Many children with complex right ventricle outflow tract anomalies such as Tetralogy of Fallot, common arterial trunk, and pulmonary atresia with ventricular septal defect require repeated heart surgeries early in life, but also later throughout their lifetime, thereby emphasising the importance of careful life-long follow-up. Reference Ho, Schamberger, Hurwitz, Johnson, Sterett and Ebentoth1 The need for repeated heart surgeries during childhood is recognised as a heavy burden on the child. Reference Andresen, Andersen, Lindberg and Døhlen2 Optimising the time point for re-intervention is important, since delaying re-intervention for these children can lead to complications such as ventricular arrhythmias, heart failure, and death. Reference Gatzoulis, Balaji and Webber3 To this purpose, thorough pre-operative assessment (henceforth named as assessment) including clinical examination, echocardiography, MRI, and exercise test need to be performed whenever the indication for reoperation is suspected. It is likely to believe that children who are going through this kind of assessment that may lead to heart surgery need extra support. According to previous research, children with complex heart disease fear for the possibility of surgery Reference Chong, Fitzgerald and Craig4 and the thought of future repeated heart surgery is associated with anxiety. Reference Andresen, Andersen, Lindberg and Døhlen2 This might have an impact on children’s everyday life and in research nowadays involving children with CHD, the focus has changed from survival to how these children experience their everyday life. Reference Svensson, Walhberg and Gislason5 Earlier studies have shown that they experience physical activities limitation Reference Elissa, Sparud-Lundin, Axelsson, Khatib and Bratt6,Reference Shearer, Rempel, Norris and Magill-Evans7 and feelings of isolation, Reference Lee and Kim8 but no study has yet studied how children with right ventricle outflow tract anomalies experience their everyday life. To be able to provide support, studies