In low- and middle-income countries, perinatal depression is a major public health problem, affecting up to a quarter of all pregnant women in rural Pakistan. Reference Rahman, Malik, Sikander, Roberts and Creed1–Reference Rahman, Iqbal and Harrington3 In addition to its effects on the mother's well-being, perinatal depression is associated with adverse outcomes of pregnancy Reference Grote, Bridge, Gavin, Melville, Iyengar and Katon4 and adverse effects on the infant including delayed growth Reference Surkan, Kennedy, Hurley and Black5 and poor health and development. Reference Wachs, Black and Engle6 Relevant effective interventions are being developed Reference Rahman, Malik, Sikander, Roberts and Creed1,Reference Rojas, Fritsch, Solis, Jadresic, Castillo and González7 but their effectiveness in low- and middle-income countries may be limited by factors that maintain persistent depression, such as poverty, lack of social support and women's lack of financial independence from their husbands. Reference Rahman and Creed8,Reference Kermode, Herrman, Arole, White, Premkumar and Patel9
Poverty and mental ill health interact in a negative cycle and this is relevant to postnatal depression in low- and middle-income countries. Reference Rahman and Creed8,Reference Chandran, Tharyan, Muliyil and Abraham10 Poverty alleviation interventions do not appear to improve mental health but mental health interventions may be associated with improved economic outcomes, although more high-quality research is needed. Reference Lund, De Silva, Plagerson, Cooper, Chisholm and Das11 The identification of moderators can specify for whom, or under what conditions, the treatment works, to guide the design of future randomised controlled trials (RCTs) and to advance our understanding of the nature of clinical disorders. To date the moderators of treatment of postnatal depression have been studied little. Reference Leis, Mendelson, Tandon and Perry12 In particular, it is not known whether psychological interventions can reduce depression in women who are very poor and financially dependent on their husbands, or whether these factors limit the effectiveness of the intervention. Reference Kermode, Herrman, Arole, White, Premkumar and Patel9
In a recent RCT (trial registration: ISRCTN65316374) we tested an intervention, ‘The Thinking Healthy Programme’, which was based on culturally adapted cognitive–behavioural therapy (CBT) principles but also involved the husband and family in supporting the woman with depression during therapy. Reference Rahman, Malik, Sikander, Roberts and Creed1 The intervention was delivered by local community health workers; these workers were women who were influential and resourceful, and could help the women with depression and their families to mobilise community resources to overcome psychosocial difficulties through problem-solving. Reference Rahman13 Qualitative evaluations demonstrated that the problem-solving approach in the hands of these resourceful women was useful in addressing some of the socioeconomic risk factors at a practical level, for example, assisting women in obtaining small loans from government microcredit schemes. Through an agenda of effective child-rearing, the intervention also gently challenged gender stereotype and encouraged fathers to play an active role in supporting the mother in child care and interaction. The trial was effective in treating depression (effect size 0.66) but had additional benefits on maternal support, family relationships and infants’ health. Reference Rahman, Malik, Sikander, Roberts and Creed1 These benefits are compatible with the underlying theory of our approach, which regards the child as the centre of the intervention with the mother and father working together with the ‘lady health worker’ (LHW) to achieve child health. The present study was aimed at identifying the moderators of treatment outcome, on the basis that if a treatment has its effects by influencing a particular process this finding establishes the importance of the process in maintaining the disorder and may lead to further refinements of the intervention in a future trial. Specifically, we wished to determine whether poverty, debt or any of the other social variables associated with persistent depression (lack of financial empowerment, lack of social support) moderated the effect of treatment. We wished also to assess whether the intervention reduced the proportion of women with household debt and increased the proportion who were financially empowered.
Method
Study area, participants and sampling
This study used data from a cluster, randomised, community-based trial of a psychological intervention for perinatal depression in two rural subdistricts (Gujar Khan and Kallar Syedan) of Rawalpindi, Pakistan, between 2004 and 2007. The details of the methods and the main results of this trial have been reported elsewhere. Reference Rahman, Malik, Sikander, Roberts and Creed1 In a cluster randomised trial (Fig. 1), 40 union councils (an administrative unit consisting of 5–10 villages and a population of about 20 000) were randomised into an equal number of treatment and control clusters. A total of 3898 women in their third trimester of pregnancy were identified by obtaining official lists from 250 government-employed LHWs, who routinely collect data on new pregnancies. All married women aged 17–40 years in their third trimester of pregnancy, who had depression, were considered for inclusion in the study (Fig. 1). Women with a diagnosed medical condition, pregnancy-related illness, significant physical or intellectual disability, postpartum or other form of psychosis and severe depression were excluded. We obtained informed verbal and written consent from the participants. Ethical approval for the study was granted by committees of the University of Manchester, UK, and the Institute of Psychiatry, Rawalpindi.
