Electroconvulsive therapy (ECT) is an effective treatment for patients with depression, but patients are prone to relapse during the first weeks and by 6 months more than a third of patients have relapsed.Reference Jelovac, Kolshus and McLoughlin1–Reference Hermida, Glass, Shafi and McDonald4 Suicide is a potential consequence of relapse. Lithium may decrease the risk of suicide for patients with unipolar depression,Reference Cipriani, Hawton, Stockton and Geddes5 but the effect of lithium on suicide risk specifically following ECT is unknown. Older age, being married, the presence of psychotic features, continuation ECT and treatment with antidepressants are associated with a reduced risk of relapse after ECT. Substance use disorder, antidepressant medication resistance, benzodiazepine treatment and medication with antipsychotics for patients without psychotic features correlate with an increased risk.Reference Sackeim, Haskett, Mulsant, Thase, Mann and Pettinati2,Reference Sackeim, Prudic, Devanand, Decina, Kerr and Malitz6–Reference Rasmussen11
For bipolar depression lithium is efficient at preventing relapse, but for unipolar depression the effect has not been clearly established.Reference Geddes, Burgess, Hawton, Jamison and Goodwin12,Reference Bauer, Adli, Ricken, Severus and Pilhatsch13 Lithium decreased the relapse risk after ECT in a few studies.Reference Sackeim, Haskett, Mulsant, Thase, Mann and Pettinati2,Reference Coppen, Abou-Saleh, Milln, Bailey, Metcalfe and Burns14 Nevertheless, only a minority of patients in clinical practice receive lithium following ECT for unipolar depression. This could partly be because of the uncertain protective effect of lithium after ECT. A list of published studies on the effect of lithium after ECT was compiled by Rasmussen.Reference Rasmussen11 It includes two studies where patients have been randomised to use lithium after ECTReference Sackeim, Haskett, Mulsant, Thase, Mann and Pettinati2,Reference Coppen, Abou-Saleh, Milln, Bailey, Metcalfe and Burns14 and four cohort studies where the association between relapse and lithium was reported.Reference Nordenskjold, von Knorring and Engstrom9,Reference Perry and Tsuang15–Reference Atiku, Gorst-Unsworth, Khan, Huq and Gordon17 The numbers of patients treated with lithium in the two randomised trials were 28 and 18, and 50 in the largest cohort study.Reference Sackeim, Haskett, Mulsant, Thase, Mann and Pettinati2,Reference Nordenskjold, von Knorring and Engstrom9,Reference Coppen, Abou-Saleh, Milln, Bailey, Metcalfe and Burns14 Larger studies are required to verify the effects of lithium after ECT in order to guide patients and clinicians in their choices of prophylactic treatments. Our study aims to quantify the effect of lithium on suicide and hospital readmission after ECT for unipolar depression in a clinical population of psychiatric in-patients. A secondary aim was to identify factors that are associated with suicide and hospital readmission.
Method
Design
This study was a register-based cohort study of in-patients who received ECT for the treatment of depression. Several Swedish population-based registers were compiled using the Swedish personal identity number. The outcomes were suicide rate and time to hospital readmission.
Participants
All patients in the Swedish National Quality Register for ECT who had received index ECT for unipolar depression (diagnosis codes: F321, F322, F323, F331, F332, or F333 according to the Swedish version of ICD-10-SE) between 2011 and 2016, and were registered as in-patients in the Swedish National Patient Register at the start of the treatment series were considered for inclusion in the study.18 If an individual had received several treatment series during the time period only the first one was selected. Exclusion criteria were age under 18 years of age, readmission on the same day as discharge, death registered before or on the day of discharge, or incomplete data on marital status.
Follow-up
Start of follow-up was calculated as the discharge date or end of ECT series, whichever came last. End of follow-up was the date of readmission to a hospital for a psychiatric diagnosis (ICD-10-SE Chapter F), death or the end of 2016, whichever came first.
Data management
Data was obtained from several registers. Information was linked by Statistics Sweden and the Swedish National Board of Health and Welfare using the Swedish personal identity number.
(a) The Swedish National Patient Register contains data on all public and private hospital admissions in Sweden. The registry has a high coverage, with 99% of all hospital discharges registered.Reference Ludvigsson, Andersson, Ekbom, Feychting, Kim and Reuterwall19 This database was used to obtain information on suicide attempts, post-traumatic stress disorder, attention-deficit hyperactivity disorder, anxiety disorder, obsessive–compulsive disorder, autism, personality disorder, substance use disorder and psychosis before admission.