are needed to explore how these children experience the period from assessment to decision, as well as the months thereafter. Therefore, the aim of this study was to explore how children diagnosed with complex right ventricle outflow tract anomalies experience their heart disease and their everyday life during the assessment and after the decision on whether to perform a new cardiac surgery.
Materials and methods
Study design
A longitudinal qualitative inductive study design was used since it is suited to understanding subjective experiences over time. For gathering children’s experiences, interviewing is a recommended method. Reference Patton9 In this study, children with right ventricle outflow tract anomalies were interviewed at three chosen time points during and after the assessment stages, in total 27 interviews (Fig 1).
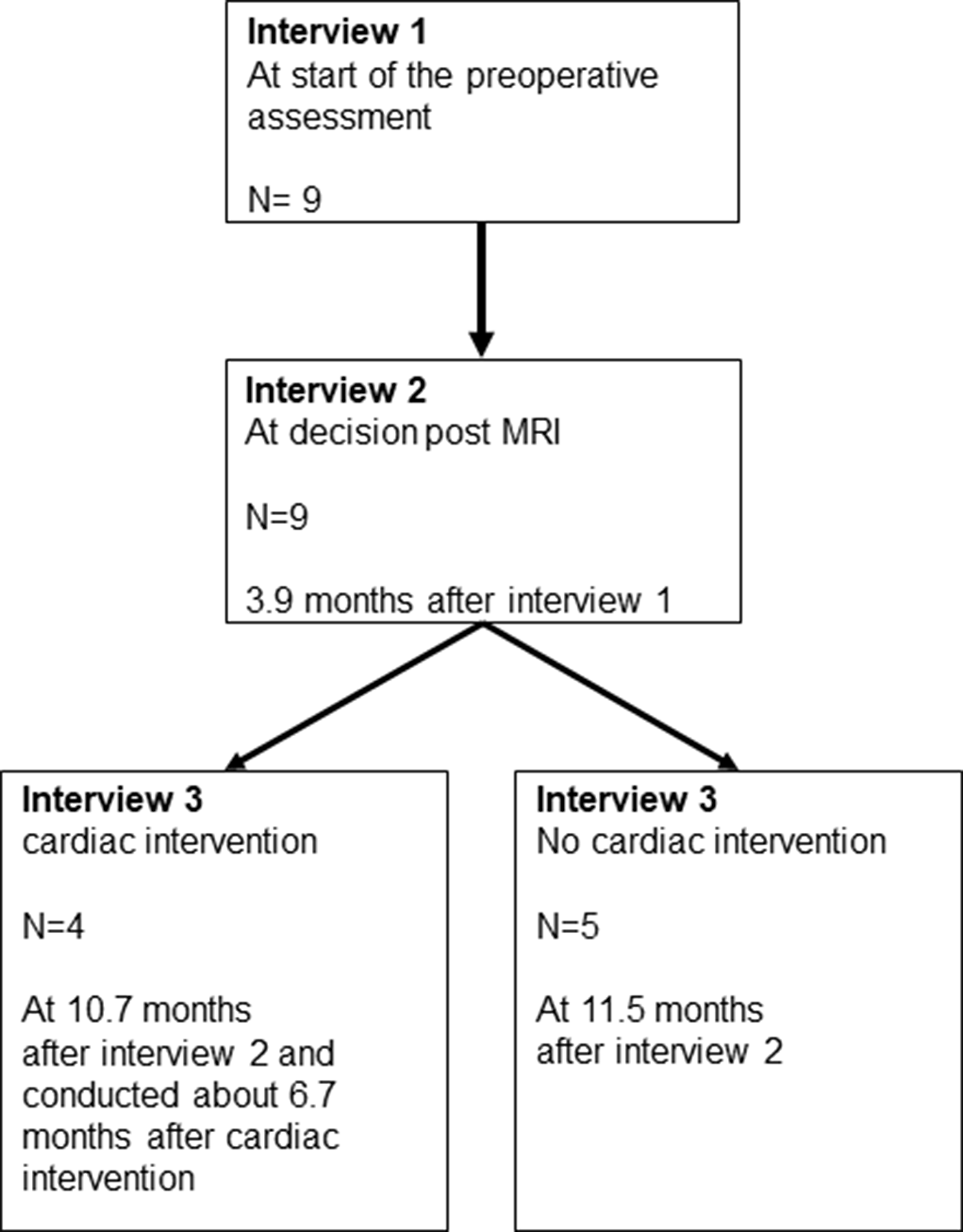
Figure 1. Mean Time points for the three interviews, the assessments stages and the number of children interviewed.
Participants
During the period 2014–2016, nine children (six girls) with complex right ventricle outflow tract anomalies aged between 9 and 17 years (mean age 13.8) were included in the study (Table 1). The inclusion criteria were age 9–18 years, diagnosis of complex right ventricle outflow tract anomalies, previous surgical repair, and a completed MRI. The exclusion criteria were children unable to speak and understand Swedish or unable to participate in an interview situation due to cognitive impairment. Totally 15 children and their guardians were invited to participate, where six of the guardian’s declined participation for themselves and the child.
Table 1. Characteristics of the participants, previous surgical repair with transannular patch or conduit, and outcome of the latest MRI
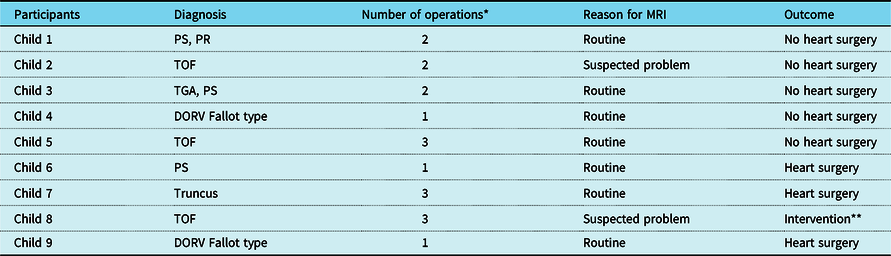
DORV = double outlet right ventricle, PR = pulmonary regurgitation, PS = pulmonary stenosis, TGA = transposition of the great arteries, TOF = tetralogy of Fallot.
* Number of operations before the pre-operative assessment.
