Introduction
Maternal depression confers risk for a range of internalizing problems in offspring, including depression, anxiety, and irritable mood (Goodman et al., Reference Goodman, Rouse, Connell, Broth, Hall and Heyward2011). While ample evidence supports that maternal depression influences children’s internalizing symptoms, less research has examined reciprocal pathways in which children’s internalizing symptoms exert effects on maternal depressive symptoms over time (Sameroff, Reference Sameroff2009). Though limited, research examining reciprocal associations (i.e., bidirectional effects) between children and mothers has been mixed, and importantly, the vast majority of these studies have failed to parse between- and within-person associations, comparing average levels of symptoms between individuals in a sample rather than changes within the individual (Hails et al., Reference Hails, Reuben, Shaw, Dishion and Wilson2018; Hentges et al., Reference Hentges, Graham, Plamondon, Tough and Madigan2021; Kuckertz et al., Reference Kuckertz, Mitchell and Wiggins2018; Roubinov et al., Reference Roubinov, Epel, Adler, Laraia and Bush2022; Tyrell et al., Reference Tyrell, Yates, Reynolds, Fabricius and Braver2019). Thus, a between-person approach does not show how changes in both mother’s and offspring’s internalizing symptoms, relative to their own means, lead to increases in each other’s symptoms over time. In the current report, we address this major gap by examining within-person reciprocal associations among maternal depressive symptoms, and child depressive, anxiety and irritability symptoms using a random intercept cross-lagged panel model (RI-CLPM).
Importance of within-person effects for developmental research
Although prior longitudinal research has largely relied on between-person approaches, developmental theories are concerned with changes within individuals across time that require a within-person approach. For example, research has consistently shown that offspring of mothers with higher levels of depressive symptoms relative to other mothers (the sample mean) have a greater likelihood of experiencing higher levels of internalizing symptoms relative to other children in the sample (Goodman et al., Reference Goodman, Rouse, Connell, Broth, Hall and Heyward2011); this is an example of a between-person effect because symptom levels are being compared across individuals within a given sample. We cannot infer from this between-person effect, however, that when mothers experience greater depression relative to their typical (average) levels, their children would also be at increased risk to experience greater internalizing symptoms relative to their typical (average) levels of internalizing symptoms (i.e., a within-person effect). By examining change in repeated assessments over time, within-person models can elucidate factors that may be responsible for changes in the individual’s symptom trajectories over time. The RI-CLPM approach may therefore be more clinically useful, as clinicians are generally concerned with change in the individual patient’s symptoms, such as detecting and predicting worsening symptoms.
A RI-CLPM approach uniquely parses between- and within-person effects, which may yield distinct relations between maternal depression and offspring internalizing psychopathology over time (Curran & Bauer, Reference Curran and Bauer2011). For example, while some between-person studies found reciprocal associations between greater child internalizing symptoms and maternal depression, (Hails et al., Reference Hails, Reuben, Shaw, Dishion and Wilson2018; Kuckertz et al., Reference Kuckertz, Mitchell and Wiggins2018; Wiggins et al., Reference Wiggins, Mitchell, Stringaris and Leibenluft2014), the only two within-person studies found unidirectional effects, from within-person maternal depression to greater child internalizing symptoms, with no effect from child to maternal symptoms (Cioffi et al., Reference Cioffi, Leve, Natsuaki, Shaw, Reiss, Ganiban and Neiderhiser2021; Tyrell et al., Reference Tyrell, Yates, Reynolds, Fabricius and Braver2019). Furthermore, robust between-person research on the development of internalizing symptoms has documented evidence of both homotypic (i.e., one disorder predicts the same disorder over time) and heterotypic (i.e., one disorder predicts another disorder over time) continuity in the course of child depression, anxiety and irritability across development (Bornstein et al., Reference Bornstein, Putnick and Esposito2017; Vidal-Ribas and Stringaris, Reference Vidal-Ribas Belil and Stringaris2021); however, research examining within-person homotypic and heterotypic continuity of children’s internalizing symptoms is far more limited (Cohen et al., Reference Cohen, Andrews, Davis and Rudolph2018; Ezpeleta et al., Reference Ezpeleta, Penelo, Navarro, Osa and Trepat2020; Long et al., Reference Long, Young and Hankin2019; Steinsbekk et al., Reference Steinsbekk, Ranum and Wichstrøm2022). Only RI-CLPM allows us to examine the simultaneous relations from 1) deviations in within-person maternal depressive symptoms relative to her mean at age 3 to deviations in child depressive (or child anxiety or irritability) symptoms relative to the child’s mean at age 15, 2) within-person deviations in child depressive (or child anxiety or irritability) symptoms relative to the child’s mean at age 3 to deviations in maternal depressive symptoms relative to her mean at age 15, and 3) within-person deviations in child depressive (or anxiety or irritability) symptoms relative to the child’s mean at age 3 to changes in child depressive (or anxiety or irritability) symptoms relative to the child’s mean at age 15.