(b) The Swedish Prescribed Drug Register, contains records of all prescription medications sold in Sweden since July 2005.20 This database was used to identify collection of any of the following medications within 100 days after the end of ECT: antidepressants, antiepileptics, antipsychotics, anxiolytics, benzodiazepines, central stimulants, lamotrigine, lithium, quetiapine and valproate. If follow-up time was shorter than 100 days collections before admission for 100 minus the number of follow-up days was also checked. This database was also used to identify medications obtained in the year before the start of ECT series, and this information was used to complete a version21 of the Antidepressant Treatment History Form (ATHF).Reference Oquendo, Baca-Garcia, Kartachov, Khait, Campbell and Richards22
(c) The Longitudinal Integration Database for Health Insurance and Labour Market Studies contains information on social and demographic factors and is compiled on a yearly basis.23 This database was used to obtain information on patient, gender, age, education, marital status and employment status in the year before ECT.
(d) The Swedish Cause of Death Register contains, the dates and causes of deaths as determined by a physician, including suicides (ICD codes X60–X84 and Y10–Y34), for all individuals in Sweden and all Swedish residents who die in a foreign country.Reference Brooke, Talback, Hornblad, Johansson, Ludvigsson and Druid24
(e) The Swedish National Quality Register for ECT contains information on ECT treatment series and the patients receiving treatment. The register had a coverage of 85% of all ECT in Sweden in 2013.Reference Nordanskog, Hulten, Landen, Lundberg, von Knorring and Nordenskjold25 This database was used to obtain information on the number of ECT in series, pulse width, frequency, duration, electric current, electrode placement, Clinical Global Impression (GGI)Reference Guy26 severity before treatment, CGI improvement and continuation ECT.
With the exception of marital status, missing values for categorical variables were identified and coded as a separate category. For marital status, patients with missing data were excluded.
ATHF
The ATHF was used to evaluate the pharmacological treatment for depression in the year before ECT.Reference Oquendo, Baca-Garcia, Kartachov, Khait, Campbell and Richards22 The ATHF quantifies which types of antidepressant treatments and how much of each type a patient has used. Medication dosage was used rather than blood levels. A single dispensing of a drug was taken to indicate a usage of less than 4 weeks. Two or more dispensations were taken to indicate usage of 4 weeks or more. The following changes were made from the original ATHF:
(a) collections of fluoxetine and citalopram were counted separately and not combined;
(b) tranylcypromine was combined with isocarboxazid (same categories as for isocarboxazid);
(c) usage of ECT and lithium as an augmenting agent was not considered;
(d) levomepromazine, alimemazine, and promethazine were added with one point for any dispensation;
(e) vortioxetine was added with one point for one dispensation or multiple dispensation with doses <5 mg/day, two points for multiple dispensations with doses 5–9 mg/day, three points for multiple dispensations with doses 10–19 mg/day and four points for multiple dispensations with doses ≥19 mg/day;
(f) agomelatine was added with one point for a single dispensation or multiple dispensations with doses under 15 mg/day, two points for multiple dispensations with doses 15–35 mg/day, three points for multiple dispensations with doses 35–65 mg/day and four points for multiple dispensations with doses ≥65 mg/day;
(g) escitalopram was added with one point for a single dispensation or multiple dispensations with doses <5 mg/day, two points for multiple dispensations with doses 5–10 mg/day, three points for multiple dispensations with doses 10–20 mg/day and four points for multiple dispensations with doses >20 mg/day;
(h) duloxetine was added with one point for a single dispensations or multiple dispensation with doses <30 mg/day, two points for multiple dispensations with doses 30–39 mg/day, three points for multiple dispensations with doses 40–59 mg/day and four points for multiple dispensations with doses ≥60 mg/day or more;
(i) reboxetine was added with one point for a single dispensation or multiple dispensations with doses <4 mg/day, two points for multiple dispensations with doses 4–7 mg/day, three points for multiple dispensations with doses 8 mg/day and four points for multiple dispensations with doses ≥8 mg/day.
Statistics
Chi-square tests and descriptive statistics were used to characterise the data. For sparse data Fisher's exact tests were used instead of χ2. Kaplan–Meier plots and survival analysis using proportional hazards Cox regression was performed to estimate differences in time to suicide and readmission between groups based on treatment, social and individual background factors. Both unadjusted and adjusted models were used. The adjusted model included the variables listed in supplemenary Table 1 available at https://doi.org/10.1192/bjo.2019.37. If Cox estimates could not be calculated because of few (or most) of the patients having the outcome, pairwise Fisher's exact tests were used instead. Models stratified by use of antidepressants and lithium use were used to investigate if the effect of lithium/antidepressant use differed between those with and without antidepressant/lithium use. Models with interaction effects between lithium and antidepressants were generated. Numbers needed to treat were calculated from the adjusted Cox model. In addition, times to death by non-suicide causes between lithium and non-lithium users were calculated.
