Introduction
Posttraumatic stress disorder (PTSD) can develop after exposure to serious injury, death, or a potential threat to the physical integrity of self or others (Diagnostic and Statistical Manual of Mental Disorders-5; DSM-5, American Psychological Association, 2013). People with PTSD may have cognitive decline, a risk which can be particularly threatening during older age, since cognitive deterioration becomes more common as people grow old (Golier et al., Reference Golier, Harvey, Legge and Yehuda2006). However, some prominent issues remain unclear concerning this PTSD-cognitive decline link in older adults (Palmer, Reference Palmer2021). The current study will specifically address three issues, the directionality of this association, its nature, and an underlying mechanism.
Directionality of cognitive decline and PTSD in old age
The negative effects of PTSD on cognitive function have been widely documented, and a meta-analysis revealed that PTSD has large effects in the domains of verbal learning, speed of information processing, attention/working memory, and verbal memory (Scott et al., Reference Scott2015). Such effects were found following exposure to warfare (Vasterling et al., Reference Vasterling, Duke, Brailey, Constans, Allain and Sutker2002). The effects of warfare on cognition are particularly relevant for older adults, who face greater risks of cognitive decline (Deary et al., Reference Deary2009). Indeed, exposure to warfare and ensuing PTSD symptoms were previously shown to be associated with worse cognitive functioning of older adults (Schuitevoerder et al., Reference Schuitevoerder2013; Shrira et al., Reference Shrira2017). This direction, of PTSD symptoms leading to cognitive decline, has more relevance in older adults, as potentially explained by the allostatic load theory (McEwen, Reference McEwen1998), which suggests that stressful experiences across life can produce “wear-and-tear,” ultimately leading to cognitive decline at older ages (Juster et al., Reference Juster, McEwen and Lupien2010).
Yet the opposite direction, of cognitive function predicting PTSD, is also supported, as both functional impairment and brain anomalies predict future PTSD (Ben-Zion et al., Reference Ben-Zion2020; Rutter et al., Reference Rutter, Vahia, Passell, Forester and Germine2021). Specifically, there is some evidence that smaller hippocampal volume, which affects long-term memory, constitutes a risk factor for the development of PTSD (Gilbertson et al., Reference Gilbertson2002). However, this direction is disputed, with some authors not finding any such association between hippocampal volume and PTSD (e.g. Bonne et al., Reference Bonne2001). Diminished hippocampal volume is accompanied by an impairment in associative memory, which has been suggested to render one more vulnerable to the aftermath of trauma exposure, that is, more likely to develop PTSD (Lambert and McLaughlin, Reference Lambert and McLaughlin2019).
As both directions have received prominent support, making a specific prediction beyond reciprocal effects may be challenging. However, as opposed to the bulk of reviewed literature which focused primarily on younger adults, different factors may play a role in older adults and yield a more directional hypothesis. First, cognitive decline becomes more common in older adults without PTSD and has been linked to variety of issues, for example, institutionalization (Harmand et al., Reference Harmand2014) and hospitalizations (Sprung et al., Reference Sprung2021). Second, the allostatic load previously mentioned may render an older individual more vulnerable to the aftermath of PTSD. While this could provide some background for the study hypotheses, we did not directly examine allostatic load in the current study. Thus, cognitive decline is more likely to follow PTSD in older adults rather than the opposite direction.
Extent of PTSD-related cognitive decline
The second question addresses the extent of cognitive impairment following PTSD; whether overall cognition will be impaired or whether only specific cognitive domains will show a decline. Support for the first possibility stems from the psychiatric classification and evaluation that treats PTSD as an anxiety-related disorder as in the DSM-4 (American Psychiatric Association, 1994). Even according to the DSM-5 (American Psychiatric Association, 2013), the negative alteration cluster overlaps with some anxiety symptoms. Previous research revealed a variety of cognitive impairments for those with elevated anxiety (Bensi and Giusberti, Reference Bensi and Giusberti2007; Eysenck et al., Reference Eysenck, Derakshan, Santos and Calvo2007). Thus, persons with PTSD may display overall cognitive impairment across tasks (e.g. see for review, Remmers and Zander, Reference Remmers and Zander2018).
