Much of the initial evidence concerning possible ‘toxic’ effects of duration of untreated psychosis (DUP) was based on post hoc inferences about groups of patients likely differing in DUP rather than having DUP directly measured or manipulated and related to outcome (Reference WyattWyatt, 1991). Within the past 10 years, there have been increasing reports (using retrospective and prospective designs) in which efforts are made to measure DUP and relate it to treatment outcome.
Estimating DUP is challenging given potential difficulties in dating onset of psychosis; establishing criteria for the initiation of effective treatment; the often intermittent or episodic nature of active psychosis; problems of retrospective reports; and discrepancies that can occur between patients and family or close associates in the observation of varying types of symptoms (Reference Norman and MallaNorman & Malla, 2001). Fortunately, in more recent publications reliability data are often provided (e.g. Reference Browne, Clarke and GervinBrowne et al, 2000; Reference Drake, Haley and AkhtarDrake et al, 2000; Reference Malla, Norman and ManchandaMalla et al, 2002a ), but there are still instances in which the methods for assessing DUP are not well described and/or reliability estimates not reported (e.g. Reference Altamura, Bassetti and SassellaAltamura et al, 2001). Footnote 1 For current purposes, we report only results of studies in which the measure of DUP attempts to reflect time from initial onset of positive psychotic symptoms to treatment as opposed to the delay from onset of any psychiatric symptoms (often referred to as duration of untreated illness or DUI). These studies were identified primarily from previous reviews (e.g. Reference Norman and MallaNorman & Malla, 2001), articles identified from MEDLINE and PSYCINFO related to duration of untreated psychosis as well as reference lists of articles identified using these methods.
METHOD
Is DUP correlated with treatment outcome?
Thirteen reports from independent databases examined whether DUP predicts time to remission of psychotic symptoms, such as hallucinations or delusions, or level of such symptoms after a set follow-up period, typically 6 months to 1 year (Reference Loebel, Lieberman and AlvirLoebel et al, 1992; Reference Szymanski, Cannon and GallacherSzymanski et al, 1996; Reference McGorry, Edwards and MihalopoulosMcGorry et al, 1996; Reference Scully, Coakley and KinsellaScully et al, 1997; Reference Haas, Garratt and SweeneyHaas et al, 1998; Reference Linszen, Lenior and De HannLinszen et al, 1998; Reference Wiersma, Nienhuis and SlooffWiersma et al, 1998; Reference Craig, Bromet and FenningCraig et al, 2000; Reference Ho, Andreasen and FlaumHo et al, 2000; Reference Larsen, Moe and Vibe-HansenLarsen et al, 2000; Reference Black, Peters and RuiBlack et al, 2001; Reference Verdoux, Liraud and BergeyVerdoux et al, 2001; Reference Malla, Norman and ManchandaMalla et al, 2002a ). Of these, nine reports found statistically significant relationships between longer DUP and longer time to remission or lower level of positive symptoms at follow-up. In addition, Drake et al (Reference Drake, Haley and Akhtar2000) report shorter DUP correlating with total symptoms after 6–12 weeks of treatment. Examining the strength of the relationships as estimated either using correlations reported in the above reports or through post hoc calculation of effect size correlations (Reference Rosnow and RosenthalRosnow & Rosenthal, 1996), we obtain a range of estimates (0.09–0.50) which generally tend to cluster around 0.30.
Several factors might account for inconsistencies in findings between these studies. For instance, the distribution of DUP tends to have a marked positive skew, suggesting the appropriateness of transformations or non-parametric analyses. Three of the four non-significant findings did not do so (Reference Scully, Coakley and KinsellaScully et al, 1997; Reference Linszen, Lenior and De HannLinszen et al, 1998; Reference Craig, Bromet and FenningCraig et al, 2000); on the other hand, some studies that found a significant relationship do not report using such procedures (e.g. Reference Larsen, Moe and Vibe-HansenLarsen et al, 2000; Reference Black, Peters and RuiBlack et al, 2001). Non-significant reports may also be a result of a restricted range of DUP (e.g. Reference Linszen, Lenior and De HannLinszen et al, 1998); combining data for patients who may vary widely in the treatment received (Reference Craig, Bromet and FenningCraig et al, 2000) or possible marked difficulties in estimating DUP using very distant historical data (e.g. Reference Scully, Coakley and KinsellaScully et al, 1997). One must be cautious in undertaking such post hoc explanations for discrepancies. At this point, however, a majority of relevant studies are reporting significant bivariate relationships between DUP and level of initial recovery from positive symptoms over the first year or so.
