1. Introduction
Schizophrenia is frequently a chronic and progressively disabling illness with negative impact on all aspect of a person’s life [Reference Owen, Sawa and Mortensen1]. It is a neurodevelopmental, heritable disorder with complex etiopathogenesis. The lifetime prevalence of schizophrenia is 0.8–1.5% of the population over 18 years; approximately 7–8 individuals out of 1000 will be diagnosed with schizophrenia in their lifetime [Reference Owen, Sawa and Mortensen1, Reference Tandon, Keshavan and Nasrallah2].
The illness has a considerable negative impact not only on patients' health and well-being, but also on their immediate environment, posing a substantial burden for primary caregivers and families. The costs of the illness management are high both for individuals and society [Reference Jin and Mosweu3]. Mortality rates are approximately two to three times higher than those of the general population, due to both natural (attributable to a variety of somatic conditions) and unnatural causes (accidents, suicides), resulting in reduced life expectancy of 15–20 years [Reference Walker, McGee and Druss4]. Comorbid medical conditions, including consequences of life-style factors (e.g., smoking) and sub-optimal treatment of physical disorders, contribute to about 60% of the excess mortality; the lifetime rate of suicide risk in schizophrenia is approximately 5% [Reference Tandon, Nasrallah and Keshavan5, Reference Hor and Taylor6].
Symptoms of schizophrenia follow a typical path of development from a premorbid phase with detectable cognitive, motor or social deficits, through a prodromal phase characterized by brief, attenuated positive symptoms, and/or functional decline [Reference Tandon, Nasrallah and Keshavan5]. Alternatively, sudden onset of psychosis is also possible. Fully developed illness manifests itself as an acute psychotic phase with positive symptoms, resulting in a post-acute and subsequently a stable phase with negative and cognitive symptoms, subthreshold or residual positive symptoms, social and functional impairment [Reference Tandon, Nasrallah and Keshavan5].
The course of illness is highly variable, typically episodic, with exacerbations and remissions. Frequent relapses contribute to neurobiological impairment, further functional and social decline, and poor treatment response [Reference Emsley, Chiliza, Asmal and Harvey7, Reference Emsley, Chiliza and Asmal8]. Relapse can be defined as a return of illness or symptoms after partial recovery; recurrence is a reappearance of illness after full remission or recovery. Exacerbation of illness might be triggered by drug withdrawal, non-specific psychosocial stressful situations (e.g., stress in professional environment, academic, personal life [relational distress]), or substance misuse. Schizophrenia outcome is a multidimensional concept that includes domains of psychopathology, social functioning, life-span and various aspects of quality of life, and societal impact [Reference Tandon, Nasrallah and Keshavan5]. Commonly cited predictors of more favorable outcome are acute onset of illness, good premorbid functioning, better cognitive function, absence of substance abuse, female gender, and a later age of onset.
More than 50% of schizophrenia patients suffer from intermittent but long-term psychiatric problems and approximately the same number of them has unfavorable outcome with chronic symptoms and disability, varying across countries [Reference Harrison, Hopper, Craig, Laska, Siegel and Wanderling9–Reference Kotov, Fochtmann, Li, Tanenberg-Karant, Constantino and Rubinstein11]. It has been shown that even chronic illness can be effectively managed. Recovery and social reintegration through adequate treatment and care is possible in many cases, up to 20% of patients meet defined criteria of recovery [Reference Jääskeläinen, Juola, Hirvonen, McGrath, Saha and Isohanni12]. However, data indicate that more than 50% of people with schizophrenia do not receive appropriate, timely, and adequate treatment. The World Health Organization assessed the accessibility of mental health services for schizophrenia patients and their utilization in 50 low- and middle-income countries [Reference Lora, Kohn, Levav, McBain, Morris and Saxena13]. The treatment gap was measured as the absolute difference between the prevalence of schizophrenia and the proportion of treated individuals. The median value for treatment coverage was 31%; i.e., approximately two thirds (69%) of the people with schizophrenia do not receive treatment. The treatment gap was larger in lower-income countries (89%) than in lower-middle-income (69%) and upper-middle-income countries (63%) [Reference Lora, Kohn, Levav, McBain, Morris and Saxena13].
More than a decade ago, the European Brain Council (EBC) published a report “The Economic Cost of Brain Disorders in Europe” [Reference Andlin-Sobocki, Jönsson, Wittchen and Olesen14]. An updated report from 2010 estimated the total cost (direct healthcare and non-medical plus indirect) of psychotic disorders (including schizophrenia) in Europe at 93.9 billion Euros, 18,796 EUR per patient [Reference Gustavsson, Svensson, Jacobi, Allgulander, Alonso and Beghi15].
