a copy of the JCP was also attached to their electronic medical records in order to maximise dissemination of the plan within the local mental health trust.
Treatment as usual
Participants in both groups continued to receive standard care from their treating CMHT. This included, as a part of the care programme approach (CPA), the provision for service users to receive written copies of their care plan, including a brief ‘crisis contingency plan’, in addition to regular contact with a care coordinator or allocated member of the clinical team.
Outcome measures
The primary outcome was the proportion of participants reporting self-harm at 6 months post-randomisation. Self-harm data were obtained from an established self-report questionnaire. Reference Hawton, Rodham, Evans and Weatherall14 Items included ‘How many times in the past year [or ‘past six months’ at follow-up] have you deliberately tried to harm yourself?' Secondary clinical outcomes, all measured at baseline and follow-up, and their corresponding instruments were as follows.
-
(a) Depression and anxiety: HADS. Reference Zigmund and Snaith11 This is a 14-item self-report scale for detecting states of depression and anxiety in out-patients, with higher scores indicating higher levels of depression/anxiety.
-
(b) Working alliance: Working Alliance Inventory (WAI). Reference Horvath and Greenberg15 The WAI is a 12-item self-report instrument for measuring the perceived quality of working alliance between client and practitioner, with higher scores indicating a more positive perception of alliance.
-
(c) Satisfaction with services: Client Satisfaction Questionnaire (CSQ). Reference Larsen, Attkisson, Hargreaves and Nguyen16 The CSQ is an eight-item measure of participants' level of satisfaction with treatment received, with higher scores indicating a higher level of satisfaction with services.
-
(d) Engagement with services: Service Engagement Scale (SES). Reference Tait, Birchwood and Trower17 The SES is a 14-item self-report scale, completed by the participant's treating clinician - in our trial typically a care coordinator or key worker - to measure the participant's level of engagement with community mental health services. Higher scores reflect a greater level of difficulty engaging with services.
-
(e) Well-being: Warwick-Edinburgh Mental Well-Being Scale (WEMWBS). Reference Tennant, Hiller, Fishwick, Platt, Joseph and Weich18 The WEMWBS is a measure of subjective mental well-being over the preceding 2 weeks and focuses entirely on positive aspects of mental health. Higher scores indicate a higher level of well-being.
-
(f) Social functioning: Work and Social Adjustment Scale (WSAS). Reference Mundt, Marks, Shear and Greist19 The WSAS is a five-item self-report instrument to assess impaired functioning, with higher scores indicating a higher level of impairment.
-
(g) Perceived coercion: Treatment Experience Scale (TES). The TES was adapted from the Admission Experience Survey, Reference Gardner, Hoge, Bennett, Roth, Lidz and Monahan20 a 16-item instrument designed to assess the perceived level of coercion experienced by service users during hospital admission. Respondents endorse each item as either ‘true’, ‘false’ or ‘don't know’.
-
(h) Health-related quality of life: EuroQoL 5-dimensions (EQ-5D). Reference Kind and Spiker21 The EQ-5D assesses respondents' subjective health-related quality of life across five life domains: mobility, self-care, usual activities, pain/discomfort and anxiety/depression. A higher score indicates a better health-related quality of life.
-
(i) Resource-use: Adult Service Use Schedule (AD-SUS) adapted for use in this trial based on previous research involving people with personality disorders. Reference Byford, Knapp, Greenshields, Ukoumunne, Jones and Thompson22 The AD-SUS, completed by participants in interview at baseline and 6-month follow-up, collected data on use of all hospital and community health and social services. To enhance accuracy, in-patient psychiatric admission data were additionally collected from electronic clinical records of the local National Health Service (NHS) trust (South London and Maudsley). This data replaced self-reported contact data for this NHS trust, although self-reported contacts with other trusts were retained. The economic evaluation took a health and social care perspective, in line with National Institute for Health and Clinical Excellence guidelines. 23 Unit costs for the financial year 2009-2010 were applied, and these are detailed in online supplement DS2.
