Treatment non-adherence remains one of the greatest challenges in psychiatry. It has been estimated that 20–50% of any patient population is at least partially non-compliant, and that in patients with schizophrenia and related psychotic disorders rates can run as high as 70–80% (Reference Breen and ThornhillBreen & Thornhill, 1998). Adherence has been defined as the extent to which a person's behaviour coincides with the medical advice given (Reference Sackett and HaynesSackett & Haynes, 1976). The definition of non-adherence includes failure to enter a treatment programme, premature termination of therapy and incomplete implementation of instructions (including prescriptions).
Several randomised controlled trials (RCTs) and controlled clinical trials (CCTs) have been conducted to assess the efficacy of a wide range of clinical interventions to reduce non-adherence in patients with psychosis (Reference ChenChen, 1991). The focus of most of these studies has been the reduction of non-adherence to psychotropic medication or to scheduled appointments. Zygmunt and colleagues, who systematically reviewed RCTs and CCTs assessing psychosocial interventions for improving medication adherence in schizophrenia, showed that only a third of included studies reported significant treatment effects (Reference Zygmunt, Olfson and BoyerZygmunt et al, 2002). However, this review did not employ meta-analytic techniques, excluded studies assessing interventions for improving adherence to scheduled appointments and included highly selected populations of patients with schizophrenia. In this systematic review we adopted meta-analytic techniques to establish whether there are effective clinical interventions that community psychiatric services can implement to reduce medication and appointment non-adherence in patients with psychosis.
METHOD
Inclusion criteria
The review included studies assessing the efficacy of interventions aimed at reducing patient non-adherence. Studies with a random assignment design and studies with a comparison of outcome between two or more groups without a random assignment design were considered for inclusion. Only studies of patients with schizophrenia and related disorders or psychoses were selected. Studies, written in English, were included if adherence was one of the primary outcome measures, if patients were recruited in a psychiatric setting and if the control group received standard care. Studies of compulsory treatment and those assessing adherence to initial appointments were excluded. However, studies focusing on adherence to after-care programmes (i.e. appointments after hospital discharge) were included.
Search strategy
Relevant studies were located by searching Medline and PsycINFO from January 1980 onwards. The following keywords were used: ADHERENCE or COMPLIANCE or DROPOUT or ATTENDANCE or CONCORDANCE or TERMINATION or CONTINUITY and SCHIZOPHRENIA or PSYCHOSIS. Reference lists of relevant papers and previous systematic reviews were hand-searched for published reports and citations of unpublished research.
Data extraction
An ad hoc data extraction form was developed. Two reviewers independently extracted the following information: country in which the study was conducted, study setting, design, length of follow-up, main patient characteristics, description of experimental and control intervention, and definition of non-adherence. Definitions were grouped into two categories:
-
(a) not taking psychotropic drugs as prescribed
-
(b) not keeping appointments as scheduled.
Several methods have been reported to establish adherence; these were grouped into four categories:
-
(a) patient interview
-
(b) case-note evaluation
-
(c) rating scale
-
(d) urine test.
Clinical interventions for improving patient adherence were grouped into the following categories:
-
(a) educational strategies
-
(b) psychotherapy
-
(c) prompts
-
(d) specific service policies
-
(e) family interventions.
From each study the number of patients assigned to the experimental and control group was extracted, as was the number of patients meeting each study's definition of non-adherence. When appropriate, if only percentages were reported, they were converted into absolute numbers. For continuous outcomes the mean scores on any rating scale assessing non-adherence and the number of patients included in this analysis were recorded. Mean scores were recorded with the standard deviation (s.d.) or standard error (s.e.) of these values. When only the s.e. was reported, it was converted into s.d. using the method described by Altman & Bland (Reference Altman and Bland1996).
Statistical analysis
Dichotomous outcomes were summarised by calculating a Peto odds ratio (OR) for each study, together with the 95% confidence interval (CI). An overall weighted OR was then calculated as a summary measure. Continuous outcomes were analysed by calculating a standardised mean difference (SMD) for each study. This measure gives the effect size of an intervention in units of standard deviation so that scores from different outcome scales can be combined into an overall estimate of effect. A random effects model, which takes into consideration any between-study variation, was adopted to combine the effect sizes. Heterogeneity of treatment effect between studies was formally tested using the χ2 statistic. A meta-regression technique was in addition adopted to examine the extent to which study-level covariates predicted treatment effect.
RESULTS
The search
The electronic search generated 47 studies that met the inclusion criteria. In 23 of these (Appendix 1) results were reported without absolute numbers suitable for re-analysis. The remaining 24 studies (Appendix 2), which reported outcome data suitable for re-analysis, were included in our systematic review. Excluded and included studies did not differ with respect to the proportion of positive studies: a claim of efficacy was present in 13 out of 23 excluded studies (57%, 95% CI 34.4–76.8) and in 15 out of 24 included studies (63%, 95% CI 40.5–81.1) (χ2=0.174, P=0.676).