Maternal depression and children’s internalizing psychopathology
Prior work has consistently supported between-person pathways from maternal depression to child depression (e.g., Goodman et al., Reference Goodman, Rouse, Connell, Broth, Hall and Heyward2011; Weissman et al., Reference Weissman, Wickramaratne, Gameroff, Warner, Pilowsky, Kohad, Verdeli, Skipper and Talati2016), anxiety (e.g., Klein & Finsaas, Reference Klein and Finsaas2017; Rice et al., Reference Rice, Sellers, Hammerton, Eyre, Bevan-Jones, Thapar, Collishaw, Harold and Thapar2017), and irritability (e.g., Dougherty et al., Reference Dougherty, Smith, Bufferd, Stringaris, Leibenluft, Carlson and Klein2013; Krieger et al., Reference Krieger, Polanczyk, Goodman, Rohde, Graeff-Martins, Salum, Gadelha, Pan, Stahl and Stringaris2013) across development. Likewise, studies examining within-person trajectories have also found that maternal depression predicts high and increasing levels of offspring internalizing symptoms across childhood and adolescence (Ezpeleta et al., Reference Ezpeleta, Penelo, Navarro, Osa and Trepat2020; Fanti & Henrich, Reference Fanti and Henrich2010; Gartstein et al., Reference Gartstein, Bridgett, Rothbart, Robertson, Iddins, Ramsay and Schlect2010; Gutman & Codiroli McMaster, Reference Gutman and Codiroli McMaster2020; Leve et al., Reference Leve, Kim and Pears2005; Sterba et al., Reference Sterba, Prinstein and Cox2007; Wiggins et al., Reference Wiggins, Mitchell, Stringaris and Leibenluft2014). For example, Ezpeleta et al. (Reference Ezpeleta, Penelo, Navarro, Osa and Trepat2020) found that maternal depressive symptoms at age 3 predicted chronically high within-person trajectories of child depressive, anxiety, and irritability symptoms from age 3 to age 11. In contrast, tests of reciprocal effects using between-person approaches (i.e., child effects on mothers’ symptomatology) have been mixed, with some demonstrating reciprocal associations (Hails et al., Reference Hails, Reuben, Shaw, Dishion and Wilson2018; Kuckertz et al., Reference Kuckertz, Mitchell and Wiggins2018; Roubinov et al., Reference Roubinov, Epel, Adler, Laraia and Bush2022; Wiggins et al., Reference Wiggins, Mitchell, Stringaris and Leibenluft2014), and others observing no effects of child internalizing symptoms on maternal depressive symptoms (Hentges et al., Reference Hentges, Graham, Plamondon, Tough and Madigan2021; Mennen et al., Reference Mennen, Negriff, Schneiderman and Trickett2018; Paquin et al., Reference Paquin, Castellanos-Ryan, Vitaro, Côté, Tremblay, Séguin, Boivin and Herba2020). To our knowledge, only two studies have employed within-person methods to examine reciprocal relations between maternal and child symptoms. The first study found that within-person maternal depressive symptoms at 18 months predicted greater child internalizing symptoms (parent-reported composite of depressive and anxiety symptoms) at age 27 months, but not vice versa; no effects were found in either direction between within-person maternal depressive symptoms and child symptoms from ages 27 months to 6 years old (Cioffi et al., Reference Cioffi, Leve, Natsuaki, Shaw, Reiss, Ganiban and Neiderhiser2021). The second study found similar patterns in older youth: within-person maternal depressive symptoms at age 13 predicted increases in offspring’s self-reported internalizing problems at age 22 but not vice versa (Tyrell et al., Reference Tyrell, Yates, Reynolds, Fabricius and Braver2019).
Studies investigating within-person developmental pathways that include both mother and child symptoms are scarce. To our knowledge, no study has tested serial mediation (i.e., more than one mediating variable in a pathway) among within-person maternal and child internalizing symptoms. Given the long-term consequences of maternal depression and youth depressive, anxiety, and irritability symptoms (Goodman et al., Reference Goodman, Rouse, Connell, Broth, Hall and Heyward2011), it is crucial to understand the sequential and reciprocal unfolding of these problems from early childhood to adolescence. Furthermore, existing studies have generally examined children’s internalizing problems broadly, using composite measures of anxiety and depression, rather than measures of multiple distinct internalizing symptoms (Cioffi et al., Reference Cioffi, Leve, Natsuaki, Shaw, Reiss, Ganiban and Neiderhiser2021; Tyrell et al., Reference Tyrell, Yates, Reynolds, Fabricius and Braver2019). This approach may obscure unique associations among specific internalizing problems (i.e., depression, anxiety, irritability) and between specific internalizing problems and maternal depressive symptoms over time, particularly as different facets of child internalizing symptoms may pose unique challenges to parents (Kiff et al., Reference Kiff, Lengua and Zalewski2011).