Sample size and power calculation
Sample size calculations are not required for most pilot studies, because the aim is to gather information about recruitment processes, consent and attrition rates and trial procedures. Nevertheless, we wanted to know whether it was feasible to recruit and retain a pre-determined number of people with borderline personality disorder into a trial of JCPs and, for this reason, we undertook a power calculation in order to give us a target sample size to aim for. The trial was powered to detect a threefold difference in the proportions of participants who had self-harmed during the follow-up period (36% in the TAU group v. 12% in the JCP + TAU group). The predicted TAU proportion of self-harm (36%) was the same proportion of self-harm as that observed in a previous RCT of cognitive therapy to reduce repetition of self-harm. Reference Tyrer, Thompson, Schmidt, Jones, Knapp and Davidson24 On the basis of these figures, an overall sample of 114 (randomised 1:1 to JCP + TAU:TAU) would provide 80% power to detect an observed difference between JCP + TAU and TAU alone, based on a two-sided test at the 5% significance level. The target sample size was increased to 120 in order to allow for attrition and loss of data on self-harm. This sample would also be large enough to provide 80% power to detect a constant hazard ratio between the groups of 0.29 with proportions of episodes in the two groups as stated above, based on the log-rank statistic assuming no accrual rate, a fixed time of follow-up and an estimated 10% rate of drop out.
Statistical analyses
All analyses were based on the intention-to-treat sample using a statistical analysis plan finalised by the trial statistician (J.M.H.) and approved by the principal investigator (P.M.) in advance of conducting any analyses. All analyses were performed with Stata version 11.0 for Windows.
Analysis of outcome variables
We summarised continuous variables as mean (s.d.) and categorical variables as n (%). We assessed the primary outcome with a logistic regression model with treatment and stratification factors; alcohol misuse (AUDIT) and depression (HADS) as covariates. Model assumptions were checked by the use of diagnostic plots. Models were undertaken with the assumption that data were missing at random. Categorical data were compared using Fisher's Exact test. We analysed secondary outcomes in a generalised linear model (GLM) framework; covariates in the model were treatment group, baseline value of outcome, alcohol misuse and depression. For the frequency of self-harm at 6-month follow-up, a negative binomial distribution was specified with a log link. Logistic regression was utilised for binary outcomes and clinical scales were analysed using the assumption of a normal distribution. Results of the treatment effects were summarised as odds ratios (ORs, logistic and ordinal logistic regression), incidence rate ratios (RRs, negative binomial distribution GLM) and effect sizes (Gaussian models) at 6-month follow-up with two-sided 95% confidence intervals.
Analysis of cost data
Differences in the use of services between randomised groups were compared descriptively and no statistical comparisons were made. Total cost per participant over the 6-month follow-up was calculated and compared statistically. Although costs were not normally distributed, analysis compared mean costs between the two randomised groups using standard parametric tests, as recommended for the analysis of cost data, Reference Barber and Thompson25 with the robustness of the parametric tests confirmed using bias-corrected, non-parametric bootstrapping. Reference Efron and Tibshirani26 Baseline cost and stratification variables (alcohol misuse and depression) were included as covariates.
Cost-effectiveness analysis
For this feasibility study, cost-effectiveness was primarily explored descriptively, taking a cost-consequences approach, which involves the presentation of a range of outcome measures alongside the costs. In cost-consequences analysis, no attempt is made to combine the costs and effectiveness of alternative interventions and decision makers are left to form their own opinion regarding the relative importance of the alternative outcomes presented. A formal cost-effectiveness analysis was carried out, as detailed in our original protocol; Reference Moran, Borschmann, Flach, Barrett, Byford and Hogg9 however, given the small sample sizes involved, this was considered hypothesis-generating only and is reported in online supplement DS2 for information.
Results
Feasibility of recruitment
Two full-time research workers recruited 88 participants over 17 months. In total, 133 individuals were referred; 30 declined and 3 were unable to read or write in English (both being necessary for participation in the formulation of a written crisis plan). Of the remaining 100 consenting individuals, 12 were ineligible (7 did not meet diagnostic criteria for borderline personality disorder and 5 had not self-harmed in the previous 12 months); the final sample, therefore, consisted of 88 participants (Fig. 1). A total of 46 participants were randomised to the JCP + TAU arm and 42 were randomised to the TAU arm. We obtained complete follow-up data on 73 (83.0%) participants; 37 (80.4%) from the JCP + TAU arm and 36 (85.7%) from the TAU arm.
