People with mental disorders suffer high rates of mortality due to physical illnesses, including ischaemic heart disease (IHD) (Reference Harris and BarracloughHarris & Barraclough, 1998). IHD mortality has been in steady decline in Australia over the past 20 years, owing to the success of public health campaigns aimed at reducing risk factors, and the introduction of new treatments (Reference Beaglehole, Stewart and JacksonBeaglehole et al, 1997). Have people with mental illness also benefited from these interventions and participated in the favourable trends? We examined this question in a large population-based record-linkage study. We used the Western Australian Health Services Research Linked Database (WA Linked Database) to measure mortality rates, hospital admission rates and revascularisation procedure rates in a geographically defined population of people with diagnosed mental illness, and to compare these rates with those in the general population.
METHOD
Data sources and case selection
The WA Linked Database was used as the source of data. It links together records of all private and public hospital separations (patient discharges, transfers to another facility or deaths), contacts with state mental health services (including public out-patient clinics), death registrations and several other sets of health data for the entire state of Western Australia (Reference Holman, Bass and RouseHolman et al, 1999). Three files were extracted from the WA Linked Database for this analysis. The first file contained all records for any person who had been in contact with mental health services in Western Australia during 1966-1998. The second file contained all records for any person admitted to an acute hospital with selected cardiovascular conditions during 1980-1998. The selection was based on primary diagnoses, which were coded using ICD—9 (World Health Organization, 1977a ). The following conditions were selected: IHD (ICD—9 410-414), hypertensive disease (401-405), cerebrovascular disease (430-438) or peripheral vascular disease (443). The third file contained all records for any person admitted for a revascularisation procedure in Western Australia during 1980-1998. Procedures were classified using the International Classification of Procedures in Medicine (ICPM) (World Health Organization, 1977b ) until 1987, and using the clinical modification of the Ninth Revision of the International Classification of Diseases (ICD—9—CM) (National Coding Centre, 1996) from 1988 onwards. Procedures selected were removal of coronary artery obstruction (ICPM 5-363; ICD—9—CM 36.0) and coronary artery bypass graft or arterial implant (ICPM 5-361, 5-362; ICD—9—CM 36.1-36.9). Each file provided data on acute hospital admissions, death records, psychiatric in-patient movements and contacts with community-based psychiatric services.
Classification of mental disorders
Principal psychiatric diagnoses were assigned from the records of contacts with mental health services. The Mental Health Information System (MHIS) is a core component of the WA Linked Database. The MHIS records separate diagnoses for each contact with mental health services using ICD—9. The final diagnosis was extracted for each episode of care. The latest informative psychiatric diagnosis across the episodes was then assigned as the principal psychiatric diagnosis for each patient according to the following hierarchy of diagnoses:
-
(a) ICD—9 290, 293-296: dementia, organic psychotic conditions, schizophrenia and affective psychosis;
-
(b) ICD—9 291-292, 297-305, 313-315: alcohol and drug psychoses, paranoid states, other non-organic psychoses, neurotic disorders, personality disorders, sexual deviations, alcohol and drug dependence, childhood disorders;
-
(c) ICD—9 306-312, 317-319: adjustment reaction, reaction to stress, depressive disorders not elsewhere classified, conduct disorders not elsewhere classified, special syndromes not elsewhere classified, mental retardation;
-
(d) non-chapter 5 (Mental Disorders) diagnoses.
For instance, if the last episode of care recorded a diagnosis of alcohol dependence, but the previous episode recorded schizophrenia, then a diagnosis of schizophrenia was assigned. The purpose of this strategy was to give precedence to the more severe disorders, and to allow for certain conditions such as alcohol or drug dependence to be considered as a potential comorbidity of a psychotic condition. More than 70% of people on the MHIS had only one diagnosis recorded (at the level used in this study). Of the remaining cases there were three main groups: those who had a less-specific diagnosis (such as depressive disorder not elsewhere classified) together with a more-specific diagnosis (such as neurotic depression); those who had an alcohol/drug condition as well as a psychotic condition; and those for whom the specific type of psychosis had been refined after further observation (particularly between schizophrenia and affective psychosis). The hierarchical approach was designed to select the most appropriate diagnosis in these cases.