Current study
The current study aims to address these gaps and employs a RI-CLPM approach to examine reciprocal influences of within-person maternal depressive symptoms and children’s depressive, anxiety and irritability symptoms from ages 3 to 15 years old. While the majority of work has focused on youth depression and anxiety (Luby et al., Reference Luby, Si, Belden, Tandon and Spitznagel2009; Steinsbekk et al., Reference Steinsbekk, Ranum and Wichstrøm2022), recent work using between-person methods has provided compelling evidence that childhood irritability also predicts subsequent depressive and anxiety disorders in youth and adults (Brotman et al., Reference Brotman, Kircanski, Stringaris, Pine and Leibenluft2017; Sorcher et al., Reference Sorcher, Goldstein, Finsaas, Carlson, Klein and Dougherty2022; Stringaris et al., Reference Stringaris, Cohen, Pine and Leibenluft2009) and is linked with maternal depression (Dougherty et al., Reference Dougherty, Smith, Bufferd, Stringaris, Leibenluft, Carlson and Klein2013; Vidal-Ribas et al., Reference Vidal-Ribas, Brotman, Valdivieso, Leibenluft and Stringaris2016; Wiggins et al., Reference Wiggins, Mitchell, Stringaris and Leibenluft2014). No study, however, has investigated within-person, reciprocal pathways between child irritability and maternal depressive symptoms. Moreover, no prior work has explored serial mediation of within-person maternal depressive symptoms and child depressive, anxiety and irritability symptoms across development.
We used a community sample of 609 children from the Stony Brook Temperament Study (SBTS), a longitudinal study following a large cohort from age 3 to 15 years old with assessments every 3 years (Klein & Finsaas, Reference Klein and Finsaas2017). First, we hypothesized that within-person maternal depressive symptoms and child depressive, anxiety, and irritability symptoms would reciprocally influence one another from ages 3 to 15, such that greater within-person maternal symptoms will predict greater child symptoms and vice versa. Furthermore, consistent with prior between-person research (Goodman et al., Reference Goodman, Rouse, Connell, Broth, Hall and Heyward2011), we hypothesized that maternal depressive symptoms, and child depressive, anxiety, and irritability symptoms would show robust and positive associations with one another at the between-person level.
Though limited, a few studies investigating within-person person trajectories found that depressive, anxiety, and irritability symptoms are concurrently and prospectively related from childhood to adolescence (Chad-Friedman et al., Reference Chad-Friedman, Galano, Lemay, Olino, Klein and Dougherty2021; Ezpeleta et al., Reference Ezpeleta, Penelo, Navarro, Osa and Trepat2020) and from adolescence through young adulthood (Leadbeater et al., Reference Leadbeater, Thompson and Gruppuso2012), suggesting that these three symptoms may influence one another reciprocally across development. Thus, we hypothesized that deviations in within-person child depressive, anxiety, and irritability symptoms will predict one another from ages 3 to 15. Finally, we hypothesized that greater child depressive, anxiety, and irritability symptoms would be associated with one another at the between-person level, consistent with prior work (for a review, see: Vidal-Ribas Belil & Stringaris, Reference Vidal-Ribas Belil and Stringaris2021).
Methods
Participants
Participants were selected from the Stony Brook Temperament Study, a longitudinal study examining the role of early temperament on the development of internalizing disorders (for detailed description of the study sample and recruitment see Klein & Finsaas, Reference Klein and Finsaas2017). In 2004, families with a 3-year-old child were recruited within 20 contiguous miles of Stony Brook University and identified via commercial mailing lists. Eligible families had a child between 3 and 4 years old with no developmental disabilities or serious medical conditions and at least one English-speaking biological parent. The study was approved by the human subjects review committee. Parents provided informed consent and children ages 9 and older provided assent. Families were financially compensated for participating in the study.
Participants were assessed at ages 3, 6, 9, 12, and 15 years old. At baseline (age 3: M = 3.55 years, SD = .26), 559 families entered the study and 473 mothers completed a measure about their depressive symptoms and 547 mothers completed a measure about their child’s irritability, depressive, and anxiety symptoms. At the age 6 assessment (age M = 6.11 years, SD = .44), an additional 50 Black/African American, Asian, and Hispanic families were recruited to increase the racial and ethnic diversity of the sample and better reflect the demographic composition of the surrounding area. In addition, 470 mothers completed a measure about their depressive symptoms and 467 mothers completed a measure about their child’s behaviors. At ages 9 (age M = 9.23 years, SD = .42), 12 (age M = 12.66 years, SD = .46), and 15 (age M = 15.25 years, SD = .41), mothers completed measures about their depressive symptoms (9: n = 482, 12: n = 469, 15: n = 449) and their child’s behaviors (9: n = 490, 12: n = 472, 15: n = 454). See Table 1 for demographic information and sample characteristics.