Feasibility of the baseline assessments
All 88 participants completed the full battery of assessments at baseline, with the exception of the WEMWBS, which was added to the battery, on the advice of the project advisory group, after 48 participants had entered the study. Consequently, only 40 participants (45.4%) completed this measure at baseline. All assessment sessions lasted between 45 and 90 min.
Baseline characteristics
Table 1 shows the participant demographics recorded at baseline. The majority of participants were White British, female, aged in their 30s, single and unemployed. Most had left school prior to the age of 16. Demographic data were evenly matched across the TAU and JCP + TAU arms, reflecting the effectiveness of the stratified randomisation process.
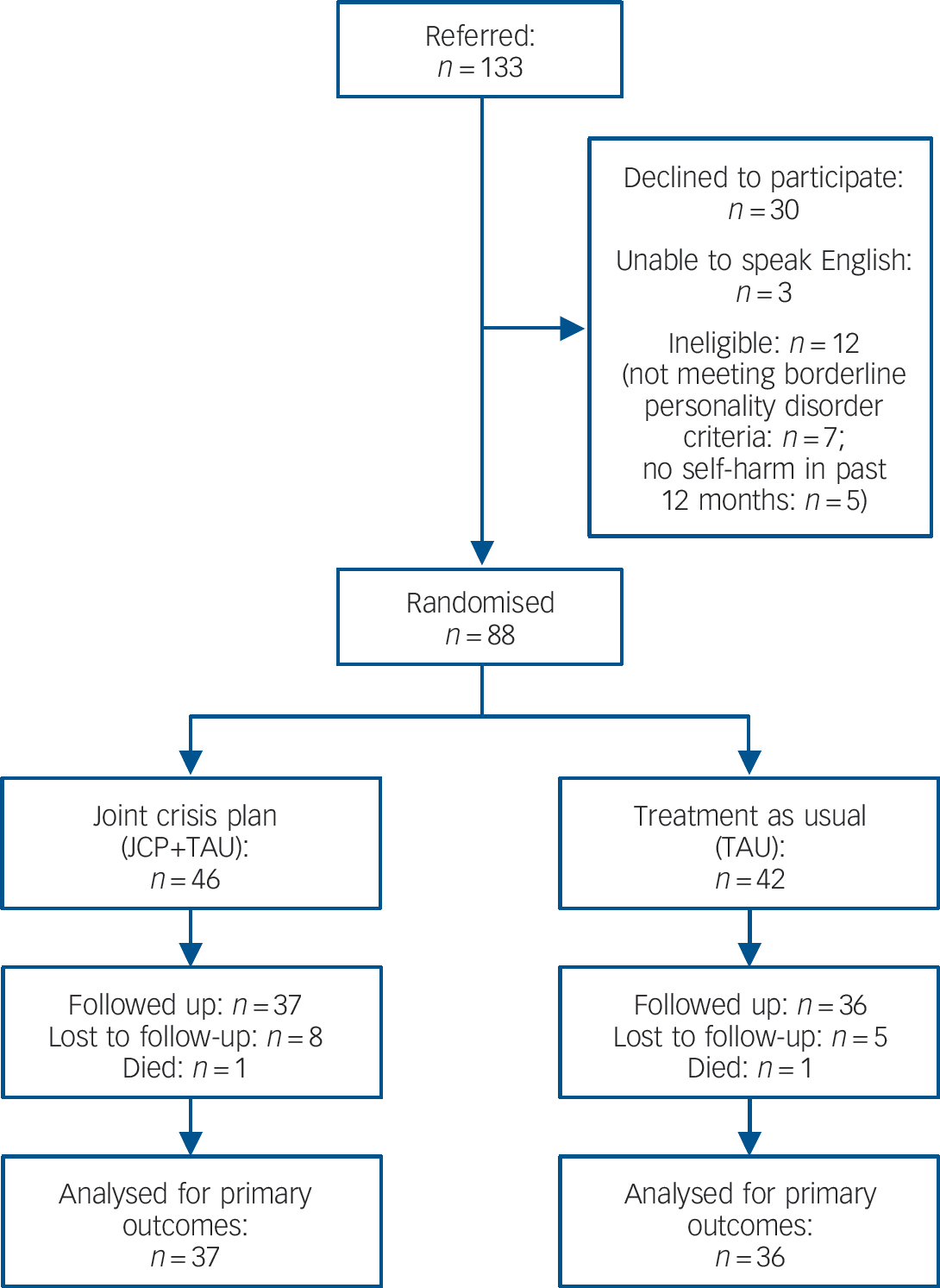
Fig. 1 Trial CONSORT diagram.
