Mental health needs include broad domains of health and social functioning, which are necessary to survive and prosper in the community. Needs can be assessed from different perspectives, including staff, patient or carer, and have been differentiated into unmet needs (current serious problems, whether or not help is given) and met needs (no or moderate problems because of help given) (Reference Phelan, Slade and ThornicroftPhelan et al, 1995). A consensus is emerging across Europe and Australasia that mental healthcare should be provided on the basis of need, with an intended goal of improving subjective quality of life (e.g. Mental Health Branch, 1997; Department of Health, 1999; Reference Lasalvia, Ruggeri and MazziLasalvia et al, 2000). This study investigated whether high levels of need cause poor quality of life. If confirmed, then this study will provide evidence supporting the view that mental health services should routinely assess and meet unmet needs, in order to improve quality of life.
METHOD
Hypotheses
This study was a hypothesis-driven pre-planned analysis nested within a randomised controlled trial (to be reported separately) investigating routine use of outcome measures in adult mental health services (international standard randomised controlled trial number (ISRCTN) 16971059).
Bollen (Reference Bollen1989) proposed three criteria for establishing a causal relationship: association (the putative cause and effect have temporal and spatial contiguity), direction (cause precedes effect) and isolation (the effects of a cause are isolated from competing causes). Cross-sectional association and isolation in the relationship between needs and quality of life have been shown previously (Reference Slade, Leese and TaylorSlade et al, 1999a ; UK700 Group, 1999; Reference Wiersma and van BusschbachWiersma & van Busschbach, 2001; Reference Hansson, Sandlund and Bengtsson-TopsHansson et al, 2003; Reference Slade, Leese and RuggeriSlade et al, 2004). The first aim of this study was to investigate whether association remains in longitudinal data. The hypothesis was that higher patient-rated unmet need is associated with lower individual quality of life assessments by a patient over time. The second aim was to investigate temporal precedence in the relationship between patient-rated unmet need and quality of life, with the aim of establishing direction in the relationship. The hypothesis was that reduction in patient-rated unmet need precedes improvement in quality of life.
Participants
The inclusion criteria were that patients had been on the case-load of any of the eight community mental health teams in Croydon (South London) on 1 May 2001 for at least 3 months, and were aged between 18 and 64 years inclusive. Croydon has a population of 319 000 and its population is nationally representative. Approximately 3500 patients use community mental health teams in Croydon. To ensure epidemiological representativeness, stratified random sampling was used for sample selection. Identified prognostic factors were age (tertiles), gender, ethnicity (White v. Black and minority ethnic), clinical diagnosis (psychosis v. other) and community mental health team (1–8). Men and women were equally represented in the base population, but had different age distributions, with more women in the highest tertile. The sample was therefore stratified by tertiles within gender, to give six age – gender combinations having approximately equal proportions in the base population. Similarly, the distribution of patients across the eight community mental health teams was not equal, so a proportionately higher recruitment target was set for those dealing with more patients than average. The sample was therefore carefully selected to ensure that prognostic factors were in proportion to their representation in the base population of Croydon mental health patients. This approach of equal sample fractions allows straightforward analysis without weighting, since the sample is fully representative of the base population. Participants were recruited between May 2001 and December 2002.
Measures
Measures were chosen following application of pre-planned criteria to assessments intended for routine clinical use (Reference SladeSlade, 2002). Quality of life was assessed using the Manchester Short Assessment of Quality of Life (MANSA; Reference Priebe, Huxley and KnightPriebe et al, 1999), a 16-item measure derived from the Lancashire Quality of Life Profile (Reference Oliver, Huxley and PriebeOliver et al, 1997). MANSA comprises 4 objective questions and 12 subjective questions. The subjective items assess satisfaction with life as a whole, job (or sheltered employment, or training/education, or unemployment/retirement), financial situation, number and quality of friendships, leisure activities, accommodation, personal safety, people that the individual lives with (or living alone), sex life, relationship with family, physical health and mental health. Each item is rated on a seven-point satisfaction scale, from 1=‘Couldn't be worse’ to 7=‘Couldn't be better’. The summary score used in this study is the mean of the 12 subjective items (range 1 to 7, the higher the score the better the quality of life).
