Introduction
Migraine is a prevalent neurobiological disorder characterized by increased central nervous system excitability. Diagnosing migraine involves identifying specific headache characteristics and accompanying symptoms. The primary symptom is a pulsating, severe, typically unilateral headache, often accompanied by increased sensitivity to light and sound, nausea, and vomiting. Migraine attacks, lasting 4 to 72 h, are frequently preceded by visual, auditory, and sensory auras (Amiri et al., Reference Amiri, Kazeminasab, Nejadghaderi, Mohammadinasab, Pourfathi, Araj-Khodaei, Sullman, Kolahi and Safiri2022).
Migraine is one of the most common neurological disorders worldwide. The global prevalence of migraine is estimated to be around 14.7%, affecting approximately one billion people, and it is more common in women than men, with a prevalence rate of 18% and 6% in orderly, likely due to hormonal differences (Gupta & Gaurkar, Reference Gupta and Gaurkar2022). Chronic migraine affects about 1–2% of the world’s population, with 2.5% of episodic migraine cases progressing to chronic migraine, increasing disability and healthcare utilization (Gawde et al., Reference Gawde, Shah, Patel, Bharathi, Patel, Sethi and Kaka2023).
Pharmacological treatments for migraine include a variety of medications designed to alleviate symptoms and reduce the frequency of attacks. Acute treatments aim to relieve pain and include nonsteroidal anti-inflammatory drugs, triptans, and ergotamines. Prophylactic treatments are used to prevent migraines and include beta-blockers, antidepressants (Puledda et al., Reference Puledda, Tassorelli and Diener2023). Despite their effectiveness, these pharmacological therapies have limitations, including side effects, contraindications, and the potential for medication overuse headache. Some patients may also experience inadequate relief or develop tolerance to medications over time, leading to a need for alternative treatment strategies.
Since 1998, researchers have investigated hyperbaric oxygen therapy (HBOT) for treating migraines (Wilson et al., Reference Wilson, Foresman, Gamber and Wright1998). In their 2021 systematic review, Ciarambino et al. reported evidence suggesting that HBOT may help relieve migraine headaches (Ciarambino et al., Reference Ciarambino, Sansone, Menna, Para, Signoriello, Leoncini and Giordano2021). Various studies also indicated that high-flow oxygen therapy (HFOT) for migraine is a safe, effective acute treatment option and may be better tolerated than other treatments (Singhal et al., Reference Singhal, Maas, Goldstein, Mills, Chen, Ayata, Kacmarek and Topcuoglu2017; Schindler et al., Reference Schindler, Wright, Weil, Gottschalk, Pittman and Sico2018).
However, there are significant limitations to the accessibility and feasibility of HBOT and HFOT for migraine treatment. HBOT requires specialized equipment and facilities, making it inaccessible for many patient. HFOT, while more accessible than HBOT, still requires medical-grade oxygen and proper administration, which may not be feasible for all patients. These limitations highlight the need for more accessible and affordable treatment options for migraine management (Wang et al., Reference Wang, Lan, Dandu, Ding, Ji and Meng2023).
Breathing techniques in meditation and yoga have been found to have effects comparable to those of HBOT. A 2017 study found that these techniques can increase arterial oxygenation and activate the parasympathetic system by improving ventilation efficiency (Russo et al., Reference Russo, Santarelli and O’Rourke2017). A 2011 study showed that yoga-based respiratory training could lower breathing rates and increase resting oxygen saturation (Santaella et al., Reference Santaella, Devesa, Rojo, Amato, Drager, Casali, Montano and Lorenzi-Filho2011). Additionally, a 2021 study indicated that slower breathing rates during yoga might reduce sensitivity to hypoxic and hypercapnic reflexes (Santaella et al., Reference Santaella, Devesa, Rojo, Amato, Drager, Casali, Montano and Lorenzi-Filho2011).