In separate analysis, the outcome of time to suicide using the same follow-up period as in readmission analysis but with time to suicide as the outcome with censoring for hospital readmission, non-suicide death and the end of 2016 was analysed.
Ethics
The study was approved by the regional ethics vetting board in Uppsala, registration number 2014/174. This was a register-based study and no informed consent was collected from the participants. The patients could choose to not be included in the Swedish National Quality Register for ECT.
Results
There were 7569 individuals who met the inclusion criteria. Twelve patients were excluded because they died on the day of discharge, 203 because they were readmitted on the day of discharge, 8 because they were under the age of 18 years, and 8 because they had missing information on marital status. The remaining 7350 patients were included in the analysis.
Characteristics of the cohort are shown in supplementary Table 2. Among the 7350 patients included in the analysis 638 (9%) collected lithium in connection with ECT. A history of suicide attempts was more common among patients who had collected lithium than among patients who had not collected lithium (30% v. 22%). Collection of lamotrigine and quetiapine was also more common among patients who had collected lithium than among those who had not collected lithium (14% v. 8% for lamotrigine and 23% v. 16% for quetiapine). A list of the latest suicide attempts before ECT can be found in supplementary Table 3.
Mean follow-up time was 1.4 years (s.d. = 1.5) for patients who collected lithium in connection with ECT treatment and 1.3 years (s.d. = 1.4) for patients who did not. The outcome was readmission for 4203 patients, death by suicide for 56 patients and death from other causes for 105 patients. The remaining 2986 patients did not have these outcomes until the end of follow-up on 31 December 2016. Details of the readmission diagnoses among patients with and without lithium treatment are available in supplementary Table 4.
Death by suicide
There were no suicides in the group that used lithium. A Fisher's test showed that patients who used lithium after ECT were less likely to die by suicide than patients who did not use lithium (Fisher's exact test P = 0.014). In the analysis of time to suicide men were more likely to die by suicide than women (hazard ratio (HR) = 2.13, 95% CI 1.20–3.77), widowed patients were more likely to die by suicide than married patients (HR = 4.27, 95% CI 1.43–12.70), patients with a substance use disorders were more likely to die by suicide than patients without substance use disorder (HR = 2.07, 95% CI 1.03–4.15) and patients with a history of suicide attempts were more likely to die by suicide than patients without a history of suicide attempts (HR = 2.65, 95% CI 1.41–5.00) (supplementary Table 5). There was no statistically significant difference in time to non-suicidal death between patients with and without lithium (HR = 0.37, 95% CI 0.12 –1.18).
Hospital readmission
Fig. 1 and supplementary Table 1 show associations and hazard ratios (HRs) for exposure and background factors for time to readmission. Among both those who collected lithium and those who did not 57% were readmitted. Number of previous admissions for psychiatric diagnoses associated strongly with time to readmission. Of the patients without earlier records of in-patient care with a psychiatric main diagnosis 46% were readmitted before the end of the study, whereas for patients with 31–140 previous admissions with a psychiatric main diagnosis the corresponding percentage was 91%.