Data ascertainment
Psychiatric disorder and depression severity
Assessments were carried out at all time points by two trained and experienced clinicians (A.M. and S.S.) using a structured clinical instrument for DSM-IV diagnosis of major depressive episode (SCID) 14 and the Hamilton Rating Scale for Depression (HRSD) Reference Hamilton15 to assess severity. The former was used to assess the inclusion criteria for the study and whether depressive disorder was still present at follow-up. Reference Rahman, Malik, Sikander, Roberts and Creed1 The HRSD was used to assess the severity of depression at these times. Both of these semi-structured interviews have been used repeatedly in cross-cultural, epidemiological and treatment studies of pre- and postnatal depression. All interviews were carried out in Urdu after translation, back-translation and cultural adaptation of the interview schedule using an established procedure. Reference Rahman, Iqbal, Waheed and Hussain16 Interrater reliability was established prior to the study when both interviewers independently assessed 20 women (10 had clinical depression) and agreed on the diagnosis of 9 (κ = 0.90). The interviewers were masked to the allocation status of the union councils and, therefore, the arm of the trial to which each of the women had been randomised. This masking was maintained because the interviewers had no contact with the team that did the randomisation, and throughout the duration of the study they had no contact with the LHWs or any other health personnel in the study area. Mothers were asked not to tell the interviewers anything about their meetings with the LHWs. The HRSD has a maximum score of 57; the mean baseline score in this sample was 14.6 (s.d. = 14.1).

FIG. 1 Flow diagram of cluster randomised controlled trial.
Others potential moderators of treatment effect
Social support. This was measured with the Multidimensional Scale of Perceived Social Support (MSPSS), Reference Zimet, Dahlem, Zimet and Farley17 a brief instrument that addresses subjective assessment of social support. The scale consists of 12 items; each is scored on a seven-point scale. Four questions each ask about the source of social support: family, friends, significant other. Thus, for the family support scale the scores range from 4 to 28, with higher scores indicating greater support; the mean score in this sample was 16.3 (s.d. = 6.8). The MSPSS has been locally validated and shown to have satisfactory internal reliability, factorial validity, and test and retest reliability. Reference Eker, Arkar and Yaldiz18 In addition, we assessed whether intense social support from family members for 40 days after the birth (chilla) was satisfactory.
Sociodemographic variables. Age, education, employment, family structure and composition were assessed at baseline by the same interviewers using a specially designed Personal Information Questionnaire. Education was categorised into no formal education, 1–6 years, 7–10 years and 11 or more years of formal education. Family structure was categorised into nuclear family (parents and children only) or extended family (three generations living in the same home).
Mothers’ nutritional status. Maternal body mass index (BMI) was measured as an indicator of nutritional status.
Socioeconomic status. Our study used several sources of information to determine the socioeconomic status of our participants because of the difficulty of measuring this variable in south Asia. Reference Patel, Pereira, Coutinho, Fernandes, Fernandes and Mann19 At baseline we asked LHWs, who lived in the same locality and had intimate knowledge of the families participating in our study, to rate the household on a five-point Likert scale ranging from 1 (least poor) to 5 (poorest). Participants were asked whether their family was in debt and this was verified by asking the LHW, who was generally aware of the nature of the loan, for example, to buy a tractor or to purchase healthcare for a family member. This assessment was repeated at 1-year follow-up. We also asked the participants about the family's monthly income at baseline only.
Financial empowerment. Maternal financial empowerment within the household was measured at baseline by asking the women whether they were given a lump-sum amount of money for day-to-day household expenses, and whether they could take independent decisions about its use. Mothers who answered ‘yes’ to both questions were classified as financially empowered within the household. Called ‘kharcha’, this is a culturally valid concept indicating a degree of empowerment within the household even if the women were not earning. This assessment was repeated at 6 months after baseline.
Statistical analysis
All analyses were carried out with SPSS for Windows, version 16. The first analysis (data not shown) included all the participants in the trial for whom complete data were available at 1-year follow-up (n = 791). These initial univariable analyses were performed to identify baseline variables associated with HRSD scores at follow-up and used t-test, analysis of variance (ANOVA) or correlation as appropriate. We then performed multiple regression analyses with follow-up HRSD score as the dependent variable. The independent variables were: baseline HRSD, arm of trial (intervention or control), the participant's age, BMI, duration of formal education, family structure (nuclear or joint), socioeconomic status rated by the LHW, empowerment (whether the woman was empowered to manage household finances or not), and debt (yes/no).
In further regression analyses we entered in turn each of the following interaction terms: arm × age, arm × BMI, arm × debt (at baseline) and arm × empowerment (at baseline) to identify which of these interaction terms were significant predictors of follow-up HRSD score.