** Implantation of a percutaneous stent valve via heart catheterisation.
Data collection
After receiving oral and written age-appropriate information about the study, children and their guardians at two university hospitals in Sweden were invited to participate in the study by two nurses, working at the clinics. After obtaining written informed consent from the guardians and from children over 15 years of age and consent from children younger than 15 years of age, the first author (BS) contacted them to provide further information. Of the interviews, 24 were performed at the child’s home, two in the hospital, and one by telephone. Children (with help from their guardians) decided the time and place for the interview. All children were given age-appropriate information explaining that their participation was voluntary and could be withdrawn at any time without giving a reason. All interviews were conducted individually, except for one first interview, when the child wanted to have his mother present. The children and their guardians received the contact information of a psychologist in case they felt a need to talk to someone further after the interview.
Interview
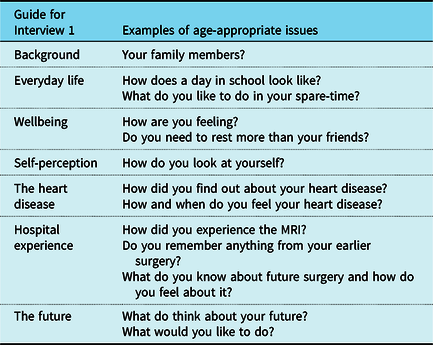
An interview guide was developed, based on a literature review focusing on the research aim. The main topics included in the interview concerned children’s everyday life during and after the assessment, their heart disease, earlier and future heart surgery, and their future. Open-ended questions were used, and follow-up questions were asked, such as “What did you feel?” and “Can you describe it?” These follow-up questions were asked whenever the narrative needed clarification. The first interview for all children started with a presentation of the interviewer, the study, and the structure of the three planned interviews. This was followed by general questions, for instance “How does a day in school look like” and “ What do you like to do in your spare-time” (Table 2). The interviewer began the second interview with “Last time I was here…and now you have got a decision,” and the third interview began, for children with no need for heart surgery, with “A year has passed since last time I was here” and, for children who had had heart surgery, “Since the last interview, you have been operated.” The children were given appropriate information clarifying that there were no right or wrong answers, and they decided whether they wanted to answer each question or not. Two questions were posed at the end of each interview: “Is there something you want to tell me that I didn’t ask you?” and “How are you feeling now?” All interviews were conducted by the first author and digitally recorded with the approval of the children. The interviews lasted from 47 to 129 minutes per child (mean 96 minutes).
Table 2. Interview guide for the first interview
Data analysis
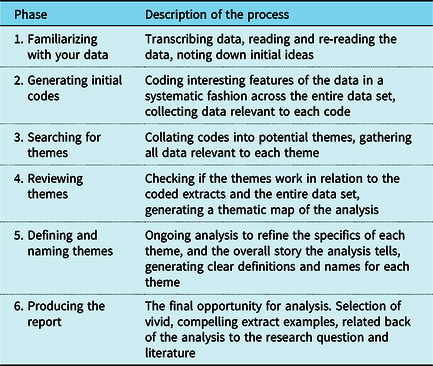
A thematic analysis approach was used to analyse the interview data and the six phases of thematic analysis by Braun and Clarke guided the analysis (Table 3). Thematic analysis is a method for identifying, analysing, and reporting patterns within the data. Reference Braun and Clarke10 An inductive approach was used at a semantic level for both a descriptive and an interpretative perspective. The first author transcribed all the recorded interviews and when all data was generated, the analysis took place for one child at a time, including all the three interviews with the child. The first and the last author (MB) coded independently, and then assessed the results together while the third author (AW) contributed to the interpretation of the themes and subthemes. After that the whole research group discussed and approved the final analysis.
Table 3. Phases of the thematic analysis as described by Braun and Clarke (2006)
Rigor
In qualitative research, trustworthiness can be demonstrated through the credibility, dependability, and confirmability. Reference Lincoln and Guba11 To ensure dependability, the first author conducted all the interviews after one pilot interview had been done. The fact that the first and last author coded independently and that the results included quotations from the interviews strengthens the credibility of the study. All children’s experiences are described in the findings and all but one is quoted 1–3 times. Confirmability was enhanced by the first author writing a reflexivity journal for personal feelings, insights, beliefs, and observations used for highlighting pre-conceptions before and during the analysis.