In 2016, EBC launched a new project, “The Value of Treatment” (VoT) that aimed to address equality gaps across the EU in early detection and intervention, diagnostics and treatments for brain (including mental) disorders. The ultimate goal was to provide evidence-based and cost-effective policy recommendations for the adoption and implementation of a more patient-centered and sustainable coordinated care model for brain disorders [16].
The VoT project focused on a number of neurological conditions and, as a single psychiatric disorder, schizophrenia. Working groups, composed by experts of the EBC member organizations, representatives of patient and family organizations, health policy and economic experts, and drug companies developed case studies for each disorder. The aim was to analyze the socioeconomic impact and health gains of selected evidence-based healthcare interventions in comparison with the cost of current care/non-treatment by carrying out combined cost-effectiveness evaluation of selected care pathway services and patients' journey and care modeling.
The patient journey is a description of how patients experience a disease or condition from their first awareness of symptoms through all stages of the illness. It represents an alternative view on mental illness, based on person’s individual experience. Documenting the patient journey aims to identify key issues in the care for schizophrenia patients that need to be improved. A care pathway is a multidisciplinary management tool based on healthcare plan for a specific group of patients with a predictable clinical course, in which the different tasks by the professionals involved in the patient care are defined, optimized and sequenced [Reference Schrijvers, van Hoorn and Huiskes17]. The aim of a care pathway is to enhance the quality of care across the continuum by improving risk-adjusted patient outcomes, promoting patient safety, increasing patient satisfaction, and optimizing the use of resources.
In this paper, we present findings from the patients' care pathway analysis in schizophrenia. The objectives were (1) to examine the patients’ needs along the patient journey; (2) to identify gaps and opportunities for improvements in the current care pathway; and (3) to propose general policy recommendations. The results of the second part, economic modeling assessing socioeconomic impact of specific clinical interventions targeted to close some of the gaps identified in the patient journey analysis (a case study from the Czech Republic), are presented in a separate paper [Reference Winkler, Broulikova, Kondratova, Knapp, Arteel and Boyer18].
2. Methods
The schizophrenia working group, led by WG, consisted of the members of the Board of the European Psychiatric Association (EPA), representatives of the Global Alliance of Mental Illness Advocacy Networks-Europe (GAMIAN-Europe), the European Federation of Associations of Families of People with Mental Illness (EUFAMI), economic and mental health policy experts of London School of Economics (LSE), Erasmus School of Health Policy & Management, Erasmus University Rotterdam,
the Czech National Institute of Mental Health (NIMH), and the representatives of pharmaceutical industry. The study was sponsored by the EBC.
The care pathway of schizophrenia patients was analyzed in order to identify major barriers preventing patients from receiving timely and adequate treatment and care. The analysis served as the basis to develop consented recommendations on how to overcome them. Due to the heterogeneous course of illness with highly diverse individual trajectories, we focused on three highly relevant patient pathways (Fig. 1):
(1) Indicated prevention in individuals at risk of developing schizophrenia;
(2) Reducing the duration of untreated psychosis by timely intervention in patients with manifest, but not yet diagnosed schizophrenia;
(3) Relapse prevention in patients after a first episode of schizophrenia, and patients with episodic course of the illness.
The journey was based on an original inventory of needs and treatment opportunities, using focus group sessions, expert interviews, users’ input, and literature review. The scope of questions covered all fields of interest: What services are currently available? What are the unmet needs along the journey? What are the major challenges and barriers? What are the opportunities for improvement? What is the optimum model of care? What are the policy recommendations? The working group meetings, organized by the EBC, took place in Brussels between January 2016 and May 2017. Patient and family members’ needs and their perspectives along the journey were collected through discussions with the patient and family organizations and from the conclusions of separately held meetings of the patients and family organizations (EUFAMI, GAMIAN). The results are based on the consensus of the experts and stakeholders.
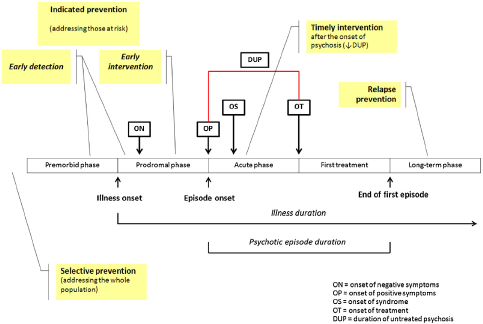
Fig. 1. Intervention strategies in the early course of schizophrenia (modified from [Reference Larsen, Friis, Haahr, Joa, Johannessen and Melle19]).