Attrition
Thirteen participants (14.7%) dropped out of the trial prior to follow-up; 8/46 (17.4%) from the JCP + TAU group and 5/42 (11.9%) from the TAU group. This figure was higher than the 10% we had estimated and contributed to the trial being underpowered. Additionally, there were two serious adverse events as two participants (one from each trial arm) died during the follow-up period; neither of these deaths was related to the intervention.
Feasibility of the follow-up assessments
In total 73 participants completed the battery of assessments at follow-up and, because of the shorter battery length, assessment sessions lasted between 30 and 60 min. All outcome measures were completed by between 63 and 73 participants (71.6-82.9%) at follow-up.
Self-harm
Table 2 shows the mean number of self-harm episodes reported by participants in each arm of the trial, along with the dichotomised self-harm data at baseline and 6-month follow-up. In both arms, at 6-month follow-up, the proportion of participants reporting self-harm had fallen. However, there was no significant difference in the proportion reporting self-harm between the JCP + TAU and TAU arms (OR = 1.9, 95% CI 0.53-6.5, P = 0.33). There were also no significant differences in the number of self-harm acts reported between the two groups (RR = 0.74, 95% CI 0.34-1.63, P = 0.46).
Table 1 Baseline demographics and stratification of study participants
| Variable | Treatment as usual (n = 42) |
Joint crisis plans + treatment as usual (n = 46) |
Total (n = 88) |
|---|---|---|---|
| Alcohol, Alcohol Use
Disorders Identification Test score: n (%) |
|||
| <8 | 20 (47.6) | 19 (41.3) | 39 (44.3) |
| 8-15 | 5 (11.9) | 9 (19.6) | 14 (15.9) |
| >15 | 17 (40.5) | 18 (39.1) | 35 (39.8) |
| Depression, Hospital
Anxiety and Depression Scale (depression subscale): n (%) |
|||
| <8 | 6 (14.3) | 8 (17.4) | 14 (15.9) |
| 8-10 | 10 (23.8) | 6 (13.0) | 16 (18.2) |
| >10 | 26 (61.9) | 32 (69.6) | 58 (65.9) |
| Age at randomisation,
years: mean s.d) |
36.1 (12.37) | 35.6 (11.1) | 35.8 (11.6) |
| Male, n (%) | 7 (16.7) | 10 (21.7) | 17 (19.3) |
| Relationship status, n (%) | |||
| In a relationship | 5 (11.9) | 8 (17.4) | 13 (14.8) |
| Not in a relationship | 37 (88.1) | 38 (82.6) | 75 (85.2) |
| Living status, n (%) | |||
| Alone | 20 (47.6) | 22 (47.8) | 42 (47.7) |
| With other(s) | 19 (45.2) | 20 (43.5) | 39 (44.3) |
| Supervised/assisted living | 3 (7.1) | 4 (8.7) | 7 (8.0) |
| Ethnicity, n (%) | |||
| Asian | 1 (2.4) | 0 (0.0) | 1 (1.1) |
| Black | 3 (7.1) | 6 (13.0) | 9 (10.2) |
| White | 31 (73.8) | 34 (73.9) | 65 (73.9) |
| Mixed | 4 (9.5) | 3 (6.5) | 7 (8.0) |
| Other | 3 (7.1) | 3 (6.5) | 6 (6.8) |
| Employment status, n (%) | |||
| In paid work | 4 (9.5) | 6 (13.0) | 10 (11.4) |
| Not working | 16 (38.0) | 20 (43.5) | 36 (40.9) |
| Permanently sick or disabled | 22 (52.4) | 20 (43.5) | 42 (47.7) |
| Age left school, years | |||
| Mean (s.d.) | 15.9 (1.3) | 15.8 (1.4) | 15.9 (1.3) |
| Range (minimum to maximum) | 12-18 | 10-19 | 10-9 |
| Further education, yes: n (%) | 30 (71.4) | 31 (67.4) | 61 (69.3) |
| Site, n (%) | |||
| Lambeth | 7 (16.7) | 4 (8.7) | 11 (12.5) |
| Southwark | 17 (40.5) | 18 (39.1) | 35 (39.8) |