Results
The data analysis yielded three themes and eight subthemes. The children’s experiences of the heart disease in their everyday life are described in the theme Me and my heart disease. The theme Being me concerns children’s sense of self. Their experiences during the assessment and its consequences are described in the theme Being placed in someone else’s hands. The themes and subthemes are presented in Figure 2.
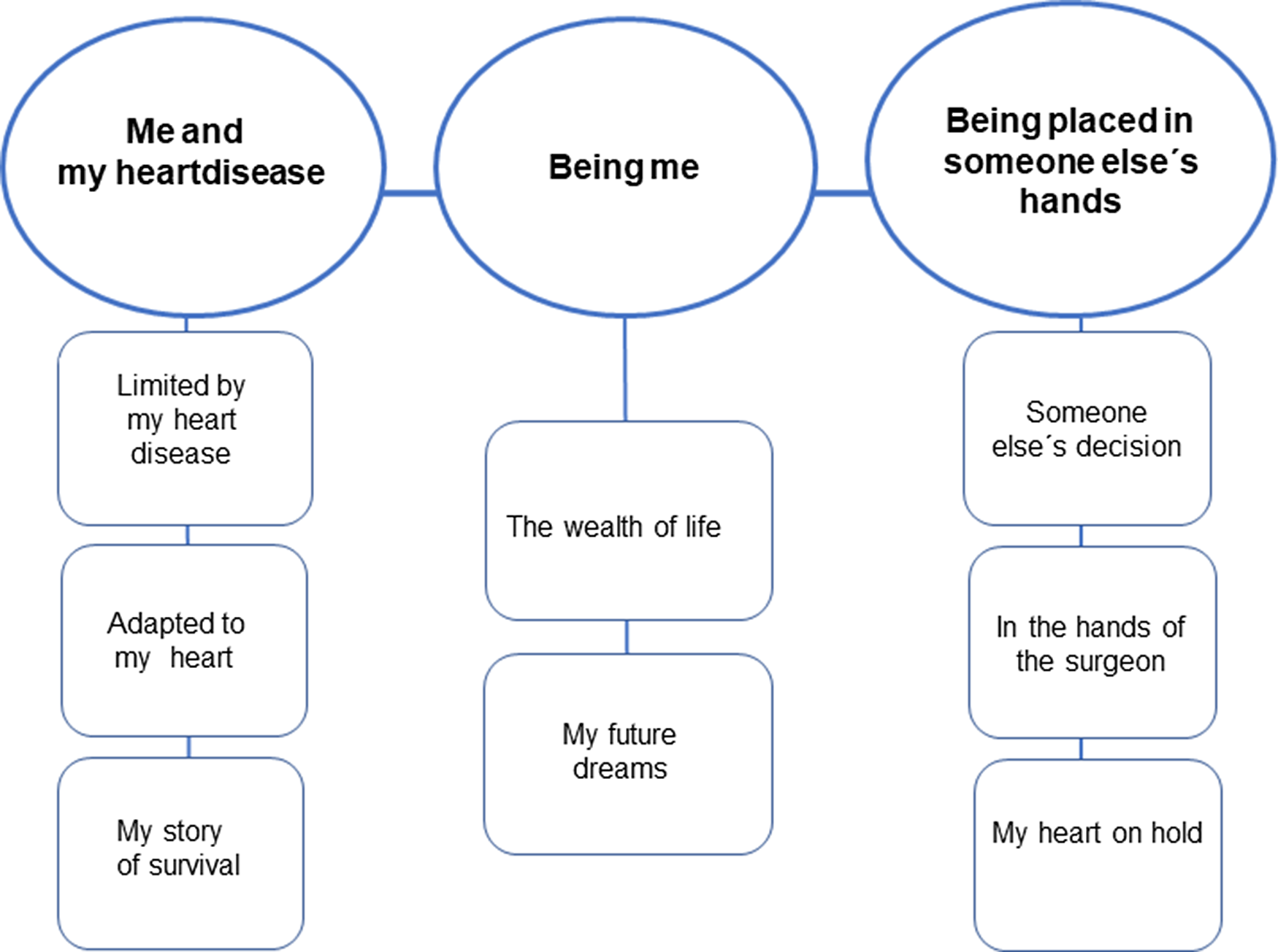
Figure 2. Thematic map over the three themes with the eight subthemes.