3. Results
The paramount points concerning crucial illness stages, from at risk states through recovery, are listed in the Table 1.
Factors affecting patients' journey along the schizophrenia illness trajectory found in our care path analysis are summarized in the Table 2.
4. Discussion
The value of treatment in psychiatry cannot be reduced to economic and financial aspects only. It is an asset for society, which can be measured as a value that an intervention provides to the patient and a “value for money” that the intervention provides to the payer. Thus, value comprises a combination of symptom reduction, improving quality of life, better social functioning, subjective well-being, physical health, guaranteed safety (e.g., suicide prevention programmes), and achieved cost-effectiveness. Long-term psychiatric treatment includes not only health care, but also requires resources and involvement of the social system. Comprehensive care should be provided and organised according to the patient’s needs (person-oriented care). This means an easily accessible and a seamlessly integrated care network which is aimed at improving quality of life, while respecting patients’ rights. Inevitable provisions of involuntary treatment or commitment in warranted cases must be regulated by the law, maintaining basic human rights. The network of care, where the patient is a partner, should consist of in- and out-patient services, community care centres, self-help groups, family organizations, psychiatrists, psychologists, nurses, social workers, case managers, and GP’s.
Our assessment of three pre-defined patient pathways (indicated prevention, reduction of untreated psychosis, relapse prevention) identified several critical barriers to optimal treatment.
4.1. Indicated prevention: needs and treatment gaps
Conspicuously, available health care services regularly miss or delay detection of symptoms and/or diagnosis. Current systems do not provide appropriate prevention for patients at risk and early detection services. Other contributing factors include lack of illness awareness among patients, families, and the public; lack of information, training and education among primary care providers; stigmatizing beliefs, prejudices and discriminating attitudes and actions towards schizophrenia patients.
From a biomedical perspective, selective schizophrenia prevention is not possible yet, since there are no reliable biomarkers or other measures for valid prediction of illness onset [Reference Cannon, Cornblatt and McGorry25]. Identifying individuals at risk of illness could improve early diagnosis, initiate timely treatment, and ultimately contribute to the prevention of psychotic disorders [Reference Tandon, Shah, Keshavan and Tandon26]. So far, population at-risk states can be detected only insufficiently clinically and genetically (e.g., based on family history) [Reference Smieskova, Marmy, Schmidt, Bendfeldt, Riecher-Rӧssler and Walter27]. Additional nonspecific environmental risk factors include prenatal infection or malnutrition, perinatal complications, season of birth, urbanicity, cannabis use, history of migration, etc [Reference Tandon, Keshavan and Nasrallah2].
More accessible preventive measures can be implemented in the population with manifest behavioral changes and nonspecific symptoms, such as odd thinking, social withdrawal, bizarre behavior, aggressiveness (i.e., indicated prevention). Effective prevention includes both early detection (identification of at-risk individuals, recognition of premorbid and prodromal changes) and early intervention (elimination of risk factors, preventive programs). The most typical periods for the onset of schizophrenia are late adolescence and early adulthood. Otherwise common displays of teens during puberty, adolescents, such as change of friends, giving up hobbies, worsening of school or academic performance, sleep problems, mood swings, irritability, can also be first signs of imminent psychosis, and can therefore make diagnosis difficult. Indicated prevention has a potential to prevent a transition to psychotic disorder.
Table 1 Patient and family member viewpoints.

4.1.1. Early detection
First premorbid signs of psychosis include mild cognitive impairments, social deficits; prodromes manifest themselves as ‘attenuated psychotic symptoms’, or ‘brief limited intermittent psychotic symptoms’ [Reference Fusar-Poli, Cappucciati, Borgwardt, Woods, Addington and Nelson28, Reference Schultze-Lutter, Michel, Schmidt, Schimmelmann, Maric and Salokangas29]. Early detection and intervention may reduce the risk of conversion into fully blown illness [Reference Larsen, Melle, Auestad, Haahr, Joa and Johannessen30]. Diagnosis of psychosis is based on observed behavior, subjective experiences, and reports from others who are familiar with the person [Reference American Psychiatric Association31]. Prodromal psychotic syndrome can be assessed using various measures (e.g., Structured interview for Prodromal syndromes, SIPS; Scale of Prodromal Symptoms, SOPS; At Risk Mental State, ARMS; Brief Limited Intermittent Psychotic Symptoms, BLIPS; Comprehensive Assessment of At-Risk Mental States; CAARMS) [Reference Fusar-Poli, Cappucciati, Rutigliano, Lee, Beverly and Bonoldi32–Reference Fusar-Poli, Cappucciati, De Micheli, Rutigliano and Bonoldi34]. A combination of factors can predict schizophrenia in up to 80% of young teenagers who are at high risk of developing the illness.