Characteristics of included studies
The majority of included studies were conducted in North America, four in Europe, four in China and one in Egypt (Table 1). A random allocation design was adopted in 58% of studies, whereas the others adopted a CCT design. The length of follow-up ranged from 2 weeks to 72 weeks, with a median of 24 weeks; this figure, however, did not include studies assessing non-adherence to after-care programmes, since the length of follow-up in these reports varied for each included patient depending on the length of time between hospital discharge and the scheduled appointment (Table 1). The mean number of patients per study was 149 (s.d. 159.3, median 81.5, range 21–660). Most studies were performed in out-patient settings, 38% followed patients from hospital to community and only a minority were conducted in hospital.
Table 1 Characteristics of included studies
| Study | Country | Design | Duration (months) | Setting | Special population of patients | Sample size (n) | Description of experimental intervention | Description of control intervention | Study end-point | Method used to assess non-adherence | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Experimental group | Control group | ||||||||||
| Boswell et al (1983) | USA | RCT | 12 | Out-patients | No | 184 | 185 | Telephone call before scheduled appointments | Usual care | Not keeping appointments as scheduled | Case notes |
| Chaplin & Kent (1998) | UK | RCT | 24 | Out-patients | No | 28 | 28 | Educational sessions about medication | Usual care | Missing more than 2 weeks of medication | Patient interview |
| Cramer & Rosenheck (1999) | USA | RCT | 24 | Out-patients | Low- adherence patients | 41 | 40 | Educational sessions to remember daily medication | Usual care | Not taking medication as prescribed | Electronic devices |
| Glick et al (1986) | USA | RCT | 48 | Hospital discharge patients | No | 42 | 37 | Time-limited partial hospitalisation programme | Non-specific intervention | Not keeping appointments after discharge | Medication compliance scale |
| Gomez Carrion et al (1993) | USA | CCT | 48 | Out-patients | No | 55 | 56 | Educational sessions about medication | Non-specific intervention | Not keeping appointments as scheduled | Case notes |
| Hayward et al (1995) | UK | RCT | 4-8 | Hospital discharge patients | No | 10 | 11 | Motivational interview psychotherapy | Non-specific intervention | Not taking medication as prescribed | Three-point scale |
| Hornung et al (1998) | Germany | CCT | 48 | Out-patients | No | 84 | 64 | Psychoeducational medication training | Non-specific intervention | Not taking medication as prescribed | Patient interview |