Me and my heart disease
The children’s experiences of their heart disease in everyday life and how these experiences affected their ability to adapt are described in the subthemes Limited by my heart disease and Adapted to my heart. All the children had experiences of earlier heart surgery and of having a scar, which is described in the subtheme My story of survival.
Limited by my heart disease
Almost all the children had symptoms and experienced varying degrees of tiredness that forced them to take a rest every day, sometimes for the whole day. Physical activity reduced their energy especially, and the difference between their tiredness and lack of energy was expressed as “I suppose I get more tired and then if I exert myself, I get out of breath much faster, yes…. if I get out of breath it will pass but if I get tired, I am tired the whole day” (Girl, 16 yrs.). It was unusual that children felt chest pain but some of them reported that their heart was beating hard and fast during certain activities and that they sometimes felt that it would stop. Experiencing limitations was common among the children, for example, being unable to play football although it was the child’s greatest wish.
Adapted to my heart
All the children had become accustomed to their heart disease, but still some of them speculated about who they would be without it. Sometimes they had not noticed their symptoms, including feeling breathless and needing rest, until after the surgery, when they could make a comparison. They also found their tiredness hard to interpret: was it the heart disease, or adolescence, or were they just having a bad day? The children sometimes talked about being used to the limitations resulting from their heart disease so they did not experience them as limitations. “It has always been there without affecting me, except I can’t exert myself too much” (Girl,17 yrs.). The most common adaptation they learned was to rest and take short breaks, but also to manage their strength so it would last longer. Others had developed skills for showing their lack of energy without expressing it in words.
My story of survival
All the children had gone through at least one heart surgery earlier in life, but these memories were not accessible for most of the children. “I don’t remember the operation itself or afterwards or all that. I only remember that I was well taken care of and so on. But maybe it’s good that I don’t remember everything” (Girl, 17 yrs.). They all had experiences related to their scar, which was seen as a reminder of their survival. “But I think it is nice…like a story…something to be proud of…it’s thanks to that that I am alive…otherwise I wouldn’t be alive. So it’s something to be proud of because not everybody survives such operations…that’s how it is” (Girl, 17 yrs.). From that perspective, the scar became a reminder of strength and power, but it could also be a reminder of exclusion and not being like others, or just a minor difference. “I am like anyone else with a scar”(Girl, 11 yrs.).
Being me
The children’s narratives revealed a sense of self in which the heart disease did not feature, described in the subthemes The wealth of life and My future dreams.
The wealth of life
The children’s sense of self was described in a positive way with words like happy, social, kind, independent, and open-minded. They described having a strong social network, both at home and in school. Almost all also expressed a steady well-being that was naturally affected by the ups and downs of life, such as success in school and getting new friends or periods of lacking energy in the winter darkness. The most important aspects of their lives were their family and friends and having fun. “Doing what you want, in other words, avoiding what you don’t want” (Boy, 17 yrs.). Their spare time was filled with activities such as football, dance, biking, playing, reading, singing, listening to music, or just relaxing. All the children mentioned something or somebody that made them happy.
My future dreams
All the children easily shared their thoughts and feelings about the future and described different future dreams, which were either imaginative, “I want to live in Monaco …there are a lot of car races and suchlike, so that’s why…also because some celebrities live there” (Boy, 13 yrs.), or more realistic, such as their career choices, including carpenter, doctor, nurse, professional singer, confectioner, and personal assistant. They wanted to travel to foreign places or work abroad, but some children also expressed a wish to stay close to their childhood home and city. They talked about settling down with a partner, with or without starting a family. Their stories sparkled with hope that the future was theirs for the taking.