Three publications have examined whether DUP is related to likelihood of relapse once remission has been attained. Altamura et al (Reference Altamura, Bassetti and Sassella2001), in a retrospective study, found that patients with apparently short DUP were less likely to have a multi-episode course. Prospective studies by Robinson et al (Reference Robinson, Woerner and Alvir1999) and Linszen et al (Reference Linszen, Lenior and De Hann1998) did not find DUP to predict relapse.
Of ten reports (again using independent databases) examining the relationship of DUP to negative symptoms outcomes (Reference Szymanski, Cannon and GallacherSzymanski et al, 1996; Reference Scully, Coakley and KinsellaScully et al, 1997; Reference Haas, Garratt and SweeneyHaas et al, 1998; Reference Linszen, Lenior and De HannLinszen et al, 1998; Reference Edwards, McGorry and WaddellEdwards et al, 1999; Reference Craig, Bromet and FenningCraig et al, 2000; Reference Ho, Andreasen and FlaumHo et al, 2000; Reference Larsen, Moe and Vibe-HansenLarsen et al, 2000; Reference Black, Peters and RuiBlack et al, 2001; Reference Malla, Norman and ManchandaMalla et al, 2002a ), four (Reference Scully, Coakley and KinsellaScully et al, 1997; Reference Haas, Garratt and SweeneyHaas et al, 1998; Reference Edwards, McGorry and WaddellEdwards et al, 1999; Reference Larsen, Moe and Vibe-HansenLarsen et al, 2000) have shown a significant relationship. The strength of the relationship for DUP and negative symptoms may be somewhat less than that for positive symptoms, with an average correlation in the low 0.20s.
The few reports examining possible relationships between DUP and social functioning during follow-up have yielded inconsistent results (cf. Reference McGorry, Edwards and MihalopoulosMcGorry et al, 1996; Reference Ho, Andreasen and FlaumHo et al, 2000; Malla et al, Reference Malla, Norman and McLean2001, Reference Malla, Norman and Manchanda2002b ).
On the whole, the current evidence suggests there is frequently a bivariate relationship between DUP and time to or level of remission of positive symptoms, although there may be less consistency with respect to DUP predicting level of negative symptoms after treatment and/or likelihood of relapse after remission.
Is there a confound?
It is important to examine whether any relationship that does exist between DUP and outcome could be explained by other confounding factors which have in the past been found to predict treatment outcome. With respect to gender, Loebel et al (Reference Loebel, Lieberman and Alvir1992) and Larsen et al (Reference Larsen, McGlashan and Moe1996) report males having a longer DUP than females, but five other studies did not find a difference (Reference Haas, Garratt and SweeneyHaas et al, 1998; Reference Browne, Clarke and GervinBrowne et al, 2000; Reference Drake, Haley and AkhtarDrake et al, 2000; Reference Ho, Andreasen and FlaumHo et al, 2000; Reference Black, Peters and RuiBlack et al, 2001). Ho et al (Reference Ho, Andreasen and Flaum2000) found that longer DUP significantly related to younger age of onset, but six studies did not (Reference Haas and SweeneyHaas & Sweeney, 1992; Reference Loebel, Lieberman and AlvirLoebel et al, 1992; Reference Larsen, McGlashan and MoeLarsen et al, 1996; Reference Haas, Garratt and SweeneyHaas et al, 1998; Reference Black, Peters and RuiBlack et al, 2001; Reference Kalla, Aaltonen and WahlstromKalla et al, 2002). Several studies have reported longer DUP to be associated with higher levels of at least some aspects of negative or deficit symptoms at presentation for treatment (Reference Larsen, McGlashan and MoeLarsen et al, 1996; Reference Browne, Clarke and GervinBrowne et al, 2000; Reference Black, Peters and RuiBlack et al, 2001; Reference Malla, Takhar and NormanMalla et al, 2002c ). Drake et al (Reference Drake, Haley and Akhtar2000) found a relationship between longer DUP and higher positive but not negative symptoms at presentation, but others have found no relation of DUP to initial positive symptoms (e.g. Reference Larsen, McGlashan and MoeLarsen et al, 1996; Reference Malla, Norman and ManchandaMalla et al, 2002a ). DUP is not systematically related to substance use/misuse or adherence to medication (Reference Drake, Haley and AkhtarDrake et al, 2000; Reference Norman and MallaNorman & Malla, 2002). It is important to note, however, that significant relationships of DUP to outcome generally remain when such factors as age at onset, gender and baseline symptoms are entered as predictors (e.g. Reference McGorry, Edwards and MihalopoulosMcGorry et al, 1996; Reference Szymanski, Cannon and GallacherSzymanski et al, 1996; Reference Altamura, Bassetti and SassellaAltamura et al, 2001; Reference Harrigan, McGorry and KrstevHarrigan et al, 2003).