Alternatively, cognitive impairment could be observed only in cognitive domains related to PTSD. Brain regions associated with PTSD include the hippocampus, prefrontal lobes, and amygdala (e.g. Fenster et al., Reference Fenster, Lebois, Ressler and Suh2018). Following, it would be logical to expect cognitive decline in tasks linked with these regions, that is, recall memory would be impaired in persons with PTSD, as it depends on the hippocampus. Similarly, working memory tasks such as fluency would also be impaired, as it is linked with the prefrontal lobes (Wagner et al., Reference Wagner, Sebastian, Lieb, Tüscher and Tadić2014; Yeung et al., Reference Yeung2016). By the same token, tasks that are not linked with these regions, that is, numeracy, which is linked with parietal regions (Arsalidou et al., Reference Arsalidou2018), would not be impaired.
Depressive symptoms as a potential mediator
The third and final question we address is whether a link between PTSD and cognitive decline is mediated by depressive symptoms. Although numerous investigations have explored the brain mechanisms related to PTSD (Duval et al., Reference Duval, Javanbakht and Liberzon2015; Kühn and Gallinat, Reference Kühn and Gallinat2013), emotional pathways, such as depression, are less explored in older adults. In both younger (Dretsch et al., Reference Dretsch, Thiel, Athy, Irvin, Sirmon‐Fjordbak and Salvatore2012) and middle-aged adults (Ritchie et al., Reference Ritchie2021), depression was found to mediate the linking of PTSD with cognitive measures. As depression per se is related to cognitive performance in older adults (Cohn-Schwartz, Reference Cohn-Schwartz2020; Hertzog et al., Reference Hertzog, Kramer, Wilson and Lindenberger2009; Schwartz et al., Reference Schwartz, Khalaila and Litwin2019; Wilson et al., Reference Wilson2014), the possibility of depression mediating the PTSD cognition links is likely. Furthermore, herein, we specifically address depression which is related to one’s struggle with trauma exposure, as close to 50% of those with PTSD also have depression (Flory and Yehuda, Reference Flory and Yehuda2015). A recent study found that older adults whose PTSD was coupled with depression were less healthy compared to those with PTSD alone (Shrira and Hoffman, Reference Shrira and Hoffman2021). Since physical and cognitive health are linked (Blankevoort et al., Reference Blankevoort2013), these findings suggests that such depression may especially be detrimental and potentially accelerate cognitive decline.
The present study
In summary, the aim of this investigation is threefold: first, to assess the directionality of the PTSD and cognitive function associations in older adults. Although the reviewed literature indicates reciprocal effects, we hypothesized that PTSD symptoms would predict subsequent cognitive decline. Second, we asked whether cognitive decline will exist in tasks unrelated to the PTSD circuit? Based on the above, it is difficult to make a sharp hypothesis and the results should be revealing in discerning between the previously outlined options. Third, to assess whether PTSD-driven depression can mediate a PTSD-cognitive link in older adults. Based on past research, we hypothesize that depressive symptoms will indeed mediate this link. Supplementary Figure 1 shows an overview of the main study model.
Methods
Data and participants
The current study used Survey of Health, Ageing and Retirement in Europe (SHARE; Litwin, Reference Litwin2009) a panel survey conducted in over 20 European countries and Israel, which focuses on community-dwelling adults aged 50 years and above and their spouses (Börsch-Supan et al., Reference Börsch-Supan2013). SHARE is based on a generic questionnaire collected by means of a unified face-to-face computer-assisted personal interview. The survey also includes a drop-off supplement – a leave behind paper-and-pencil questionnaire that each country can modify to explore topics of interest are not included in the generic SHARE questionnaire (Litwin, Reference Litwin2009). In Israel, data were collected by B.I. and Lucille Cohen Institute for Public Opinion Research at Tel-Aviv University. SHARE-Israel received ethical approval from the Institutional Review Board of the Hebrew University of Jerusalem. Israel joined SHARE in 2005.
