Substance use may influence the onset and course of psychosis. Reference Álvarez-Jiménez, Parker, Hetrick, McGorry and Gleeson1 Ongoing substance use is associated with negative outcomes Reference Gonzalez-Pinto, Alberich, Barbeito, Gutierrez, Vega and Ibanez2-Reference Wade, Harrigan, Edwards, Burgess, Whelan and McGorry4 but may also be a marker for other factors that affect prognosis, including younger age at onset and male gender. Reference Wade, Harrigan, Edwards, Burgess, Whelan and McGorry4 Many young people with psychosis misuse stimulant drugs; Reference Sara, Burgess, Malhi, Whiteford and Hall5,Reference Hides, Dawe, Kavanagh and Young6 however, most of these young people also misuse cannabis, Reference Degenhardt, Dierker, Chiu, Medina-Mora, Neumark and Sampson7 making it difficult to separate the effects of these two drugs. In a large Thai sample, more than half of first admissions with specific diagnoses of methamphetamine psychosis went on to have further episodes of psychosis. Reference Kittirattanapaiboon, Mahatnirunkul, Booncharoen, Thummawomg, Dumrongchai and Chutha8 We are not aware of any study examining the relationship between stimulant disorders and outcome in young people with broadly diagnosed psychoses. Our study used a large population-based sample of people aged 15-29 years with a first hospital admission with psychosis. We examined readmission within 2 years as a measure of relapse or recurrence. Reference Gleeson, Alvarez-Jimenez, Cotton, Parker and Hetrick9 Our first aim was to examine whether baseline cannabis or stimulant disorders predicted later readmission. Our second aim was to examine the impact of ongoing problem drug use on readmission.
Method
Setting and participants
The study was approved by the New South Wales (NSW) Population and Health Services Research Ethics Committee. New South Wales had an estimated resident population of 7.3 million persons in 2012, of which approximately 20% were aged 15-29. 10 Admissions to NSW state-operated (’public’) hospitals were linked using a unique health identifier.
Figure 1 summarises the study’s method. For all persons with a diagnosis of psychosis, the first ever (index) hospital admission with psychosis was identified. People aged 15-29 whose index admission occurred within the study period (July 2005 to June 2010) were included. Exclusion criteria were:
-
(a) admissions where the person was admitted and discharged on the same day;
-
(b) persons whose usual residence was another country or another Australian state;
-
(c) persons with organic psychosis or schizotypal disorder as the only psychosis diagnosis;
-
(d) persons whose index admission ended in death;
-
(e) persons not yet discharged 2 years after index admission.
The period July 2000 to June 2005 was used as a baseline period for determining incident cases. All participants had no admissions with a psychosis diagnosis for at least 5 years prior to their index admission. Admissions in the baseline period for non-psychotic conditions (such as mood, anxiety, adjustment or substance disorders) were not excluded, as these conditions frequently precede psychosis. Reference Yung and McGorry11

Fig. 1 Overview of method.
Admissions to all New South Wales (NSW) public hospitals, 2000-2012. Diagnostic exclusions: schizotypal disorder (n = 34) and organic psychosis (n = 22).
We identified readmissions to any NSW public hospital with a primary or additional diagnosis of psychosis within 2 years of discharge from the index psychosis admission. We excluded readmissions due to transfer between hospitals or occurring on the day of discharge of the index admission. Readmission data were available to 30 June 2012.
Measures
Primary and additional diagnoses were made by the treating psychiatrist and extracted from clinical notes by medical record coders. Psychosis was defined by the presence of a primary or additional ICD-10 12 diagnosis code for a psychotic disorder, including affective psychoses (mania or depression with psychosis specified) and drug-induced psychosis. Substance-related disorders were identified by diagnosis codes for abuse, dependence, intoxication or poisoning. Drug-induced psychoses were counted as both psychosis and substance use disorder. Amphetamines and cocaine were grouped into a single ‘stimulant’ disorder category. All individual substance diagnoses were recorded; polydrug disorder was recorded only where this was specifically diagnosed (ICD-10 code F19).
Binary variables were constructed to indicate prior hospital admissions with non-psychotic mental health conditions, cannabis disorders or stimulant disorders.
