With great interest, we have read the letter by Rayman and Calder recently published in the British Journal of Nutrition (Reference Rayman and Calder1). In that letter, the importance of an optimal nutritional adequacy to optimise the efficacy of the COVID-19 vaccine was emphasised. In that respect, older subjects were mentioned as a target group, as they are characterised by a weakened immune response, as shown by poor responses to several vaccines, amongst others the Oxford COVID-19 vaccine(Reference Ramasamy, Minassian and Ewer2). Since it has been suggested that poor vaccination responses in older people are related to deficiencies in minerals and vitamins, Rayman and Calder suggested that nutritional supplements containing different vitamins and minerals should be provided to all subjects aged 70 years and older for a period of week before and after they get vaccinated.
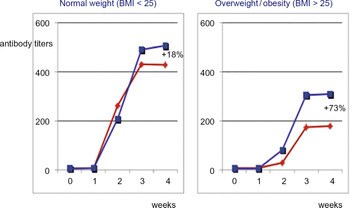
Besides older people, there is also another group at risk with a poor vaccination response: people with overweight or obesity(Reference Sheridan, Paich and Handy3–Reference Tagliabue, Principi and Giavoli5). In fact, a recent trial showed that the response to the COVID-19 vaccination of BioNTech/Pfizer was also impaired for people with a higher BMI(Reference Pellini, Venuti and Pimpinelli6). More specifically, the antibody response was more efficient in under-weight and normal-weight groups v. the pre-obesity and obesity groups (P < 0·0001). This association was confirmed after adjusting for age (P = 0·003). There was even a significant relation between four BMI classes and antibody titters (p = 0·02). It is possible that improving nutritional status would strengthen the immune response of subjects with overweight and obesity, since they often do not have an optimal nutritional status because of low dietary quality. However, based on our earlier studies, we suggest to consider also an alternative intervention. In an earlier double-blind placebo-controlled human intervention study in asthma patients, we found that 4-week consumption of plant stanol ester enriched foods prior to vaccination as well as 4 weeks after vaccination, significantly increased IgG antibody titters against hepatitis A (antiHAV titters) in response to a hepatitis A vaccination, while IgE levels decreased(Reference Brüll, Desmet and Mensink7). Antibody titters in overweight or obese subjects (BMI > 25 kg/m2) from the control group were at least half of those in normal-weight subjects (BMI < 25 kg/m2), showing that a high BMI indeed compromised the immune response. Moreover, upon plant stanol ester consumption, antibody titters increased by 18 % in normal-weight asthma patients and by 73 % in asthma patients with overweight and obesity. However, antibody titters in the high-BMI group after plant stanol ester consumption were still lower as compared with subjects with normal weight in the control arm (Fig. 1)(Reference Plat, Baumgartner and Vanmierlo8).

Fig. 1. Increase of 73 % in antiHAV titers (IU/l) in the high-BMI plant stanol group (blue line) compared with the high-BMI control group (red line) as compared with an 18 % increase in antiHAV titers (IU/l) in the low-BMI plant stanol group (blue line) v. the low-BMI control group upon hepatitis A vaccination in week 0(Reference Brüll, Desmet and Mensink7,Reference Plat, Baumgartner and Vanmierlo8) .
The suggested underlying mechanism for this effect may relate to effects on T cell behaviour. In more detail, we postulated that effects of plant stanol ester consumption increased the activity of the regulatory T cells, which in asthma patients dampened the Th2 response and improved the Th1 response. Based on these findings, we now hypothesise that people with a higher BMI might particularly benefit from plant stanol consumption several weeks prior and after receiving the COVID-19 vaccination. Therefore, we recently initiated another double-blind placebo-controlled intervention trial to evaluate the effects of a daily intake of 4 g plant stanols as their fatty acid esters in subjects with overweight or obesity (BMI 27–35 kg/m2). This trial was recently approved by our local Medical Ethical Committee (METC 21-013) and registered at http://www.clinicaltrials.gov as NCT04844346. Recruitment and execution have started.
Besides possible effects on T cell behaviour, another mechanism related to plant stanol ester consumption may be worthwhile to explore in the context of COVID-19 exposure. For this, we need to highlight a few recent findings: first, the observation by Lamers et al. (Reference Lamers, Beumer and van der Vaart9) who have shown that the SARS-CoV-2 virus can also enter intestinal cells; second, the work by Wei et al. (Reference Wei, Wan and Yan10) showing that SARS-CoV-2 needs to bind cholesterol to enter the cells via the ACE receptor; and third, the work by Wang et al. (Reference Wang, Li and Hui11) show that replacement of cholesterol in the cell membrane by 25-OH cholesterol hampers the infection rate of the virus. Altogether, these findings show an essential role of cholesterol in the membrane in cellular infection. Moreover, it also suggests that plant stanols, when replacing cholesterol in cell membranes which is plausible in enterocytes, might lower the possibility for the virus to infect enterocytes. This hypothesis of course is currently speculative and needs to be confirmed or refuted by specifically for these purpose-designed studies.