Introduction
Coronavirus disease 2019 (COVID-19) has led to the first truly global pandemic. At the time of writing this paper, there were over 2 million reported cases worldwide and more than 130,000 deaths attributed to COVID-19 acute infection [Reference Dong, Du and Gardner1]. Based on models of its spread, and potential for morbidity and mortality, most governments worldwide have adopted mitigation strategies that essentially limit social contacts [Reference CJL2,Reference Ferguson, Laydon, Nedjati-Gilani, Imai, Ainslie and Baguelin3]. The goal of these measures is to “flatten the curve” of acute presentations so as to prevent widespread morbidity and the breakdown of health care systems. Variants of these social mitigation strategies range from “social distancing,” at-home confinement—referred to as “self-isolation,” to selective “quarantine,” and to population “lockdown” that includes restriction of movement outdoors and closure of schools and all nonessential services and businesses.
None of the existing models have factored the possible adverse mental health effects of mitigation at a population level. These adverse effects can be intuitively anticipated, but have never been rigorously modeled [Reference Brooks, Webster, Smith, Woodland, Wessely and Greenberg4]. Negative mental health outcomes can be attributed to the emotional and physiological effects of the risk posed by the virus and by reduced physical activity, social interaction, and human physical contact [Reference Kerr, Wiechula, Feo, Schultz and Kitson5–Reference Jones and Sloan7]. Studies on prior pandemics, such as the severe acute respiratory syndrome (SARS), found that the length of quarantine was an important predictor of post-traumatic stress disorder, depression, and anxiety, with a cumulative prevalence exceeding 30% of the population [Reference Hawryluck, Gold, Robinson, Pogorski, Galea and Styra8,Reference Reynolds, Garay, Deamond, Moran, Gold and Styra9]. Psychosocial stressors within families and loneliness for those living alone are also likely to spike in confinement and have adverse effects on mental and physical health [Reference Rendall, Weden, Favreault and Waldron10–Reference Fiorillo and Gorwood15]. Available data suggest that stress associated with population-wide disasters increases the level of violence, including domestic violence and child abuse [Reference Stark and Ager16,Reference Schumacher, Coffey, Norris, Tracy, Clements and Galea17]. These are recognized risk factors for mental health and substance abuse problems [Reference Van Der Velden, Kleber, Neria, Galea and Norris18] as well as suicide [Reference Reger, Stanley and Joiner19].
The anticipated impact of the COVID-19 pandemic on mental health is expected to be significant but has not been considered in the formulation of current public policies. To address this gap, this study makes a rapid model-projection concerning the years of life lost (YLL) if restrictive social mitigation measures are implemented for a period of 3 months. This duration was chosen as it aligns with the expected duration of social mitigation in many countries. We used data from Switzerland as an example. YLL indicates the number of years that persons affected by the disease or condition are likely to die earlier than they would otherwise. YLL is a measure frequently used in the literature to indicate the health costs of a disease or condition, including for COVID-19 [Reference Hanlon, Chadwick, Anoop, Wood, Minton and McCartney20]. The model focuses on what we consider to be the major contributors to YLL affecting the majority of the population, namely suicide, emergence or increase in psychopathology, childhood physical abuse, and continued restriction of movement and at-home confinement.
To be clear, this model focuses on changes in psychosocial risk factors. The COVID-19 crisis may also have other adverse consequences that may impact on longevity, such as economic adversity, changes to activities of daily living such as eating, sleeping, smoking and ordinary alcohol consumption, or decrease in medical provision to those who have health problems unrelated to COVID-19. Such additional factors are, however, beyond the scope of this study. A more precise estimation of the mental health impact of the pandemic will be possible as relevant data become available.
Methods
Model
We conducted a literature review focusing on studies reporting on YLL in connection to situations conceptually similar to the current pandemic. These included data from studies on confinement in different contexts and from previous disasters, including pandemics. The model includes literature that appeared up to April 18, 2020. We focused on studies from developed countries, primarily Switzerland, and when not available, from Europe followed by the United States, based on the United Nations Development Program Country Classification System. Switzerland has a population of 8.57 million [21] and introduced an “extraordinary situation” on March 16, 2020. All boarders were closed to travel; all schools, markets, restaurants, nonessential shops, bars, and entertainment and leisure facilities were closed; and all public and private events and gatherings were prohibited [22]. Several regions had already taken a number of these measures in the preceding days and weeks. The Federal Council called on members of the public to avoid all unnecessary contact, maintain physical distance from others, and stay whenever possible at home. According to government announcements, these measures are expected to continue until at least April 27, 2020, while a number of measures aimed at “social distancing,” including prohibition of gatherings, are expected to last until at least June 8 [23].