| Kelly & Scott (1990) | USA | RCT | 24 | Out-patients | No | 314 | 104 | Health education | Usual care | Not taking medication as prescribed | Patient interview |
| Kemp et al (1996) | UK | RCT | 72 | In-patients | No | 39 | 35 | Cognitive psychotherapy | Non-specific intervention | Not taking medication as prescribed | Adherence scale |
| Kopelowicz et al (1998) | USA | RCT | NS | Hospital discharge patients | No | 28 | 31 | Community re-enter educational programme | Non-specific intervention | Non-attendance at first post-discharge appointment | Case notes |
| Masnik et al (1981) | USA | CCT | 24 | Out-patients | Low-adherence patients | 73 | 204 | Seeing patients on a walk-in basis | Usual care | Non-attendance at appointments | Case notes |
| Olfson et al (1998) | USA | CCT | NS | Hospital discharge patients | No | 53 | 51 | Pre-discharge out-patient clinician contact | Usual care | Non-attendance at first post-discharge appointment | Patient interview |
| Ran & Xiang (1995) | China | CCT | 24 | Out-patients | No | 22 | 10 | Psychoeducational family intervention | Usual care | Not taking medication as prescribed | Case notes |
| Robinson et al (1986) | USA | RCT | 2 | Hospital discharge patients | No | 50 | 50 | Educational sessions about medication | Usual care | Not taking medication as prescribed | Rating scale |
| Seltzer et al (1980) | Canada | CCT | 20 | In-patients | No | 32 | 35 | Educational group sessions about medication | Usual care | Not taking medication as prescribed | Urine test |
| Sharma et al (1995) | USA | CCT | NS | Hospital discharge patients | No | 25 | 57 | Pre-discharge out-patient clinician contact | Usual care | Non-attendance at first post-discharge appointment | Case notes |
| Shivack & Sullivan (1989) | USA | CCT | NS | Hospital discharge patients | No | 221 | 439 | Telephone call before scheduled appointments | Usual care | Non-attendance at first post-discharge appointment | Case notes |
| Sledge et al (1990) | USA | CCT | NS | Out-patients | First cases | 34 | 115 | Time-limited psychodynamic psychotherapy | Non-specific intervention | Dropping out during psychotherapy | Case notes |
| Stickney et al (1980) | USA | CCT | NS | Hospital discharge patients | No | 200 | 200 | Pre-discharge out-patient clinician contact | Non-specific intervention | Non-attendance at first post-discharge appointment | Case notes |
| Strang et al (1981) | USA | RCT | 6 | Out-patients | No | 17 | 15 | Family therapy | Non-specific intervention | Not taking medication as prescribed | Plasma level |
| Xiang et al (1994) | China | RCT | 16 | Out-patients | No | 36 | 41 | Psychoeducational family intervention | Usual care | Not taking medication as prescribed | Case notes |