| Lewisham | 3 (7.1) | 7 (15.2) | 10 (11.4) |
| Croydon | 14 (33.3) | 10 (21.7) | 24 (27.3) |
| Greenwich | 1 (2.4) | 7 (15.2) | 8 (9.1) |
Use of JCPs
Of the 46 participants allocated to receiving JCP, 41 (89.1%) attended their JCP planning meeting. Of these, 34 (82.9% of JCP + TAU participants) were available for follow-up (along with 3 participants who did not attend their JCP meeting). In total, 25 (73.5%) of these individuals reported using their JCP during a crisis and 15 (44.1%) reported using it between crises. Almost half (n = 16, 47.1%) reported that using their JCP had contributed to having a greater feeling of control over their problems and 47.1% reported that it had contributed to an improved relationship with their mental health team. Twenty-nine (85.2%) stated that they would recommend using a JCP to other service users.
Resource use and costs
The mean number of contacts participants had with all health, social care and criminal justice sector services over the 6-month follow-up period is detailed in Table 3. Mean costs per participant over the 6-month follow-up period are detailed in Table 4. The average cost of the JCP intervention was estimated to be £146 per participant. There were no significant differences in total health and social care costs (mean cost £5631 TAU v. £5308 JCP + TAU, P = 0.20). Sensitivity analyses exploring the impact of missing data and the cost of JCPs (available from the author on request) did not alter these findings.
Table 2 Comparisons of the differences in self-harm at 6 months from the final adjusted modelsFootnote a
| Treatment as usual | Joint crisis plans + treatment as usual | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Self-harmed n(%) |
Self-harm frequency, episodes | Self-harmed n(%) |
Self-harm frequency, episodes | Odds ratio (OR) of
self-harming in comparison with TAUFootnote b |
Rate ratio (RR) of
frequency of self-harm in comparison with TAUFootnote b |
|||||||
| n | Mean (s.d.) | Median (IQR) | n | Mean (s.d.) | Median (IQR) | OR (95% CI) | P | RR (95% CI) | P | |||
| Baseline (past 12 months) | 42 | 42 (100) | 56.2 (102.2) | 5.5 (47) | 46 | 46 (100) | 51.2 (126.4) | 6 (37) | ||||
| Follow-up (6 months) | 36 | 20 (55.6) | 20.3 (67.0) | 1 (3.5) | 36 | 25 (69.4) | 20.6 (89.7) | 2 (7.0) | 1.86 (0.53–6.51) | 0.33 | 0.74 (0.34–1.63) | 0.46 |
a. Results are from the fully adjusted models at 6 months post-randomisation.
b. Whole sample at follow-up n = 73.
Secondary outcomes
Table 5 shows the secondary outcomes reported at baseline and follow-up by participants in the two trial arms. Randomisation was stratified by AUDIT (alcohol) and HADS (depression) scores; at baseline, participants recorded a mean depression score of 11.77 (s.d. = 4.64) from a possible score of 21, reflecting the presence of moderate depressive symptoms across the sample. Participants recorded a mean alcohol score of 13.2 (s.d. = 12.0) from a possible score of 40, placing the average participant into the ‘moderately problematic’ category of alcohol consumption. Reference Saunders, Aasland, Babor, de la Fuente and Grant10 There were no significant differences between the groups on any of the secondary outcome measures at follow-up.