Data for the current study were taken from the third and fourth Israeli waves, collected in 2013 and 2015, respectively. These waves were chosen due to their implementation of unique drop-off questionnaires, which addressed exposure and reactions to potentially traumatic events. In 2013, the participants were asked about exposure to different warfare events since July 2006, specifically missile attacks from the Gaza strip, the Second Lebanon War, or other hostile or terrorist actions. Missile attacks from the Gaza strip have been ongoing from 2001 to the end of 2013. During this period, there were approximately 15,000 rocket and mortar attacks from Gaza on towns and villages in southern Israel. The Second Lebanon War lasted 33 days during the summer of 2006, during which the Hezbollah Organization launched close to 4,000 missile attacks over northern Israel. The second measurement of exposure to warfare events was carried out in 2015, when respondents were asked about exposure to warfare events during the 2014 Gaza–Israel conflict (a.k.a. Operation Protective Edge). During the conflict, Hamas fired approximately 4,600 mortars and rockets that reached most parts of Israel (Chorev, Reference Chorev2014). Many Israeli adults were further exposed to the events through excessive news consumption during the conflict (Palgi et al., Reference Palgi, Shrira and Hoffman2017).
A total of 2,599 respondents participated in the 2013 wave of SHARE-Israel, out of which 1,792 were interviewed again in the 2015. The analysis focused on adults who reported experiencing at least one traumatic event in 2013 who were 50 years old or over, who did not report being diagnosed with Alzheimer’s disease, dementia, organic brain syndrome, senility, or any other serious memory impairment, and who also filled in the drop-off questionnaires in 2015. Thus, the total analytic sample numbered 567 participants. We conducted an attrition analysis comparing those who completed the drop-off at both time points to those who completed to drop-off only at baseline. T-tests were conducted with continuous variables, and chi-square tests for binary variables. Respondents who completed the drop-off at both time points were significantly (p < 0.05) older (Cohen’s d = 0.15), had better financial status (Cohen’s d = 0.20), had less activities of daily living (ADL) limitations (Cohen’s d = 0.12), better hearing (Cohen’s d = 0.14), and better fluency scores (Cohen’s d = 0.10). They did not differ in terms of their PTSD symptoms, gender, education, depressive symptoms, numeracy, or recall scores.
Measures
Cognitive function
The measures of cognitive functioning were a set of three widely used cognitive tests that are sensitive to aging-related decline (Dewey and Prince, Reference Dewey, Prince and Börsch-Supan2005). The verbal recall measure was a combination of the immediate and delayed memory tests. In the immediate recall test, the interviewer reads out a list of 10 words, after which the respondent is asked to recall as many of them as possible. In the delayed recall test, the respondent is asked to recall these words after a period of about 10 min. The combined score ranges from 0 to 20. These tests are a modified version of Rey’s Auditory Verbal Learning Test – RAVLT, which tests short-term verbal learning and memory and information retention (Dal Bianco et al., Reference Dal Bianco, Garrouste, Paccagnella and Börsch-Supan2013). The verbal fluency test asked respondents to name as many distinct animals within 1 min. Due to outliers in one case, scores above 45 were re-coded as 45. The fluency task examines executive functioning and language ability (Dal Bianco et al., Reference Dal Bianco, Garrouste, Paccagnella and Börsch-Supan2013). The measure for numeracy was based on a Serial Sevens test, in which respondents are asked to subtract 7 from 100, and then to continue on subtracting from the given answer four more times. Respondents received one point for each correct answer and if they made mistakes, their subsequent responses were counted if they were correct in relation to the previous number (Scholey et al., Reference Scholey, Harper and Kennedy2001). Since a high percentage of participants (70% and above) had correct scores on all five trials, we dichotomized the numeracy variable into 0 (no errors) and 1 (at least one error). The test is a measure of concentration and basic calculation skill (Karzmark, Reference Karzmark2000).
PTSD symptoms
Participants in both waves were asked about exposure to traumatic events and subsequent PTSD symptoms. In 2013, they were asked about exposure to difficult and hostile events since July 2006, experienced either as part of the Second Lebanon War, missile attacks from the Gaza strip, or other hostile or terrorist actions. In 2015, respondents were asked about exposure to traumatic events during the 2014 Israel–Gaza conflict. In each interview, participants were shown a list of 12 occurrences and asked to indicate which events they experienced since July 2006 (for the 2013 interview) or during the conflict or in the preceding period, in which missile attacks were sporadically launched from Gaza towards Israel (in the 2015 interview). The events listed included injuries and physical danger to self and to a close other, and damage or danger of damage to one’s personal property or workplace. Participants who reported exposure to any of these events were directed to the 4-item PTSD SPAN (Startle, physically upset by reminders, anger, and numbness; Meltzer-Brody et al., Reference Meltzer-Brody, Churchill and Davidson1999), which examines symptoms of startle response, physiological arousal, anger, and numbness, and has been shown to be as sensitive as longer PTSD measures (Brewin, Reference Brewin2005), and its Hebrew version in older adults has been examined as well (Schwartz and Shrira, Reference Schwartz and Shrira2019; Shrira et al., Reference Shrira2017). Respondents were asked to rate their emotions during the past week in relation to the noted events on a scale of 0–4, and their responses were summed to create a summary score of PTSD symptoms severity (range: 0–16). The scale had good internal consistency (T1: α = 0.86; T2: α = 0.82). Participants who did not report exposure to traumatic events during the 2014 Israel–Gaza conflict (T2) received a score of 0 in the scale of PTSD symptoms, since in that conflict most of Israel was under missile attacks and they therefore did not experience additional warfare-related events.