Statistical methods
Age-standardised rates of mortality from IHD were calculated for the general population, and for people who had contact with mental health services. Direct standardisation was used (Reference RothmanRothman, 1986), with the Western Australian population used as the standard (Australian Bureau of Statistics, 1980-1998). For population rates, the denominators were calculated from estimated resident population figures published by the Australian Bureau of Statistics (Australian Bureau of Statistics, 1980-1998). Among users of mental health services, calculation of mortality rates was restricted to 165 699 patients whose first contact with mental health services occurred during 1980-1998, excluding 44 430 patients with previous contact. This was done to avoid the results being biased by the healthy-survivor effect. The start of follow-up was the date of each patient's first contact with mental health services. They were then censored either at death or on 31 December 1998. Rates were calculated by principal psychiatric diagnosis and gender. Rates were also calculated separately for each year in the study period. Rate ratios were calculated comparing the cohort of users of mental health services with the entire Western Australian population. For each rate and rate ratio, 95% confidence intervals were calculated.
Rates of first hospital admission and rates of vascularisation procedures were calculated in a similar fashion. The only difference was that the full cohort of 210 129 patients was used, as there was no evidence of a healthy-survivor bias. Rates were also calculated restricted to the inception cohort but, as there was no evidence of any differences, results shown here are from the analysis of the full cohort (which has greater statistical power). Rates were restricted to the first admission for each patient during 1980-1998, and follow-up began on 1 January 1980 for patients whose first contact with mental health services occurred before 1980. When examining individual heart conditions and procedures, calculations were made separately for each condition and individual patients could contribute to more than one condition if they had separate admissions for separate conditions. Patients were censored at time of admission or procedure, or on 31 December 1998.
Poisson regression was used to analyse trends in IHD mortality. Poisson regression models the relationship between counts of events (in this case, deaths) and a set of explanatory variables (in this case, age and year). Separate models were run for each gender for both the cohort of users of mental health services and the total Western Australian population.
RESULTS
There were 44 767 deaths due to IHD during 1980-1998. Of these deaths, 3796 occurred in users of mental health services. The standardised mortality rate was almost twice as high in users of mental health services than in the overall population (Table 1). The majority of deaths (59%) were ascribed to acute myocardial infarction (ICD—9 410.9); however, the mortality rate ratio was higher for other IHD (most of these deaths were coded to coronary atherosclerosis, ICD—9 414.0, or unspecified chronic ischaemic heart disease, ICD—9 414.9).
Table 1 Observed and expected number of deaths and mortality rate ratios from ischaemic heart disease in users of mental health services
| Cause of death (ICD-9 code) | Males | Females | ||||
|---|---|---|---|---|---|---|
| Observed | Expected | Mortality rate ratio (95% CI) | Observed | Expected | Mortality rate ratio (95% CI) | |
| Acute myocardial infarction (410) | 1109 | 637 | 1.74 (1.64-1.85) | 1129 | 652 | 1.73 (1.63-1.84) |
| Other IHD (411-414) | 757 | 341 | 2.22 (2.06-2.39) | 801 | 362 | 2.21 (2.05-2.38) |
| Total IHD (410-414) | 1866 | 977 | 1.91 (1.82-2.00) | 1930 | 1016 | 1.90 (1.81-1.99) |
There has been a steady decline in the mortality rate due to IHD in the Western Australian population overall during 1980-1998, dropping from 209 per 100 000 person-years to 143 per 100 000 person-years in males, and from 139 per 100 000 person-years to 117 per 100 000 person-years in females. In contrast, the IHD mortality rate over the period has remained approximately constant in male psychiatric patients (an average 280 per 100 000 person-years) but increased from 153 per 100 000 person-years to 234 per 100 000 person-years in female psychiatric patients (Fig. 1).