| Xiong et al (1994) | China | RCT | 72 | Out-patients | No | 34 | 29 | Psychoeducational family intervention | Usual care | Not taking medication as prescribed | Patient interview |
| Youssef (1984) | Egypt | RCT | 24 | Hospital discharge patients | No | 18 | 18 | Educational sessions about medication | Usual care | Not taking medication as prescribed | Pill counts |
| Zhang et al (1994) | China | RCT | 72 | Out-patients | First cases | 42 | 41 | Psychoeducational family intervention | Usual care | Not taking medication as prescribed | Case notes |
In 14 studies the experimental intervention was an educational programme, in five cases specifically developed for family members. Five studies evaluated specific service policies, such as pre-discharge contacts between patients and the community team, or pre-discharge educational sessions about antipsychotic medication. Three studies assessed the benefit of psychotherapeutic interventions, in two cases adopting a cognitive approach and in one case a psychodynamic approach. Two studies assessed the effect of prompts in the form of telephone calls. Usual care was the control intervention in 63% of studies; in the others a non-specific intervention, similar to the experimental programme in terms of number of sessions, was employed. These interventions were developed to reduce non-adherence to psychotropic medication in 14 studies, assess attendance at first appointments after hospital discharge in six studies and increase attendance at scheduled appointments in four studies (Table 1).
Outcome of studies
Of the 24 included studies, 19 reported dichotomous and 5 continuous outcome data. In 4 studies dichotomous outcome data were inferred from percentages reported in the study tables. The treatment effect of each study is presented in Figs 1 and 2. Overall, clinical interventions for reducing patient non-adherence were significantly more effective than control interventions. The pooled OR for dichotomous outcomes was 2.59 (95% CI 2.21–3.03; Fig. 1); similarly, the pooled SMD for continuous outcomes was 0.36 (95% CI 0.06–0.66; Fig. 2). The funnel plot for studies with dichotomous outcome was not symmetrical, indicating that publication bias could not be ruled out (Fig. 3).
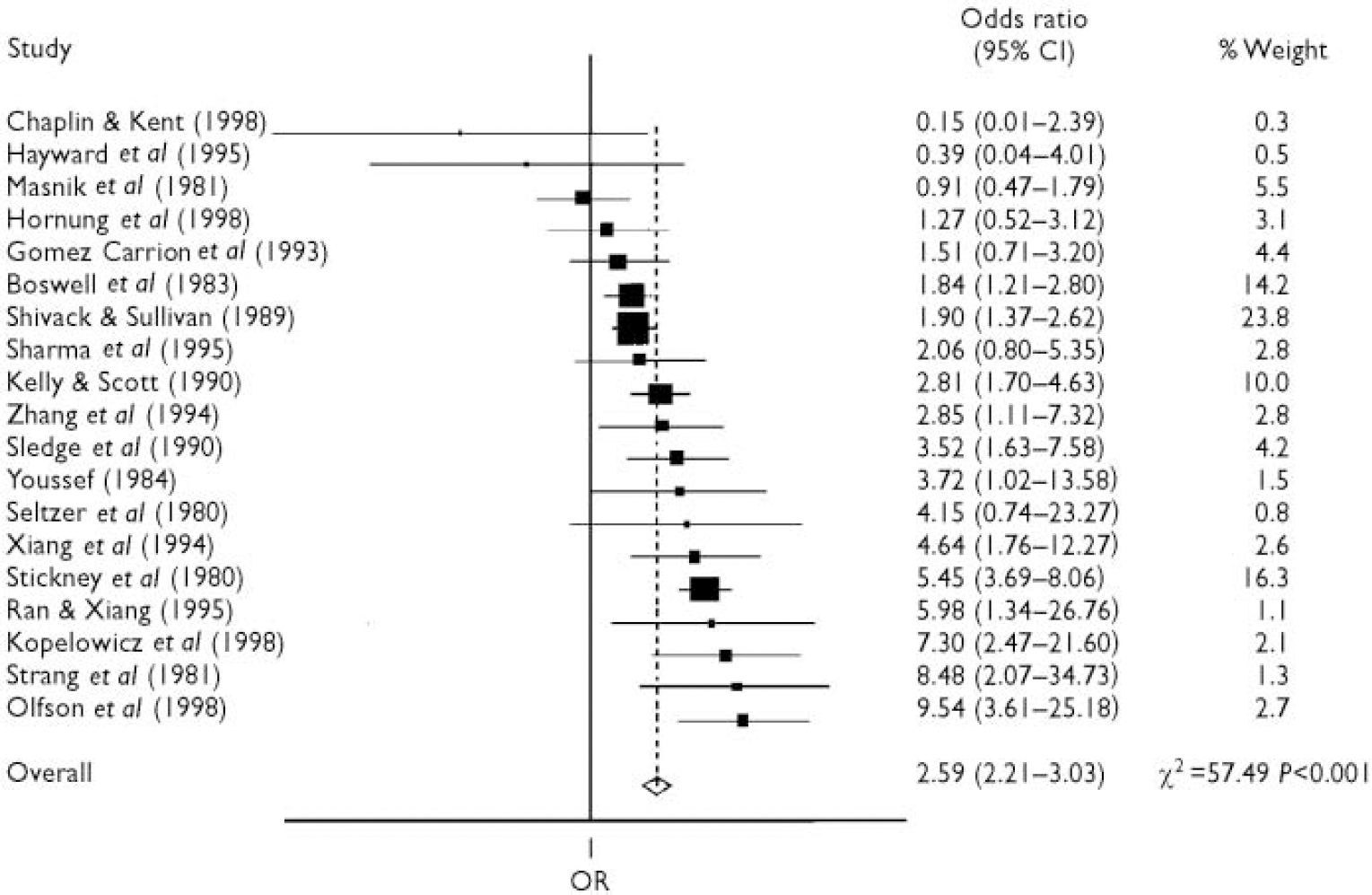
Fig. 1 Meta-analysis of studies assessing the effect of interventions for improving adherence: overall treatment effect for dichotomous outcomes. Odds ratio (OR) > 1 favours experimental interventions; OR < 1 favours usual care.
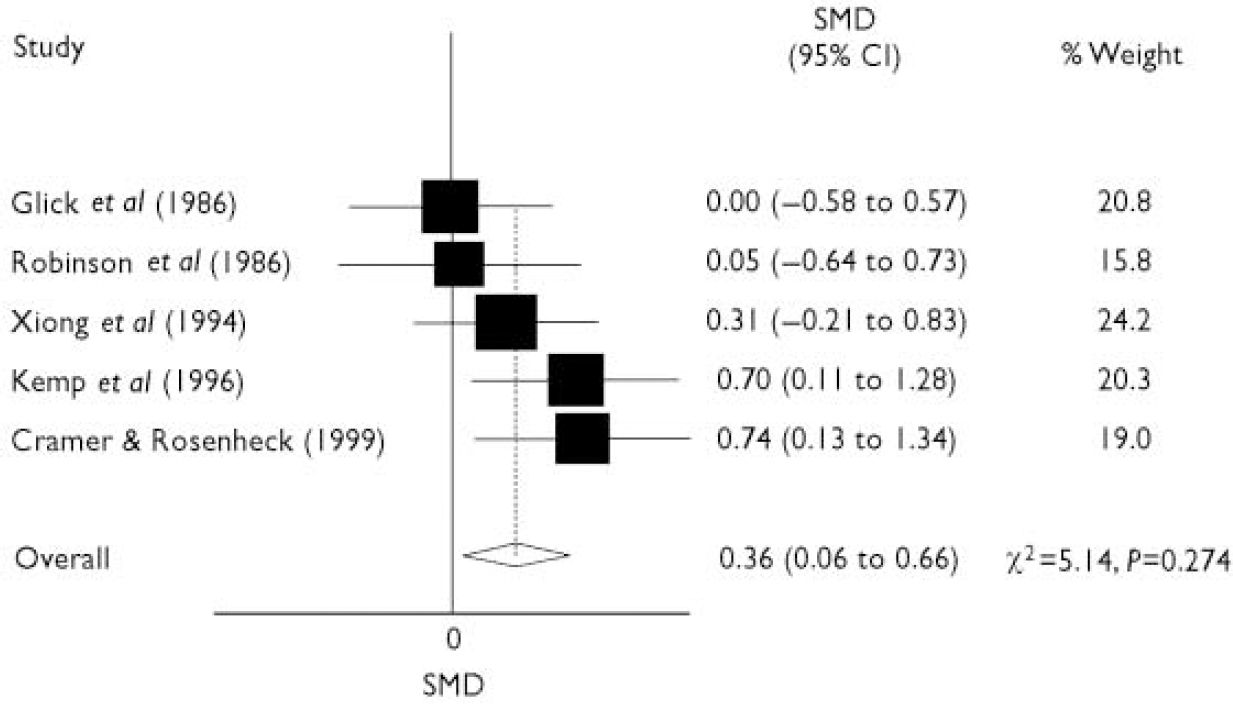
Fig. 2 Meta-analysis of studies assessing the effect of interventions for improving adherence: overall treatment effect for continuous outcomes. Standardised mean difference (SMD) > 0 favours experimental interventions; SMD < 0 favours usual care.