A non-invasive technique is alternate nostril breathing (ANB), which improves respiratory function, regulates sympathetic-vagal balance, reduces stress, enhances metabolism, boosts cognitive functions, and mitigates physiological aging (Nivethitha et al., Reference Nivethitha, Mooventhan and Manjunath2016). Regular yoga practice, including ANB, is an excellent exercise for maintaining health across all age groups, beneficial in preventing, controlling, and rehabilitating many diseases.
This study aims to investigate the impact of the ANB technique on the frequency and severity of migraine-type headaches, as well as its effect on migraine-related disability.
Method
Study design
This study is designed as a single-center, open-label, two-arm, parallel-group randomized controlled trial (RCT) conducted at six Family Health Centers (FHCs) of Dokuz Eylul University in different regions of Izmir. This study was reviewed and approved by the Ethics Committee of Izmir Dokuz Eylul University, with the file number 7201-GOA. The trial was registered on 09/09/2022 with the registration number ‘NCT05536635’ in the US NIH clinical trials database.
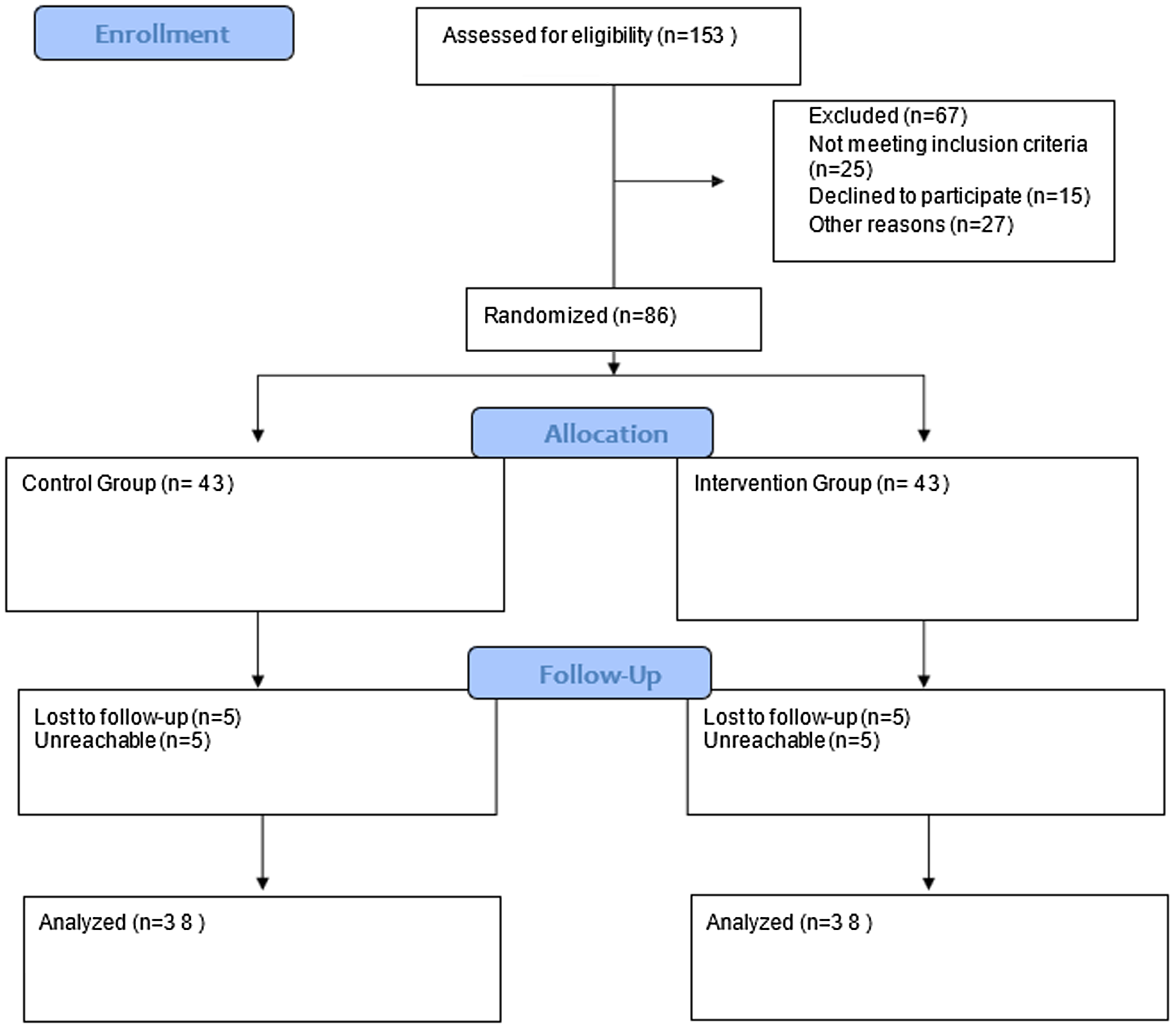
Figure 1. CONSORT diagram.