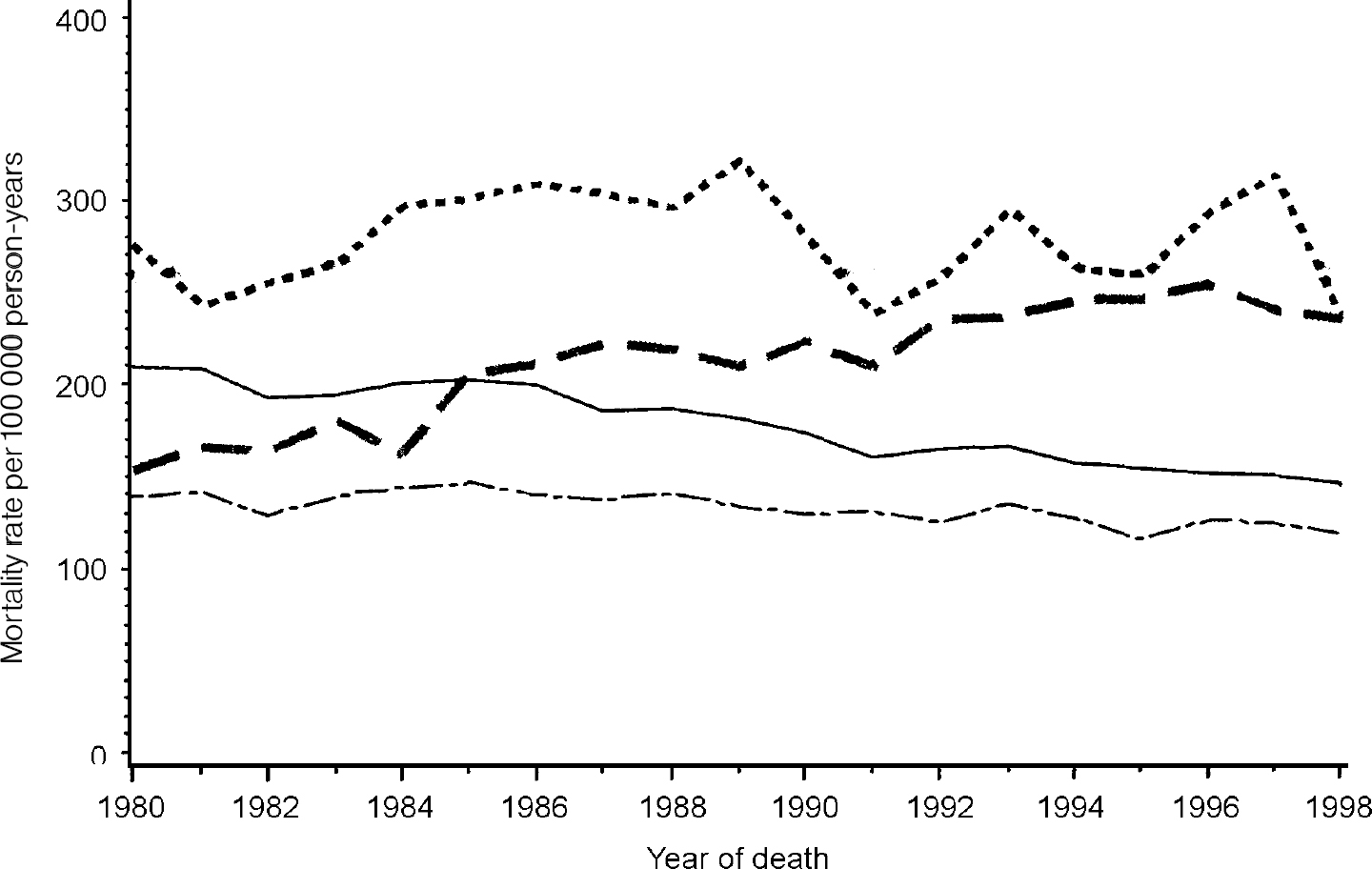
Fig. 1 Ischaemic heart disease mortality rates in Western Australia 1980-1998, total population rates (— males; -—- females) and rates in mental health service users ([UNK], males; — — —, females).
