Introduction
In the treatment of head-and-neck cancer (HNC) with intensity-modulated radiation therapy (IMRT), a stable and highly precise immobilisation of the head, neck and upper chest is required to guarantee the reproducibility of the patient’s position between and during treatment fractions. Immobilisation is usually accomplished by simulating the patient in a supine position on a flat carbon fibre board, with stabilisation of the head and neck via fabrication of a custom thermoplastic mask attached to the board. However, some patients have great difficulty tolerating a flat position for the several minutes that are required to deliver an IMRT treatment.
A variety of medical or physical conditions may make the supine position challenging for a patient. In patients with cardiac insufficiency, redistribution of blood volume into the lungs during recumbency causes reduction in vital capacity and pulmonary compliance.Reference Go, Mozaffarian and Roger 1 , Reference Mukerji 2 Pulmonary disease, common among smokers, is another important cause of orthopnoea.Reference Mukerji 2 , Reference Ang, Ong and Eke 3 For patients experiencing orthopnoea, total lung capacity and vital capacity are enhanced with an elevated position.Reference Navajas, Farre, Rotger, Milic-Emili and Sanchis 4 , Reference Vilke, Chan, Neuman and Clausen 5 Specifically in patients with HNC, the additional factor of excessive salivation is one of the most common patient-reported symptoms. An elevated position decreases pooling of accumulated saliva in the pharynx, reduces the hazard of choking and assists in fluid clearance.Reference Epstein, Thariat and Bensadoun 6 In our clinical experience, even very fit patients who do tolerate a flat position complain about the accumulation of salivary mucus and the choking and orthopnoea that result.
Tilt boards have been used previously for patients unable to tolerate a supine position.Reference Yarbro, Wujcik and Gobel 7 There are several commercially available carbon fibre boards designed to tilt the patient’s upper body upwards during radiotherapy. Typically used for the treatment of breast or thoracic cancers, some of these boards are compatible with a head-only thermoplastic mask, but a board compatible with a full-length head-and-shoulder mask has not been previously available. Extended-field IMRT has become the dominant mode of HNC radiotherapy treatment and requires full-length immobilisation.
In this report, we developed a prototype head-and-shoulder adapter plate to attach to a tilting board and used this setup to deliver IMRT to a patient in an elevated position using a full-scale head-and-shoulder mask. We verified that the board met standards for dosimetric and clinical acceptability and quantified the impact of the tilted position on dosimetry and intra-fraction motion.
Materials and Methods
The patient was a 28-year-old young male who had near-total glossectomy and bilateral neck dissection, with pathologic diagnosis of pT4aN2cM0, Stage IVA squamous cell carcinoma of the tongue, as per AJCC 7th edition staging.Reference Edge, Byrd, Compton, Fritz, Greene and Trotti 8 The primary cancer occupied nearly the entire anterior oral tongue, crossing midline and invading the left tonsil, skeletal muscle and salivary glands. At surgery, there were positive microscopic margins and extranodal extension was identified in one of the two involved lymph nodes. Postoperative chemoradiotherapy was recommended.
The patient weighed 313 pounds, was 6 feet tall and had a body mass index (BMI) of 43·6 (obesity is typically defined as a BMI of 30). Due to the presence of the large soft tissue reconstruction in his mouth, he had near-constant, copious salivary secretions requiring frequent suction. For these reasons, he had difficulty lying flat and was sleeping upright in a chair at home.
Radiation therapy simulation
It was anticipated that a flat supine setup might be intolerable for the patient. Thus, it was decided to attempt simulation in both the flat and tilted positions to decide which would be more tolerable. The Access Supine Breast and Lung board (QFix, Avondale, PA, USA) was utilised for the base board (Figure 1). A prototype adapter plate, produced by the manufacturer and developed with our group, was attached to the top of the board. The adapter plate has pegs that fit into the tilt board to secure it in place and the adapter plate has the required holes to secure a full-length thermoplastic head-and-shoulder mask (Civco Medical Solutions, Coralville, IA, USA). The tilt board has a set of underbraces that produce various degrees of tilt up to 15°.

Figure 1 Tilting base board and head-and-neck adapter plate.
Except for the tilt board and adapter plate, the remainder of the patient’s setup was according to our departmental standards, including the use of custom plastic dental guards to prevent backscatter from metal fillings. The patient could not tolerate a tongue-depressing stent due to gagging. Computed tomography (CT) scans at 3 mm slice thickness were acquired with the patient at a 0° and a 10° tilt. The patient required preparatory suctioning and oxygen via nasal cannula during the 0° simulation but did not require these supports in the tilted 10° position.