Unmet need was assessed using the Camberwell Assessment of Need Short Appraisal Schedule (CANSAS; Reference Slade, Thornicroft and LoftusSlade et al, 1999b ), a modified version of the Camberwell Assessment of Need (CAN; Reference Phelan, Slade and ThornicroftPhelan et al, 1995). The CANSAS assesses needs in 22 health and social domains: accommodation, food, looking after the home, self-care, daytime activities, physical health, psychotic symptoms, information (about condition and treatment), psychological distress, safety to self, safety to others, alcohol, drugs, company, intimate relationships, sexual expression, childcare, basic education, telephone, transport, money and benefits. For each domain, the possible ratings are unmet need (current serious problem, regardless of any help received), met need (no/moderate problem because of help given), no need or not known. Data reported here are from the patient-rated version: CANSAS–P. The summary unmet need score (CANSAS–P unmet) is the number of domains with an unmet need (range for both 0–22, low score better).
The National Adult Reading Test (Reference NelsonNelson, 1982) assesses premorbid IQ. The Brief Psychiatric Rating Scale (BPRS) is an 18-item interviewer-rated assessment of symptoms (summary score range 0–126, low score better) (Reference Overall and GorhamOverall & Gorham, 1988).
Procedures
All assessments were completed at baseline, through case-note audit and staff and patient interviews. The aim of this study was to collect routine outcome data, which involves patients self-rating the patient-rated measures rather than the interviewer completing them through interview. Backward chaining was used at baseline to train the patient to self-rate CANSAS–P and MANSA at the baseline assessment. The first few questions of CANSAS–P were completed by the researcher asking questions, giving a verbal description of which rating is appropriate, giving a visual prompt by pointing at the correct box to tick, and then ticking the box. These prompts were then withdrawn in order, so that initially the patient was given the pen but the questions and verbal and visual prompts were given so the patient only had to tick the box, then the visual prompt was withdrawn, then the question was asked but no verbal prompting was given, and finally no questions were asked. A similar approach was used for MANSA where necessary. Following baseline assessment, patients were randomly allocated to either the intervention (n=101) or control (n=59) group. Data from the intervention group only are reported here.
Those in the intervention group were asked to complete a postal questionnaire on a monthly basis. The postal questionnaire included CANSAS–P and MANSA. One month after baseline assessment (with the researcher), the first postal questionnaire was sent. Thereafter postal questionnaires were sent monthly for a further 4 months, and then follow-up assessments were made 2 months after the last postal questionnaire. At the follow-up assessment patients self-completed CANSAS–P and MANSA with no input from the researcher. Excluding the baseline assessment, which was completed with the active involvement of the researcher, six rounds of self-completed routine data were therefore obtained. Rounds 1–5 were 1 month apart, with 2 months between rounds 5 and 6.
Analysis
Differences between responders and non-responders were assessed using χ2 and independent samples t-test analysis. A longitudinal regression model was fitted, to assess the effects of both cross-sectional and longitudinal associations (Reference Diggle, Heagerty and LiangDiggle et al, 2002). The dependent variable was the MANSA at each round from 1–6 (i.e. a maximum of six records per person). The mean patient-rated unmet need (CANSAS–P unmet) over the six rounds was included to model the cross-sectional association. The change from the current value of unmet need to the value 1 month previously was included to model the longitudinal association. Number of months since baseline was included to reflect any overall linear trend in time. The effect of community mental health team (1–8) was assessed in preliminary analyses, but was omitted from the final model as it was not significant. Correlation between repeated measurements for individual patients was accounted for by including a random effect for each patient, within the random effects regression model. The percentage of variation explained between and within patients is presented, as well as the breakdown of residual variation into components associated with individual patients (patient level random effects) and completely unexplained variation. The model was fitted: (a) with level, change and time trend as potential explanatory variables; (b) as (a) plus socio-demographic variables (gender, age, White v. Black and minority ethnic, full-scale IQ); and (c) as (b) plus BPRS and diagnosis (psychosis v. other). The model was also fitted with (c) plus interaction terms to investigate whether the difference in full-scale IQ found between responders and non-responders affected the relationship between mean and changed unmet need and quality of life. The acceptability of the final model was tested by visual assessment of histograms showing the distributions of the random effects and of the residual random errors, and by considering associations with the dependent variables using scatter plots. The distribution of residuals was normal and uncorrelated with the main explanatory variables. All analysis was undertaken using Stata Version 8.0 for Windows.