Although several studies have found DUP and indices of premorbid adjustment are not significantly correlated (Reference Loebel, Lieberman and AlvirLoebel et al, 1992; Reference Browne, Clarke and GervinBrowne et al, 2000; Reference Ho, Andreasen and FlaumHo et al, 2000); others have found lower premorbid adjustment to be significantly associated with longer DUP (Reference Verdoux, Bergey and AssensVerdoux et al, 1998; Reference Malla, Norman and ManchandaMalla et al, 2002a ). Any index of premorbid adjustment based on the individual's behaviour close to the onset of psychosis may actually reflect the impact of the symptoms, whereas the use of premorbid adjustment indices based on behaviour earlier in life, such as childhood or early adolescence, are less likely to reflect active psychosis. Malla et al (Reference Malla, Norman and Manchanda2002a ) found that DUP predicted level of positive symptoms at 1 year independently of childhood or early adolescent premorbid adjustment. Larsen et al (Reference Larsen, Moe and Vibe-Hansen2000) entered gender and premorbid adjustment for childhood, early adolescence, late adolescence, or adulthood into a regression equation before DUP and found that only the latter significantly predicted symptoms 1 year after initiation of treatment. In a 10-year follow-up of an epidemiological first-episode cohort, White et al (further details available from S.W.L. on request) found both premorbid adjustment and DUP to be independent predictors of symptomatic and functional outcomes. Verdoux et al (Reference Verdoux, Liraud and Bergey2001) report data suggesting that premorbid adjustment might account for the relationship of DUP to outcome. It should be noted, however, that Verdoux et al used the best level of the Global Assessment of Functioning Scale (GAF) for any month in the year preceding hospitalisation as the index of premorbid adjustment and clearly such an index could reflect the impact of untreated psychosis. These authors tried to address this possibility by excluding from their analysis patients with a DUP longer than 12 months – but this has the effect of reducing the potential of DUP to predict by truncating its range.
The interpretation of findings with respect to premorbid adjustment as a possible explanation for any relation between DUP and treatment outcome is potentially complex. Does poor premorbid adjustment lead to worse outcome and also result in longer DUP with the relationship between the latter two variables being spurious? Is the correlation of premorbid adjustment with outcome largely reflecting the influence of untreated psychosis? Are both having independent effects? In a recent report, Harrigan et al (Reference Harrigan, McGorry and Krstev2003) demonstrate that in a large sample of patients with first-episode psychosis, the effects of DUP on several dimensions of outcome are independent of premorbid adjustment prior to the onset of prodromal or psychotic symptoms. In multiple regression equations that included premorbid adjustment, gender, prodrome duration, diagnosis, age at onset and severity of drug use, DUP remained a significant (and relatively important) predictor of 12-month outcome scores on a quality of life scale as well as negative and positive symptoms. Furthermore, Drake et al (Reference Drake, Haley and Akhtar2000) and Harrigan et al (Reference Harrigan, McGorry and Krstev2003) have reported comparable dose–response curves for the effects of DUP on outcome.