Population and sample
The study population comprises patients registered at the FHC of Dokuz Eylul University, diagnosed with migraine (International Classification of Diseases, 10th Revision (ICD-10) code G43 and its subcategories), and experiencing migraine attacks less than once every three months.
The sample size was calculated considering a 5% margin of error, 80% power, medium effect size, and a 15% dropout rate, resulting in a required sample size of 86 participants. These participants will be equally divided into control and intervention groups. The sample size was calculated using G*POWER 3.1.9.2.
Inclusion and exclusion criteria
Participants aged 18–50 years, owning an internet-enabled communication device, and willing to participate were included. Eligible participants were required to have a migraine diagnosis with attack frequency of less than three months and meet specific migraine diagnostic criteria. Exclusion criteria included severe anatomical abnormalities of the airway, pregnancy, diagnosed psychiatric disorders, current use of psychiatric medications, and significant speech or hearing problems. Additionally, patients with chronic comorbidities such as diabetes, hypertension, Chronic Obstructive Pulmonary Disease (COPD), asthma, and cardiac diseases were excluded. Only individuals without active complaints, no history of related medication use, and clean records in electronic health systems were considered for inclusion. None of the participants were on prophylactic treatment before the study, and any participants who would have started prophylactic treatment during the study were to be excluded, although this did not occur. Every participant continued their usual treatment, and no interventions were made to alter their pharmacological therapy.
Participant recruitment and randomization
Data were collected through face-to-face interviews conducted between 01.1.2023 and 30.1.2023 at the FHCs of Dokuz Eylul University. Initially, eligible participants from each six different FHCs were listed separately and subsequently selected using a random number generator. The selection conducted to achieve an equal number of participants within each center. These centers were then cluster-randomized into two groups: three were assigned to the intervention group and three to the control group. This cluster randomization process was also performed using a random number generator, and the entire procedure was carried out by the researcher (Figure 1).
Data collection tools
Personal data form
A questionnaire was developed to capture sociodemographic information such as gender, marital status, educational level, employment status, income status, and age.
Migraine Disability Assessment Scale (MIDAS)
Migraine Disability Assessment Scale (MIDAS) assesses the level of disability in migraine patients by evaluating daily life activities affected by migraine attacks. The MIDAS consists of five questions that assess the number of days migraines have impacted various aspects of daily life over the past three months. These include days missed at work or school, days of reduced productivity at work or school, days missed doing household work, days of reduced productivity in household work, and days missed in social or leisure activities. Each question is scored based on the number of days affected, with higher scores indicating greater disability. Additionally, the MIDAS includes questions on headache frequency (number of migraine days) and severity (measured using a Visual Analog Scale, VAS) to provide a comprehensive assessment of the migraine’s impact on the individual’s life. The scale’s Turkish validity and reliability were confirmed by Ertaş et al. in 2004, with a Cronbach’s alpha of 0.76.