RESULTS
One hundred and sixty patients were recruited, of whom 101 were randomly allocated to the intervention group and reported here. The response rates for rounds 1–6 were 85%, 84%, 76%, 76%, 76% and 92%. In total, 73 of the 101 patients completed at least two consecutive ratings, allowing them to be considered in this analysis. The characteristics of the responders (n=73) and non-responders (n=28) are shown in Table 1.
Table 1 Baseline characteristics of participants with (n=73) and without (n=28) two consecutive ratings

| Characteristic | Responders | Non-responders |
|---|---|---|
| Age: years (s.d.) | 42.4 (11.0) | 40.1 (12.3) |
| Male: n (%) | 36 (49) | 12 (43) |
| White: n (%) | 55 (75) | 22 (79) |
| Psychosis: n (%) | 46 (63) | 14 (52) |
| Assessments: mean (s.d.) | ||
| Full-scale IQ | 100.7 (15.3) | 92.9 (13.2) |
| BPRS | 32.7 (8.4) | 35.2 (10.6) |
| MANSA | 4.3 (1.0) | 4.1 (1.0) |
| CANSAS–P | 4.3 (3.6) | 4.5 (2.5) |
| unmet | ||
The only significant difference between patients with and without two consecutive ratings was in premorbid IQ, and this difference did not alter the model that was developed (analysis not shown).