Poisson regression analysis of the mortality rates found that, in the Western Australian population, the mortality rate had been decreasing by 1.9% per year (95% CI 1.7-2.1%) in males and by 0.7% per year in females (95% CI 0.5-1.0%). In contrast, in users of mental health services the mortality rate was not significantly changed in males (95% CI for annual increase -0.5% to 0.9%), and was increasing at a rate of 2.2% per year in females (95% CI 1.5-3.0%).
Whereas psychiatric patients had higher mortality rates, the age-standardised rates of first hospital admission of psychiatric patients for IHD were little different from those in the general population (Table 2). The number of first hospital admissions for acute myocardial infarction was close to that expected for males but lower than expected for females. Rates significantly higher than expected were observed for other acute and subacute IHD, and marginally elevated rates for angina pectoris. The rate of hospital admissions for coronary atherosclerosis was slightly but significantly down in male psychiatric patients, and there was a small but statistically significant elevation in female psychiatric patients.
Table 2 Observed and expected number of patients admitted to hospital for ischaemic heart disease in users of mental health services
| Principal diagnosis (ICD—9 code) | Males | Females | ||||
|---|---|---|---|---|---|---|
| Observed | Expected | Admission rate ratio (95% CI) | Observed | Expected | Admission rate ratio (95% CI) | |
| Acute myocardial infarction (410) | 1236 | 1314 | 0.96 (0.91-1.01) | 1187 | 1273 | 0.93 (0.87-0.99) |
| Other acute & subacute IHD (411) | 997 | 742 | 1.34 (1.25-1.44) | 954 | 649 | 1.47 (1.37-1.57) |
| Angina pectoris (413) | 1426 | 1294 | 1.10 (1.04-1.17) | 1396 | 1120 | 1.25 (1.17-1.32) |
| Coronary atherosclerosis (414.0) | 1173 | 1292 | 0.91 (0.85-0.97) | 633 | 544 | 1.16 (1.07-1.27) |
| Other IHD (412, 414.1-414.9) | 428 | 394 | 1.09 (0.99-1.21) | 349 | 268 | 1.30 (1.16-1.46) |
| Total (410-414) | 3440 | 3471 | 0.99 (0.95-1.02) | 2984 | 2710 | 1.10 (1.06-1.15) |
Mortality and first hospital admission rates for IHD relative to the general community are shown in Table 3 by principal psychiatric diagnosis. Patients with dementia experienced the highest excess mortality, followed by patients with other psychoses. In males, elevated mortality rates were observed in all diagnostic groups except personality disorders, adjustment disorder and non-specific diagnoses. However, only males with neurotic disorder and attempted self-harm had elevated rates of hospital admission for IHD. Males with schizophrenia were only 60% as likely to be admitted for IHD compared with males in the general population, despite being 1.8 times as likely to die from IHD. A similar pattern of excess mortality was observed in females, with the exception of females with schizophrenia. For patients with neurotic disorders, significantly elevated hospital admission rates were observed, together with correspondingly elevated mortality rates. For most other conditions, including dementia, alcohol and drug disorders, schizophrenia and other psychoses, personality disorders and depressive disorder, the mortality rate ratio was markedly higher than the hospital admission rate ratio.