Table 2 Factors affecting patients’ journey.

The first recognition of psychosis is frequently not made by healthcare professionals, but by family and teachers, in medical emergency services or police / criminal justice system. Thus, awareness campaigns need to train teachers, sport coaches, etc. how to identify young people at risk. High-risk adolescents might be screened for example on the presence of prodromal symptoms or the history of schizophrenia in first-degree relatives. If necessary, an intervention program that aims to improve stress resilience, suboptimal maturation of neuronal pathways, prevent or alleviate adverse environmental circumstances and insults, can be implemented [Reference Sommer, Bearden, van Dellen, Breetvelt and Duijff20].
The setting for prevention would be schools, universities, workplaces, primary care (GP offices), or local public health authorities. A campaign underscoring the importance of an early diagnosis and intervention should also target first-line health care professionals, nurses, GP's, so they can refer patients to psychiatrists. It should be noted, that while prevention is usually funded from a budget of a single sector, prevention-related cost savings are beneficial across sectors. This makes it more difficult to persuade a single stakeholder to invest into the prevention. Convincing more stakeholders to take a joint action and invest into prevention together is a lengthy process, which requires highly developed diplomatic and negotiating skills.
Studies showed that more than 20% of schizophrenia patients who experienced barriers to contact a doctor to treat their physical problems reported stigma and fear of disclosing their mental health problem to a GP [Reference Brohan, Elgie and Sartorius35]. Reduction of stigma associated with mental illness over time is feasible and may contribute to effective prevention [Reference Angermeyer, Matschinger, Carta and Schomerus36]. Mental health awareness campaigns should use evidence-based strategies to eliminate or reduce stigma, this may subsequently also improve the early detection [Reference Thornicroft, Mehta, Clement, Evans-Lacko and Doherty37].
Media play an important role; thus, all campaigns should specifically address the negative image of mental illness and patients among general public. The term of ‘schizophrenia’ itself can be perceived negatively even by health professionals, other diagnoses are often given instead. Interestingly, some Asian countries (Japan, Korea) recently changed the term ‘schizophrenia’ into ‘integration disorder’ or 'attunement disorder', respectively, which subsequently reduced stigmatization and fostered acceptance of diagnosis [Reference Sartorius, Chiu, Heok, Lee, Ouyang and Sato38].
4.1.2. Early intervention
Many of the affected individuals suffer considerably at early stage. Symptomatic treatment (psychosocial and/or pharmacological) is indicated at this stage, especially for those with a considerable degree of distress. Cognitive behavioral therapy (CBT) can reduce the risk of developing psychosis in those at high risk after a year and is recommended by the National Institute for Health and Care Excellence (NICE) [Reference Stafford, Jackson, Mayo-Wilson, Morrison and Kendall39, 40]. Another preventive measure is to avoid psychoactive substances that have been associated with development of the disorder [Reference Picchioni and Murray41]. A number of interventions that have demonstrated efficacy in other conditions are beneficial in schizophrenia, as well (e.g., physical exercise) [Reference Rosenbaum, Tiedemann, Sherrington, Curtis and Ward42]. Preventive psychosocial interventions aim at stress reduction, educational campaigns inform about risks related to substance misuse, accessible and low-threshold services provide counseling, support, and safe social environment to interact with peers.
Early intervention programs are already available in numerous countries. There are positive long-term experience from Australia (Personal Assessment and Crisis Evaluation Clinic, PACE), United Kingdom (Outreach and Support in South London, OASIS), Denmark (OPUS Study) and others [Reference Yung, Yuen, McGorry, Phillips, Kelly and Dell’Olio43–Reference Albert, Melau, Jensen, Emborg, Jepsen and Fagerlund45]. The UK has implemented clinical guidelines and quality guidelines for such services, and the baseline auditing report has been published [46]. It reveals a large disparity in the services available across the UK, with some NHS Trusts offering the entire spectrum appropriately and others very little. The same observation applies for a view across various countries. There are data supporting the effectiveness of early intervention programs aiming to prevent schizophrenia [Reference Marshall and Rathbone47]. A meta-analysis of published studies suggested that it might be possible to delay or prevent transition to psychosis in individuals at high risk, using various (psychological, pharmacological, or nutritional) interventions, with the best evidence for CBT [Reference Stafford, Jackson, Mayo-Wilson, Morrison and Kendall39].