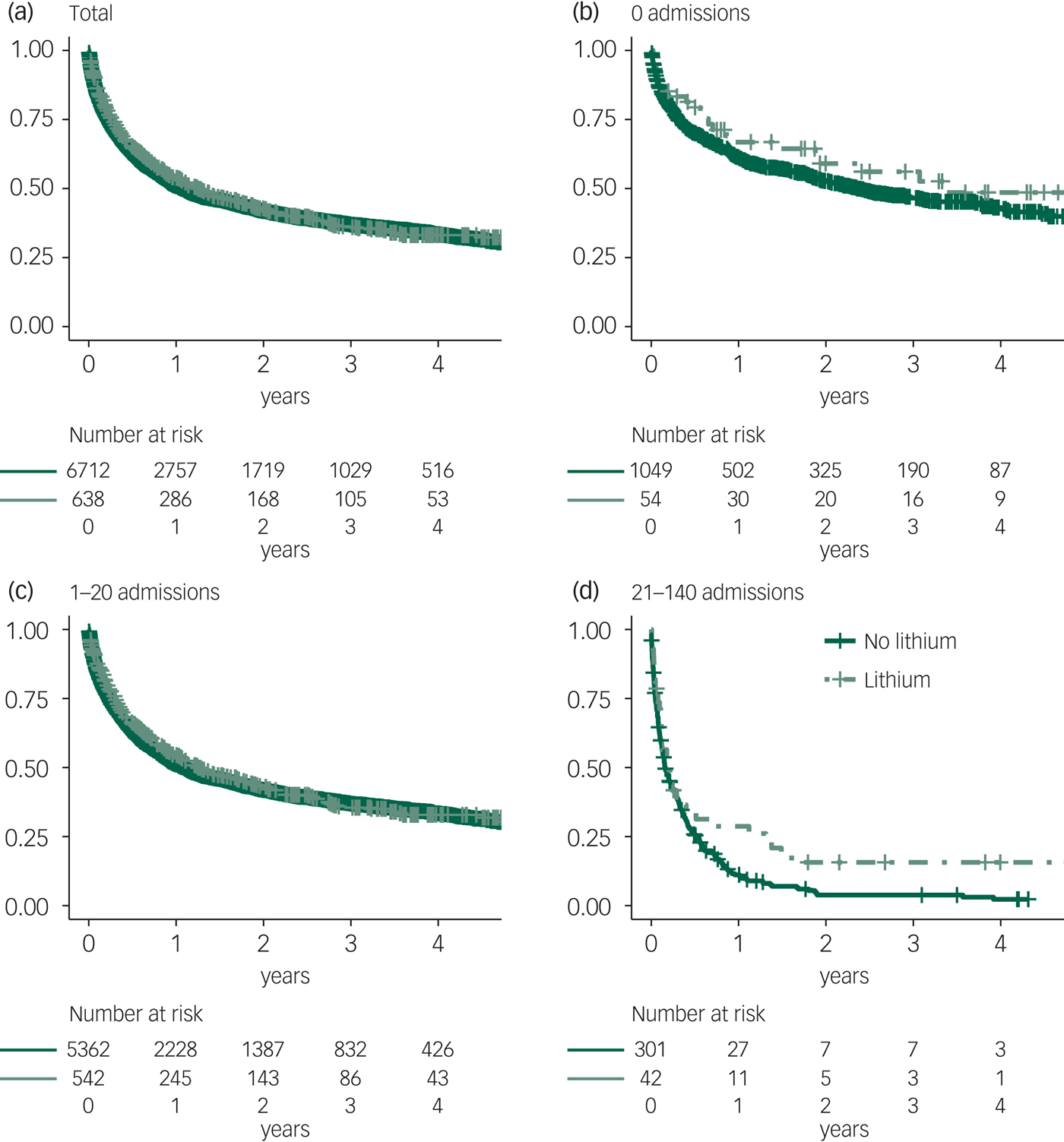
Fig. 1 Time to hospital readmission for patients using lithium after electroconvulsive therapy and those not using lithium, stratified by the number of earlier hospital admissions for psychiatric care.
In the adjusted model, patients who collected lithium had a lower risk of readmission than patients who did not collect lithium (HR = 0.84, 95% CI 0.75–0.93). The number of patients who needed to be treated with lithium to prevent one readmission was 16 (95% CI 10–38). Patients aged 18–29 years, were more likely to be readmitted than older patients. Divorced patients were more likely to be readmitted than married or cohabiting patients, and unemployed patients were more likely to be readmitted than employed patients. Patients with a history of anxiety were more likely to be readmitted than patients without diagnosed anxiety disorder. Patients with psychotic depression were less likely to be readmitted than patients with non-psychotic depression. Patients who were scored as severely ill or among the most severely ill prior to ECT were more likely to be readmitted than patients with less severe symptoms prior to ECT. Patients who were minimally improved, did not change or got worse after ECT were more likely to be readmitted than patients who were very much improved after ECT. Patients who received continuation ECT were less likely to be readmitted than patients who did not receive continuation ECT. Patients taking antidepressants after ECT were less likely to be readmitted than patients not taking antidepressants after ECT. Patients taking antipsychotic medications, anxiolytic medications or benzodiazepines after ECT were more likely to be readmitted than patients not taking those medications after ECT. A higher measure of pharmacological resistance (represented by a higher ATHF score) was associated with higher risk of readmission as was a greater number of previous in-patient treatments for psychiatric disorders.
In the analysis stratified by antidepressant use, the HR of lithium for time to hospital readmission after ECT was 0.71 (95% CI 0.53–0.94) for patients who did not collect antidepressants. For patients who collected antidepressants after ECT the HR for lithium was 0.86 (95% CI 0.77–0.97). The analysis stratified by lithium use showed no significant effect of antidepressants (HR = 1.18, 95% CI 0.86–1.63) for those who used lithium but the effect of antidepressants was significant for those not using lithium (HR = 0.82, 95% CI 0.74–0.91). In the model with the interaction effect between lithium and antidepressant the interaction was statistically significant (HR = 1.41, 95% CI 1.05–1.89).