Ho et al (Reference Ho, Andreasen and Flaum2000) have suggested that reports that find a relationship between DUP and outcome may be confounded by diagnosis, particularly the difference between affective psychosis and schizophrenia-spectrum disorders. There are now several reports that find DUP to predict treatment response in samples which do not include patients with affective psychoses (e.g. Reference Larsen, Moe and Vibe-HansenLarsen et al, 2000; Reference Black, Peters and RuiBlack et al, 2001; Reference McGorry, Harrigan and AmmingerMcGorry et al, 2001; Reference Harrigan, McGorry and KrstevHarrigan et al, 2003). It has also been suggested that inclusion of schizophreniform psychosis and other diagnoses with lower duration thresholds than schizophrenia may distort the relationship between DUP and outcome (Reference Ho, Andreasen and FlaumHo et al, 2000). The number of individuals with such diagnoses that are present in samples examining DUP is generally quite small (e.g. Reference Larsen, Moe and Vibe-HansenLarsen et al, 2000; Reference Black, Peters and RuiBlack et al, 2001; Reference Malla, Norman and ManchandaMalla et al, 2002a ). Furthermore, such an argument assumes that there is a fundamental difference in the pathophysiology of such diagnoses. The primary characteristic that distinguishes schizophreniform psychosis from schizophrenia is the duration of psychotic symptoms (Reference Zarafe, Tohen and LandZarafe et al, 2000) and so elimination of patients with such a diagnosis would not be consistent with examining the impact of the full range of DUP.
What are likely mediators of any effects of DUP?
The postulate of ongoing neurodegenerative processes in psychosis is controversial, although there is evidence consistent with there being neuroanatomical changes associated with the onset of and continuation of psychotic disorders (e.g. Reference Velakoulis, Wood and SmithVelakoulis et al, 2001; Reference Pantelis, Velakoulis and McGorryPantelis et al, 2003). Several publications have found no relationship between measures of brain morphology and DUP (Reference Fannon, Chitnis and DokuFannon et al, 2000; Reference Hoff, Sakuma and RaziHoff et al, 2000; Reference Malla, Mittal and LeeMalla et al, 2002d ; Reference Ho, Alicata and WardHo et al, 2003). Madsen et al (Reference Madsen, Karle and Rubin1999) report DUP to be positively associated with extent of frontal sulcal enlargement at first admission and Keshavan et al (Reference Keshavan, Haas and Kahn1998) found DUP to be inversely related to the volume of the left superior temporal gyrus.
Barnes et al (Reference Barnes, Hutton and Chapman2000), Hoff et al (Reference Hoff, Sakuma and Razi2000) and Norman et al (Reference Norman, Townsend and Malla2001) found DUP unrelated to performance on a variety of neurocognitive tests. Amminger et al (Reference Amminger, Edwards and Brewer2002) reported longer DUP to be related to an index of cognitive deterioration (based on ‘hold’ v. ‘no hold’ indices of performance), but Norman (Reference Norman2002) did not find DUP to be related to the same index in other data. In the most recent report relevant to DUP and cognitive functioning, Joyce et al (Reference Joyce, Hutton and Mutsatsa2002) found DUP unrelated to level of performance on tasks assessing planning, spatial memory or pattern recognition; but did find shorter DUP related to performance on a task requiring shifting attention from one dimension of a stimulus to another – which is postulated to particularly reflect prefrontal functioning.
On the whole, the results with reference to structural and neurocognitive functioning and DUP are mixed. Several studies on neurotoxicity in relation to DUP have used small samples, but sample size does not seem to have a clear relationship to the likelihood of significant findings. To the extent that the data provide any evidence of a neurotoxic effect of untreated psychosis, it seems most likely to emerge with reference to frontal or temporal lobe deterioration and frontal cognitive performance. These correspond to the areas implicated in recent longitudinal studies of changes associated with onset of psychosis (e.g. Reference Pantelis, Velakoulis and McGorryPantelis et al, 2003).