4.2. Timely intervention for manifested psychosis: needs and treatment gaps
Although the population screening process can be costly, early intervention services have been shown to yield significant savings in societal (health- and social-care, and productivity) costs through preventing hospitalizations, increasing employment rates and decreasing involvement with the criminal justice system [Reference Park, McCrone and Knapp48, Reference Andrew, Knapp, McCrone, Parsonage and Trachtenberg49]. Therefore, there is a need to move away from the classical model where doctors assume a passive role, sitting within the service facility, waiting for patients to "find" them.
The typical experience of family members of schizophrenia patients with the first service contact is not through prevention/screening/early interventions; in almost all cases their journey started with a crisis. Emergency medical assistance is needed, often followed by a hospital admission. There is a strong consensus that broad availability of well-organized outpatient services, mobile outreach teams, or low-threshold units (e.g., 24/7 crisis centers) could prevent many crises, involuntary treatments, it could reduce harm. The first encounter and experience with psychiatric services and treatment may determine not only patient’s attitude towards therapy, but also the future course and outcome of illness. Therefore, access to a psychiatric expert or unit should be improved. GP’s should refer the individual earlier to a specialized team; if they believe that the patient manifests with psychotic symptoms, they should refer him/her to a psychiatrist. Touchpoints for early diagnosis would be family and teachers who can reach out to psychology/counseling services.
The period between the onset of psychosis and treatment initiation is critical. Duration of untreated psychosis (DUP) is defined as the time from the first manifestation of the first psychotic symptom emergence to initiation of adequate drug treatment [Reference Murru and Carpiniello50]. DUP encompasses both extrinsic factors, such as the local legal provisions (i.e. requirement of dangerousness for involuntary treatment), accessibility to mental health services, and intrinsic, illness-related factors. Mean values of DUP range from 8 to 48 weeks, it is important to keep in mind that potential deterioration in schizophrenia occurs most aggressively in the first 2–3 years.
The duration of untreated psychosis can serve as an indirect measure of the effectiveness of early detection strategies and also as a predictor of treatment outcome [Reference Marshall, Lewis, Lockwood, Drake, Jones and Croudace51–Reference Penttilä, Jääskeläinen, Hirvonen, Isohanni and Miettunen53]. Length of DUP has been related to a poor treatment response, insufficient symptom control, prominent negative symptoms, and poor overall functional outcome (failure to achieve remission, decreased social functioning, lower quality of life) [Reference Murru and Carpiniello50]. On the other hand, evidence of the impact of DUP on the brain structural abnormalities is not fully conclusive, mainly due to the methodological inconsistencies (e.g., small sample sizes), similarly as the equivocal effect on cognitive impairment.
Early recognition and diagnosis, plus early intervention, can thus reduce the burden of schizophrenia; minimizing of DUP improves overall outcome and prognosis. Timely treatment reduce the number and duration of hospitalizations over 1–2 years after a first episode of psychosis [Reference Petersen, Jeppesen, Thorup, Abel, Øhlenschlaeger and Christensen54, Reference Craig, Garety, Power, Rahaman, Colbert and Fornells-Ambrojo55], although the impact is less clear over the longer course of illness [56, Reference Gafoor, Nitsch, McCrone, Craig, Garety and Power57].