A scatter plot of quality of life and unmet need scores is shown in Fig. 1. A scatter plot of changes in these scores is shown in Fig. 2.
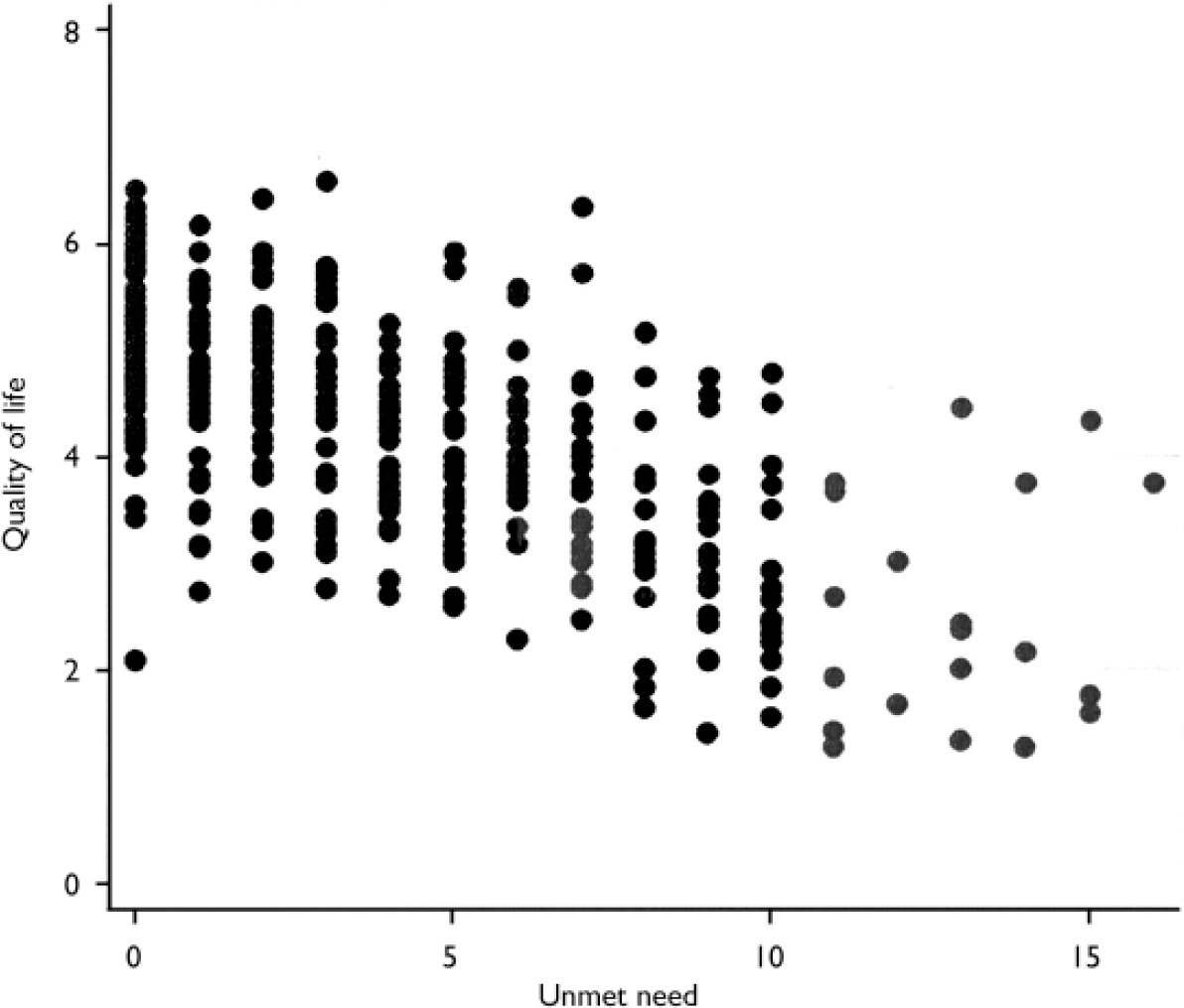
Fig. 1 Levels of quality of life and unmet need in 101 individuals using adult mental health services.
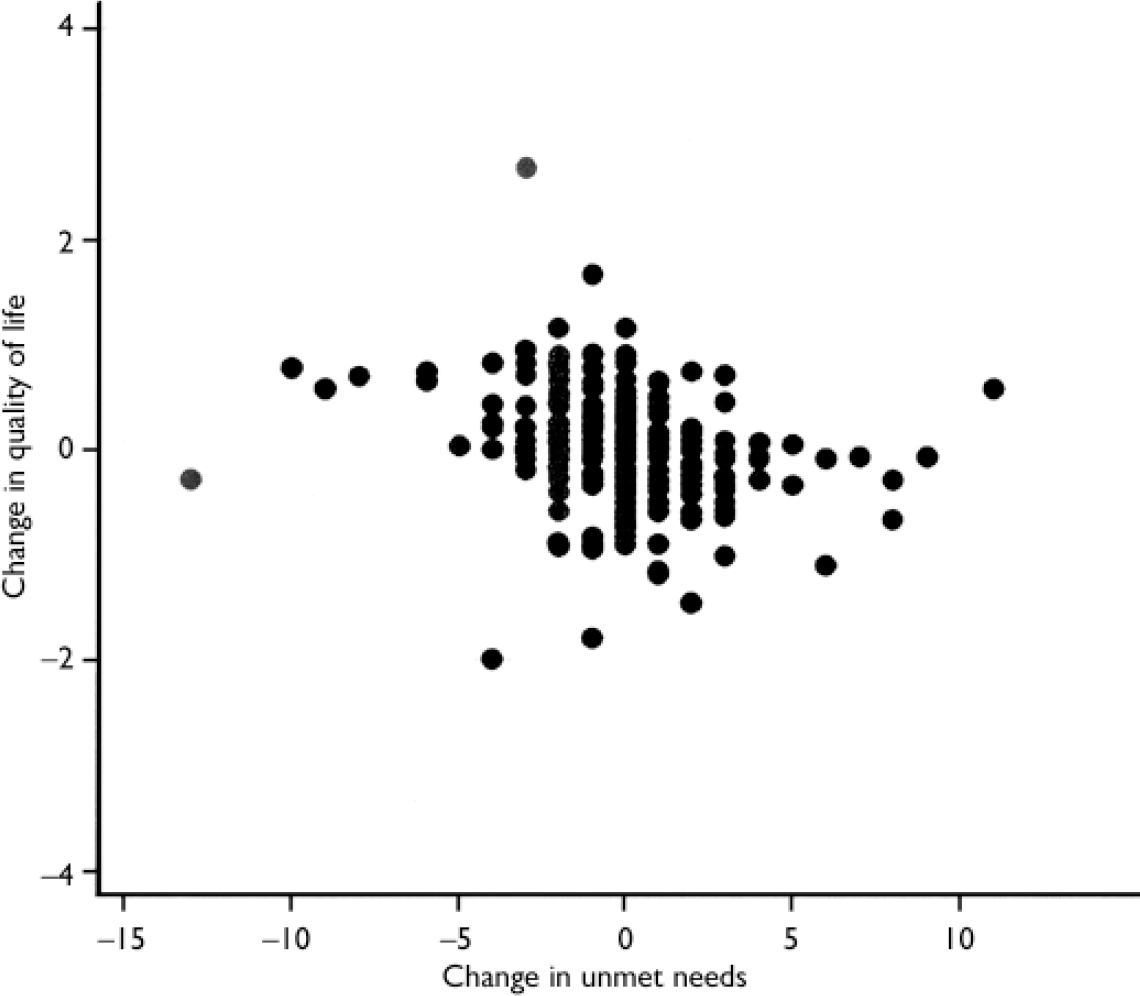
Fig. 2 Changes in quality of life and unmet need in 101 individuals using adult mental health services.
A total of 240 separate pairs of consecutive assessments was made by the 73 patients with at least two consecutive assessments. Using these data, three longitudinal random effects regression models were fitted (Table 2).
Table 2 Longitudinal regression analysis of quality of life (model 1), and with baseline socio-demographic (model 2) and socio-demographic and clinical (model 3) variables included

| Variable | Model 1 | Model 2 | Model 3 | |||
|---|---|---|---|---|---|---|
| B (95% CI) | P | B (95% CI) | P | B (95% CI) | P | |
| Mean level of unmet need | –0.26 (–0.31 to –0.21) | <0.001 | –0.27 (–0.32 to –0.22) | <0.001 | –0.23 (–0.29 to –0.17) | <0.001 |
| Change in unmet need over preceding month | –0.04 (–0.06 to –0.02) | <0.001 | –0.04 (–0.06 to –0.02) | <0.001 | –0.04 (–0.06 to –0.02) | <0.001 |