Migration status was based on country of birth recorded at index admission. Rurality and disadvantage measures used Australian Bureau of Statistics reference data (available at http://www.abs.gov.au/ausstats/abs@nsf/mf/2033.0.55.001 and http://www.abs.gov.au/websitedbs/d3310114.nsf/home/remoteness+structure) for the statistical local area of residence at index admission.
A proxy measure of ongoing problem drug use was constructed for individuals who had contact with community mental health services or were readmitted to hospital for any reason after their index admission. This proxy measure could not be constructed where a person had no further contact with NSW hospital or community services following their index admission. New South Wales in-patient and community mental health services collect diagnoses and periodic ratings using the Health of the Nation Outcomes Scales (HoNOS). Reference Wing, Beevor, Curtis, Park, Hadden and Burns13 Ratings are made by the treating clinician (case manager or psychiatrist). Ongoing drug problems were defined as present if, during the follow-up period, the person had either (a) any diagnosis of a substance use disorder in hospital or community records or (b) at least one completed HoNOS with a score of 2 (’Loss of control of drinking or drug-taking’), 3 (’Marked craving or dependence’) or 4 (’Incapacitated by alcohol and drug problems’) on the HoNOS Problem Drinking or Drug-taking Scale (i.e. HoNOS Item 2). HoNOS does not distinguish the type of substance used. A threshold score of 2 or more was chosen to define problem substance use, in keeping with expert clinician ratings of ‘clinically significant’ problems on the HoNOS. Reference Burgess, Trauer, Coombs, McKay and Pirkis14 Baseline and ongoing drug diagnosis and HoNOS measures were combined to create a composite variable with three possible values: no drug problem (baseline or ongoing), drug problem ceased (drug diagnosis at index admission but no ongoing problem) and drug problem ongoing (drug problem in ongoing measure, with or without drug diagnosis at index admission).
Analysis
Statistical analyses were undertaken using Stata v11 SE for Windows. Univariate Cox regressions were conducted on candidate variables. Proportional hazards assumptions were tested by visual examination of log-log survival plots and by testing for significant interactions when each variable was entered as a time-based covariate. Variables of interest, with univariate P<0.2, and which satisfied proportional hazards assumptions, were entered into a multivariate Cox regression. This model was stratified on local mental health service, because observations may have been correlated within health services due to local population or resource factors. Two variables failed proportional hazards assumptions and were therefore included as stratifiers rather than covariates: (a) admission to a non-specialised mental health unit; and (b) psychosis as a comorbid diagnosis rather than a primary diagnosis for the index admission. The distribution of deviance residuals was examined to identify multivariate outliers.
Differences between people with and without ongoing service contact were examined using binary logistic regression. The proxy measure of ongoing drug problems was analysed for the subset of participants for whom the measure was available, using the same Cox regression method described above.
Results
There were 7269 persons aged 15-29 who had a first admission in the study period (Table 1). Two-thirds (66%) were male and only 24% were aged under 20. The most common diagnoses at first admission were schizophrenia or delusional disorders (36%) and drug-induced psychosis (22%). Thirty per cent had a comorbid cannabis disorder and 16% a comorbid stimulant disorder. One in six (16%) had prior admissions for mental health or substance-related problems but without a psychosis diagnosis.
Table 1 Characteristics of study group and readmission rate within 2 years of first admission with a diagnosis of psychosis

| n (%) | % readmitted (95% CI) |
|
|---|---|---|
| Total | 7269 (100) | 37 (37-37)Footnote e |
| Gender | ||
| Male | 4810 (66) | 39 (38-40) |
| Female | 2459 (34) | 34 (32-35) |
| Age group, years | ||
| 15-19 | 1736 (24) | 42 (40-45) |
| 20-24 | 2718 (37) | 37 (36-39) |
| 25-29 | 2815 (39) | 34 (32-36) |
| Diagnosis | ||
| SchizophreniaFootnote a | 2602 (36) | 42 (40-44) |
| Schizoaffective | 343 (5) | 41 (35-48) |
| Affective psychosisFootnote b | 939 (13) | 28 (25-31) |
| Brief psychosis | 919 (13) | 38 (35-42) |
| Drug-induced psychosis | 1570 (22) | 36 (33-38) |
| Other psychosisFootnote c | 896 (12) | 36 (33-40) |
| Baseline drug diagnoses | ||
| Cannabis | 2197 (30) | 41 (38-43) |
| Stimulants | 1162 (16) | 38 (35-42) |
| Prior care | ||
| Prior admissionsFootnote d | 1177 (16) | 42 (38-45) |
| Prior cannabis | 645 (9) | 41 (36-45) |
| Prior stimulants | 372 (5) | 46 (39-53) |
| Person | ||
| Migrant | 1332 (18) | 35 (32-38) |
| Rural residence | 3013 (41) | 39 (37-41) |
| Most disadvantaged | 3183 (44) | 39 (38-41) |
a. Includes delusional disorder.