Pre-randomization and baseline evaluation
All patients attended an individual session at their respective FHCs, where they received standardized education on migraine management, including topics such as migraine triggers, available treatment options, and recommended lifestyle modifications. This initial education ensured a uniform baseline level of knowledge across participants. Following this, an initial evaluation was conducted individually with both the intervention and control groups to establish a baseline for the study. Participants from both groups completed the required forms in the presence of the researcher, who provided assistance as needed to minimize misunderstandings and potential errors. This approach ensured accuracy and consistency in data collection across both groups.
Intervention
Patients in the intervention group participated in a 30-min, one-on-one session with the researcher at their respective FHCs. During this session, the researcher provided individualized instruction and practice in the ANB technique. The researcher demonstrated the technique and guided each participant through the exercises, ensuring correct understanding and performance. To support ongoing practice and adherence, participants in the intervention group received comprehensive written materials, including step-by-step instructions and additional guidance on the ANB technique (Supplementary Material 1).
Follow-up and outcome
Throughout the study, participants in the intervention group received weekly phone calls to support adherence to the ANB technique. Each weekly call, lasting approximately 5–10 min, focused on the following topics:
Adherence to the exercise regimen and frequency of practice
Correct technique for performing ANB
Addressing any questions or concerns related to the exercise
Encouragement and motivation to continue the practice
Additionally, both the intervention and control groups received monthly phone calls, each lasting 10–20 min, which provided general support and follow-up related to their migraine conditions. Topics covered in these monthly calls included:
Monitoring any changes in migraine frequency, duration, and intensity
General health updates and well-being checks
Guidance on lifestyle or dietary adjustments that may help manage migraines
Emotional and psychological support related to migraine management.
At the end of the three-month period, participants from both groups were contacted by phone, and the MIDAS questionnaire was administered again. The primary outcomes were the changes in headache frequency and severity, as recorded by participants in a diary. Headache frequency was defined as the number of migraine days. Severity was measured using the VAS from 0 to 10. Participants were provided with instructions on how to identify and record migraine-specific headaches. The secondary outcomes focused on changes in the MIDAS score. A migraine day was defined as any day with migraine symptoms. Attacks lasting over 24 h were considered one attack. At the conclusion of the study, the control group was informed about the exercise technique and invited to a session to learn and practice it. There were no complications reported during the study.
Statistical analysis
Dependent variables included pain intensity, pain frequency, and MIDAS score. Independent variables included sociodemographic characteristics and the use of breathing techniques. Data analysis was performed using IBM SPSS Statistics V27.0. Descriptive analyses were conducted for all variables. For comparisons, means and standard deviations were used for continuous variables, and frequencies and percentages for categorical variables. Chi-square tests were used for categorical independent and dependent variables. To test the distributions, the Kolmogorov–Smirnov test was used. The MIDAS scores, which followed a normal distribution, were analyzed using independent t-tests for comparisons between the intervention and control groups and paired t-tests for within-group comparisons. For attack frequency and attack severity, which did not follow a normal distribution, the Mann–Whitney U test was used for between-group comparisons, and the Wilcoxon test was employed for within-group comparisons. Analyses followed the intention-to-treat principle using the multiple imputation method, with a significance level set at p < 0.05.