| Linear trend (month) | 0.02 (0.00–0.05) | 0.08 | 0.02 (0.00–0.05) | 0.10 | 0.02 (0.00–0.05) | 0.10 |
| Age | 0.01 (–0.01 to 0.02) | 0.38 | 0.01 (–0.01 to 0.02) | 0.47 | ||
| Gender (men v. women) | –0.07 (–0.40 to 0.25) | 0.67 | –0.03 (–0.35 to 0.28) | 0.83 | ||
| Ethnic group (White v. Black and minority) | –0.17 (–0.55 to 0.22) | 0.40 | –0.05 (–0.43 to 0.33) | 0.80 | ||
| Full-scale IQ | 0.00 (–0.02 to 0.01) | 0.44 | 0.00 (–0.02 to 0.01) | 0.46 | ||
| Diagnosis (psychosis v. other) | 0.35 (–0.03 to 0.72) | 0.07 | ||||
| Symptoms (BPRS) | –0.01 (–0.03 to 0.01) | 0.23 | ||||
| σu | 0.65 | 0.65 | 0.61 | |||
| σe | 0.34 | 0.34 | 0.34 | |||
| ρ | 0.78 | 0.79 | 0.76 | |||
| R 2 (within subjects) | 0.14 | 0.14 | 0.14 | |||
| R 2 (between subjects) | 0.56 | 0.59 | 0.62 | |||
| R 2 (overall) | 0.54 | 0.58 | 0.64 | |||
The σs indicate the amount of variation not explained in the regression model which can be attributed to individual differences (σu) and how much is random (σe). Rho is the percentage of the variation attributable to individual differences, showing that a substantial amount of the unexplained variance in quality of life was accounted for by individual factors which are stable over time.