b. Mania or depression where psychosis specified.
c. Includes other non-organic psychosis (ICD-10 code F28) and psychosis not otherwise specified (F29).
d. Prior admissions for mental healthcare but no prior psychosis diagnosis.
e. Readmission rate 37.35% (95% CI 37.33-37.38).
Table 2 Cox regression analyses of readmission within 2 years of first admission with psychosis (persons aged 15-29, n = 7269)

| Univariate | MultivariateFootnote f | |||||
|---|---|---|---|---|---|---|
| n | HR | 95% CI | P | HR | 95% CI | |
| Male | 4810 | 1.21 | 1.11-1.31 | <0.001 | 1.13 | 1.04-1.24 |
| Age group, years | ||||||
| 15-19Footnote a | 1736 | 1.00 | - | <0.001 | 1.00 | - |
| 20-24 | 2718 | 0.85 | 0.77-0.93 | 0.80 | 0.73-0.89 | |
| 25-29 | 2815 | 0.76 | 0.69-0.83 | 0.72 | 0.65-0.80 | |
| Diagnosis | ||||||
| SchizophreniaFootnote a , Footnote b | 2602 | 1.00 | - | <0.001 | 1.00 | - |
| Schizoaffective | 343 | 0.98 | 0.82-1.17 | 1.01 | 0.84-1.21 | |
| Affective psychosisFootnote c | 939 | 0.61 | 0.53-0.69 | 0.56 | 0.48-0.64 | |
| Brief psychosis | 919 | 0.91 | 0.80-1.02 | 0.80 | 0.73-0.89 | |
| Drug-induced psychosis | 1570 | 0.83 | 0.75-0.92 | 1.13 | 1.04-1.24 | |
| Other psychosisFootnote d | 896 | 0.85 | 0.75-0.97 | 0.81 | 0.71-0.92 | |
| Baseline drug diagnoses | ||||||
| Cannabis | 2197 | 1.15 | 1.06-1.25 | <0.001 | 1.06 | 0.97-1.16 |
| Stimulants | 1162 | 1.05 | 0.95-1.16 | NSFootnote e | 1.02 | 0.90-1.14 |
| Prior care | ||||||
| Prior admissions | 1177 | 1.18 | 1.07-1.30 | <0.001 | 1.22 | 1.08-1.37 |
| Prior cannabis | 645 | 1.11 | 0.97-1.26 | NS | 0.97 | 0.82-1.14 |
| Prior stimulants | 372 | 1.30 | 1.11-1.51 | NS | 1.36 | 1.12-1.66 |
| Person | ||||||
| Migrant | 1332 | 1.11 | 1.00-1.22 | NS | 1.04 | 0.93-1.16 |
| Rural residence | 3013 | 1.10 | 1.02-1.19 | NS | 1.03 | 0.86-1.24 |
| Most disadvantaged | 3183 | 1.13 | 1.04-1.22 | <0.001 | 1.07 | 0.95-1.21 |
HR, hazard ratio; NS, not significant.
a. Reference group.
b. Includes delusional disorder.
c. Mania or depression where psychosis specified.
d. Includes other non-organic psychosis (ICD-10 code F28) and psychosis not otherwise specified (F29).
e. Not significant (P>0.05).
f. P for overall model <0.001.
Thirty-seven per cent of persons were readmitted with psychosis within 2 years. The risk of readmission was highest immediately following the index admission; 17% of participants were readmitted within 90 days (representing 45% of those who were readmitted).