We performed a sensitivity analysis without the 40% of patients who lacked CGI-improvement scores and obtained similar results.
Discussion
Main findings and comparison with findings from other studies
Patients treated with lithium after ECT for unipolar depression were less likely to die by suicide or be readmitted to hospital than patients not treated with lithium after ECT for unipolar depression. Our model with data on more than 7000 patients followed for an average of over 1 year indicates that to prevent 1 readmission 16 patients need to be treated with lithium. This is a clinically relevant effect for a disorder that is hard to treat and whose consequences are severe. This finding supports existing Swedish guidelines that advocate the use of lithium for prophylaxis after ECT for depression.27 In this population-based study only 9% of patients were treated with lithium. Thus, there is a potential to increase the usage of lithium.
Antidepressants also seems to lower the risk of readmission, but were not associated significantly with suicide risk. Antidepressants are used widely and the potential for increased use is low. Our data suggest that lithium reduces the risk of readmission among patients taking or not taking antidepressants. Antidepressant use was only significantly associated with reduced risk of readmission among patients not taking lithium. Because few patients were taking lithium without antidepressants, the effect of antidepressants among lithium users is uncertain.
Continuation ECT was associated with reduced relapse risk. This is in line with data from randomised controlled trials.Reference Nordenskjold, von Knorring, Ljung, Carlborg, Brus and Engstrom28,Reference Kellner, Husain, Knapp, McCall, Petrides and Rudorfer29 Patients that receive continuation ECT are likely to have been selected for this treatment because the physician thought that pharmacotherapy would not be sufficient. We built models to try to account for selection bias, but there is nevertheless risk that the effect of continuation ECT is underestimated. Only 10% of the patients received continuation ECT, thus more patients could potentially benefit.
Antipsychotics and benzodiazepines were associated with increased risk for relapse, in line with earlier studies. Indication bias is likely to have influenced these associations, because antipsychotics and benzodiazepines are used to treat residual symptoms, and incomplete remission were associated with relapse. However, another possibility is that the negative effects on neuroplasticity of benzodiazepines contribute to explain the increased risk for relapse.Reference Nicholson, Sweeney, Pekle, Alam, Ali and Duchen30,Reference Maya Vetencourt, Sale, Viegi, Baroncelli, De Pasquale and O'Leary31 Many patients experience side-effects of antipsychotics including weight gain. Considering the sparse effect of this class of prophylactics on unipolar depression antipsychotics should be used cautiously in maintenance treatment of depression.
Patients who were treated for depression with psychotic symptoms were less likely to be readmitted than patients who were treated for depression without psychotic symptoms. This was also seen in an earlier study by our group.Reference Nordenskjold, von Knorring and Engstrom9 The outcomes of ECT for patients with psychotic depression is generally very favourable.Reference Brus, Cao, Gustafsson, Hulten, Landen and Lundberg32,Reference Petrides, Fink, Husain, Knapp, Rush and Mueller33
Older age, marriage and employment were associated with less readmission in line with earlier findings Reference Rosen, Kung and Lapid8 The suicide rate per year in this study was 0.5%, which is comparable with the 0.7% rate found in an earlier study.Reference Munk-Olsen, Laursen, Videbech, Mortensen and Rosenberg34
Limitations and strengths
This was a cohort study of a clinically treated population, thus, observed differences may depend on other, unmeasured factors that correlate both with exposure and outcome. We tried to limit this risk by including many factors that are likely to affect the outcome in the multivariate models. The data on diagnoses were not obtained using the same diagnostic instruments for all study participants, but rather were collected in routine clinical settings. There is a risk that a few patients with bipolar disorder might have been included in the study, although we tried to limit this number by excluding patients with previous in-patient treatment for bipolar disorder. A strength is that the registers used in this study are of high quality and coverage.Reference Ludvigsson, Andersson, Ekbom, Feychting, Kim and Reuterwall19,20,23–Reference Nordanskog, Hulten, Landen, Lundberg, von Knorring and Nordenskjold25
In conclusion, lithium can be beneficial in reducing the risk of readmission and suicide for patients treated with ECT for unipolar depression. and there is potential for its increased use.
Funding
The study is funded by the authors' respective employers.
Supplementary material
Supplementary material is available online at https://doi.org/10.1192/bjo.2019.37.




eLetters
No eLetters have been published for this article.