Table 1. Sample characteristics (n = 609)
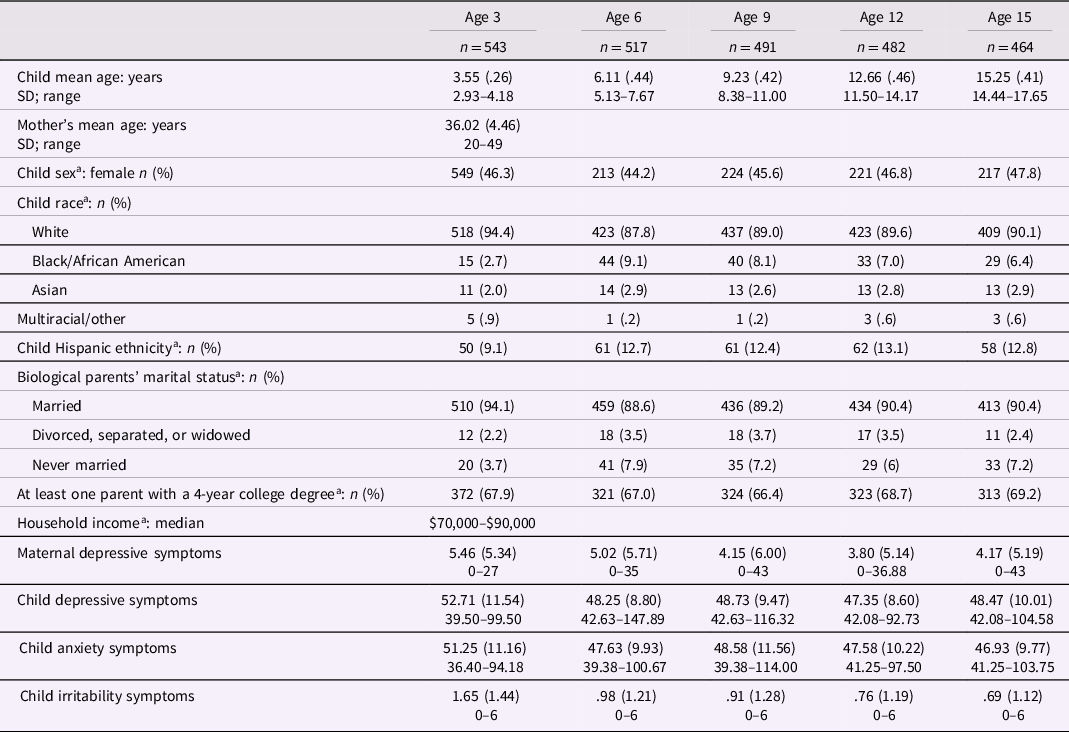
Note. The sample (n = 605) includes any child whose parent completed at least one measure about their own depression or a measure about their child’s symptoms. An additional 50 participants were recruited at the age 6 assessment. Parental depressive symptoms were assessed using the Diagnostic Inventory of Depression (DID) self-report scale. Child depressive symptoms, anxiety symptoms, and irritability symptoms were assessed using the parent-report Child Behavior Checklist (CBCL).
Of the 605 families who provided data, 304 participants provided data across all five waves, and 122 participants provided data across 4 waves; 64 and 39 participants completed data across three and two waves, respectively. Those with at least some missing data did not differ significantly from the remainder of the sample with complete data (all ps > .05). Little’s MCAR test (Little & Rubin, Reference Little and Rubin1989) confirmed that missingness was unrelated to any mother-report variable in our study: X2 (60) = 75.35, p = .087. Maximum likelihood (ML) procedures were therefore considered appropriate for modeling the missing data (Schafer & Graham, Reference Schafer and Graham2002).
Measures
Maternal depressive symptoms. Across all waves, mothers completed the 19-item Diagnostic Inventory for Depression (DID; Zimmerman et al., Reference Zimmerman, Sheeran and Young2004). The DID is a self-report scale used to assess symptoms of DSM-IV depressive symptoms over the past week in adults. The DID has achieved high levels of internal consistency, test–retest reliability, and construct validity and is a valid measure of symptom change over time (Zimmerman et al., Reference Zimmerman, Sheeran and Young2004). In the current sample, internal consistency was excellent at all timepoints (Median α = .87, range = .85–.90). Based on clinical interviews conducted at ages three and nine assessments with parents using the Structured Clinical Interview for DSM-IV (First et al., Reference First, Spitzer, Gibbon and Williams1996), 215 mothers (36.4%) had a lifetime history of a depressive disorder. At the age 3 and 9 assessments, 37 mothers (6.9%) and 15 mothers (3.1%) had a current depressive disorder (in the past month), respectively.
Child behavior checklist (CBCL). We used the mother report CBCL to assess nonoverlapping child symptoms of irritability, depression, and anxiety (Achenbach & Rescorla, Reference Achenbach and Rescorla2001; Achenbach, Reference Achenbach2000). The CBCL was selected because it was the only measure assessed at each time point and it therefore allowed us to examine within-person changes in child symptoms overtime. The CBCL captures the past 6 months and has been used extensively to assess children’s internalizing symptoms in longitudinal studies (Achenbach & Ruffle, Reference Achenbach and Ruffle2000). At age 3, mothers completed the CBCL 1.5–5 (Achenbach, Reference Achenbach2000) and at ages 6 and older, mothers completed the CBCL 6–18 version (Achenbach & Rescorla, Reference Achenbach and Rescorla2001). Items on the CBCL are rated by parents on a 3-point scale (0 = never/not true; 1 = sometimes; 2 = often/very true). To assess child irritability, we used the empirically derived CBCL-irritability factor score (Evans et al., 2020; Roberson-Nay et al., Reference Roberson-Nay, Leibenluft, Brotman, Myers, Larsson, Lichtenstein and Kendler2015; Stringaris et al., Reference Stringaris, Zavos, Leibenluft, Maughan and Eley2012). The CBCL-irritability factor score sums three items assessing irritable mood, sudden changes in mood, and temper outbursts. The parent-report CBCL-irritability factor score has been used with children ranging from preschool-age through adolescence and demonstrates acceptable reliability, convergent validity, and structural invariance over time (Aebi et al., Reference Aebi, Plattner, Metzke, Bessler and Steinhausen2013; Roberson-Nay et al., Reference Roberson-Nay, Leibenluft, Brotman, Myers, Larsson, Lichtenstein and Kendler2015; Stringaris et al., Reference Stringaris, Zavos, Leibenluft, Maughan and Eley2012; Tseng et al., Reference Tseng, Moroney, Machlin, Roberson-Nay, Hettema, Carney, Stoddard, Towbin, Pine, Leibenluft and Brotman2017; Wiggins et al., Reference Wiggins, Mitchell, Stringaris and Leibenluft2014). Internal consistency of the irritability score was acceptable across assessments (median α = .73, range: α = .68–.77).