Table 2 shows the results of univariate and multivariate Cox regression. In univariate comparisons, readmission at 2 years was significantly more likely in males (hazard ratio (HR) 1.21, 95% CI 1.11-1.31) and in younger individuals. The highest rate of readmission (42%) was for people with an index diagnosis of schizophrenia. By comparison with schizophrenia, the risk of readmission was reduced in those with affective psychosis (HR = 0.61, 95% CI 0.53-0.69), drug-induced psychosis (HR = 0.83, 95% CI 0.75-0.92) and atypical psychosis (HR = 0.85 95% CI 0.75-0.97). Cannabis disorders at index admission were associated with a greater risk of readmission (HR = 1.15, 95% CI 1.06-1.25), but cannabis disorders prior to the index admission were not (HR = 1.11, 95% CI 0.97-1.26). This pattern was reversed for stimulants: baseline stimulant disorders were unrelated to risk of readmission, but people with an admission with stimulant disorders prior to their index admission had a higher risk of readmission (HR = 1.30, 95% CI 1.11-1.51).
The results of multivariate analysis differed slightly: after controlling for other variables, affective, brief and atypical psychoses were associated with lower risk of readmission than schizophrenia, but drug-induced psychosis was associated with a higher risk (HR = 1.13, 95% CI 1.04-1.24). Baseline cannabis disorder was no longer associated with readmission. Findings regarding stimulants were unchanged in the multivariate analysis: prior stimulant disorders predicted readmission (HR = 1.36, 95% CI 1.12-1.66) but a baseline stimulant diagnosis did not. There was no relationship between readmission and migrant status, rural location or residing in more disadvantaged localities.
Examining multivariate outliers, 80 participants (1.1%) had deviance residuals greater than 2.5 standard deviations (s.d.), but none greater than s.d = 3.0. These individuals did not differ significantly from other participants on age, gender, diagnosis group, rate of substance use or year of admission, but they were more likely to have had their index admission outside a specialist mental health unit. Index admission occurred outside a specialised mental health unit for 1068 persons (15% of the study group). These admissions were more common in rural hospitals, and were not excluded from the study in order to avoid systematic underrepresentation of rural residents. Sensitivity analysis was conducted by refitting the multivariate Cox regression model after removing this group; the risk of readmission for brief psychosis was slightly reduced, and now differed significantly from that for schizophrenia (HR = 0.84, 95% CI 0.74-0.96) in the revised model. The model was otherwise unchanged.
Sensitivity analysis was conducted on the effects of different methods for dealing with tied observations within a Cox regression. There was no significant difference between exact and approximate methods; the results presented used the Efron approximation.
A total of 31% of participants had no further contact with NSW community mental health or in-patient services in the 2 years after their index admission, and therefore had no diagnostic or HoNOS information for ongoing care in the study period. People with no ongoing service contact were more likely to be younger, to have an index diagnosis of brief (odds ratio (OR) 1.39, 95% CI 1.01-1.91), drug-induced (OR = 1.27, 95% CI 1.02-1.58) or atypical/unspecified psychosis (OR = 1.49, 95% CI 1.07-2.07), and to have had prior admissions with cannabis (OR = 1.47, 95% CI 1.07-1.27) or stimulant (OR = 1.50, 95% CI 1.01-1.21) diagnoses. They were less likely to have baseline cannabis diagnoses (OR = 0.43, 95% CI 0.36-0.52) but did not differ from people with ongoing contact on gender, baseline stimulant use, urban/rural location or migration status.
Excluding people with no further contact with NSW health services, the proxy measure of ongoing drug problems was available for 69% of the study group (n = 4993). Their 2-year readmission rate (54%) was higher than for the study group as a whole, since the readmission rate for those with no further contact was zero. Those with ongoing contact were divided into three groups: no drug problem (n = 2209), drug problem ceased (n = 866) and drug problem ongoing (n = 1918). Figure 2 shows the cumulative readmission curve for these groups. The readmission rate was highest for the drug-problem-ongoing group (66%, 95% CI 63-69), intermediate for those with no drug problem (50%, 95% CI 47-52) and lowest for the drug-problem-ceased group (40%, 95% CI 37-44). This difference was significant (Wilcoxon-Breslow test, χ2 = 147.92, P<0.0001). The proportional hazards assumption for Cox regression was not met: examination of the survival curves (Fig. 2) suggests that the reason for this was that the drug-problem-ceased group had a lower rate of early readmission, but not of later readmission when compared with the no-drug-problem group. Sensitivity analysis, where people with an index diagnosis of drug-induced psychosis were excluded, did not change these results; readmission rates after exclusion of drug-induced psychosis were: drug problem ongoing, 67% (95% CI 63-71); no drug problem, 50% (95% CI 48-52); and drug problem ceased, 43% (95% CI 38-48).