Results
Baseline findings
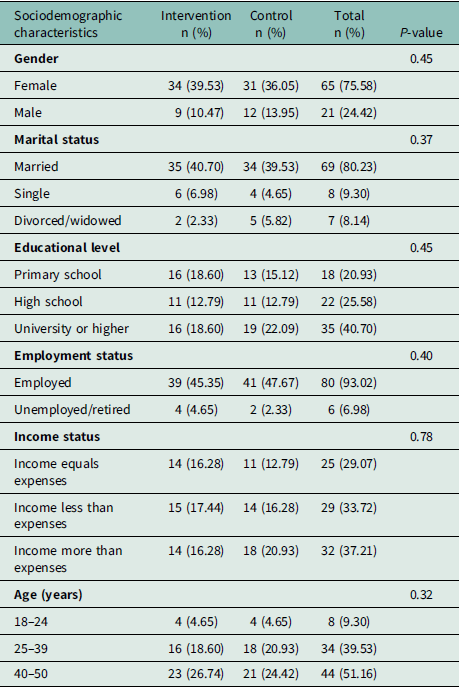
Eighty-six migraine patients aged 18–50 years participated in the study. The mean age of the participants was 39.11 ± 7.21 years, and 51.16% (44 participants) were aged 40–50 years. Among the participants, 75.58% (65 individuals) were female, 80.23% (69 participants) were married, and 40.70% (35 participants) had university-level or higher education, 93.02% (80 participants) were employed, and 33.72% (29 participants) had income less than expenses. There was no statistically difference between the control and intervention groups (Table 1).
Table 1. Sociodemographic characteristics of participants
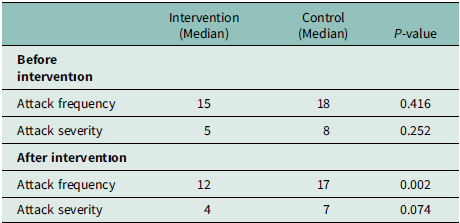
Attack frequency, severity, and MIDAS score
While the frequency and severity of attacks did not follow a normal distribution, the MIDAS score was normally distributed. The median attack frequency was lesser among the intervention groups after the intervention (P = 0.002), while no statistically significant difference was existed before (P = 0.415). There was no statistically significant difference between control and intervention groups neither before nor after the intervention (P-value was equal to 0.252 and 0.074 orderly) (Table 2).
Table 2. Comparison of attack frequencies and severities between groups before and after the ıntervention
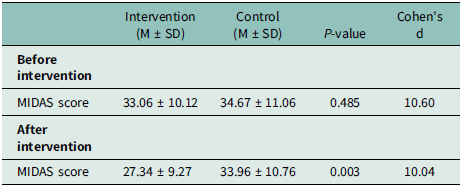
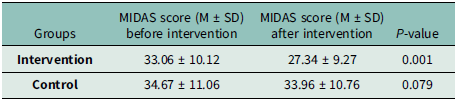
Also MIDAS score was lesser within the intervention group after the intervention (p = 0.003), though there was no statistically significant difference between the groups before (P = 0.484) (Table 3).
Table 3. Comparison of MIDAS scores before and after the ıntervention
Within-group comparisons
Attack frequency, severity and MIDAS score was significantly lower in the intervention group (P = 0.001, P = 0,001, and P = 0,001 orderly) on where as there was no significant change in the control group for attack frequency and MIDAS score before and after intervention (P = 0.589 and P = 0,079 orderly). Only attack severity was decreased within the control group after intervention (P = 0.001) (Table 4, 5).
Table 4. Examination of changes in attack frequencies and severities within groups between the beginning and end
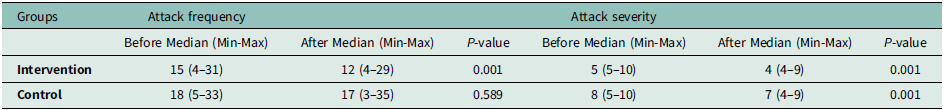
Table 5. Examination of changes in MIDAS scores within groups before and after the ıntervention
Discussion
Our study highlights the importance of using the ANB technique as a non-pharmacological method for managing migraine headaches and its impact on patients’ migraine-related disability. As a non-invasive, non-pharmacological approach, the breathing technique can be easily applied without side effects or additional costs for both practitioners and patients. This technique can be integrated into patients’ daily routines and may have positive effects on migraine control with regular practice.