Table 3 Standardised mortality rate ratios and standardised hospital admission rate ratios for ischaemic heart disease comparing users of mental health services with the general community, by principal psychiatric diagnosis
| Principal psychiatric diagnosis | Males | Females | ||
|---|---|---|---|---|
| Mortality rate ratio (95% CI) | Admission rate ratio (95% CI) | Mortality rate ratio (95% CI) | Admission rate ratio (95% CI) | |
| Dementia | 4.48 (3.09-6.49) | 0.76 (0.46-1.25) | 2.88 (2.56-3.23) | 1.15 (0.68-1.95) |
| Alcohol/drug disorders | 1.57 (1.38-1.79) | 0.94 (0.87-1.02) | 1.75 (1.38-2.22) | 1.01 (0.86-1.19) |
| Schizophrenia | 1.78 (1.21-2.61) | 0.59 (0.49-0.71) | 0.86 (0.50-1.49) | 0.60 (0.47-0.76) |
| Affective psychosis | 1.58 (1.32-1.90) | 1.00 (0.89-1.13) | 1.35 (1.13-1.60) | 1.06 (0.95-1.18) |
| Other psychoses | 2.47 (2.15-2.85) | 0.90 (0.75-1.07) | 2.85 (2.54-3.19) | 0.96 (0.81-1.13) |
| Neurotic disorder | 1.36 (1.16-1.59) | 1.34 (1.25-1.45) | 1.23 (1.08-1.41) | 1.46 (1.36-1.56) |
| Personality disorder | 1.22 (0.73-2.04) | 1.06 (0.86-1.31) | 1.37 (0.71-2.61) | 0.95 (0.67-1.34) |
| Adjustment disorder | 0.96 (0.69-1.34) | 0.94 (0.75-1.17) | 0.67 (0.46-0.97) | 1.07 (0.87-1.33) |
| Depressive disorder | 1.81 (1.50-2.19) | 1.12 (0.94-1.34) | 1.87 (1.60-2.18) | 1.25 (1.08-1.45) |
| Other mental disorders | 1.57 (1.27-1.95) | 1.03 (0.90-1.18) | 1.26 (0.95-1.66) | 1.26 (1.07-1.49) |
| Attempted self-harm | 1.72 (1.32-2.24) | 1.24 (1.04-1.47) | 1.55 (1.11-2.17) | 1.34 (1.10-1.64) |
| Non-specific diagnoses | 1.02 (0.83-1.25) | 0.96 (0.84-1.08) | 1.38 (1.13-1.69) | 1.01 (0.88-1.17) |
| Total | 1.91 (1.82-2.00) | 0.99 (0.95-1.02) | 1.90 (1.81-1.99) | 1.10 (1.06-1.15) |
Of IHD deaths, 13% occurred within 28 days of admission for acute myocardial infarction. The 28-day case fatality rate was directly comparable between people with previous contact with mental health services (12.2% mortality) and the remainder of the population (13.0% mortality). The excess mortality from IHD in psychiatric patients occurred outside the hospital environment. In those who survived for at least 28 days following admission for acute myocardial infarction, longer-term survival was worse in psychiatric patients (12% mortality after 2 years, compared with 7% mortality in the remainder of the population).
During 1980-1998, there were 30 593 hospital admissions for revascularisation procedures (17 348 for coronary artery bypass grafts and 13 245 for removal of coronary artery obstructions), representing 23 900 individual patients. Of these patients, 1807 had previous contact with mental health services. First hospital admission rates for revascularisation procedures were lower than expected in male psychiatric patients, and about what was expected in females (Table 4). Slightly lower rate ratios were observed for coronary artery bypass grafts compared with removal of coronary artery obstructions. Procedure rates were significantly lower in males with dementia, alcohol/drug disorders, schizophrenia, affective disorder and other psychosis, and in females with schizophrenia. Patients with neurotic disorders had elevated rates of revascularisation procedures.
Table 4 Revascularisation procedure rate ratios (95% CIs) comparing users of mental health services with the general community, by procedure type and principal psychiatric diagnosis
| Males | Females | |
|---|---|---|
| Procedure type | ||
| Removal of coronary artery obstruction | 0.85 (0.78-0.93) | 0.98 (0.87-1.11) |
| Coronary artery bypass graft or arterial implant | 0.75 (0.70-0.80) | 0.90 (0.81-1.01) |
| Principal psychiatric diagnosis | ||
| Dementia | 0.14 (0.07-0.26) | 0.53 (0.16-1.74) |
| Alcohol/drug disorders | 0.60 (0.52-0.68) | 0.86 (0.61-1.21) |
| Schizophrenia | 0.31 (0.21-0.45) | 0.34 (0.18-0.64) |
| Affective psychosis | 0.77 (0.64-0.93) | 0.79 (0.62-1.01) |
| Other psychoses | 0.66 (0.48-0.91) | 0.79 (0.52-1.20) |
| Neurotic disorder | 1.21 (1.09-1.35) | 1.28 (1.12-1.46) |
| Personality disorder | 0.97 (0.72-1.31) | 0.90 (0.50-1.65) |
| Adjustment disorder | 1.06 (0.79-1.41) | 1.12 (0.76-1.66) |
| Depressive disorder | 0.86 (0.64-1.15) | 0.85 (0.60-1.20) |
| Other mental disorders | 0.98 (0.81-1.19) | 1.05 (0.75-1.47) |
| Attempted self-harm | 1.04 (0.80-1.35) | 1.31 (0.91-1.88) |
| Non-specific diagnoses | 0.83 (0.69-1.00) | 0.94 (0.72-1.25) |
DISCUSSION
Mortality rates from IHD were high and have been increasing in users of mental health services. IHD was the leading cause of excess mortality in users of mental health services (accounting for 16% of all excess deaths, compared with 8% of excess deaths due to suicide). By contrast, the rate of hospital admission was practically no different from that in the general community, suggesting that case fatality is a major issue in this group. Revascularisation procedure rates were low, particularly in patients with psychoses, raising questions of access to services and equity of service provision.