Discussion
It is clinically important to identify factors which predict outcome in first-episode psychosis, and especially to identify prognostic factors which may be influenced by intervention. Some studies have found that substance use at psychosis onset predicts poorer outcomes. Reference Malla, Norman, Bechard-Evans, Schmitz, Manchanda and Cassidy15,Reference Addington, Beck, Wang, Adams, Pryce and Zhu16 We have used health-system data for a population of 7.3 million persons to examine the risk of readmission in young people following a first admission for psychosis. Neither cannabis nor stimulant diagnoses at baseline predicted readmission after controlling for age, gender and diagnostic subtype. Our findings are consistent with those suggesting that ongoing substance use is the more important issue. Reference Bertelsen, Jeppesen, Petersen, Thorup, Ohlenschlaeger and Le Quach3,Reference Wade, Harrigan, Edwards, Burgess, Whelan and McGorry4,Reference González-Pinto, Alberich, Barbeito, Gutierrez, Vega and Ibáñez17
Cannabis disorders and readmission
We found univariate associations between baseline cannabis and outcome; however these were no longer significant after controlling for age, gender and diagnostic subtype. Our findings are consistent with studies reporting that baseline cannabis use did not predict poor outcome. Reference Gonzalez-Pinto, Alberich, Barbeito, Gutierrez, Vega and Ibanez2,Reference Addington and Addington18 Some of the apparent association between baseline cannabis use and adverse outcome may be due to confounding of cannabis disorders with other factors which predict readmission, namely, being younger, male and having a primary diagnosis of schizophrenia. Baseline use of cannabis or other drugs may also be a predictor of ongoing drug use.
Stimulant disorders and readmission
Stimulant disorders at baseline were not associated with readmission, but hospital admissions with stimulant disorders prior to the index admission were. The finding is consistent with evidence that the risk of developing drug-related psychosis after prolonged drug use is greater for stimulants than for cannabis, Reference Degenhardt, Roxburgh and McKetin19 and with sensitisation models of the interaction between stimulant use and psychosis. Reference Curran, Byrappa and Mcbride20,Reference Hermens, Lubman, Ward, Naismith and Hickie21 Prior stimulant-related admissions are likely to be indicators of severe or enduring stimulant use, since most people with stimulant misuse or dependence are not admitted to hospital. Severe stimulant disorders may also be associated with misuse of a wider range of substances, including heavier or more sustained cannabis use. However, the same association was not found for prior cannabis use disorders.
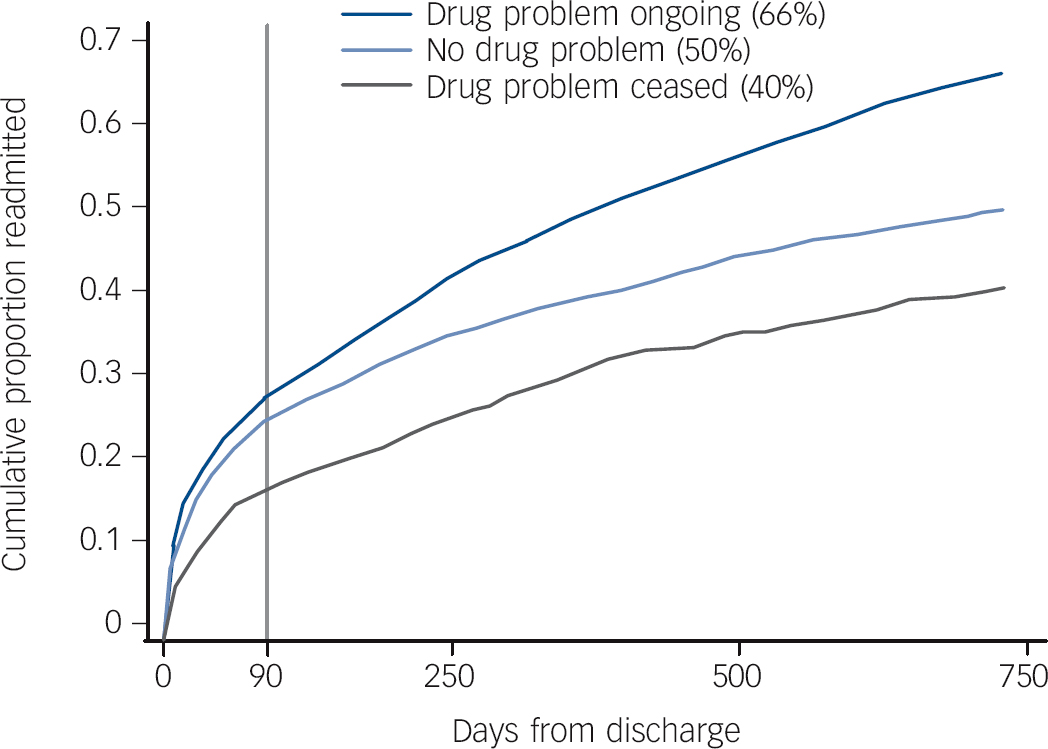
Fig. 2 Readmission within 2 years of first admission for psychosis, by pattern of ongoing problem drug use.
Results for 4993 persons (69% of total sample) for whom a proxy measure of ongoing drug problems was available. Two-year readmission rate for total sample: 37%.
Ongoing drug use