Any ‘toxic’ effects of untreated psychosis are not necessarily mediated through the neural domain. Longer periods of untreated illness could lead to disruptions in social support and it is certainly conceivable that DUP might have effects mediated through reduced self-confidence, increased hopelessness or engulfment, or pre-treatment disruption of education or vocation, all of which could have an impact on treatment outcome.
Other sources of evidence
Definitive evidence of a causal relationship between DUP and clinical outcome could only come from a randomised control trial comparing earlier and later detection and treatment. Although using such a design would be challenging, McGorry (Reference McGorry2000) argues that it might be feasible under some circumstances. An alternative is the use of quasi-experimental designs comparing treatment results for geographical regions in which differences have been introduced in infrastructure for early detection and treatment and/or historical control design that contrast outcomes for patients before and after such system changes. Up to this point, the most noteworthy study of this sort is probably the TIPS trial (Reference Johannessen, McGlashan and LarsenJohannessen et al, 2001) in which geographical regions were pseudo-randomised to receive an intensive public education campaign plus an early detection service or conventional care. Preliminary reports suggest that both DUP and clinical severity at presentation for treatment have been significantly reduced in the experimental district. No outcome data have yet been reported and interpretation of findings may be challenging (Reference McGorryMcGorry, 2000; Reference Larsen, Friss and HaahrLarsen et al, 2001). It is particularly important to guard against the possibility that interventions designed to reduce DUP do not improve outcome primarily through increased detection of cases that naturally have a more benign course.
DISCUSSION
What are the implications for early intervention?
There is certainly evidence consistent with the postulated relationship of DUP to outcome during the first year or so of treatment. This relationship appears to generally be independent of other predictors of outcome. There is certainly a need for longer-term follow-up studies and the results of quasi-experimental controlled designs could be especially valuable. In Fig. 1 (from Reference Drake, Haley and AkhtarDrake et al, 2000) there is evidence for a non-linear dose–response relationship between DUP and clinical symptoms after treatment. Harrigan et al (Reference Harrigan, McGorry and Krstev2003) have reported a very similar relationship for DUP