We used the Diagnostic and Statistical Manual (DSM)-oriented CBCL scales to assess children’s symptoms of depression (Affective Problems scale) and anxiety (Anxiety Problems scale) (Achenbach and Rescorla, Reference Achenbach and Rescorla2001; Achenbach, Reference Achenbach2000). These scales contained no overlapping items with the CBCL-irritability factor scale and had acceptable internal consistency at each timepoint (Affective Problems: median: α = .68, range: α = .62–.78; Anxiety Problems: median: α = .72, range: α = .64, –.76). Given that the different versions of the CBCL include different items, we converted the raw DSM-oriented scales into age- and sex-based T-scores, with higher scores indicating more frequent symptoms (Achenbach & Rescorla, Reference Achenbach and Rescorla2001; Achenbach, Reference Achenbach2000). Unlike standardized z-scores, T-scores are sample independent and do not remove between-person and within-person variability.
Data analysis plan
Analyses were conducted using Mplus Version 8. We conducted a random intercept cross-lagged panel model (RI-CLPM) to examine reciprocal relations among maternal depressive symptoms, child depression, anxiety, and irritability. The traditional cross-lagged panel model is limited, given it aggregates between- and within-person levels of variance and can therefore yield erroneous conclusions about causal patterns or biased parameters and coefficients (Hamaker et al., Reference Hamaker, Kuiper and Grasman2015; Mund & Nestler, Reference Mund and Nestler2019). Thus, we used the RI-CLPM, which includes important features of the CLPM, but extends it by partialling out between-person variance in a random intercept (one for each construct: maternal depressive symptoms, child depression, anxiety, and irritability). Correlations between the random intercepts of each construct (which aggregate data across all assessment waves) represent the concurrent between-person associations between maternal depressive symptoms, and child depressive, anxiety, and irritability symptoms. Partialling out between-person variance in random intercepts allows for an examination of cross-lagged within-person change over time. This is critical, given that the cross-lagged relationships pertain to a process that takes place at a within-person levelFootnote 1 .
We thus estimated lagged effects and stability paths between within-person centered variables. We modeled the residuals of the within-person stability paths for each construct across timepoints (e.g., from age 3 within-person child depression to age 6 within-person child depression) and all within-person variables within each time point were covaried. We also modeled between-person concurrent associations (the random-intercepts of each construct). All waves of data were included and all variables were entered simultaneously to examine unique relations among maternal depressive symptoms and child depressive, anxiety, and irritability symptoms, while controlling for the other variables. We followed model specifications outlined in Hamaker et al (Reference Hamaker, Kuiper and Grasman2015). Our focal model did not include constraints on the same paths across time. Serial indirect effects were estimated via bootstrapping procedures (Hayes & Rockwood, Reference Hayes and Rockwood2017). Serial mediation tests the sequential mediating pathways between all variables across the 5 time points from ages 3 to 15.
As measures of goodness of fit, chi-square, the comparative fit index (CFI), the root-mean-square error of approximation (RMSEA), and the Standardized Root Mean Square Residual (SRMR) were used. Generally, CFI values greater than .90 (Hoyle & Panter, Reference Hoyle and Panter1995), and a RMSEA and SRMR of less than .08 (Kline, Reference Kline1988) indicate acceptable fit.
Results
Bivariate correlations among maternal depressive, child depressive, child anxiety, and child irritability symptoms across waves are presented in Supplementary Table 1.
Maternal depressive symptoms, child irritability, child depressive symptoms, and child anxiety
Model fit. The RI-CLPM is presented in Figure 1. The model demonstrated excellent fit to the data: χ2 (82, N = 605) = 139.92, p < .001, CFI = .985, RMSEA = .034, SRMR = .043.