4.3. Long-term management and relapse prevention: needs and treatment gaps
One of the principal goals in the long-term management is to prevent relapses, maintain remission, and achieve functional recovery. Optimal illness management can positively influence the whole patient journey, as the vicious circle (psychotic episode, social withdrawal, quitting job/school, functional impairment, suicidal ideations, etc.) can be broken. Ideal treatment is characterized by adequate utilization of both the pharmacological and psychosocial interventions. Patients should consult on a regular basis a specialized team, to discuss their needs, short-term and long-term goals, treatment plans. The role of a psychiatrist is to manage the treatment pathway of the patient. There is an important role of therapeutic guidelines, available evidence suggests that adherence to guidelines improves patient outcomes, in contrast to treatment as usual, driven by clinical judgment only [Reference Howes, Vergunst, Gee, McGuire, Kapur and Taylor58, Reference Bighelli, Ostuzzi, Girlanda, Cipriani, Becker and Koesters59]
Schizophrenia is typically a multi-episodic disorder. Each relapse can worsen the course and outcome of the illness, reduce treatment response, have a severe negative impact on patients, their carers, and the whole health and social system [Reference Emsley, Chiliza and Asmal8]. Therefore, relapse prevention is essential for the management of schizophrenia. Among the factors that contribute to relapse/recurrence of illness, drug discontinuation plays a prominent role. Not only complete withdrawal of medication is hazardous, but also intermittent treatment jeopardizes patient’s well-being [Reference De Hert, Sermon, Geerts, Vansteelandt and Peuskens22]. Continuous treatment has been shown to be paramount in the reduction of relapse risk; patients are able to stay relapse-free for a significantly longer period of time.
Various sources report the rate of 40–50% schizophrenia patients who are non-adherent; 50–55% of all hospitalizations can be attributed to non-adherence [Reference García, Martínez-Cengotitabengoa, López-Zurbano, Zorrilla, López and Vieta60]. Adherence to antipsychotic medication can be improved by using long-acting injectable antipsychotics (LAI), also called “depot” [Reference Haddad, Brain and Scott61]. The advantage of LAI in comparison with oral formulations was not apparent in randomized controlled trials, since these tend to exclude non-adherent patients, and also generally increase adherence [Reference Leucht, Heres, Kane, Kissling, Davis and Leucht62, Reference Kane, Kishimoto and Correll63]. True benefit of LAI has been shown in pragmatic naturalistic studies that enroll all ‘real-life’ patients, including those who are non-adherent, relapsing, non-cooperative, with comorbid physical conditions, with aggressive behavior [Reference Kirson, Weiden, Yermakov, Huang, Samuelson and Offord64, Reference Mohr, Knytl, Voráčková, Bravermanová and Melicher65].
Non-pharmacological interventions include psychoeducation, problem-oriented therapy, management of symptoms with cognitive-behavioral therapy (CBT), social skills training, cognitive remediation, etc. Involvement of the caregivers is very important: they need to be provided with information about the illness, psychoeducation on the importance of treatment continuity, how to recognize early symptoms of a new episode. Electronic systems monitoring early warning signs of imminent relapse (using text messages, apps, actigraphs) can be also employed. Telemetric warning signs monitoring (e.g., ITAREPS program) may significantly reduce the risk of relapse and help in timely intervention [Reference Spaniel, Vohlídka, Hrdlicka, Kozený, Novák and Motlová24, Reference Komatsu, Sekine, Okamura, Kanahara, Okita and Matsubara66]. Moreover, technology could be used to monitor stable patients. The follow-up of patients on regular basis (monthly, bi-monthly, or three-monthly) could be automatic: i.e. electronic reminders sent to the patient and caregivers with a text indicating that the patient has an appointment. If the patient does not show up, a member of the assertive outreach mobile team or the informal carer can visit the patient at home [Reference Van Loon, Peuskens, Dubois, Gillain, Vanderboelle and Geerts67].
Although insight (self-awareness of illness) is a prerequisite for therapy adherence and self-management, it might not be easily achieved [Reference Forbes68]. Self-awareness of illness is a concept used to describe patient's acknowledgement of his/her strengths and limitations, in particular the ability to understand the nature of impairment and recognize its implications. Patients may not believe they are ill and may deny the need for therapy or they may have such disorganized thinking that they cannot remember to take their daily doses. There is a range of interventions that facilitate the development or improvement of self-awareness. Generally, it is believed that an individualized approach to address impairments of self-awareness is necessary: it takes into account whether the impairment of self-awareness is neurological, psychological or environmental in origin [Reference Fleming and Ownsworth69].
People with schizophrenia can take an active role in managing their own condition. Once they learn basic facts about the illness and its treatment, they can make informed decisions about their care, including pharmacotherapy, actively participate in shared decision on treatment and drug choice [Reference Morrison, Hutton, Shiers and Turkington70]. If patients know how to watch for the early warning signs of relapse and how to make a plan to respond, they can learn how to prevent relapses. Patients can also develop and use coping skills to deal with persistent symptoms.