The following risk factors were considered based on their importance and data availability: suicidality, depression, alcohol use disorder (AUD), childhood trauma due to domestic violence, changes in marital status, and social isolation. The projection of YLL for each of these factors is further described below. Data concerning the incidence of the risk factors as well as their impact on YLL were then applied to a model that assumes population-wide severe social mitigation policies (stay-at-home and restriction of outdoors movement) for a duration of 3 months. As a general rule, the present model erred on the conservative side when choosing YLL. For purposes of illustration only, we also present projected YLL for countries other than Switzerland based on their population size [24] assuming similar prevalence of risk factors.
The model involved a six-step process.
For each factor,
1. Estimation of baseline risk of outcome i (BRi) based on the literature.
2. Estimation of YLL per incident of outcome i (YLLi) from the literature.
3. Estimation of increased risk factor during the pandemic for outcome i (PRi), where possible based on literature.
4. Estimation of the increased incident cases relating to the pandemic outcome i (PICi).
PICi = (PRi – 1) × BRi × 0.25, where PRi is the estimate of the increased risk of outcome i relating to the pandemic and D is the duration of the social mitigation measures, which is fixed 0.25 years (3 months)i.
5. Estimation of YLL for incidence due to the pandemic (PYYLi).
PYLLi = PICi × YLLi.
6. Calculation of summary statistics.
PICs is the sum of all PICi; PYLLs is the sum of all PYLLi.
Average YLL per impacted person: PICs/PYLLs.
Percentage of persons impacted: PICs/100 × population of Switzerland (8.57 million).
Average PYLL per person of the general population: PYLLs/population of Switzerland (8.57 million).
To align with current models that focus on acute mortality, we focus on the 3-month period which represents an underestimate of the overall impact of the pandemic.
Results
A summary of the results is provided in Table 1, and details of the estimation of the increased YLL linked to the pandemic are presented below. For illustrative purposes only, we also extrapolated these numbers to other selected countries, if their confinement measures, disorder, and social representation were the same as those in Switzerland (this is simply a multiplication of YLL by the size of the population) (see Table 2).
Table 1. Projection of lost years of life for the population of Switzerland due to demographics and mental health changes related to a mass confinement of 3 months.

Abbreviations: PICi, estimated persons affected with reduced longevity; YLL, years of life lost.
Table 2. Number of years of life lost that selected other countries would be projected to have, if their confinement measures, disorder, and social representation were the same as those in Switzerland (this is simply a multiplication of the YLL by the size of the population).
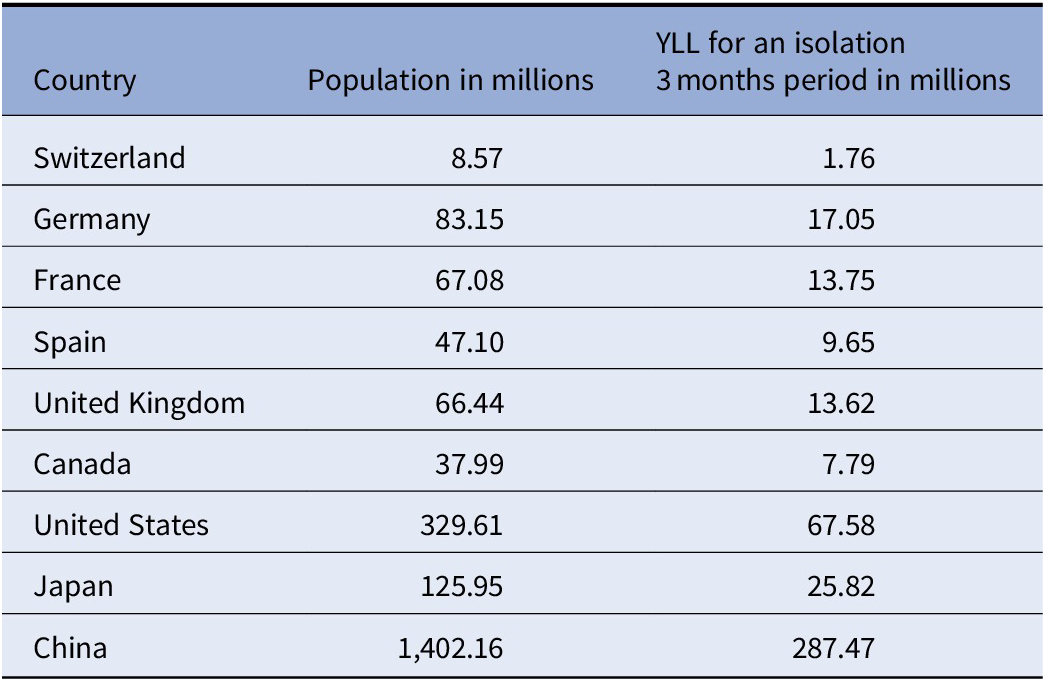
Population numbers for countries other than Switzerland were sourced from Wikipedia [24].