Being placed in someone else’s hands
Experiences of going through an assessment and receiving a decision about heart surgery are described in the subtheme Someone else’s decision. The experiences of the heart surgery are described in the subtheme In the hands of the surgeon, and the subtheme My heart on hold describes the experiences of those who did not need heart surgery.
Someone else’s decision
As soon as the assessment started, the children feared having to undergo heart surgery, but their everyday life was not markedly affected at first. To some extent, the children hoped for a decision against heart surgery, but they all knew that it would be needed someday. Irrespective of the outcome, they welcomed the assessment, which they saw as a safety net. All the children received the decision via their guardians and, where there was no need for heart surgery, the children’s reactions were positive and life went on as before. Nevertheless, it only meant a temporary reprieve, since they knew that surgery would be needed, but they did not know when. The decision could give them some relief but not an assurance. “It is very good that I do not need surgery but at the same time, I myself feel that it’s heading that way, I feel worse than maybe a year ago” (Girl, 17 yrs.). When the assessment resulted in a decision that heart surgery or an intervention would be needed, the children’s reactions varied. One was relieved that the decision was for an intervention rather than heart surgery, while another felt that her everyday life was turned upside-down and began to prepare for her forthcoming funeral. Thus, their feelings ranged from joy, expectancy, and being offered their lives back, to one child suffering pronounced loneliness, exacerbated by the fact that the decision to perform heart surgery did not correspond to how she felt. “They see something that I do not feel, with the heart that is, that needs to be repaired” (Girl, 17 yrs.).
In the hands of the surgeon
Some children were dissatisfied with the health care professional’s communication. One child had earlier got the information that the new valve would be a mechanical valve, but the day before surgery the surgeon informed her that a biological valve would be the best. This rapid change was extremely distressing as she was reluctant to receive a biological organ. After surgery and before going home, she realised what valve they had actually implanted. “Then he said biological valve and everything burst for me and I got so miserable and I thought that I would have that person’s characteristics…I got so afraid…I know I looked at myself in a mirror afterwards and thought, I still have brown eyes…I don’t know but I got some sort of strong anxiety and everything became chaos for me” (Girl, 17 yrs.) Despite setbacks during the surgery and the hospital stay, the children didn’t give up. “I don’t know much….it is sad that it has happened…but I can’t do anything about that…battle on…yes” (Boy, 13 yrs.).
My heart on hold
The children’s experiences varied when heart surgery was not needed. Most of the time they could suppress or even forgot their worries, but on bad days, such as when they felt sad, these thoughts came back. They were so used to the prospect of heart surgery that they found it hard to say how their lives were affected, but nevertheless, the thought of future surgery was worrying. Their worries ranged from everyday life concerns, such as missed schoolwork, to matters of life and death. “Like when they are going to operate then I will be very nervous [whispers nervously] …that…I might die…like, that nervous” (Girl, 9 yrs.). One child could talk about everything, but when it came to surgery, his only response was tears. Some of the children wondered when to expect the future surgery. “…mm, the only thing I wonder about my heart disease is… is when…because I would like to know when I will be operated…that’s the only thing I want to know…but I don’t know…I mean, I would like to know when, but I don’t know if it would have been better to know” (Girl, 11 yrs.).
Discussion
To our knowledge, this is the first study focusing on the everyday life experience of children with complex right ventricle outflow tract anomalies at different assessment stages and months after the medical decision was taken. Although this thorough assessment is a milestone in the follow-up, these children did not see it as a cause for concern, at least not until the decision was taken. Importantly almost all had symptoms from their heart disease but they did not always pay attention to them. They had developed strategies to manage their heart disease in their everyday life, sometimes so well that their everyday life showed no trace of the heart disease. This could be seen as an adaptation to the disease.