Depressive symptoms
Depressive symptoms assessed via the Euro-D scale (Prince et al., Reference Prince1999) which constituted the mediator variable. The multivariate analyses used the Euro-D scale from the 2013 survey (T1) and also included the Euro-D from the survey conducted in 2009/2010 (T0; parallel to the second wave of SHARE-Europe) as a control variable. The scale consists of 12 yes\no questions about symptoms experienced in the past month (e.g. depressed mood, fatigue). The scale has a range of 0–12, and a minimum of 10 completed items was required for using the score, such that scores with 10–11 complete items were interpolated. The scale has good internal reliability in the current sample (T0: Kuder–Richardson = 0.70; T1: Kuder–Richardson = 0.76).
Covariates
Several sociodemographic and health covariates were used, due to their potential associations with the main study variables. Age was used as a continuous variable and gender as a dummy variable. Level of education was based on years of formal education. Financial status was tapped via difficulty in making ends meet (range: 1–4), with higher scores indicating better financial adequacy (Litwin and Sapir, Reference Litwin and Sapir2009). Physical health was measured as a count of self-reported functional limitations in ADL of more than 3 months’ duration, such that higher scores indicated more limitations. Self-assessed hearing ability was also included as a covariate, insofar as the recall test required the interviewer to read words aloud (range: 1–5), with higher scores representing better self-rated hearing.
Data analysis
First, we examined descriptive data, followed by bivariate analysis of Pearson’s correlations. We conducted the main data analysis using path analysis. Each cognitive variable was measured at both time points, and the model examined its bidirectional associations with PTSD symptoms. The models also explored the mediation of depressive symptoms, measured at T1. The mediation effects were calculated through bootstrapping set at 5,000 samples (Preacher and Hayes, Reference Preacher and Hayes2008) and in the text they are shown as unstandardized coefficients. Depressive symptoms at baseline were also predicted using depressive symptoms measured previously in 2009/2010 (T0), to rule out the effects of previous depression. Full information maximum likelihood was used to handle missing data. The models were run with a maximum likelihood estimator with robust standard errors to allow variables to deviate from multivariate normality (Satorra and Bentler, Reference Satorra and Bentler2010). Model fit was evaluated based on the criteria of Comparative Fit Index (CFI) > 0.95, Standardized Root Mean Squared Residual (SRMR) < 0.08, and Root Mean Square Error of Approximation (RMSEA) < 0.08 (Hooper et al., Reference Hooper, Coughlan and Mullen2008).
Results
Table 1 shows the descriptive statistics of the study variables. Participants remembered on average nine words correctly in the verbal recall task at T1, which slightly increased to an average of 10 words at T2. They named a mean of 19 animals at baseline and 22 animals in the second measurement. In terms of numeracy, 70% of participants had correct answers on all five trials and 76% were correct at T2. As in previous studies, while healthy older adults report few PTSD symptoms (average scores of 1–2 in a range of 0–16), its existence has detrimental consequences (e.g. Cook et al., Reference Cook, McCarthy and Thorp2017). Participants reported two depressive symptoms on average. The sample was aged 66 years on average and had a slight majority of women. They had over 12 years of education and reported under one ADL on average.