Abbreviation: YLL, years of life lost.
Suicidality
BRi: In 2017, Switzerland counted 1,043 suicides excluding assisted suicide or euthanasia. Non-euthanasia-related suicide was the cause of death in 16 out of 1,000 deaths [25].
YLLi: U.S. data from 2016 showed 1.542 million years were lost due to suicide [26] across 44,965 suicides [27] leading to 34.3 YLL per death (1.542 million/44,965).
PRi: We extrapolated on the relationship between confinement and suicidality from data from the penitentiary system. Community cell-confined prisoners already have an increased suicide rate by factors between 3.5 and 21 compared to the general population [Reference Roma, Pompili, Lester, Girardi and Ferracuti28,Reference Eck, Scouflaire, Debien, Amad, Sannier and Chan Chee29]. However, the risk of suicide for prisoners in single cells is further increased, approximately 9–15 times [Reference Duthe, Hazard, Kensey and Shon30]. Extrapolating from these data, we assume that confinement in the household increases their likelihood of suicide by a factor of 3 in multi-person households and a factor of 27 in single-person households (3 × 9). We assume this increase is stable for the entire 3-month duration. In Switzerland, 16% of the population live in single-person households [31]. These calculations result in a population-wide PRi of 6.84 (0.16 × 27 + 0.84 × 3).
PICi: 5.84 × 1,043 × 0.25 = 1,523 additional suicides.
PYLLi: 1,523 × 34.3 = 52,239.
Depression
General: As mood and anxiety disorders are comorbid, we used data on depression in our model as it is likely to capture much of the distress-related psychopathology; additionally, depression has the most convincing link to YLL, which is our outcome of interest [Reference Charlson, Baxter, Dua, Degenhardt, Whiteford, Vos, Patel, Chisholm, Dua, Laxminarayan and Medina-Mora32].
BRi: We used population prevalence data for depression as they capture both incident and preexisting conditions [Reference Wittchen, Jacobi, Rehm, Gustavsson, Svensson and Jonsson33,Reference Ten Have, Penninx, Tuithof, van Dorsselaer, Kleinjan and Spijker34]. Accordingly, we estimated that the prepandemic risk of depression for the Swiss population in a 3-month period is 3.45% (i.e., 8.57 million × 0.0345 = 295,665) with 64.7% of affected individuals being women. Because BRi is already adjusted for the 3-month period, no further correction for PICi was undertaken.
YLLi: Using data from a prior study on depression [Reference Plana-Ripoll, Pedersen, Agerbo, Holtz, Erlangsen and Canudas-Romo35], we assumed loss of 7.91 years of life for men and 6.22 for women. Given the male–female ratio for depression (64.7% women), this results in YLLi = 6.82.