4.4. Long-term management: towards recovery
The prognosis of social and professional reintegration is negatively correlated with the number of episodes of illness. Longer duration of untreated psychosis, higher number of relapses make it more difficult to fully recover and recovery will take more time. Moreover, untreated illness is associated with substance abuse and increased risk of violent behavior. A major factor causing non-adherence to drug treatment, in addition to illness-related factors (lack of insight), is that patients are often not well informed on the medication side effects and/or how to manage them.
Symptoms and cognitive impairment disrupt the psychosocial functioning of schizophrenia patients and often result in social problems, e.g., difficulties in relationships, giving up hobbies, decline in academic and/or work performance with subsequent economic and social decline [Reference Galderisi, Rossi, Rocca, Bertolino, Mucci and Bucci71]. The onset of illness during adolescence or young adulthood prevents patients from completing their academic or vocational training, establishing age-appropriate social relationships, initiating family life. Throughout the course of illness, impairments in adaptive life skills are a major source of disability. Many patients have difficulty keeping a job or taking care of themselves; thus, they have to rely on others to assist them. Stigmatizing attitudes and beliefs about schizophrenia are widespread and may interfere with patients’ willingness to discuss their problems and seek treatment. High unemployment rate, lower educational level and socioeconomic status compared to unaffected peers, with subsequent dependence on social welfare may also have a negative impact on real-life functioning. Moreover, schizophrenia is associated with poor physical health, premature death and suicide, prejudice (stigma) and discrimination in many facets of life [Reference Corrigan and Watson72, Reference Fleischhacker, Arango, Arteel, Barnes, Carpenter and Duckworth73].
On the other hand, if properly treated via integrated biopsychosocial approach (including optimal antipsychotic treatment combined with psychosocial interventions), people with schizophrenia can live a fulfilling life. Effective, low-dose, safe and continuous antipsychotic treatment might lead to a functional recovery [Reference De Hert, Sermon, Geerts, Vansteelandt and Peuskens22]. In the long-term management, the availability of rehabilitation programs is limited.
Rehabilitation emphasizes social and vocational training to assist people with schizophrenia participate fully in their communities. Since the patients’ professional and social life trajectories are compromised, they need to develop new skills to reintegrate. Rehabilitation programs include employment services, money management counseling, cognitive remediation, and social skills training. These non-pharmacological interventions play an important role in the long-term schizophrenia management, improving overall functioning. Work reintegration is a frequently expressed goal for patients. While some patients cannot pursue their professional activity, many continue to work or wish to do so. The ability to keep a job with adequate support often results in improved quality of life and minimizes the negative financial impact and the risk of social exclusion.
We can witness a shift from emphasis on symptom control, achieving and maintaining remission, to the functional recovery. This approach is supported by growing clinical evidence indicating that a certain degree of recovery is possible, despite the presence of residual symptoms, and that some people with schizophrenia actually may achieve full recovery [Reference Warner74].
There are different definitions of recovery, clinical and patient-based [Reference Van Eck, Burger, Vellinga, Schirmbeck and de Haan75]. The clinical recovery accentuates remission and functional improvement. Remission is defined as a reduction/absence of symptoms to the point that they do not interfere significantly with behaviour, using clinical rating scales [Reference Liberman, Kopelowicz, Ventura and Gutkind76, Reference Andreasen, Carpenter, Jr, Kane, Lasser and Marder77]. Functional improvement implies the ability to function in the community, socially and vocationally living independently, having friends, etc. The patient-based definition of recovery has been developed based on personal experiences of people with mental illness [Reference Van Eck, Burger, Vellinga, Schirmbeck and de Haan75]. The most frequently used definition is: “the development of new meaning and purpose in one’s life, as one grows beyond the catastrophic effects of mental illness.” [Reference Anthony78] Recovery from schizophrenia is a highly individual process. The four key processes of personal recovery are finding hope, re-establishment of identity, finding meaning in life, and taking responsibility for recovery. In other words: connectedness, hope, identity, meaning, and empowerment (the acronym “CHIME”) [Reference Andresen, Oades and Caputi79, Reference Leamy, Bird, Le Boutillier, Williams and Slade80].
Box 1 Opportunities for improvement in the management of schizophrenia.
Fight stigma, raise awareness, target public opinion, policy makers, other medical professionals (including GP’s), media.
Be inspired and learn from available experiences and existing preventive programs.
Promote psychoeducation.
Develop network of outpatient and community services; improve access to social services.
Provide individual case management to address specific patient’s needs.
Make non-pharmacological therapeutic options available (CBT, cognitive remediation…).