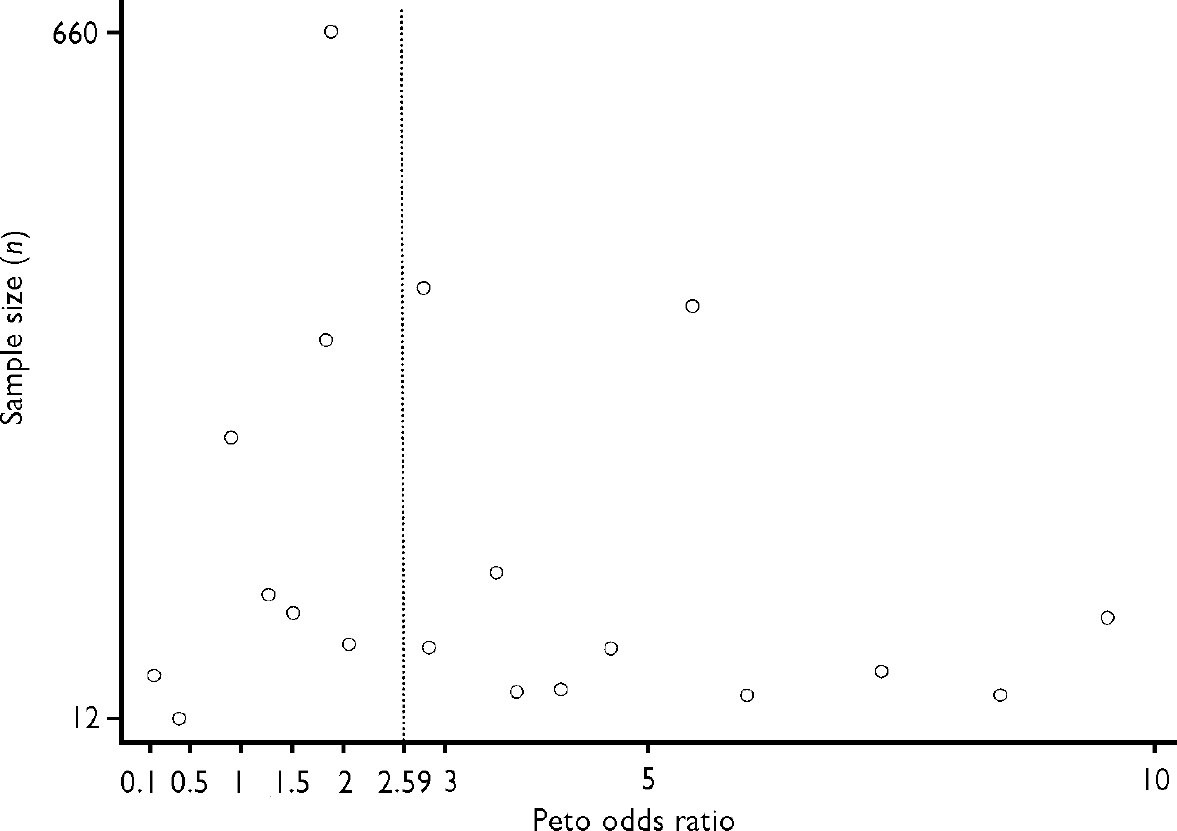
Fig. 3 Funnel plot of estimated odds ratio against the size of the study. The broken vertical line represents the overall intervention estimate.
Subgroup analysis
A subgroup analysis was carried out by stratifying the 19 studies with dichotomous outcome data by the study characteristics reported in Table 2. Studies adopting an RCT design yielded an OR similar to studies adopting a CCT design. The effect of clinical interventions for reducing non-adherence was greater in studies with a short follow-up period (OR 2.27, 95% CI 1.78–2.90) than in those with a follow-up of 6 months or more (OR 1.70, 95% CI 1.04–2.78); moreover, it was slightly greater in studies enrolling homogeneous populations of patients with schizophrenia, and in studies assessing adherence with hospital discharge programmes (Table 2). Studies assessing adherence to medication yielded a slightly higher OR than studies assessing adherence to out-patient and post-discharge appointments. All five categories of clinical interventions were more effective than control interventions in reducing patient non-adherence.