Commissioning of the tilting board
The physical density of the prototype adapter plate was calculated based on volume and weight measurements, and the electron density was estimated by acquiring a megavoltage CT image on a Tomotherapy unit (Accuray Inc., Sunnyvale, CA, USA) and interpolating from the electron density calibration curve. To validate the dose calculations in the treatment planning system for posterior beams that pass through the tilt board, several dose measurements were taken using calibrated Gafchromic film (Ashland Inc., Covington, KY, USA). To investigate the accuracy of patient surface dose calculations, six film pieces were placed directly on the tilt board at various locations with solid water placed on top for backscatter. To investigate the accuracy of the dose calculated at depth in the patient, a 2 cm thick slab of solid water was placed on the tilt board and then six more film pieces and remaining solid water placed on top. Posterior 6 MV fields were delivered and the measured dose was compared with the Pinnacle calculations for the same setup. The standard clinical CT density table was used with no special override performed on the CT image of the tilt board and adapter plate.
Delineation of target volumes and organs at risk (OARs)
CTV6600 (clinical target volume prescribed to 6,600 cGy) included a small area at particularly high risk for recurrence and received 6,600 cGy over 30 fractions. CTV6000 included the primary tumour bed, the left neck nodal levels 1a–4 and the right neck nodal levels 1b–2. CTV5600 included the contralateral neck nodal levels 3–4 as well as the bilateral low neck. Uniform expansions of 0·3 cm were added to define the corresponding planning target volumes (PTVs). OARs were contoured per our departmental standards, including the brainstem, spinal cord, optic nerves and chiasm, right and left cochlea, parotid glands and mandible.
Treatment planning
Two treatment plans were developed in the Pinnacle treatment planning system (Philips Radiation Oncology Systems, Fitchburg, WI, USA) based on the flat position and the tilted position. Both plans used a single isocentre, nine widely distributed gantry angles and employed a step-and-shoot IMRT technique. IMRT was deemed necessary due to the decreased doses to the parotid gland as compared with 3D conformal radiation therapy.Reference Nutting, Morden and Harrington 9 Target and OAR dose–volume statistics were compared between the two plans. Plans were deemed clinically acceptable if OAR dosimetry met our pre-specified departmental standards (Table 1).
Table 1 Comparison of dosimetric parameters between plans created in flat and tilted positions
Abbreviation: PTV, planning target volume.
Imaging verification
The patient had a difficult experience lying flat and chose to be treated in the tilted position. Daily pre-treatment image guidance using kilovoltage cone-beam CT (CBCT) (XVI; Elekta, Atlanta, GA, USA) was performed; pre-treatment CBCT was registered in real time before each fraction was delivered. To check for intra-fraction motion, CBCTs were obtained immediately following treatment in a subset of fractions, once per week throughout the treatment course. It was decided not to obtain the post-treatment CBCT daily, given the excessive additional lengths of time the patient would be required to be on the table. The post-treatment CBCT was registered offline to the pre-treatment CBCT. The differences between the translations of the patient from the known couch shift performed before treatment and the post-treatment CBCT alignment were used to estimate the intra-fractional patient motion that had occurred between the time of pre-treatment and post-treatment.
Results
The physical density of the prototype adapter plate was calculated to be 0·98 g/cc and the electron density (relative to water) was 0·8. The attenuation and bolus effect of the adapter plate and tilt board were accurately calculated in the planning system to within 5% (mean absolute difference 2%) and 10% (mean absolute difference 5%) at 2 cm depth in the patient and on the patient surface, respectively.
Figure 2 displays sagittal CT images of the patient in the flat and tilted positions, along with contours and isodose lines for treatment plans. The plans demonstrate similar PTV coverage and OAR sparing, both within clinical acceptability (Table 1). All pre-specified OAR constraints were met in both plans.