We found that people with ongoing problem drug use had a rate of readmission nearly a third higher than people with no drug use. An association between ongoing drug use and poor outcome is not surprising, however our findings help to quantify the scale of this effect in a representative population-based sample, and underline the significant personal and health system impacts of ongoing drug use.
Conversely, we found that the best outcome (as measured by hospital readmission) occurred in people with baseline substance diagnoses but no ongoing substance use problems. Several studies have found that young people with psychosis who cease substance use have better outcomes than those who have never used substances. Reference Strakowski, DelBello, Fleck, Adler, Anthenelli and Keck22-Reference Lambert, Conus, Lubman, Wade, Yuen and Moritz24 A recent meta-analysis of this issue concluded that further and larger studies were needed. Reference Gupta, Mullin, Nielssen, Harris and Large25 Our findings add further evidence on this issue.
An association between substance use and positive outcome in psychosis may seem counterintuitive, since substance use in people with psychosis is associated with negative prognostic factors including younger age, male gender and social disadvantage. However, there is increasing evidence that comorbid drug use in psychosis is also associated with better neurocognitive performance, fewer negative symptoms, fewer neurological soft signs and more positive symptoms. Reference Rabin, Zakzanis and George26,Reference Yucel, Bora, Lubman, Solowij, Brewer and Cotton27
Three explanations have been proposed for these findings. First, cannabis may have direct neuroprotective effects. Reference Yucel, Bora, Lubman, Solowij, Brewer and Cotton27 Second, Meuser et al Reference Mueser, Drake and Wallach28 have proposed that this effect is mediated through social competence, whereby more ‘socially oriented patients with serious mental illness are more likely to come into contact with drugs and subsequently develop substance use disorder’ (p. 726). Third, these findings may reflect varying degrees of personal vulnerability: psychosis in the absence of substance use is likely to reflect greater genetic or developmental diathesis in the person affected, whereas cannabis or other drugs may precipitate psychosis in individuals with less intrinsic vulnerability. Reference Schnell, Koethe, Daumann and Gouzoulis-Mayfrank29,Reference Loberg and Hugdahl30 Our findings cannot distinguish between greater social competence and lesser personal vulnerability as explanations for positive outcome in former drug users with psychosis, and further research on this question is needed. The association between ongoing substance use and worse outcome is inconsistent with cannabis having a neuroprotective effect in psychosis.
Regardless of the mechanism, our findings underline an important and hopeful clinical message. Young people with first-episode psychosis and comorbid substance disorder may have the best outcomes, provided that substance disorder is properly managed.