Discussion
Main findings
Our study revealed that it is feasible to recruit and retain people with borderline personality disorder to a clinical trial of JCPs. We recruited approximately three-quarters of our target sample size and retained more than 80% of participants through the trial. Moreover, the intervention appeared to have high face validity with the trial participants. Although other borderline personality disorder intervention studies have included a crisis management component as one of the ingredients of treatment, Reference Bateman and Fonagy27,Reference Linehan, Armstrong, Suarez, Allmon and Heard28 to our knowledge, this is the first RCT of a crisis intervention specifically tailored to people with borderline personality disorder. The JCPs were used both during and between crises and were viewed favourably by participants. Approximately half of participants reported a greater sense of control over their problems and an improved relationship with their mental health team when using a JCP and the large majority of participants stated that they would recommend using a JCP to other service users. At follow-up, the proportion of participants reporting self-harm fell in both groups. However, there was no significant difference in the proportions reporting self-harm between groups, and no significant differences between the groups on any of the secondary outcome measures. In addition, we did not detect a significant health and social care cost difference between the two groups over the 6-month follow-up, although there was some suggestion of greater service use in the TAU group.
Possible explanations for the findings
The lack of statistically significant differences between the groups on primary or secondary outcomes in the face of high user acceptability is counter-intuitive. However, we may have failed to detect significant differences between the two groups for a number of reasons. First, crisis planning for people with borderline personality disorder may be more successful when the crisis plan is fully integrated with other components of treatment, Reference Bateman and Fonagy29 as opposed to the one-off intervention offered to participants in the experimental arm of this trial. Second, we underrecruited to the study and it was therefore underpowered to detect a significant difference on the primary outcome. Recruitment was more difficult and attrition higher than we had originally anticipated when designing the trial. These findings emphasise the need to allow for a longer recruitment phase and larger inflation factors in the calculation of sample size for trials involving people with borderline personality disorder. Less than a third of publicly funded trials manage to recruit according to their original plan Reference Campbell, Snowdon, Francis, Elbourne, McDonald and Knight30 and so the recruitment difficulties we experienced may also have reflected a current wider problem of underrecruitment of NHS patients into research studies. Third, some participants in the TAU group may have received a generic, but equally efficacious, crisis contingency plan as part of their concurrent TAU under the CPA. However, a 2007 audit of South London and Maudsley Trust service users who had attended the emergency department (followed up 9 months later) revealed that 42% of those under the standard CPA did not have a crisis contingency plan on their electronic records (unpublished data). Of those that did, only 37% of plans contained any information that was specific to the service user, with the remaining plans consisting solely of generic information. It seems unlikely, therefore, that such generic crisis contingency plans (which are written by the clinician, without input from the service user), would have contributed to the absence of a significant difference between intervention groups in this study.
Table 3 Mean use of health and social care services over 6-month follow-up
| Mean (s.d.) | ||
|---|---|---|
| Treatment as usual (n = 36) |
Joint crisis plans + treatment as usual (n = 37) |
|
| In-patient mental health nights | 4.3 (17.2) | 6.1 (12.2) |
| In-patient physical health nights | 0.2 (0.9) | 0.3 (1.0) |
| Out-patient appointments | 7.5 (20.4) | 4.4 (7.7) |
| Accident and emergency attendances | 1.3 (3.0) | 2.1 (5.9) |
| General practitioner contacts | 9.0 (10.1) | 6.2 (7.2) |
| Community mental health contacts | 32.2 (51.8) | 22.5 (18.9) |
| Community healthcare contacts | 3.3 (6.2) | 1.8 (6.0) |
| Community advice contacts | 5.7 (16.4) | 3.6 (6.5) |
Table 4 Total health and social care cost per participant over 6-month follow-up
| Mean (s.d.), £ | ||||
|---|---|---|---|---|
| Treatment as
usual (n = 36) |
Joint crisis plans +
treatment as usual (n = 37) |
Mean difference (95% CI, bootstrapped)Footnote a |
P | |
| Joint crisis plan | 0 (0) | 146 (0) | ||
| Hospital | 2690 (8083) | 2761 (3919) | ||
| Community health and social care | 2255 (3158) | 2115 (2819) | ||
| Medication | 447 (887) | 260 (497) | ||
| Criminal justice sector services | 238 (664) | 26 (90) | ||
| Total service costs | 5631 (10 293) | 5308 (5486) | –324 (–6369-2034) | 0.20 |
a. Adjusted for baseline cost, alcohol misuse (Alcohol Use Disorders Identification Test) and depression (Hospital Anxiety and Depression Scale).