Relevance of the study group
Migraine prevalence tends to peak around the age of 40 years in both men and women and decreases with age, as supported by studies showing similar age distribution patterns (Piccinini et al., Reference Piccininni, Brinks, Rohmann and Kurth2023). Also it is much prevalent among women (Özdemir et al., Reference Ozdemir, Aygül, Demir, Ozel, Ertekin and Ulvi2014). The average age of participants in our study was 39.11 ± 7.21 years with the number of female participants being three times greater than that of male participants.
According to our study results, the participants’ baseline MIDAS score was 33.87 ± 1.14, with an attack frequency of 17.50 ± 0.68 (over a three-month period) and an attack severity of 8.08 ± 0.17. Medrano Martínez et al. (Reference Medrano Martínez, Francés Pont, Hernández Rubio, González Fernández, Fernández Izquierdo and Mallada Frechin2021) reported a mean MIDAS score of 39.88 and an average attack severity of 7.49, while Guilbot et al. (Reference Guilbot, Bangratz, Ait Abdellah and Lucas2017) found a monthly attack frequency of 4.9. On the other hand, the mean MIDAS score in our study was comparable to national data from Turkey, where the average MIDAS score is 35.32 ± 36.59 (Çimen, Reference Çimen2019). These findings affirm the relevance of our study population, as their characteristics reflect both national and international migraine data. Therefore, while our results are applicable to our study population, caution should be exercised when considering the generalizability of our findings to broader populations, as RCTs are inherently limited to the populations in which they are conducted.
Many studies have reported higher MIDAS scores in patients with comorbid conditions, such as depression (43.0 ± 43.8) (Hans et al., Reference Hans, Stonnington, Zhang, Butterfield and Friedman2023). Also Sengul et al. (Reference Sengul, Sengul, Bakim, Yucekaya, Yucel and Akgun2014) state that higher MIDAS scores correlate with anxiety and sleep disorders. This observation suggests that patients with higher baseline MIDAS scores, potentially associated with comorbid conditions, might respond more favorably to ANB, as ANB has shown improvements in various health conditions and comorbidities (Jahan et al., Reference Jahan, Begum, Akhter, Islam, Jahan, Samad, Das, Rahman and Haque2021). However, further studies are needed to substantiate these findings and explore the extent of ANB’s effectiveness in this context.
Importantly, there were no significant differences between the intervention and control groups in terms of sociodemographic variables, MIDAS scores, attack frequency, or attack severity at baseline. This balance between the groups shows our study’s randomization process, ensuring that the comparison of outcomes post-intervention is methodologically sound.
Outcomes
For our intervention’s effectiveness, it is essential to note that there were no significant differences between the two groups in terms of sociodemographic variables, MIDAS score, attack frequency, and attack severity prior to the intervention. Therefore, no adjustment analysis was necessary for the results obtained.
The intervention group showed a significant reduction in attack frequency post-intervention, while no significant change was observed in the control group. This suggests that ANB effectively reduces the frequency of migraine attacks. The intervention group also exhibited a significant reduction in MIDAS scores, indicating improved daily functioning and migraine-related disability. The control group showed no significant change, underscoring the effectiveness of the breathing technique. But in contrary, there was no significant difference on attack severity between the groups, suggesting that while the intervention may reduce severity, other factors also contribute to this outcome. These findings suggest that the intervention effectively reduces attack frequency and improves MIDAS scores. However, its effect on attack severity was not as pronounced, which may be due to several factors. The intervention may influence the pathways that initiate migraine attacks but not the mechanisms affecting pain intensity. Further research is needed to explore the intervention’s impact on these pathways.
Hypoxia is known to trigger migraine-like and aura attacks by causing arterial dilation (Arngrim et al., Reference Arngrim, Schytz, Britze, Amin, Vestergaard, Hougaard, Wolfram, de Koning, Olsen, Secher, Larsson, Olesen and Ashina2016). ANB may reduce this hypoxic state, potentially decreasing the frequency of migraine attacks. However, it does not seem to affect cortical spreading depression (CSD), the electrophysiological event underlying migraine auras (Kudo et al., Reference Kudo, Nozari, Moskowitz and Ayata2008). This could explain the lack of significant effect on attack severity.