DISCUSSION
This study investigated whether reducing patient-rated unmet need causes quality of life to improve. It is the first attempt to use repeated-measures data to assess association and direction (Reference BollenBollen, 1989) in the relationship. Two hypotheses were tested. First, level of unmet need averaged over all rounds was found to exert a strong effect on quality of life each time the patient assessed it. This extends previous work involving cross-sectional or two time-point data (UK700 Group, 1999; Reference Slade, Leese and TaylorSlade et al, 1999a ; Reference Wiersma and van BusschbachWiersma & van Busschbach, 2001; Reference Hansson, Sandlund and Bengtsson-TopsHansson et al, 2003; Reference Slade, Leese and RuggeriSlade et al, 2004). Second, change in patient-rated unmet need over the past month was found to exert a highly significant effect on quality of life (although the effect was weaker than for the average level of unmet need). This effect remains, and is in fact marginally strengthened, when controlling for clinical and socio-demographic characteristics. The model indicates that decreasing the level of unmet need by 12 would increase quality of life by half a point. Clinically, this implies that meeting all unmet needs will on average move half the patients into the next quality of life band, for example from mixed satisfaction to being mostly satisfied with life. Overall, these results extend previous work and are indicative of a causal relationship between patient-rated unmet need and quality of life (Reference BollenBollen, 1989).
Related research
Using the Bollen (Reference Bollen1989) criteria for causality, strong cross-sectional evidence and preliminary longitudinal evidence exists for association and isolation. Robust evidence from several studies across different countries and settings has shown higher unmet needs (especially when rated by the patient) to be cross-sectionally associated with lower subjective quality of life. The UK700 Study assessed needs in four urban sites in England from the perspective of staff only (UK700 Group, 1999). Subjective patient-rated quality of life was predicted more by unmet needs than any other clinical or social variable, in the sample of 620 patients. Unmet need alone accounted for 20% of the variance, whereas social variables accounted for only 7% and all other clinical variables only 19%. A study from the PRiSM Psychosis Study compared the relative contribution of 133 staff and patient assessments of needs (Reference Slade, Leese and TaylorSlade et al, 1999a ). The study found that a higher number of unmet needs was associated with lower quality of life (replicating the UK700 Study), and the association was more robust for patient ratings of need. A multicentre Scandinavian study of 418 patients with a diagnosis of schizophrenia found that patient-rated assessments of unmet need were associated with quality of life, accounting for 6% of the variance (Reference Hansson, Sandlund and Bengtsson-TopsHansson et al, 2003). Finally, a study of 101 long-term mental health patients in The Netherlands compared patient assessments of needs, quality of life and satisfaction (Reference Wiersma and van BusschbachWiersma & van Busschbach, 2001). Quality of life was not related to satisfaction with care, but was strongly associated with level of unmet need.