Table 2 Odds ratios of subgroup analyses of studies assessing the effect of interventions for reducing non-adherence
| Study characteristic | Patients (n) | Studies1 (n) | Peto OR2 | (95% CI) |
|---|---|---|---|---|
| Design | ||||
| RCT | 1119 | 9 | 2.60 | (1.99-3.39) |
| CCT | 2030 | 10 | 2.58 | (2.12-3.14) |
| Length of follow-up | ||||
| < 6 months | 1502 | 11 | 2.27 | (1.78-2.90) |
| 6+ months | 324 | 3 | 1.70 | (1.04-2.78) |
| Not applicable | 1323 | 5 | 3.17 | (2.52-3.99) |
| Diagnosis | ||||
| Schizophrenia only | 537 | 7 | 3.21 | (2.19-4.68) |
| Severe mental disorders | 2612 | 12 | 2.47 | (2.08-2.94) |
| Intervention | ||||
| Education | 895 | 7 | 2.41 | (1.72-3.37) |
| Psychotherapy | 170 | 2 | 2.83 | (1.36-5.87) |
| Prompts | 1029 | 2 | 1.87 | (1.45-2.42) |
| Service policies | 863 | 4 | 3.63 | (2.68-4.92) |
| Family therapy | 192 | 4 | 4.45 | (2.52-7.83) |
| Adherence to | ||||
| Appointments | 2211 | 9 | 2.52 | (2.10-3.02) |
| Medication | 938 | 10 | 2.81 | (2.03-3.88) |
| Setting | ||||
| In-patients | 123 | 2 | 1.65 | (0.38-7.18) |
| Out-patients | 1664 | 10 | 2.16 | (1.72-2.70) |
| Hospital discharge | 1362 | 7 | 3.13 | (2.50-3.91) |
Meta-regression analysis
The individual contribution of each of the above-mentioned study characteristics to treatment outcome was assessed by a meta-regression analysis (Table 3). Only two covariates were significantly associated with treatment outcome, namely length of follow-up and diagnosis. Length of follow-up was significantly associated with a less favourable treatment outcome, whereas diagnosis of schizophrenia was associated with a more favourable treatment effect.
Table 3 Predictive effect of study covariates on treatment outcome (meta-regression analysis)

| Covariates | Coefficient1 (s.e.) | z | P 2 |
|---|---|---|---|
| Randomised controlled trial3 | 0.021 (1.173) | 0.02 | 0.985 |
| Length of follow-up | |||
| < 6 months | Reference | ||
| 6+ months | -5.105 (1.620) | -3.15 | 0.002 |
| Not applicable | 1.490 (2.568) | 0.58 | 0.562 |
| Schizophrenia3 | 3.802 (1.429) | 2.66 | 0.008 |
| Intervention | |||
| Education | Reference | ||
| Psychotherapy | -0.598 (1.994) | -0.30 | 0.764 |
| Prompts | -1.862 (2.036) | -0.91 | 0.361 |
| Service policies | -0.522 (1.904) | -0.27 | 0.784 |
| Family therapy | 1.349 (1.550) | 0.87 | 0.384 |
| Adherence to medication3 | -0.438 (1.750) | -0.25 | 0.802 |
| Hospital discharge3 | -0.077 (2.021) | -0.04 | 0.969 |
| Constant term | 3.449 (3.334) | 1.03 | 0.301 |
DISCUSSION
Interpretation of the results in the context of previous reviews
This systematic review showed that community psychiatric services can provide effective clinical interventions, backed by scientific evidence, for reducing patient non-adherence. The magnitude of the overall treatment estimate suggests that, after a median follow-up of 6 months, these interventions more than double the likelihood of adherence to psychotropic medications and to scheduled appointments. Chen (Reference Chen1991), who conducted a narrative review of clinical interventions in psychoses, recommended scheduling appointments before discharge from in-patient treatment, using prompts in the forms of letters and telephone calls to encourage patients to keep their appointments and offering education about treatment and medication. However, it is unclear whether these strategies are equally effective in reducing patient non-adherence. In our analysis all interventions were found to be more effective than control treatments, but with different magnitudes of effect. Differences, however, were observed in the univariate analysis only: in the meta-regression model no single intervention emerged as predictor of overall treatment effect. Although this finding might suggest that all interventions are similarly effective, caution should be adopted in drawing definitive conclusions. The number of studies supporting each intervention and the total number of patients included in the evaluation of each intervention were fairly different, raising issues of generalisability. For example, only two studies evaluated the effect of prompts, but they included more than 1000 patients; in contrast, two studies evaluating the effect of psychotherapeutic interventions included fewer than 200 patients. Evidence derived from small samples and generated in a few settings cannot be considered as robust as evidence derived from large samples recruited in a diverse range of settings. From this perspective, we found robust data supporting, for example, the implementation of specific service policies such as pre-discharge contacts between patients and the community team, or supporting educational interventions about treatment and medications. Only direct comparisons between different strategies for reducing patient non-adherence will clarify whether some interventions are more cost-effective than others.