PRi: Three years after the SARS epidemic, the proportion of persons with symptoms related to higher stress was still increased by a factor of 3.47 among those who had been in quarantine, thus demonstrating the long-term implications of the phenomenon [Reference Wu, Fang, Guan, Fan, Kong and Yao36]. A study of an Australian population quarantined due to equine flu suggested a similar threefold increase in depression [Reference Taylor, Agho, Stevens and Raphael37]. Finally, a study on depression during the lockdown in Switzerland indicated that moderately severe and severe depression prevalence had risen from 3.4 to 9.1% in only 3 weeks of confinement [Reference De Quervain, Aerni, Amini, Bentz, Coynel and Gerhards38]. Therefore, we used an estimate of PRi = 3 as an initial estimate in order to remain conservative. We also factored in that—given therapy—84% of individuals with depression are likely to remit within 3 years [Reference Ten Have, Penninx, Tuithof, van Dorsselaer, Kleinjan and Spijker34]. To be conservative and to capture cases most likely associated with mortality, we adjusted the model accordingly, leading to a PRi of 1.32.
PICi: 295,665 × 0.32 = 94,613.
PYLLi: 94,613 × 6.82 = 645,260 YLL.
Alcohol use disorder
General: Distress under any circumstances is a known risk factor for AUD. There is abundant evidence of increased alcohol consumption during the current pandemic [Reference Clay and Parker39] including a report of approximately one-third increase in alcohol sales in Germany [Reference Bartel40]. Additionally, a study on the Chinese population indicates that harmful drinking may be increased by a factor of 5.8 in the most affected Hubei province compared to other Chinese provinces [Reference Ahmed, Ahmed, Aibao, Hanbin, Siyu and Ahmad41]. Although the use of other substances may be increased as well, our model focuses on AUD as it is the most prevalent substance abuse disorder and the major contributor to mortality worldwide [42]. Substance use disorders are significantly associated with increased mortality due to increased accidents, impulse dyscontrol leading to violence and suicide, as well as increased physical morbidity (i.e., cardiovascular, gastrointestinal, hepatic, and other somatic conditions) [Reference Hiroeh, Appleby, Mortensen and Dunn43–Reference Westman, Wahlbeck, Laursen, Gissler, Nordentoft and Hallgren45].
BRi: In Switzerland, 16.1% of men and 3.2% of women were estimated to suffer from AUD, meaning that 83.5% of cases are men and 16.5% are women [42].
YLLi: A cross-national Scandinavian study indicated that life expectancy among inpatients with AUD was reduced by 24–28 years compared to the general population [Reference Westman, Wahlbeck, Laursen, Gissler, Nordentoft and Hallgren45]. When only deaths from natural causes are considered, then life expectancy is reduced by 18.1 years in men and 16.5 years in women [Reference Hiroeh, Kapur, Webb, Dunn, Mortensen and Appleby44]. To be conservative, and to account for the preponderance of men with AUD, we assumed a reduction of life expectancy by 18 years in men (83.5% of cases) and 16 years in women (16.5% of cases), resulting in a total YLLi of 17.67 years.
PRi: We assume a population-level increase in AUD of 0.15% per month, with the first month leading to a higher incidence (0.3%). Therefore, countermeasures lasting 3 months would increase incidence by approximately 0.6%.
PICi: 0.6% of the population (8.57 million) = 51,000.
PYLLi: 51,000 × 17.67 = 901,170.
Marital status
General: Recent media reports indicate that divorce rates have increased since the instigation of COVID-19 mitigation policies [Reference Smith11,Reference Prasso46]. In individual cases, divorces and separations can be beneficial to individual health and stress levels (e.g., in situations of abuse). Overall, however, even after taking into account risk factors that contribute to divorce and separation (i.e., financial stressors, mental and physical illness, and substance abuse), divorce and separation, given the experience of relational and economic stress, loss, and greater likelihood for social isolation, have been shown to have a negative impact on longevity [Reference Rendall, Weden, Favreault and Waldron10]. Causes for this may also include detrimental habits that individuals may adopt to cope with the stress, loss, and isolation (such as increased smoking [Reference Bourassa, Ruiz and Sbarra47]). Additionally, having parents who divorce during childhood has been estimated to increase mortality by 44% and reduce life expectancy by an average of 4 years [Reference Martin, Friedman, Clark and Tucker48].
BRi: In 2018, there were 16,542 divorces in Switzerland leading to a BRi = 33,084. Additionally, 12,212 minors were affected by the breakdown of marital relationships [49].
YLLi: A German study estimated that YLL attributable to divorce range between 3 and 8 years for women and 4 and 9 years for men [Reference Muth, Kruse and Doblhammer50]. For this projection, 3.5 YLLi were modeled per couple (4 years for men and 3 years for women) and 4 years for each affected minor [Reference Martin, Friedman, Clark and Tucker48].