Table 5 Secondary clinical outcomes reported at baseline and follow-up by participants in the treatment as usual and treatment as usual + joint crisis plans armsFootnote a
| Treatment as usual | Joint crisis plans + treatment as usual | |||
|---|---|---|---|---|
| Clinical scale (range) | n | Mean (s.d.) | n | Mean (s.d.) |
| Highest score is best outcome | ||||
| Working Alliance Inventory Client (WAI-C) (12-84) | ||||
| Baseline | 33 | 63.36 (17.92) | 38 | 58.47 (18.50) |
| Month 6 | 30 | 60.47 (15.92) | 33 | 58.85 (16.75) |
| Working Alliance Inventory Therapist (WAI-T) (12-84) | ||||
| Baseline | 37 | 61.27 (11.10) | 40 | 63.68 (8.72) |
| Month 6 | 25 | 62.96 (10.74) | 29 | 64.66 (10.87) |
| Client Satisfaction Questionnaire (CSQ) (4-32) | ||||
| Baseline | 37 | 18.62 (1.53) | 41 | 19.85 (1.46) |
| Month 6 | 36 | 19.64 (1.33) | 37 | 19.97 (2.0) |
| Warwick-Edinburgh Mental Well-Being Scale (WEMWBS) (14-70) | ||||
| Baseline | 23 | 31.74 (10.14) | 26 | 29.65 (11.09) |
| Month 6 | 35 | 35.26 (10.26) | 36 | 34.33 (11.40) |
| Lowest score is best outcome | ||||
| Work and Social Adjustment Scale (WSAS) (0-40) | ||||
| Baseline | 42 | 26.95 (7.36) | 46 | 27.02 (6.46) |
| Month 6 | 36 | 26.06 (7.98) | 36 | 25.81 (8.94) |
| Treatment Experience Scale (TES) (0-45) | ||||
| Baseline | 42 | 16.52 (2.75) | 46 | 17.04 (2.97) |
| Month 6 | 36 | 16.0 (3.07) | 37 | 17.68 (3.09) |
| Hospital Anxiety and Depression Scale - Depression (HADS-D) (0-21) | ||||
| Baseline | 42 | 11.76 (4.30) | 46 | 11.78 (4.98) |
| Month 6 | 34 | 10.47 (3.54) | 35 | 10.20 (4.96) |
| Hospital Anxiety and Depression Scale - Anxiety (HADS-A) (0-21) | ||||
| Baseline | 42 | 14.48 (5.55) | 46 | 14.46 (4.07) |
| Month 6 | 36 | 12.94 (4.55) | 37 | 14.57 (3.83) |
| Service Engagement Scale (SES) (0-42) | ||||
| Baseline | 34 | 10.41 (7.14) | 38 | 9.82 (6.04) |
| Month 6 | 25 | 10.88 (5.62) | 30 | 8.63 (6.11) |
a. Treatment differences were considered in a fully adjusted model. No significant differences (P<0.05) were found between the treatment as usual and joint crisis plans + treatment as usual.