Risk factors for cardiovascular disease
Risk factors for cardiovascular disease include family history, smoking, poor diet, high cholesterol, obesity, lack of exercise and stress levels. The 1997 National Survey of Mental Health and Wellbeing found that 43% of Western Australians with a diagnosable mental health condition were current smokers, compared with 24% among people without a mental disorder (Australian Bureau of Statistics, 1999). The prevalence of smoking was even higher among patients with psychosis, at 66% (Reference Jablensky, McGrath and HerrmanJablensky et al, 1999). Obesity is known to be a problem among people with chronic mental illness (Reference Wallace and TenantWallace & Tenant, 1998) and has been linked to overeating, underactivity and ignorance of correct dietary principles (Reference Gopalaswamy and MorganGopalaswamy & Morgan, 1985; Reference McCreadie, MacDonald and BlacklockMcCreadie et al, 1998). Weight gain is also a known side-effect of some antipsychotic medications (Reference Silverstone, Smith and GoodallSilverstone et al, 1988; Reference Allison, Mentore and HeoAllison et al, 1999). Lower levels of physical fitness have also been found in mental illness, linked to physical inactivity (Reference MartinsenMartinsen, 1990).
Trends in cardiovascular mortality
The rates of cardiovascular mortality in the general population of Western Australia have been in steady decline over the period from 1980 to 1998. Whereas public health campaigns and the introduction of new therapies have been shown to be very successful in the general population, it would appear that people with mental illness have received little or no benefit from this progress. Over the same period, cardiovascular mortality rates have increased in women known to mental health services and have remained approximately constant in men. The evidence cited above concerning cardiovascular risk factors in mental illness suggests that health campaigns targeted at these risk factors have had no impact in this population. Users of mental health services are a significant group numerically, representing 8% of the adult population of Western Australia. Therefore, public health and clinical strategies specifically targeted towards this group should be developed.
Psychiatric patients had a higher death rate from acute myocardial infarction than did the general community, although the rate of hospital admission was no higher than expected in males and marginally lower than expected in females. Outcomes following acute myocardial infarction are affected by how quickly emergency treatment can be administered. The lower rates of hospital admission could be due to the fact that psychiatric patients with acute myocardial infarction died before they could be admitted to a hospital emergency department. It is possible that some psychiatric conditions, such as schizophrenia, may interfere with effective communication of symptoms. In critical conditions such as acute myocardial infarction, this may result in a delay of treatment that contributes to excess mortality. Social isolation could also be an issue, as people with chronic mental disorders are more likely to live alone, in a hostel or even to be homeless. Consequently, they are more likely to be alone at the time of an infarction and therefore to lack assistance.
There are other factors that may contribute to a high rate of coronary events in this group of patients. People with mental illness may experience an elevated risk of acute coronary events due to causes of fatal arrhythmias such as heavy smoking and possibly certain psychopharmacological agents (Reference GlassmanGlassman, 1998; Reference Appleby, Shaw and AmosAppleby et al, 2000). Considering the tentative evidence that antipsychotic polypharmacy may be associated with reduced survival (Reference Waddington, Youssef and KinsellaWaddington et al, 1998), there is a need for further research into the cardiotoxic effects of pharmacotherapy in psychiatry.