In contrast with this meta-analysis, the review by Zygmunt et al (Reference Zygmunt, Olfson and Boyer2002) showed that only a third of 39 identified studies reported significant intervention effects. However, that review included only studies assessing the effect of interventions for reducing medication non-adherence. In our review, studies assessing the effect of interventions for improving adherence to scheduled appointments were included. Zygmunt et al (Reference Zygmunt, Olfson and Boyer2002) included only studies of highly selected populations of people with schizophrenia, whereas we included non-selected populations of patients with psychosis. In addition, only studies in which adherence was one of the primary outcome measures were included in our analysis, whereas Zygmunt et al (Reference Zygmunt, Olfson and Boyer2002) included studies in which adherence was not one of the primary end-points. These differences may explain their negative conclusions, as suggested by the evidence that studies where adherence was the central goal of the study provided positive results (Reference Zygmunt, Olfson and BoyerZygmunt et al, 2002). In some cases (for example, studies focusing on interventions not specifically developed for improving adherence), the decision whether adherence was one of the primary outcome measures or an ancillary variable was somewhat arbitrary. However, in most cases study authors clearly stated that the intervention was tested with the central goal of improving adherence (Bush et al, 1990; Xiang et al, 1994; Ran & Xiang, 1995; Dixon et al, 1997). We included only studies with a control group of patients receiving usual care, but Zygmunt et al (Reference Zygmunt, Olfson and Boyer2002) did not exclude direct comparisons of different active strategies for improving medication adherence, such as behavioural management v. intensive case management, or psychoeducation plus family therapy v. psychoeducation plus relatives’ groups; in only some of these direct comparisons was there a control group receiving standard care. Finally, the meta-analytic technique we employed to re-analyse outcome data systematically excluded studies without data suitable for re-analysis. Taken together, these differences may have overemphasised the treatment effect found in our analysis and explain the negative conclusions reached by Zygmunt et al (Reference Zygmunt, Olfson and Boyer2002).
Long-term effect of interventions for reducing non-adherence
A second issue, relevant from a clinical viewpoint, is the long-term benefit of these interventions. Most of the included studies showed a positive effect soon after the implementation of the intervention for reducing non-adherence, but only a minority assessed whether the effect was maintained in the long term. In the meta-regression model, length of follow-up was negatively associated with treatment effect, suggesting that the benefit of the interventions is less evident with increasing length of follow-up. Until long-term data become available and until studies establish which intervention maintains its effect in the long term, clinical interventions should be implemented in practice as short-term measures. For example, orientation and education about treatment and medications is essential to keep patients in treatment, but this intervention should be frequently and routinely repeated in the same patients, because it is unknown whether its effect is maintained in the long term. Similarly, pre-discharge contacts between patients and the out-patient team, or pre-discharge psychotherapeutic interventions, must become a routinely delivered service policy, offered each time patients are scheduled for discharge, even for patients who have already received it during previous admissions. In some community psychiatric services this goal is achieved by mixing in-patient and out-patient staff, so that in-patients are treated by the same team who will eventually offer out-patient care. This policy, which allows pre-discharge patient–staff contacts and the implementation of therapeutic plans before hospital discharge, has been shown to be associated with high rates of patient adherence in the long term (Reference Sytema, Micciolo and TansellaSytema et al, 1997).
Diagnostic issues
A third issue is that patients with psychosis are a rather heterogeneous group. In many studies this diagnosis was adopted to collect representative samples of patients seen in everyday practice, including not only those with schizophrenia and related disorders, but also those showing psychotic features requiring the use of antipsychotic drugs. In some cases ambiguous diagnostic definitions were adopted, leading to the inclusion of patients with schizophrenia and with other unspecified diagnostic characteristics. It is possible that inclusion of these patients has increased the generalisability of study findings, since in everyday conditions many typical patients do not precisely fulfil diagnostic criteria of schizophrenia. Rather than relying on diagnostic criteria only, therefore, it might be useful to include in studies patients who are clinically or epidemiologically representative (Reference Thornicroft and TansellaThornicroft & Tansella, 2002). These patients need to be characterised using valid and reliable descriptors, and in most studies this description is currently lacking.
It is possible that interventions suitable for those with schizophrenia might not be suitable for other patients. In the meta-regression model we found that studies enrolling only homogeneous samples of people with schizophrenia were associated with a more favourable treatment effect, suggesting that these interventions are less effective in patients with other diagnoses. Similar findings emerged for other patient populations. Pampallona et al (Reference Pampallona, Bollini and Tibaldi2002), who performed a systematic review of patient adherence in the treatment of depression, showed that studies on adherence did not provide either reliable or consistent indications as to the efficacy of specific interventions. It is possible that psychoeducational or cognitive interventions, developed for patients with schizophrenia and for family members of those with schizophrenia, are not easily transferred to other categories of patients and family members with the same positive results.
Adherence to medication v. adherence to scheduled appointments
The magnitude of effect of interventions developed for improving adherence to medication was similar to that of interventions developed for improving adherence to scheduled appointments. We acknowledge the difficulty of making a clear distinction between these two categories, which were in many cases ambiguous and somewhat artificial. Patients not wishing to take the prescribed medicines might miss the scheduled appointments. Similarly, patients who want to discontinue the contact with the community psychiatric service might also stop taking the prescribed medicines. It might therefore be speculated that failing to adhere to treatment programmes is a patient characteristic that might result either in dropping out of treatment or in discontinuing the medicines, or both. There is nothing in the literature to show that there are two distinct categories of non-adherent patients, according to the definition of non-adherence. In other words, the concept of non-adherence might be unified and considered as one patient-related variable which can be measured and defined in many different ways.