Overall, there is consistent cross-sectional evidence that higher patient-rated unmet need is associated with lower subjective quality of life, and that this relationship is not due to both these measures being assessed by the patient. However, all these studies have two characteristics which limit their generalisability. First, they are cross-sectional, so causal inferences are not possible. Second, they are based on data collected by researchers, rather than routinely as part of the clinical process. This is likely to improve the quality of data, but raises the question of whether any causal relationship found in research data necessarily also occurs in routine practice settings. These two issues were recently addressed in a retrospective re-analysis of existing data (Reference Slade, Leese and RuggeriSlade et al, 2004). The South Verona Outcome Project assesses needs, quality of life, symptoms, disability, function and service satisfaction in the context of a routine mental health service (Reference Ruggeri, Biggeri and RucciRuggeri et al, 1998). The re-analysis considered data for 265 patients, and (replicating previous findings) higher patient-rated unmet need was associated with lower subjective quality of life, even when controlling for the influence of all other clinical and socio-demographic variables (Reference Slade, Leese and RuggeriSlade et al, 2004). In addition, subjective quality of life was re-assessed 1 year later for a subset of 121 patients. The only baseline predictor of quality of life at 1-year follow-up (apart from baseline quality of life) was patient-rated unmet need, accounting for 58% of the variance in quality of life.
Strengths and limitations
A strength of the current study is that the population is epidemiologically representative of patients using adult community mental health teams in a demographically representative London borough. The inclusion criteria were broad to maximise external validity for community mental health teams which include heterogeneous diagnoses on their case-loads. Clinical diagnosis was not verified by assessment of a research diagnosis, since community mental health teams rely on clinical diagnosis.
The psychometric properties of MANSA and CANSAS were established using an interviewer to administer the measure. It is therefore possible that their administration through a postal questionnaire may compromise their psychometric properties. Similarly, although CANSAS–P was modified for this study from CANSAS, for which adequate psychometric properties have been demonstrated (Reference Phelan, Slade and ThornicroftPhelan et al, 1995; Reference Andresen, Caputi and OadesAndresen et al, 2000), the psychometric properties of CANSAS–P have not been established. The psychometric consequences for these measures of being self-administered by the patient are amenable to evaluation.
Another possible limitation relates to the sensitivity to change of quality of life. Ratings of quality of life were very stable – the mean rating on a scale from 1 to 7 was 4.25 for both intervention and control groups at baseline, and 4.27 and 4.20 for these two groups, respectively, at follow-up. This may indicate an insensitivity to change in quality of life – an undesirable property in a primary outcome measure. There is some evidence for a quality of life ‘equilibrium’ from the wider literature on quality of life. Cummins (Reference Cummins1995) investigated 16 general population studies of quality of life, and found a uniform population standard between 72.5 and 77.5% of the measurement scale maximum in all studies. The author noted that this is unlikely to be an artefact of the outcome measure since several different assessments were used. One proposed mechanism is the ‘standard drift fallacy’, a hypothesis proposing that patients with chronic disorders adjust their standards downwards to reduce the gap between their expectations and their achievements (Reference KatschnigKatschnig, 1997), leading to higher self-rated quality of life which appears similar to a community sample. However, the mean baseline MANSA score in the FOCUS Study was 54% of the scale maximum: lower than the 75% proposed by Cummins (Reference Cummins1995) and not consistent with the standard drift fallacy. More generally, other reviewers have concluded that quality of life changes do occur in general populations, and have specifically shown that changes in quality of life occur for mental health samples in more studies than not (Reference Evans and HuxleyEvans & Huxley, 2002).