According to Marino et al., the definition of adaptive behavior is “an age-related construct that reflects learned skills in conceptual, practical and social arenas that are necessary for function in everyday life”. Reference Marino, Lipkin and Newburger12 There might be a risk that children with CHD have difficulties adapting in their everyday life due to their underlying heart condition. Reference Marino, Lipkin and Newburger12 In our study, we could see traces of such difficulties, for instance, when the children limited themselves in their physical activity. In all the narratives, we also saw traces of adaptive behavior in their everyday life concerning their heart disease, the assessment, and future surgeries. Even though previous research has shown that future surgery is a burden for children with CHD, Reference Andresen, Andersen, Lindberg and Døhlen2,Reference Lee and Kim8 the children in our study showed that it also provides them with an opportunity to adapt to this situation, as well as to the heart disease itself.
The mechanism of adaptation could partly explain why children were not concerned in the beginning of the assessment. In the study by Shearer et al., adolescents with CHD expressed feelings of comfort while being taken care of by healthcare professionals. Reference Elissa, Sparud-Lundin, Axelsson, Khatib and Bratt6 The children in our study likewise experienced feelings of being taken care of or being placed in someone else’s hands when they went through the assessment. However, when informed about the medical decision, they demonstrated clear feelings of either safety or fear. In a study by Gutman et al, children with chronic kidney disease expressed wanting to be involved in treatment decision-making. Reference Gutman, Hanson and Bernays13 Based on our findings, we speculate that children with CHD would also benefit from being more involved in the treatment decision-making which could improve their feeling of safety.
The child’s experiences and own perspectives can be better understood and integrated in the assessment by inviting the child to participate at an early age and by asking explorative questions regarding symptoms and their change over time. This could be achieved by using the child-centered approach. According to Söderbäck et al, a child-centered approach “includes both the adult’s child perspective concerning the children’s best interests in terms of care and the child’s perspective with respect to his or her preferences.” Reference Söderbäck, Coyne and Harder14 Inviting the children to participate from the start of the assessment may also improve their hospital stay when the children were at their most vulnerable. Some of them had experienced deficient communication, and they expressed a wish to be invited both to participate and to communicate. This is also strengthened by Coyne and Gallagher study, where hospitalised children wanted to be included in communication exchanges and felt better when they were invited to participate. Reference Coyne and Gallagher15
Our results reveal a contradiction in the children’s descriptions about living with their heart disease. They describe its large impact, such as the need to rest every day, but at the same time shrug off the experience as barely worth mentioning. This could be understood by the chronic paradoxes of CHD, defined as “experiences and strategies that address the often lifelong and contradictory nature of living with CHD”. Reference Chong, Fitzgerald and Craig4 It could also be viewed by the concept of illness identity, defined as “the degree to which a chronic health condition, such as heart disease, is integrated into someone’s identity.” Reference Van Bulck, Luyckx, Hoosens, Oris and Moons16 This includes both how the disease is comprehended and how much influence the disease has on the child’s self-image.
Limitations
One limitation in our study may be the small number of children (n = 9) included; however, 27 interviews were conducted in total. For a small project, five or six interviews could be enough. Reference Braun, Clarke, Hayfield, Terry and Liamputtong17 In qualitative research, the number of participants is usually small since the aim is to give a deeper understanding of the phenomenon explored and not to generalise findings.
Conclusion
The children’s symptoms, their experiences during the assessment, their future surgeries, and how the heart disease affects their everyday life could be better understood as elements of their adaptation to the heart disease. In order to achieve individualised support based on the child’s experiences and to ensure that these children are involved in their own care, a child-centered approach is recommended. Furthermore, by inviting the children to participate during the assessment, the shortcomings in communication can better be avoided.
Acknowledgements
The authors are grateful to the children that generously shared their experiences at three times. We are also grateful to Catriona M Chaplin for language editing.
Financial support
This study was supported by Swedish Heart- and Lung Foundation (PL), the Pediatric Heart center at the Skåne University Hospital (BS), and Lund University (PL).
Conflicts of interest
None.
Ethical standards
This study was approved by the Ethical Review Board at Lund University (approval no. 2014/66) and conducted in line with the World Medical Association Declaration of Helsinki. 18