PRi: We based our calculation on the increase in divorce rate for the year following the Hurricane Hugo disaster [Reference Cohan and Cole51] (wherefore, factor D is omitted in the calculation of PICi). PRi was modeled as 1.63.
PICi: for adults, 33,084 × 0.63 = 20,842; for affected minors: 12,212 × 0.63 = 7,694.
PYLLi: for adults, 20,842 × 3.5 = 72,947; for affected minors: 7,694 × 4 = 30,776.
Childhood trauma due to domestic violence
General: Although family violence is commonly targeted toward both women and children, we focus specifically on the effects on children, as specific impact on women was hard to quantify.
BRi: Even when not directly being the victim themselves, children being witnesses to violence can be an adverse childhood event (ACE).
In 2013, 9,381 victims of domestic violence registered by the Swiss police. However, a survey indicated that this latter number of victims would only represent 22% of the actual number, which would increase the number to 42,641 victims per year (9,381/22 × 100). A total of 64.5% of domestic violence referred to violent interactions between either parents and their children or current romantic partners [Reference Zoder52] (42,641 × 0.645 = 27,503). Of Swiss multi-person-households, 46% include children [31], and on average there are 1.76 children living in each of these households [Reference Csonka and Mosimann53]. BRi is therefore assumed to be 22,266 (27,503 × 0.46 × 1.76).
YLLi: Experiencing three or more ACEs is associated with 9.5 years of reduced expected quality longevity [Reference Jia and Lubetkin54]. Among adults, 25% report having experienced multiple adverse childhood events [Reference Merrick, Ford, Ports and Guinn55]. Because of this, we conservatively project that only about every fourth of these events will lead to the full loss of 9.5 years; we therefore adjusted the YLLi to 2.37 years.
PRi: According to the World Health Organization, there has been a threefold increase in family violence since the start of the pandemic [56]. However, additional events are not likely to be normally distributed across victims [Reference Zoder52], and the measures to which these numbers refer may have been stricter than the one in Switzerland; accordingly, we adopted a conservative PRi = 2.
PICi: 22,266 × 1 × 0.25 = 5,567.
PYLLi: 5,567 × 2.37 = 13,194.
Social isolation and reduced social connectedness
General: No studies were found that indicated the cost of social isolation or reduced social connectivity in YLL in a way directly adaptable to this study. Moreover, the entire population is somewhere on a spectrum from socially hyperconnected to socially isolated. However, studies concerning risk ratios do exist.
BRi: The entire Swiss population of 8.57 million is on a spectrum from socially connected to socially isolated, depending on their personal circumstances.
YLLi: Based on the most recent data, Switzerland counted 67,008 deaths in 2018 that were distributed across age groups as follows: category 1 (ages: 0–19): 0.8%; category 2 (Reference Hanlon, Chadwick, Anoop, Wood, Minton and McCartney20–Reference Clay and Parker39): 1.2%; category 3 (40–64): 11.1%; category 4 (65–79): 25.0%; and category 5 (80+): 61.9% (25). There are no data informing on the baseline number of deaths that can be attributed to social disconnection or loneliness. In response, we averaged the life expectancy of men and women and calculated YLLi according to the following steps: (a) life expectancy by category was taken from the Federal Statistical Office of Switzerland, which gives remaining life expectancy at birth and 30, 50, 65, and 80 years of age [57]. (b) We then conservatively adjusted YLL for each age category as a very rough approximation. This approximation is—if anything—aimed at underestimating the remaining life expectancy (category 1: 73.45, category 2: 54.2, category 3: 34.8, category 4: 15.5, and category 5: 4.95). (c) Overall, remaining life expectancy was then multiplied with the percentage of deaths in each age group, leading to a cumulative YLLi = 12.03 for each additional death.