Table 1. Descriptive statistics for the study variables
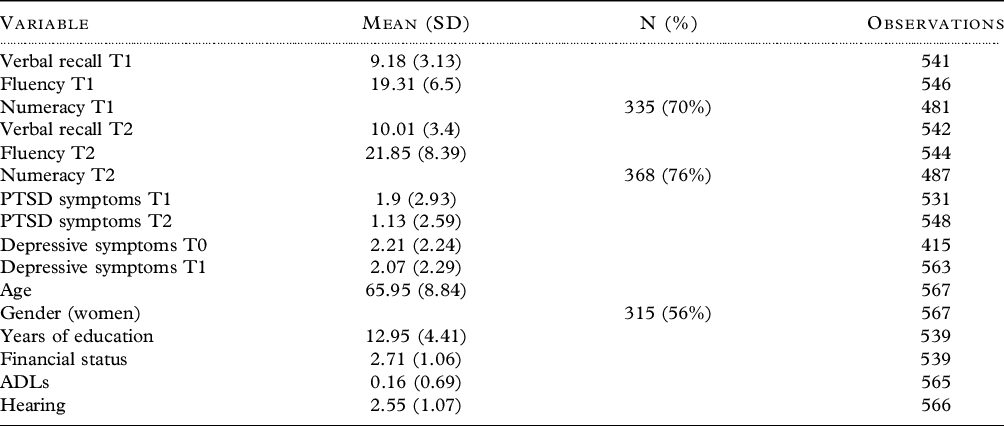
Table 2 presents the correlations between the main study variables. It shows that T1 verbal recall and fluency were negatively associated with T1 PTSD symptoms and depressive symptoms, while numeracy was associated with neither PTSD symptoms nor depressive symptoms. Verbal recall and fluency at T2 were associated with fewer PTSD and depressive symptoms at both time points. Numeracy at T2 was associated with fewer PTSD symptoms at T2 and fewer depressive symptoms at T1.
Table 2. Correlations between the main study variables
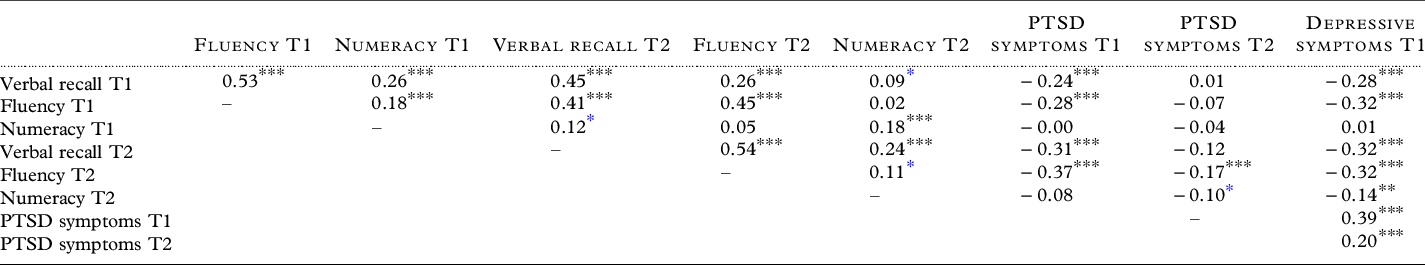
* p < 0.05; ***p < 0.001.
Table 3 shows the bidirectional mediation model for verbal recall and PTSD symptoms. The model exhibited good fit to the data (χ 2 = 8.41, df = 2, CFI = 0.99, RMSEA = 0.075, SRMR = 0.01). The results indicate that adults who had more PTSD symptoms at T1 also had worse recall 2 years later, at T2. Recall at T1 was not associated with future PTSD symptoms. Mediation analyses showed depressive symptoms mediated the association between PTSD symptoms and verbal recall, that is, greater PTSD symptoms at T1 were related to more depressive symptoms, which in turn were related to worse subsequent verbal recall. This indirect effect was −0.03, bootstrapped 95% CIs [−0.061, −0.006], indicating the effect was significant (below the 0.05 level).