Utilize new drug formulations (e.g., long-acting injectable, LAI).
Employ IT technologies in monitoring early warning signs and relapse prevention.
Use real-life (effectiveness) outcome measures beyond symptom control: subjective well-being, satisfaction with medication, quality of life, functional recovery.
Focus on somatic health of patients, improve their physical well-being.
Reduce burden of comorbidities (e.g., substance abuse).
Engage patients in treatment decisions.
Support active involvement of families and families organizations.
Box 2 Policy recommendations.
Promote and facilitate efficient health services organization: develop integrated community care and the cooperation of caregivers, social workers, nurses, psychologists, specialists, families, and peers.
Improve economic aspects (cost-effectiveness) of the systems: promote early detection programs and utilize most already available treatments.
Consider evidence-based resource allocations, support neuroscience research.
Governmental financial incentives are needed to create the optimal environment to succeed.
Shift policy recommendations from reducing high costs of brain disorders to modification of health systems. Close the gap between public policies and practice.
Raise awareness of general public and other medical professionals; fight stigma. Support volunteers empowered by professionals and responsible authorities.
Support patients and groups of caregivers for information, expertise, sharing experiences, and advocacy.
Facilitate the establishment of active partnerships and cooperation with other stakeholders, e.g. the media organizations (local, regional, national, European and academic institutions), employers and trade unions, pharmaceutical industry, governments, regulatory bodies and insurers with a goal to
○ secure the best possible treatment for patients with a mental illness and at the earliest possible opportunity.
○ support the development of health/mental health policies which take into account patients’ perspective.
Recovery is not mere absence of symptoms, but a journey through which the person may achieve a meaningful life. Attaining an improved quality of life, physical health, social integration, instrumental competence and self-agency, independent living, and competitive employment can be seen as elements of a meaningful life, and therefore pursued to a variable degree, depending on the person and the context.
Our analysis of the patient journey showed that the current model of care does not provide optimal management of schizophrenia due to the poor collaboration among health and social care professionals and lack of continuity of the antipsychotic treatment. Furthermore, there is insufficient cooperation between care providers and patients and their families, plus inadequate utilization of pharmacological and psychosocial interventions, and proper patient monitoring. There is still low implementation of deinstitutionalization across many, especially Central and Eastern European countries [Reference Winkler, Krupchanka, Roberts, Kondratova, Machů and Höschl81]. Taking patients out of the hospitals, back to their own environments, has been demonstrated to be beneficial to the patients while not leading to severe adverse consequences [Reference Kunitoh82–Reference Winkler, Barrett, McCrone, Csémy, Janousková and Höschl84]. By deinstitutionalization, we mean a careful and responsible shift in the locus of care from psychiatric hospitals to communities, i.e. strongly supporting community care and families while making a transition and reducing the number of beds in long-term psychiatric wards.
The reviewed data suggested a significant overlap between patient/family and professional perspectives - trust amongst them being the foundation for successful management throughout the illness course [Reference Gaebel, Muijen, Baumann, Bhugra and Wassermann85]. Opportunities for further improvement of care provided by the mental health professionals can be seen in various areas, as summarized in the Box 1.
The results of our analysis have also significant policy implications. Based on the available evidence and users’ needs, further supported by the economic data, we can sum up general policy recommendations addressed to the policymakers and respective authorities (Box 2).
5. Conclusions
Most people with schizophrenia need a lifelong treatment; however, they can live their own life if they receive timely and proper treatment. In general, we found that the provision of early detection and early intervention programs is of great importance for an effective management of the illness. Optimal management requires a paradigm shift in the focus of schizophrenia treatment, from mere symptom control, achieving and maintaining remission, to the emphasis on recovery. Economic arguments supporting this call are provided in the accompanying report [Reference Winkler, Broulikova, Kondratova, Knapp, Arteel and Boyer18]. Changing the paradigm demands challenging adaptations of health and social care, moving away from fragmentation to a seamless care model. For this purpose, effective mental health policies are needed.
Funding
This work on schizophrenia is part of a series of case studies covering nine neurological and psychiatric conditions, conducted within the “Value of Treatment for Brain Disorders” research project of the European Brain Council. PM and PW were supported by the Ministry of Education, Youth and Sports of the Czech Republic (project NPU4NUDZ: LO1611); PM was supported by the Ministry of Health of the Czech Republic (grant No. AZV 15-28998A).
Declarations of interest
None.






Comments
No Comments have been published for this article.