The duration of the intervention may also have been insufficient to affect attack severity. Future studies should consider longer intervention periods to assess sustained effects. Previous studies on alternative migraine treatments have typically involved three-month periods (Fuglsang et al., Reference Fuglsang, Johansen, Kaila, Kasch and Bach2018; Xie et al., Reference Xie, Tian, Hui, Qin, Gao, Zhang, Ma, Suen, Wang, Liu, Hao, Yang and Loke Yuen2022).
Another consideration is that participants may not have performed the ANB technique correctly during an attack, affecting its efficacy on attack severity. Detailed examination of the timing and application of the intervention in future research is necessary.
Both groups showed improvements in attack severity from baseline to post-intervention, which could be attributed to all participants receiving the latest migraine information, while continuing their usual treatment, thereby increasing disease management awareness and resulting in similar improvement potentials in both groups.
These results indicate that patient awareness of migraine symptoms is crucial for effective management. Recognizing trigger factors and taking appropriate measures are vital. Additionally, regular monitoring and appropriate treatment recommendations by healthcare professionals play a critical role in managing migraine symptoms (Rosignoli et al., Reference Rosignoli, Ornello, Onofri, Caponnetto, Grazzi, Raggi, Leonardi and Sacco2022).
This study is the first to investigate the use of ANB in migraine patients, making a significant contribution to the literature.
Limitations and strengths of the study
This study was conducted in a primary care setting, providing insights into how migraine treatment can be implemented within basic health services, which is important for broader patient access. Including participants without comorbidities allows for a more direct interpretation of results concerning migraine itself, minimizing the influence of other health conditions. As one of the first studies to examine the effects of ANB in migraine treatment, it contributes new knowledge to the field. Using cluster sampling reduced the risk of contamination between groups, enhancing the reliability of the results.
The intervention period may have been too short to evaluate long-term effects, necessitating longer follow-up in future studies. The long-term impact of the intervention on behavioral and symptomatic outcomes was not assessed, leaving a gap in understanding its lasting effects. Increased contact between the researcher and the intervention group could have introduced observer bias; however, this was mitigated by providing both groups with equal information and using cluster sampling to randomize intervention and control groups. Also tracking changes in drug usage frequency could provide important insights into this technique’s potential as an alternative or complementary migraine treatment. Future studies will incorporate this measure to enhance the comprehensiveness of the findings. Despite conducting multiple training sessions and follow-up meetings to ensure participants executed the breathing techniques correctly, there remains the possibility that some participants did not practice the techniques accurately. This potential inconsistency could influence the integrity of the results and does not entirely eliminate the influence of placebo effects or participant variability. To address these concerns, we recommend that future studies incorporate a comparison with a similar but inactive intervention. The study’s reliance on measurable evaluation instruments might have limited the inclusion of biological or objective data, which could enhance the reliability of the results. Lastly, the study’s design may have led to more frequent contact between the researcher and the intervention group compared to the control group, potentially introducing observer bias.
Conclusion
This study suggests that ANB may be beneficial in reducing the frequency of migraine attacks and improving migraine-related disability. Future research should confirm the effectiveness of this technique and explore its broader applications. A multidisciplinary approach that includes primary care, with regular monitoring and comprehensive treatment recommendations by healthcare professionals, is essential. Further studies are needed to validate the efficacy of ANB and promote its use among a wider patient population.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S1463423625000064
Author contributions
O.Ç.: Writing – original draft and Writing – review & editing; G.L.: Conceptualization and Writing – review & editing; D.G.: Conceptualization, Supervision, Methodology, and Writing – review & editing.
Funding statement
We would like to clarify that this project received no external funding.
Competing interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.