Table 3. Cross-lagged models of verbal recall, depressive symptoms, and PTSD
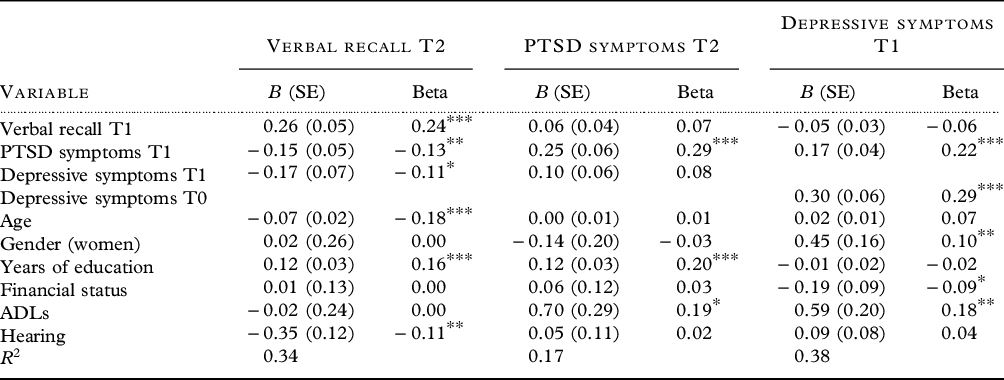
*p < 0.05; **p < 0.01; ***p < 0.001.
Table 4 shows the bidirectional mediation model for fluency and PTSD symptoms. The model exhibited good fit to the data (χ 2 = 8.29, df = 2, CFI = 0.99, RMSEA = 0.075, SRMR = 0.01). It indicates that PTSD symptoms at T1 were significantly related to worse subsequent fluency. Depressive symptoms mediated this association – they were associated with more PTSD symptoms at T1, and to worse fluency at T2. The indirect effect was −0.065, bootstrapped 95% CIs [−0.139, −0.011], indicating a significant effect. Fluency at T1 was not related to future T2 PTSD symptoms.
Table 4. Cross-lagged models of fluency, depressive symptoms and PTSD
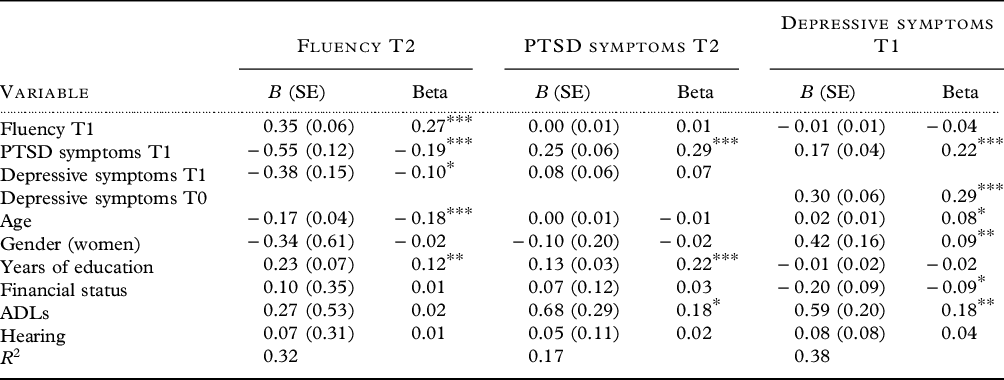
*p < 0.05; **p < 0.01; ***p < 0.001.
Table 5 presents the model results for numeracy and PTSD symptoms. The model exhibited good fit to the data (χ 2 = 5.20, df = 2, CFI = 0.99, RMSEA = 0.05, SRMR = 0.01). It shows that both constructs have no longitudinal associations. Specifically, T1 PTSD symptoms were not related to future numeracy, as T1 numeracy was not related to subsequent PTSD symptoms. However, a mediation association was seen with depressive symptoms. PTSD symptoms at T1 yielded higher depressive symptoms which in turn were linked with worse numeracy scores at T2. The indirect effect was −0.005, bootstrapped 95% CIs [−0.010, −0.001], indicating a significant effect.