PRi: Having more social connections has been associated with lower death rate with an odds ratio of 1.5 [Reference Holt-Lunstad, Smith and Layton58]. Conversely, a comprehensive meta-analysis indicated that social isolation is associated with an increase of all-cause mortality by a factor of 1.29 [Reference Holt-Lunstad, Smith, Baker, Harris and Stephenson59]. Similarly, a large-scale study estimated that social isolation increased the hazard risk by a factor of 1.26 after adjusting for multiple potential confounders, including anxiety, depression, and lower socioeconomic status [Reference Elovainio, Hakulinen, Pulkki-Raback, Virtanen, Josefsson and Jokela60]. In our model, we use the most conservative estimate of 1.26. In a phase of confinement, we assume that the majority of the population (75%) experiences either reduced social connectedness and/or increased social isolation. This would lead to a PRi of 1.208.
PICi: Based on the 2018 data on the number of deaths in Switzerland (n = 67,008) [25], PICi was estimated as 67,008 × 0.208 × 0.25 = 3,484.
PYLLi: 3,484 × 12.03 = 41,912.
Summary statistics
The findings presented above are summarized in Table 1. The contribution of the different risk factors to PYLL in descending order was as follows: AUD: 901,170, depression: 645,260, divorce: 103,723, suicide: 52,239, reduction of social contact: 41,912, and averse childhood events due to domestic violence: 13,194.
The sum of all PYLLi was 1,757,498. This represents 0.205 PYLL per person in Switzerland (1,757,498/8.57 million) (Table 1). In other words, we project a loss of 10 weeks and 5 days due to COVID-19 related mitigation strategies, if YLL is equally distributed in the entire Swiss population. The sum of all PICi was 179,520, which represents 2.1% of the Swiss population (179,520/8.57 million). Assuming that this subpopulation will be most impacted, the average PYLL was estimated to be 9.79 (1,757,498/179,520 = 9.79).
Discussion
This study focused on YLL due to the social mitigation strategies implemented in response to the COVID-19 pandemic, with a primary focus on the consequences of at-home confinement and restriction to freedom of movement.
The literature suggests that increased duration of confinement is associated with worse outcomes for psychological health of those confined [Reference Brooks, Webster, Smith, Woodland, Wessely and Greenberg4]. While some of the stress-related problems ensuing from confinement may remit, an important portion of this damage may prove to be hard or impossible to reverse and the affected individuals may experience ongoing suffering. Our projection suggests that the Swiss population will incur a substantial increase in mortality as a consequence of confinement-related psychosocial stress, which should be considered in forming public health responses to the pandemic. In the face of confinement measures, it is therefore important that mental health workers are given maximum support from all sides, including government, in order to be able to keep providing their services. Further, it is important that policy makers factor mental health when conducting cost–benefit analyses of mitigation strategies.
This study hopes to have achieved three aims: (a) to provide information that helps authorities to consider whether and, if so, how to enact these countermeasures and what resources to employ for mitigation of their adverse consequences; (b) specifically, to indicate the importance of support for mental health care workers in order to allow them to be maximally efficient in the face of confinement measures; and (c) to make the case for more comprehensive modeling of the effect of pandemic responses beyond the immediate risk attributed to acute infection.
Limitations
As we demonstrate here, the evidence base for building such comprehensive models is limited, and accordingly we had to make several assumptions. In this sense, our model projection is obviously constrained by the limitations of the available literature which, itself, involves a number of unknowns and the unknown future of mitigation measures as well as their easing. Given the time constraints, the uncertainty in those assumptions is increased; the authors, however, judge the urgency of such projections to be very high at the moment. Moreover, in this respect, our model is not dissimilar to current projections of the spread and consequences of COVID-19 which are being continually revised as more information becomes available. Additionally, the present projection is not all-encompassing concerning potential effects of confinement, such as (prolonged) grief, elder abuse, increase of sedentary lifestyle, or change of diet. The pandemic is also likely to have multiple additional consequences, including distress due to job losses and financial hardship. The projection also does not model potentially positive changes in behavior, for example, reductions in car accidents and air pollution. Due to frequent co-occurrence of certain phenomena, it is possible that a single individual may be affected by more than one of the factors presented. When possible, data were adjusted for age, sex, and socioeconomics. However, for several factors, possibilities to do so were impeded by virtue of limitations of the current literature.
Conflict of Interest
The authors received no financial support for the submitted work; the authors report no financial relationships with any organizations that might have an interest in the submitted work in the previous 3 years; the authors report no other relationships or activities that could appear to have influenced the submitted work.
Financial Support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Data Availability Statement
All applicable data are based on the existing literature and available as part of the references.





Comments
No Comments have been published for this article.