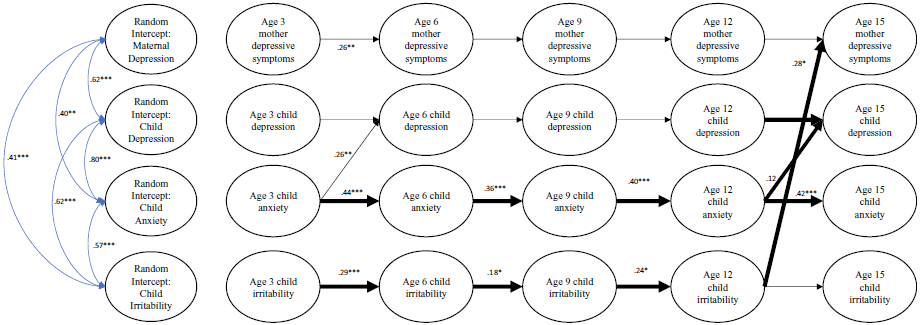
Figure 1. Random-intercept cross-lagged panel analyses (RI-CLPM) for maternal depressive symptoms, and child depressive, anxiety, and irritability symptoms from ages 3 to 15 years old. Note: Standardized values presented (B). Bolded paths are involved in indirect pathways. All stability paths and within-person cross lagged paths were included in analyses, and significant ones or those involved in indirect pathways are presented in this figure for readability. Covariances are not shown in this figure but were included between all variables measured in the same assessment wave. Between-person pathways are shown in blue. *** p < .001, ** p < .01, * p < .05.
Between-person direct effects. At the between-person level, the random intercept factor for maternal depressive symptoms was significantly and positively associated with the random intercept factors for child depressive (b = 14.13 SE = 2.75 p < .001), anxiety, (b = 10.42, SE = 2.42 p < .001), and irritability symptoms (b = 1.30 SE = .37 p < .001). The random intercept factors were also significantly and positively associated for child depressive and anxiety symptoms (b = 27.02 SE = 8.56, p = .002), child depressive and irritability symptoms (b = 2.66 SE = .73 p < .001), and child anxiety and irritability symptoms (b = 2.75 SE = .84 p = .001).
Within-person direct effects. Regarding homotypic pathways, within-person maternal depressive symptoms at age 3 predicted greater maternal depressive symptoms at age 6. Within-person child anxiety symptoms at ages 3, 6, and 9 predicted greater child anxiety at ages 6, 9, and 12, respectively. However, within-person child anxiety symptoms at age 12 did not predict anxiety at age 15. Within-person child irritability symptoms at ages 3, 6, and 9 predicted greater irritability at ages 6, 9, and 12, respectively. Within-person child irritability symptoms at age 12 did not predict irritability at age 15. Within-person child depressive symptoms at ages 3, 6, and 9 did not predict depressive symptoms at ages 6, 9, 12, and 15, respectively.
Regarding cross-lagged paths, within-person child anxiety symptoms at age 3 predicted greater child depressive symptoms at age 6 (b = .19, SE = .07, p = .008) and within-person child irritability symptoms at age 12 predicted greater maternal depressive symptoms at age 15. No other within-person direct effects were significant.
Within-person indirect effects. Three indirect pathways were observed: Within-person child anxiety symptoms at age 3 predicted greater child anxiety at age 15 via greater child anxiety from ages 6 to 12 (b = .018, p < .05, 95% CI [.004, .087]); within-person child anxiety symptoms at age 3 also predicted greater child depressive symptoms at age 15 via greater child anxiety from ages 6 to 12 (b = .006, p < .05, 95% CI [.001, .030]); and within-person child irritability symptoms at age 3 predicted greater maternal depressive symptoms at age 15 via greater child irritability from ages 6 through 12 (b = .009, p < .05, 95% CI [.001, .036]). No other indirect pathways from age 3 to 15 were significant.
We proceeded the above analyses by building pairwise models before testing the full model and included these models in Supplemental Materials 1–3.
Discussion
The current study employed a random intercept cross-lagged panel model (RI-CLPM) to examine longitudinal, within-person associations among maternal depressive and child depressive, anxiety, and irritability symptoms from early childhood to adolescence. Consistent with prior work, we found robust between-person associations: maternal depressive symptoms and child internalizing symptoms were all significantly and positively associated. The model also revealed several longitudinal indirect within-person pathways: higher levels of within-person child anxiety symptoms at age 3 predicted both greater child anxiety and depressive symptoms at age 15 via greater child anxiety from ages 6 to 12; and higher levels of within-person child irritability at age 3 predicted greater maternal depressive symptoms at age 15 through greater child irritability from age 6 to 12. We did not, however, find reciprocal relations between within-person maternal and child internalizing symptoms. Our findings offer novel insights into the serial mediation of symptoms and the effects of deviations from mean-level child internalizing symptoms on subsequent deviations in maternal depressive and child internalizing symptoms.
At the between-person level, child depressive, anxiety, and irritability symptoms were positively associated with one another and with maternal depressive symptoms. These findings align with a wealth of prior literature that shows robust co-occurrence among child internalizing symptoms and links between maternal and child symptomology (for a review, see; Goodman et al., Reference Goodman, Rouse, Connell, Broth, Hall and Heyward2011). Moreover, these between-person effects indicate that maternal and offspring internalizing symptoms are associated at the trait level and may share etiological pathways to psychopathology. By capturing between-person variance in intercepts, our model was able to disentangle trait-level effects from within-person changes in symptoms over time, illuminating longitudinal effects among maternal and child internalizing symptoms.