and longer-term quality of life after treatment. Both studies suggest that any gains from reducing DUP (assuming a causal relationship) are likely to be greater if the reduction occurs early in psychosis (for instance, reduction from 3 to 2 months) than later (reduction from 2 years to 1 year). It is also important to recognise that current approaches to the measurement of DUP may be missing substantial aspects of any untreated disease process which might be better reflected in symptoms pre-dating frank psychotic experiences (Reference HafnerHafner, 2000).
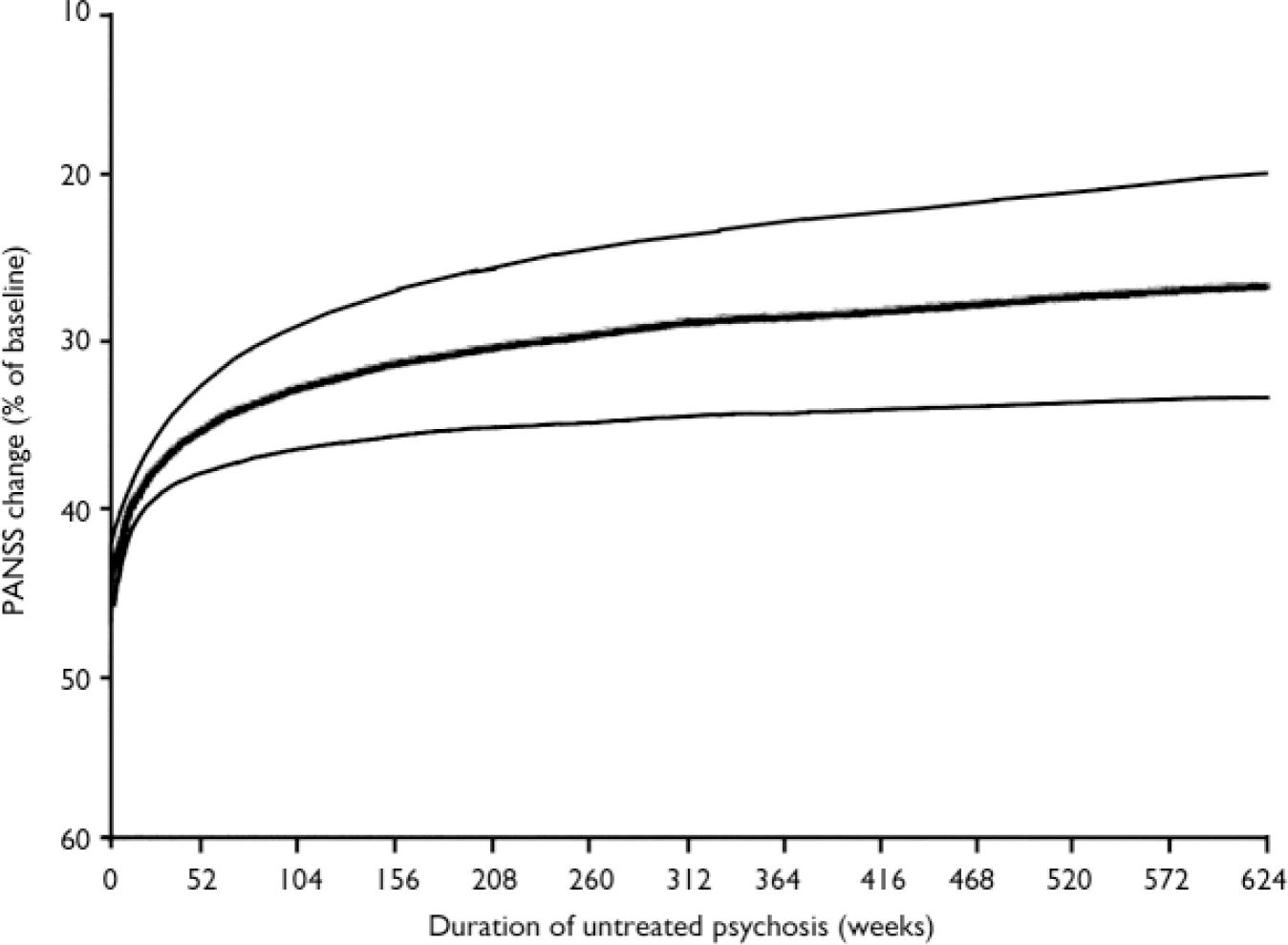
Fig. 1 Predicted change in Positive and Negative Syndrome Scale (PANSS) against duration of untreated psychosis (with 95% Cls) (from Reference Drake, Haley and AkhtarDrake et al, 2000).
Certainly, DUP is not the only influence on treatment outcome. As McGorry (Reference McGorry2000) suggests, the early intervention field must maintain a balance between enthusiasm and sound research evidence, avoiding unjustified zealotry or scepticism. A balance must also be maintained between a focus on intervening early and intervening well (Reference Carbone, Harrigan and McGorryCarbone et al, 1999; Reference Malla and NormanMalla & Norman, 2001). A major legacy of the early intervention movement is increased optimism and enthusiasm concerning the treatment of psychotic disorders. These must be channelled not only into providing earlier treatment, but also into developing and evaluating interventions that better meet the needs of patients and families.
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
▪ Duration of untreated psychosis (DUP) is frequently an independent predictor of treatment response, particularly remission of positive symptoms.
-
▪ Efforts to decrease delay in treating individuals with clearly established psychotic disorders are justified, not just by the immediate reduction in symptoms, but by potential improvement in treatment outcome.
-
▪ DUP is certainly not the only influence on treatment outcome, so efforts to treat earlier should not become the sole focus of early intervention programmes.
LIMITATIONS
-
▪ Relevant evidence is of a correlational nature relating naturally occurring variation in DUP to treatment outcome, so causal inferences cannot be made with certainty.
-
▪ There have been comparatively few studies that have examined the relationship of DUP to level of functioning and quality of life after treatment.
-
▪ Measurement of DUP is challenging and, therefore, correlational findings may sometimes underestimate its influence on outcome.




eLetters
No eLetters have been published for this article.