Table 5. Crosslagged models of numeracy, depressive symptoms, and PTSD
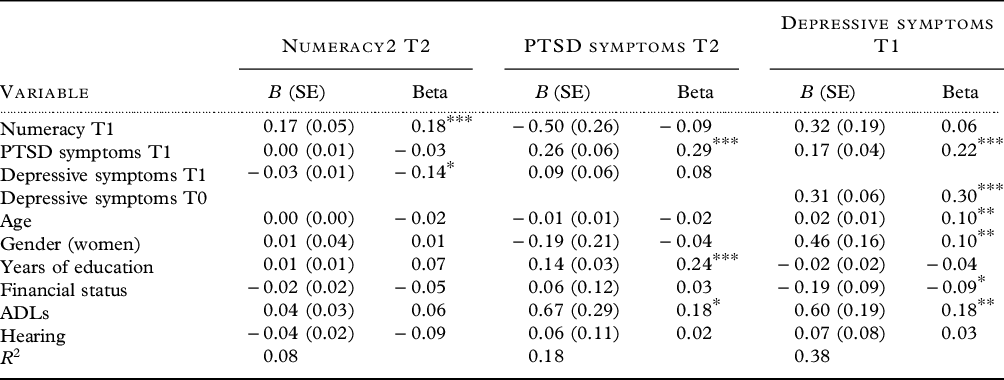
*p < 0.05; **p < 0.01; ***p < 0.001.
Discussion
In this study, we addressed three issues. First, using a longitudinal cross-lagged design, we showed that T1 PTSD symptoms were related to T2 recall memory and fluency (working memory), while the opposite direction was not significant. Second, we showed that only these two tasks were impaired, but not numeracy, a cognitive task that does not depend on neuroanatomical regions involved in the PTSD circuit. Third, we showed that depressive symptoms mediated this PTSD cognition link so that PTSD symptoms were related to depressive symptoms, which in turn were related to impaired cognition, even beyond the PTSD circuit, that is, numeracy.
The directionality of PTSD symptoms and cognitive impairments is highly important. Primarily, on a theoretical level, as results reveal that in older adults PTSD symptoms are linked to subsequent cognitive decline (Vasterling et al., Reference Vasterling, Duke, Brailey, Constans, Allain and Sutker2002). Such results can potentially support the aforementioned allostatic load theory (e.g. McEwen, Reference McEwen1998), whereby experiencing stress and suffering its wear and tear can ultimately lead to cognitive decline (Juster et al., Reference Juster, McEwen and Lupien2010). In fact, a study showed that PTSD endured over four decades ago in prisoners of war can lead to cognitive decline (Aloni et al., Reference Aloni2018). Such results are especially critical in older adults, who anyway face increased risks of cognitive decline as a function of aging, even without PTSD (e.g. Cabeza et al., Reference Cabeza2018). Following, such results of directionality may aid in enhancing cognition by encouraging interventions designed to ameliorate PTSD symptoms. This implication should be underscored, as not only may cognition be enhanced, but perhaps the deleterious effect of PTSD leading to dementia can be decreased (Desmarais et al., Reference Desmarais2020). Our paper adds to recent literature by strengthening the indications that PTSD symptoms may indeed be a risk factor for increased late-life cognitive decline (Palmer, Reference Palmer2021; Rutter et al., Reference Rutter, Vahia, Passell, Forester and Germine2021). To better understand these results, we examined the added contribution of the associations of interest to the explained variance of cognitive function. We especially focused on the combined effects of PTSD and depression which are more robust and clinically relevant than either condition alone. We found that these effects range between 2% and 4%, when also taking into account the covariates. These effects could be considered clinically significant, since old age is characterized by cognitive decline and every percentage of decline can manifest in worse functioning. These findings may suggest that interventions to reduce PTSD and depressive symptoms could produce clinically significant effects due to the increased risk and adverse consequences of cognitive decline in old age.
The second finding concerned the extent of impairments. Previous studies have shown that memory and executive functions are impaired among persons with PTSD (Schuitevoerder et al., Reference Schuitevoerder2013), yet these studies typically sampled persons in health care (Scott et al., Reference Scott2015). In addition, these studies were also typically cross-sectional; thus, it may be possible that certain cognitive impairments already existed and were not truly associated with PTSD. The current results reveal that PTSD directly predicted cognitive decline in tasks related to the PTSD circuit (Jacob et al., Reference Jacob, Dodge and Vasterling2019), namely memory (hippocampus) and fluency which depend on executive functions (prefrontal cortices). Yet the numeracy task − which is unrelated to these neuroanatomical regions but rather with the parietal lobes (Arsalidou et al., Reference Arsalidou2018) − was not directly predicted by PTSD symptoms.