At the within-person level, we found both homotypic and heterotypic pathways from child anxiety at age 3 to children’s later internalizing symptoms. Children who scored higher than their expected anxiety scores at age 3 scored higher than their expected anxiety (i.e., homotypic) and depression (i.e., heterotypic) scores at 15 years old, and this effect was mediated by a tendency for children to score higher than expected on anxiety at ages 6 through 12. Our findings align with prior work demonstrating homotypic and heterotypic between-person pathways from early childhood anxiety to adolescent anxiety and depression, respectively (Liu & Pérez-Edgar, Reference Liu and Pérez-Edgar2019). Furthermore, our findings add to the emerging literature demonstrating within-person pathways of early childhood anxiety to adolescent anxiety (Cohen et al., Reference Cohen, Andrews, Davis and Rudolph2018; Ezpeleta et al., Reference Ezpeleta, Penelo, Navarro, Osa and Trepat2020; Steinsbekk et al., Reference Steinsbekk, Ranum and Wichstrøm2022) and within-person pathways from anxiety during middle childhood to adolescent depressive symptoms (Cohen et al., Reference Cohen, Andrews, Davis and Rudolph2018; Long et al., Reference Long, Young and Hankin2019). Importantly, our study extends the predictive validity of within-person early childhood anxiety to later adolescent depressive symptoms and reveals these unique within-person pathways even after adjusting for between-person variance, within-person stability in maternal depressive symptoms, and child depressive, anxiety, and irritability symptoms.
Drawing from the between-person literature, research suggests that both early childhood fearful temperament (i.e., behavioral inhibition) and certain parenting behaviors (e.g., overprotective parenting) may play roles in pathways to a chronic course of childhood anxiety (Hudson et al., Reference Hudson, Dodd, Lyneham and Bovopoulous2011; Johnson et al., Reference Johnson, Riis and Noble2016) and the subsequent emergence of adolescent depression (Bohlin et al., Reference Bohlin, Hagekull and Andersson2005; Gazelle & Faldowski, Reference Gazelle and Faldowski2014). For example, a fearful temperament and overprotective parenting may increase a child’s avoidant behavior toward anxiety-provoking stimuli and situations, thus maintaining anxiety over time (Liu & Pérez-Edgar, Reference Liu and Pérez-Edgar2019). Moreover, children experiencing anxiety across childhood may participate in fewer enjoyable activities (related to their avoidance), in turn impeding socioemotional development and increasing risk of developing depression as children reach adolescence (Jones et al., Reference Jones, Lebowitz, Marin and Stark2015). However, it is not yet known whether these mechanisms extend to within-person pathways of anxiety. Identifying within-person mechanisms that maintain childhood anxiety problems across development is a critical next step to understanding fluctuations in individual symptoms over time.
We also found that child symptoms impact maternal symptoms at the within-person level. Specifically, we observed that within-person child irritability at age 3 predicted greater maternal depressive symptoms at age 15 through greater irritability from ages 6 to 12. Our results align with prior between-person work which found that greater early childhood irritability predicted greater subsequent maternal depressive symptoms (Wiggins et al., Reference Wiggins, Mitchell, Stringaris and Leibenluft2014), suggesting that child irritability may be particularly challenging for parents to manage, eliciting greater stress from caregivers and increasing depressive symptoms. Furthermore, mothers and children share a genetic liability for emotion dysregulation and irritability, which may increase the likelihood that parents of irritable children experience negative mood changes in response to irritability in children (Stringaris et al., Reference Stringaris, Vidal-Ribas, Brotman and Leibenluft2018; Vidal-Ribas et al., Reference Vidal-Ribas, Brotman, Valdivieso, Leibenluft and Stringaris2016). Taken together, our findings emphasize the importance of prolonged child internalizing symptoms across development. Future work should explore the mechanisms of within-person pathways from child irritability to maternal depression, as this work could illuminate important areas of intervention to prevent persistent child internalizing symptoms, individual fluctuations in irritability and subsequent maternal depressive symptoms.
We did not find that within-person child irritability predicted later youth depression or anxiety; this contrasts with prior studies documenting between-person associations between youth irritability and subsequent depressive and anxiety disorders (for a review see Brotman et al., Reference Brotman, Kircanski, Stringaris, Pine and Leibenluft2017; Sorcher et al., Reference Sorcher, Goldstein, Finsaas, Carlson, Klein and Dougherty2022). It is possible that these associations are not present at the within-person level, because absolute high levels of irritability are stronger indicators of depressive symptoms (between-person effects) than high levels of irritability relative to an individual mean. Adjusting for the shared variance of children’s depressive, anxiety, and irritability symptoms may also have partialled out a general disposition to negative affectivity, which may play an important role in within-person effects. Further examination is required to determine whether or not these within-person effects are present. We only assessed youth until age 15, which is only the beginning of the heightened risk period for internalizing disorders and assessments were limited to maternal-report of youth symptoms, which may be less sensitive than youth self-report. Given prior work finding specific associations between youth irritability and adult depressive and anxiety disorders (Brotman et al., Reference Brotman, Schmajuk, Rich, Dickstein, Guyer, Costello, Egger, Angold, Pine and Leibenluft2006; Stringaris et al., Reference Stringaris, Cohen, Pine and Leibenluft2009), future work should investigate symptoms using youth self-report measures and assess youth across adolescence and into young adulthood.