Clinical implications
Despite these limitations, this study is the first to use repeated measures to investigate whether changes in patient-rated unmet need precede changes in quality of life. Evidence was found that this causal relationship exists, and that much of the remaining unaccounted variation in quality of life is due to individual factors which are stable over time. This finding has implications for the way in which mental health problems are understood, and consequently how mental health care is provided. This issue is complex, and has been conceptualised in a number of ways: causation v. meaning (Reference Bolton and HillBolton & Hill, 1996), idiographic v. nomothetic (Reference SchaferSchafer, 1999), and modernist v. post-modernist (Reference Bracken and ThomasBracken & Thomas, 2001). The framework which will be described here to illustrate the issue has been proposed by Long & Dixon (Reference Long and Dixon1996). They identified a spectrum of approaches to understanding mental health problems, ranging from patient-defined to professionally defined. At the extreme of the patient-defined end of the spectrum lies an understanding which emphasises the importance and uniqueness of individual experience, and accords no value to comparison of one person with another. The philosophical base for this understanding is post-modernism (Reference LaugharneLaugharne, 1999), and notions of consumerism, choice and user involvement are embraced. Correspondingly, the concepts of paternalism, professional expertise and mental illness are rejected. At the extreme of the professionally defined end of the spectrum lies an understanding which emphasises the importance of using scientific knowledge to make sense of abnormal mental experiences, and accords no value to the meaning attached by the patient to these experiences. The philosophical base for this understanding is positivism, and notions of evidence-based care, clinical judgement and compliance with treatment are embraced. Correspondingly, the concepts of patient choice about treatment and the idea of a continuum of mental health problems are rejected. Most clinical practice, of course, takes place within these extremes, but the point on the continuum will influence what interventions are provided, and what outcomes are targeted for change.
Specifically, if the goal of mental healthcare is to improve quality of life, then this study indicates that practice in mental health services may need to move more towards the patient-defined end of the spectrum proposed by Long & Dixon (Reference Long and Dixon1996). Interventions to reduce symptoms will still have an important role, but the characteristics of an evidence-based service will be a focus on the patient's perspective in assessment, the systematic identification of the full range of health and social care needs of the patient, the development of innovative services to address these needs, and the evaluation of the success of the service in terms of impact on quality of life. Staff in the service will require a negotiating style in their interactions, balancing what is asked for by the patient with staff assessment of what is in the patient's interest, staff assessment of what is in society's interest, and what is available. If the tension between these considerations becomes irreconcilable, then it may be necessary to prioritise the focus on meeting patient needs, by developing approaches to support patients in taking well-managed risks. The service would need to be based on and evaluated against a model of the intended effects of increased patient involvement, and such a model is currently lacking (Reference Crawford, Rutter and ManleyCrawford et al, 2002).
In summary, this study provides the first longitudinal evidence that high levels of patient-rated unmet need may actually cause low levels of quality of life. This might be because needs are the mediating link between quality of life and all, rather than simply the psychiatric, influences. Some unmet needs cannot be met, because they cannot be directly addressed (e.g. wanting a partner), they cannot be assessed fully (e.g. because the patient refuses to discuss the need), or no intervention is possible (e.g. because the appropriate service is unavailable, or the patient refuses help). However, some needs, once identified through assessment, can be met. Emerging evidence indicates that meeting patient-rated unmet needs should be the starting point for mental healthcare.
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
▪ Patients with high unmet need will tend to have low quality of life.
-
▪ Mental healthcare should be provided on the basis of patient-rated unmet need.
-
▪ Meeting unmet needs may cause quality of life to improve.
LIMITATIONS
-
▪ This is the first study investigating longitudinal change, and requires replication.
-
▪ Clinical diagnoses were not verified by research diagnoses.
-
▪ Some questionnaires were not designed for postal administration.
Acknowledgements
The Trial Steering Committee comprised Tom Burns, Rose McCabe, Paul McCrone, Mauricio Moreno and Chris Watkins. Data were collected by Matt Gillard, Lisa McNally, Alberto Parabiaghi, Preethi Premkumar and Giovanni Salvi. Administrative support was provided by Karen Langridge, Sarah Sheppard-Wright, Ally Smith, Michelle Wilkins and Roza Wojcik, and statistical support by Ian White. Jo Wardle made valuable comments on an earlier draft. Participating staff and service users in Croydon are thanked. The study was funded through a Medical Research Council Clinician Scientist Fellowship to M.S.







eLetters
No eLetters have been published for this article.