Other findings
After controlling for other variables, the risk of readmission for people with an index diagnosis of drug-induced psychosis was higher than for those with an index diagnosis of schizophrenia. This is consistent with studies questioning the predictive validity of drug-induced psychosis diagnoses. Reference Mathias, Lubman and Hides31,Reference Crebbin, Mitford, Paxton and Turkington32 In a study of persons with diagnoses of cannabis-induced psychosis, nearly half were subsequently diagnosed with schizophrenia and 77% had further psychotic episodes. Reference Arendt, Rosenberg, Foldager, Perto and Munk-J⊘rgensen33
The association between ongoing problem drug use and readmission was not constant over time; cessation of problem drug use appeared to be associated with a reduced risk of early readmission (within 90 days of discharge from index admission). Early and late relapse or readmission may be influenced by different processes and risk factors. Reference Durbin, Lin, Layne and Teed34 This issue warrants further study.
Limitations
The scale and population coverage of administrative data-sets can complement clinical studies by allowing an examination of issues such as stimulant misuse which may be otherwise confounded by other clinical or personal variables in smaller clinical samples. However, routinely collected administrative data also have a number of limitations.
First, we have not captured all incident cases of psychosis in NSW because we have used hospitalisation data to define incidence. More than 80% of people seen by specialised early psychosis services are admitted early in their illness. Reference Sipos, Harrison, Gunnell, Amin and Singh35-Reference Wade, Harrigan, Harris, Edwards and McGorry37 Those not admitted have longer duration of psychosis, less social disadvantage and greater likelihood of manic psychosis, Reference Sipos, Harrison, Gunnell, Amin and Singh35,Reference Wade, Harrigan, Harris, Edwards and McGorry37,Reference Compton, Gordon, Goulding, Esterberg, Carter and Leiner38 but do not differ in their prevalence of positive symptoms or the likelihood of problem substance use. Reference Wade, Harrigan, Harris, Edwards and McGorry37 Our findings underestimate the total number of young people with psychosis, and our sample omitted some young people with better social support and/or a less acute onset.
Second, we do not have follow-up information on all study participants. Thirty-one per cent of participants had neither a readmission to hospital nor a contact with NSW community mental health services during the follow-up period. These individuals were younger, more likely to have index diagnoses of brief, atypical and drug-induced psychoses and to have prior (but not baseline) cannabis and stimulant diagnoses. In the Australian health system, state-operated mental health services care for most persons with psychosis. Loss of contact with specialised services may be a sign of resolution of symptoms and recovery from illness. Reference Warner39,Reference Emsley, Chiliza, Asmal and Lehloenya40 However, people losing contact with specialised services may have equivalent rates of positive symptoms and substance use to those remaining in care. Reference Stowkowy, Addington, Liu, Hollowell and Addington41 We cannot know whether those with no follow-up may have had ongoing substance use or psychosis for which they did not seek care, or were managed without contact with NSW in-patient or community mental health services.
Third, we used hospital readmission as a measure of relapse. Lack of readmission does not equate with symptomatic or functional recovery, and many significant relapses of psychoses may be managed without readmission. We did not have a measure of the severity of psychotic symptoms or of substance use. However, hospital readmission remains the most widely used indicator of relapse in young people with psychosis, Reference Gleeson, Alvarez-Jimenez, Cotton, Parker and Hetrick9 and a second hospital admission may be a very significant event for a young person and for their family.
Fourth, we have examined admissions prior to the index psychosis admission with stimulant or cannabis diagnoses. Most people with substance use disorders (misuse or dependence) are not admitted to hospital with those disorders. Therefore this measure of prior substance disorder is likely to be of high specificity but low sensitivity.
Finally, our proxy measure of ongoing drug use was imprecise. It combined data from in-patient and community diagnoses with a clinician rating of problem substance use derived from the HoNOS. The HoNOS is not a diagnostic instrument and does not distinguish the type of drug used.
Clinical implications
Cannabis or stimulant disorders at first hospital admission with psychosis may not be negative prognostic signs. Young people with substance comorbidities may have both the best and worst of outcomes, depending on whether problematic substance use is discontinued. It is critical to screen and offer intervention for drug use in early psychoses. Admissions with stimulant disorder diagnoses prior to the first psychosis admission were associated with worse outcome. This suggests that it is important not only to identify current substance use at first admission with psychosis but also to obtain a detailed history of the type, severity and duration of past substance use.







eLetters
No eLetters have been published for this article.