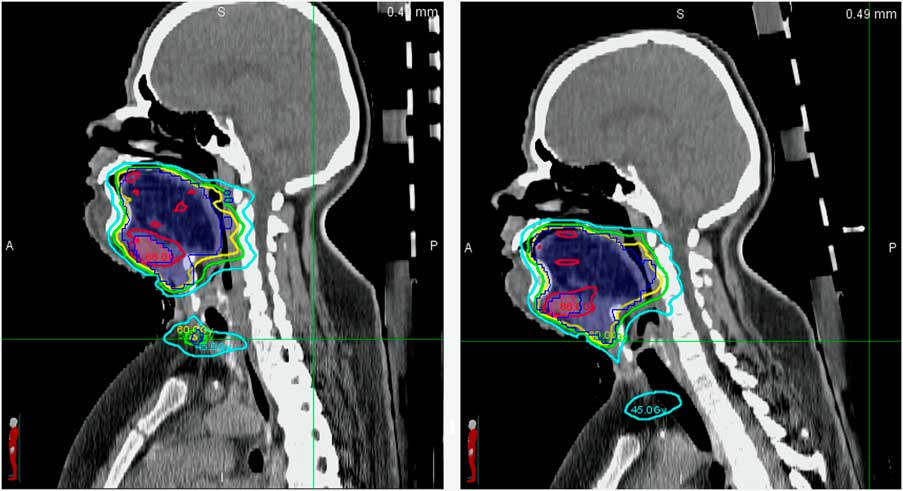
Figure 2 Sagittal computed tomographic slices of the patient in the flat (left) and tilted (right) position. Notes: The shaded blue contour is the PTV6000. The following isodose lines are displayed: 6,600 cGy (red), 6,000 cGy (yellow), 5,600 cGy (green) and 4,500 cGy (cyan). Abbreviation: PTV, planning target volume.
The intra-fraction motion was within 3 mm in all orientations at all time points (Table 2). The intra-fraction motion, estimated to equal the difference between the shifts required for CBCT alignments at the pre- and post-treatment time point, was from 0·1 to 2·6 mm. The absolute value of the intra-fraction motion did not exceed 3 mm.
Table 2 Estimated intra-fraction motion obtained from the difference in the shifts required to align pre- and post-treatment cone-beam computed tomographic scans, taken approximately once per week (mm)
Discussion
In this study, we showed that positioning on a novel tilting board was feasible and clinically acceptable for full-scale IMRT treatment of a complex HNC patient. The patient was able to complete his IMRT successfully with less fear of ‘choking and drowning’ due to the slant board. This setup could particularly benefit HNC patients who have difficulties with a flat, supine position due to orthopnoea or salivary accumulation. As the position of the entire upper body is elevated and reproducibly indexed in this setup, one could also conceive that patients with lymphoma, lung cancer or other cancers of the head-and-neck or thoracic regions could be treated in this way.
The quality of the plan in the tilted position was clinically equivalent to a treatment plan in a flat position. Both met our department’s dosimetric standards. Voong et al.Reference Voong, McSpadden and Pinnix 10 recently demonstrated that use of ‘butterfly’ IMRT beam arrangements, in conjunction with immobilisation on an inclined board with breath-hold during radiation treatment, reduced high doses to nearby critical organs and kept the low integral dose at acceptable levels in comparison with anterior-posterior techniques. In our study, meaningful differences between the two IMRT plans in the flat and tilted positions were not identified. This may be explained by the fact that both of our plans were developed using IMRT, which is an inverse planning process, and the same dose limitations were assigned to the critical organs.
Patient stability and intra-fraction motion was of concern because of the angled incline with potential for ‘sliding down the board’ and possible worsening of this effect with weight loss and loosening of the mask on the patient’s body. Using CBCT imaging taken before and after treatment at intervals throughout the treatment course, the intra-fraction motion was confirmed to be consistently <3 mm, which falls within our standard PTV margins and the usual range of motion associated with conventional flat setup positions in other reports.Reference Engelsman, Rosenthal and Michaud 11 , Reference Velec, Waldron and O’Sullivan 12
Limitations of our report are its preliminary and specific nature, the lack of quantification of benefits across a larger number of patients and the unknown variations that may occur for IMRT plans developed for other anatomic regions. There may be a range of applications that may be valid for patients who require radiotherapy treatment to the head, neck, mediastinum or upper chest, but these were outside the scope of this initial report. As we have just begun to utilise the board, structured assessments in the form of patient surveys or quality of life instruments were likewise outside the scope of this initial report. However, we are confident that we have established the feasibility and clinical acceptability of this novel tilting board for the particular application described.
This indexed, tilted board is proposed as a superior option for HNC patients who require full-scale head-and-neck immobilisation and are unable to tolerate IMRT in a flat position.