Strengths and limitations
In addition to the problem of underrecruitment, the study had other limitations. First, we relied exclusively on self-report for the collection of data on self-harm. Similar self-report methods have been used in previous RCTs aiming to reduce self-harming behaviour. Reference Bateman and Fonagy31 However, there is an inherent risk associated with using this methodology for obtaining self-harm data, as it is dependant entirely on respondents' openness and comprehension of questionnaire items. Reference Borschmann, Hogg, Phillips and Moran32 It may also be susceptible to reporting bias (unintentional or otherwise) and the occurrence of both false negatives and false positives is possible. Additionally, participant recall at 6 months may not have been accurate Reference Evans and Crawford33 and this may have had an impact on our findings. Second, with the exception of the most recent act of self-harm, we did not measure the medical severity of participants' self-harm and neither did we enquire about their behavioural intention. Given that such intentions can vary considerably between individuals and even within the same individual at different times, these may have been important data to collect.
Third, ‘treatment as usual’ for people with borderline personality disorder varies greatly between CMHTs, between clinicians and between individual service users. Some participants in our trial reported not seeing their CMHT care coordinator at all during the 6-month follow-up period (despite still being registered as an active service user), whereas others reported being in contact with their care coordinator several times each week during the same period. The net result of this was that participants allocated to the TAU arm received considerable variation in treatment, although the impact of this on our findings is difficult to assess. Finally, our follow-up period was limited to 6 months and it is possible that a longer period of follow-up may have resulted in significant clinical change.
Our trial also had several strengths. The trial was conducted in a real NHS setting, with recruitment taking place across five separate and demographically disparate boroughs during a period of considerable austerity and restructuring of services. Despite this, we recruited to approximately 75% of our target sample size and retained more than 80% at 6-month follow-up. Second, our refusal rate of 25% was comparable with those reported in other RCTs involving patients with borderline personality disorder Reference Bateman and Fonagy31,Reference Giesen-Bloo, Van Dyck, Spinhoven, Van Tilburg, Dirkson and Van Asselt34 and our response rate of 75% was twice as high as that reported in a previous large-scale RCT of JCPs. Reference Henderson, Flood, Leese, Thornicroft, Sutherby and Szmukler5 Third, the stratified randomisation process was effective, as evidenced by the similarity of the intervention and control groups in both size and demographic characteristics. Fourth, although the trial could not have utilised a double-blind methodology, all data analyses were conducted masked to treatment allocation and follow-up data were collected by a researcher masked to treatment allocation and this masking was maintained in 62 of 73 cases (85%). Finally, a total of 41 out of 46 participants in the JCP + TAU group (89%) received the active intervention, reflecting high fidelity to the intervention.
Clinical implications
Previous research using JCPs and other psychiatric advance directives has found that such plans promote self-determination and empowerment among service users Reference Henderson, Flood, Leese, Thornicroft and Sutherby35 and that they have the potential to facilitate stronger relationships between service users and providers. Reference Kim, Van Dorn, Scheyett, Elbogen, Swanson and Swartz36 Fostering collaborative relationships is essential in the treatment of people with borderline personality disorder 1 and JCPs may provide one approach to ensuring that the values and treatment preferences of such individuals remain central when they experience crises. Although we found that JCPs have high face validity for people with borderline personality disorder, we did not find evidence of clinical efficacy and so our trial does not provide justification to recommend the use of JCPs in clinical practice. However, as our trial was underpowered, it remains possible that the JCP is an effective intervention for people with borderline personality disorder. Future investigation will need to include robust process evaluation to understand why the experience of receiving this intervention was so positive.
Funding
This trial was supported by a Medical Research Council (MRC) trial platform grant (ID: 85397) in the UK. P.M., G.T. and D.R. are part-funded by the NIHR Specialist Biomedical Research Centre for Mental Health at the South London and Maudsley NHS Foundation Trust and Kings College London.
Acknowledgements
We are grateful to all trial participants and to the external members of the trial steering committee: Professor Mike Crawford (Chair) and Dr Sue Patterson from Imperial College London and Victoria Green from the University of Leeds. We also thank the King's Clinical Trials Unit for provision of the InferMed MACRO data entry system and web-based randomisation system for the trial.









eLetters
No eLetters have been published for this article.