Surprisingly, we did not find directional effects from within-person maternal depressive symptoms and child internalizing symptoms. These findings diverge from two within-person studies demonstrating links between maternal depression and children’s internalizing symptoms in infancy (Cioffi et al., Reference Cioffi, Leve, Natsuaki, Shaw, Reiss, Ganiban and Neiderhiser2021) and from adolescence to early adulthood (Tyrell et al., Reference Tyrell, Yates, Reynolds, Fabricius and Braver2019). Cioffi et al. (Reference Cioffi, Leve, Natsuaki, Shaw, Reiss, Ganiban and Neiderhiser2021), however, found no associations between maternal and child symptoms from 27 months to age 6 years. This may have been due to differences in developmental periods under investigation (i.e., infancy, adolescence to early adulthood), which suggests that maternal symptoms are less impactful on children’s symptoms from early childhood to adolescence, compared to infancy or early adulthood. In addition, the use of composite measures of internalizing symptoms may have accounted for differences in findings. Moreover, the maternal and child internalizing symptom random intercepts (i.e., aggregated between-person variance) may have accounted for a significant amount of the total variance, thereby reducing the within-person effects. It is also possible that after accounting for within-person associations between children’s depressive, anxiety, and irritability symptoms over time, effects of maternal symptoms on children were no longer significant. Additional research is needed to clarify reciprocal maternal-child pathways across development that parse between and within-person effects.
Strengths and limitations
Our study has some notable strengths. The use of repeated measures of child and maternal internalizing symptoms allowed us to evaluate serial mediation of maternal and child symptoms and test reciprocal effects at the within-person level. Our study was also strengthened by our ability to measure symptoms from early childhood through the transition to adolescence, a period during which internalizing symptoms become increasingly prevalent.
We must also consider the current findings in light of several important limitations. First, we relied on maternal report to measure child internalizing symptoms from age three to age 15. Recent work across multiple, large samples supports the use of maternal reports as a primary measure of child psychopathology as there is limited evidence for maternal psychopathology biasing reports of child behavior (Olino et al., Reference Paquin, Castellanos-Ryan, Vitaro, Côté, Tremblay, Séguin, Boivin and Herba2020, Reference Olino, Michelini, Mennies, Kotov and Klein2021). Nevertheless, we acknowledge that the use of other informants (co-parent reports, youth self-report) and methods (interview-based assessments) could be beneficial in future work (Dougherty et al., Reference Dougherty, Klein, Olino, Hunsley and Mash2018). Second, our study measured symptoms in three-year intervals from early childhood to adolescence, which could have missed important within-person symptom changes occurring at more frequent time intervals and may not match the temporal frame within which these processes unfold. Third, the sample was largely derived from White, middle-class families, limiting the generalizability of our findings to more diverse samples. Future studies should examine these pathways in culturally diverse samples to explore cross-cultural similarities and differences in relations between within-person maternal and child internalizing symptoms across development.
Conclusions
Our study is the first to use a within-person approach to study three domains of internalizing symptoms in the same model and test reciprocal relations among child and maternal symptoms from early childhood through adolescence. We found novel results regarding serial mediation among within-person child and maternal internalizing symptoms; within-person child anxiety at age 3 predicted greater youth anxiety and depressive symptoms at age 15 through greater anxiety symptoms from ages 6 to 12; and early childhood within-person irritability at age 3 predicted increases in maternal depressive symptoms at age 15 through increases in child irritability from ages 6 to 12. We extend prior literature by identifying within-person effects that are consistent with well-known between person pathways (e.g., child anxiety to depressive symptoms, child irritability to maternal depressive symptoms), and between-person effects that do not hold when tested at the within-person level (e.g., mother to child effects, child irritability to depressive and anxiety symptoms); this may suggest that within-person and between-person pathways operate uniquely.
Finally, understanding the interplay between fluctuations in child and maternal internalizing symptoms (i.e., within-person effects) across development may inform early screening and intervention efforts. For example, our findings support the use of early childhood screening for preschool-age anxiety and irritability. Early prevention and intervention efforts focused on these symptoms may prevent later internalizing problems in both children and their mothers. Moreover, parent-focused interventions that employ cognitive-behavioral techniques to reduce children’s anxiety and emotional dysregulation may be particularly useful in mitigating chronic pathways of internalizing symptoms and broader dysfunction in the family system (Beach et al., Reference Beach, Kogan, Brody, Chen, Lei and Murry2008; Shaw et al., Reference Shaw, Connell, Dishion, Wilson and Gardner2009).
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0954579423000378
Acknowledgments
We thank the families for their time and ongoing participation in the Stony Brook Temperament Study and the research staff for contributing to data collection.
Funding
Support for this research was provided by funding through NIMH R01 MH069942 (Klein) and the National Science Foundation Graduate Research Fellowship Program (Chad-Friedman).
Competing interest
The authors report no conflicts of interest.