The third finding suggests primarily that depression is a mechanism that partly drives the PTSD cognition link. As stated above, although this was partially demonstrated in previous studies with younger and middle-aged participants (Dretsch et al., Reference Dretsch, Thiel, Athy, Irvin, Sirmon‐Fjordbak and Salvatore2012; Ritchie et al., Reference Ritchie2021), here we show that trauma-related depression (net of earlier depression) mediated this link in older adults. Furthermore, even numeracy, where performance was not directly related to PTSD symptom levels, was impaired when PTSD symptoms were associated with elevated depressive symptoms. Such a finding suggests that cognitive tasks unrelated to PTSD may be impaired following elevated depressive symptoms which are related to PTSD. This finding is important since even though 50% of those with PTSD show such depression (Flory and Yehuda, Reference Flory and Yehuda2015), PTSD researchers typically lump together PTSD-only individuals along with PTSD-with-depression individuals (see Shrira and Hoffman, Reference Shrira and Hoffman2021). Accordingly, our findings may indicate a separate profile for those with PTSD alone, where impairment could be observed only in cognitive tasks related to the PTSD circuit, and individuals whose PTSD led to depression, in which case the profile of cognitive impairment will be more extensive, beyond the PTSD circuit.
This study has several strengths, such as its ample sample size of older adults exposed to warfare trauma and its longitudinal cross-lagged nature. A potential limitation is the limited number of cognitive tasks. Although these tasks allowed for an examination of both mechanisms (global vs. PTSD circuit), future research should assess a wider set of cognitive tasks. Such a wider set should include additional and more specific measures of tasks that activate different brain regions, including the prefrontal and parietal lobes, as well as tasks that involve various functions such as executive control and working memory. An additional limitation is assessing only two waves. Although, two waves of data allow for some measurement of longitudinal processes by separating the temporal order of PTSD and subsequent cognitive function, three waves of data could have provided more insight into the temporal dynamics of the mediation processes. In relation to this point, we did not have a measure of depressive symptoms between T1 and T2. To accommodate for this limitation, we controlled for depression at T0. We also note the low level of depressive symptoms (2 in a range of 0–12), although that is expected in a community-based sample (Ayalon, Reference Ayalon2016; Schwartz and Litwin, Reference Schwartz and Litwin2017). An additional limitation is that we only examined warfare-related PTSD. Future studies could address additional sources of trauma. We also note that there is high comorbidity between PTSD and traumatic brain injury (TBI). While the exclusion criteria include participants who reported an “organic brain syndrome,” this is a large category, and people with significant TBI might not always be reliable in reporting history of TBI. Thus, future studies of trauma and cognition should include a more direct assessment of TBI.
In summary, this study found that PTSD symptoms were associated with future cognitive performance; cognitive performance was not related to future PTSD symptoms. The study further indicated that these effects were partly mediated by trauma-related depressive symptoms. These findings highlight the need to treat PTSD symptoms, since if they are not untreated, they could be related to subsequent cognitive impairment. These findings further stress the importance of distinguishing between adults with PTSD-only and those with PTSD who went on to develop depression, as these distinctions can have different implications for cognitive impairment.
Conflict of interest
None.
Description of authors’ roles
E. Cohn-Schwartz designed the study, built the data set, carried out the statistical analysis, and wrote the paper. Y. Hoffman designed the study and wrote the paper. A. Shrira designed the study, gave critical comments, and edited the paper.
Acknowledgements
This paper uses data from SHARE Waves 5 and 6 (DOIs: 10.6103/SHARE.w5.700, 10.6103/SHARE.w6.700). The SHARE data collection has been funded by the European Commission through FP5 (QLK6-CT-2001-00360), FP6 (SHARE-I3: RII-CT-2006-062193, COMPARE: CIT5-CT-2005-028857, SHARELIFE: CIT4-CT-2006-028812), FP7 (SHARE-PREP: GA N°211909, SHARE-LEAP: GA N°227822, SHARE M4: GA N°261982), and Horizon 2020 (SHARE-DEV3: GA N°676536, SERISS: GA N°654221), and by DG Employment, Social Affairs & Inclusion. Additional funding from the German Ministry of Education and Research, the Max Planck Society for the Advancement of Science, the US National Institute on Aging (U01_AG09740-13S2, P01_AG005842, P01_AG08291, P30_AG12815, R21_AG025169, Y1-AG-4553-01, IAG_BSR06-11, OGHA_04-064, HHSN271201300071C), and from various national funding sources is gratefully acknowledged (see www.share-project.org).
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/S1041610222000357.