Studies published before 1980
A limitation of this analysis is the exclusion of study reports published before 1980. This exclusion criterion was imposed for the purpose of generating evidence easily applicable to the modern organisation of community psychiatric services. Most studies before 1980 recruited patients resident in psychiatric hospitals and assessed strategies for reducing non-adherence to in-patient treatment regimens, or assessed compliance with out-patient programmes implemented in a hospital-based context of care where community facilities were lacking (Reference Cramer and RosenheckCramer & Rosenheck, 1998). In contrast, after 1980 many countries developed community-oriented systems of psychiatric care, with a diminished emphasis on psychiatric hospitals and a high priority given to out-patient care delivered by community mental health centres (Reference Mosher and BurtiMosher & Burti, 1994). Continuity of care has thus become a basic quality requirement, essential to follow patients in their own context of life for a long time. We acknowledge that in our approach we might have missed some studies conducted in a community-oriented setting before 1980; however, this choice allowed us to pool data derived from a group of psychiatric services with a homogeneous commitment and a common mission. The exclusion of studies assessing adherence at initial appointments was based on similar reasoning: these constituted a separate group of studies, in which the main issue was not keeping contacts in the long term, but developing strategies for better psychiatric referral (Reference Kluger and KarrasKluger & Karras, 1983).
Studies excluded from the meta-analysis
A second limitation is the exclusion of 23 studies because of the lack of information suitable for re-analysis. This represents a well-known source of potential bias when a quantitative approach is used in systematic reviews. The funnel plot of included studies was not symmetrical, suggesting that some studies might have been missed, for example small, negative studies (Fig. 3). These studies might be those not reporting absolute numbers or, possibly, those published in non-English-language journals. Their exclusion might have overemphasised the overall effect. To decrease this possibility two approaches were adopted. First, we always attempted to infer absolute numbers from percentages reported in study tables; this was only feasible with a high degree of confidence in four cases, since in the others reviewers did not reach an agreement on the exact numbers to extract. Second, excluded studies were compared with the included ones and information on each study outcome was qualitatively extracted in agreement with what was reported by the study authors. The evidence that the proportion of reports with positive findings was similar in the two groups of studies did not corroborate (although not completely excluding) the possibility of selection bias.
Definition of adherence
Studies adopting different definitions of non-adherence and different methods of assessing non-adherence were grouped together. These differences are explained by the characteristics of the interventions under scrutiny: for example, studies evaluating prompts in the form of telephone calls adopted operational definitions of non-adherence such as non-attendance at appointments, whereas studies evaluating educational strategies on medications and side-effects measured the proportion of patients taking psychotropic drugs as prescribed. In some cases, however, the same interventions were evaluated using different definitions, for example studies assessing adherence after hospital discharge adopted definitions such as attendance at first out-patient appointment, attendance at five out-patient appointments, or attendance at a predefined proportion of appointments during follow-up. Only in a minority of studies were rating scales employed. These differences represent study limitations that might have been responsible for some between-study heterogeneity observed in the meta-analysis. The meta-regression model could have investigated this potential source of heterogeneity, but this approach was not used because it would have inevitably decreased the power of the analysis, generating findings of uncertain clinical relevance.
Recommendations
Much is still to be done in the field of treatment adherence in patients with schizophrenia and severe mental disorders. Experimental studies have to address the effectiveness of educational strategies, psychotherapeutic programmes and specific service policies in large samples of patients recruited in many different settings and followed in the long term. Patients with schizophrenia should be considered separately from those with other diagnoses. Trials must adopt a high standard in terms of conduct and reporting: exclusion rates and reasons for exclusion should always be reported, as well as the proportion of patients failing to adhere to treatment at the end of the acute phase and the proportion of patients remaining adherent at follow-up. Absolute numbers should be given, avoiding the use of percentages without reporting the denominator to which they refer. Outcome data have to be reported for both completer and intention-to-treat samples.
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
▪ A large variety of clinical interventions have been studied to reduce non-adherence to treatment in patients with psychoses.
-
▪ After a median follow-up of 6 months these interventions more than double the likelihood of adherence to psychotropic medications and to scheduled appointments.
-
▪ The long-term benefit of clinical interventions for reducing treatment non-adherence in psychoses has still to be documented.
LIMITATIONS
-
▪ The studies included adopted different definitions and different measures of non-adherence.
-
▪ The exclusion of 23 studies not reporting information suitable for re-analysis represents a potential source of bias.
-
▪ Studies published before 1980 were not included.









eLetters
No eLetters have been published for this article.