Mental illness and general health care
Although hospital admission rates for some ischaemic heart conditions were mildly elevated in users of mental health services compared with general population rates, the excess of mortality was considerably higher than the excess of hospital admission. This raises the question of whether, in spite of their rate of hospital admission, psychiatric patients are actually receiving the same level of care, relative to clinical need, that is afforded the general community for circulatory system disorders. Rates of revascularisation procedures were low considering the high rate of mortality. The results imply that people with mental illness are not receiving these interventions at a level matching that in the general population.
Druss et al (Reference Druss, Bradford and Rosenheck2000) found lower rates of cardiovascular procedures undertaken in an index admission for acute myocardial infarction if the patient had a mental disorder recorded as a comorbidity. Our results confirm in a large population-based record-linkage study that the total cardiovascular procedure rate in users of mental health services is very low relative to their heavy burden of cardiovascular morbidity and mortality, although this varies by diagnosis.
When examining procedure rates by diagnosis, it is clear that patients with schizophrenia have a much lower rate of cardiovascular procedures, even though these patients have among the highest levels of smoking, obesity and other cardiovascular risk factors. Is it possible that circulatory system disorders are underdiagnosed in mental illness, contributing to the large excess in mortality? There is some indirect evidence to support this conjecture. It is known that mental health services can miss physical conditions in their patients (Reference KoranyiKoranyi, 1979; Reference Koran, Sox and MartonKoran et al, 1989), and that not all psychiatrists undertake physical examinations of their patients (Reference McIntyre and RomanoMcIntyre & Romano, 1977; Reference PattersonPatterson, 1978). Moreover, Kendrick (Reference Kendrick1996) reported that in a survey of general practices he found that cardiovascular risk factors were regularly recorded in the notes for adults with long-term mental illness, but that the general practitioners had rarely attempted to intervene.
Stigma
Patients with neurotic disorders have a higher than average rate of revascularisation procedures, possibly because they comprise a subset of individuals with anxiety or somatisation disorders who are more likely to seek specialist consultation, or because the pressure of the physical symptoms of heart disease may be more difficult for individuals whose mechanisms of coping with stress are already challenged. In contrast, patients with schizophrenia are clearly disadvantaged regarding access to such treatment. These findings concerning the standard of health care provided to people with mental illness raise the question of whether the stigma associated with mental illness extends beyond the general community into the medical profession. Although implicit stigmatising attitudes on the part of providers of specialist care may play a role (Reference HaghighatHaghighat, 2001), the disparity in service provision may also be due to socio-economic factors. The majority of revascularisation procedures are performed as elective interventions to which carriers of private health insurance have readier access than people covered only by Medicare (the Australian national health service). Considering that, in Australia, only 13% of people with psychotic disorders have private health insurance, as compared with an average of 32% for the general population (Reference Jablensky, McGrath and HerrmanJablensky et al, 1999), the compound predicament of this group of psychiatric patients deserves further study, to develop health care policy and interventions to reduce these inequalities.
Given that the excess risk of heart disease rather than the excess risk of suicide is the leading killer of people with mental illness, mental health services should adopt a more proactive role in identifying patients with cardiovascular problems and referring them for early intervention. People with mental illness may benefit also if general practitioners have a greater role in their primary medical care.
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
▪ People with mental illness are at high risk of death due to heart disease.
-
▪ Despite the high mortality, hospital admissions for heart disease are no more common in people with mental illness than in the general community, whereas procedural interventions are much less frequently conducted.
-
▪ Greater attention needs to be paid to the general medical care of people with mental illness.
LIMITATIONS
-
▪ Information on risk factors for individuals, such as smoking, was not available.
-
▪ Clinical diagnoses were those recorded on the mental health information system, not research diagnoses.
-
▪ Detailed clinical information was not available on the mental health information system.








eLetters
No eLetters have been published for this article.