We used two-way analysis of covariance (ANCOVAR) to test for the effects of treatment arm, being in debt or not, and the interaction term arm × debt on the follow-up HRSD score. We adjusted for baseline HRSD, mother's age, BMI, years of education, family structure, and socioeconomic status rated by the LHW. This analysis was repeated for financial empowerment instead of debt.
We performed further analyses to examine how debt and financial empowerment fit into the more established risk factors for depression in this population (poverty, having numerous children, an uneducated husband and lack of a confidant or friend).
In order to examine the predictors of empowerment and freedom from debt at follow-up we performed logistic regression analysis with each of these variables as the dependent variable. The following variables were included as independent variables in model 1, which included only baseline variables: mother's age, BMI, duration of formal education, arm of trial, HRSD score, family support (MSPSS family score), financial empowerment and debt. In model 2 of the analysis with debt at 12 months follow-up as the dependent variable, the following measures made at 6 months were included: HRSD score, family support (MSPSS family score), reported relationship with husband and financial empowerment. For the analysis with financial empowerment at follow-up as the dependent variable, being in debt at 6 months was included instead of financial empowerment as an independent variable.
Results
The recruitment to the trial has been described in detail elsewhere. Reference Rahman, Malik, Sikander, Roberts and Creed1 Out of 3898 women in the last trimester of pregnancy, 3518 consented to baseline screening with the SCID and 903 eligible women had a DSM-IV major depressive episode and consented to join the trial. These women received the intervention or enhanced routine care according to the union council in which they lived and they were followed up for 1 year postnatally. This study is concerned with 791 women who completed the 1-year follow-up with complete data; details of the sample are shown in Table 1.
TABLE 1 Description of the sample: sociodemographic data
| Participants (n = 791) |
|
|---|---|
| Age, years: mean (s.d.) | 26.8 (4.9) |
| Trial arm, n (%) | |
| Intervention arm | 407 (51.5) |
| Control arm | 384 (48.5) |
| Financially empowered, n (%) | 415 (2.5) |
| Family size, n (%) | |
| Prima gravida | 136 (17.2) |
| One child only | 173 (21.9) |
| Two or more children | 482 (60.9) |
| Education, n (%) | |
| No formal education | 325 (41.1) |
| 1–6 years | 242 (30.6) |
| 7–10 years | 199 (25.2) |
| >11 years | 25 (3.2) |
| Extended family structure, n (%) | 461 (58.3) |
| SES rated by lady health worker | |
| Poorest | 172 (21.7) |
| Poor | 233 (29.5) |
| Intermediate | 308 (38.9) |
| Relatively well-off | 78 (9.9) |
| In debt, n (%) | 441 (55.8) |
SES, socioeconomic status.
All women were married and living with their husbands; only 2.6% were employed outside the home. Just over half (52.5%) were empowered to manage household finances. The mean family monthly income for the four socioeconomic groups shown in Table 1, were 4690 rupees (s.d. = 8272), 2421 (s.d. = 4651), 1506 (s.d. = 2747) and 985 (s.d. = 2096) for the relatively well-off, intermediate, poor and poorest categories respectively. These approximate to US$470, 242, 150 and 98 per month. Just over half (55%) of participants stated that their family were in debt and the proportions were: 9.9%, 38.9%, 29.5% and 21.7% for the relatively well-off, intermediate, poor and poorest categories respectively.
Depression at follow-up
At follow-up, 111/407 (27.3%) participants in the intervention arm remained depressed compared with 226/384 (58.9%) of those in the control arm. Reference Rahman, Malik, Sikander, Roberts and Creed1 Mean follow-up HRSD scores, adjusted for baseline values, were 5.4 (95% CI 4.7–6.1) in the intervention arm and 10.8 (95% CI 10.1–11.5) in the control arm (P<0.001, effect size 0.72).
Mean follow-up HRSD scores, adjusted for baseline values, were 8.9 (95% CI 8.2–9.6) and 6.9 (95% CI 6.1–7.7) for women with and without household debt respectively (P<0.001). Corresponding results for women not financially empowered and empowered were 9.4 (95% CI 8.6–10.2) and 6.7 (95% CI 6.0–7.4) (P<0.001).
Multivariate analysis
In multiple regression with follow-up HRSD score as the dependent variable, and adjusting for treatment arm, the following baseline variables predicted a high follow-up score: high baseline HRSD score, low BMI, older age, woman not empowered financially, and presence of household debt (Table 2). The MSPSS score (indicating low support) was omitted from these analyses as it was so highly correlated with financial empowerment (MSPSS score for empowered women 51.3 (95% CI 49.9–52.8) and not empowered 38.8 (95% CI 37.3–40.3)).
TABLE 2 Multiple regression analysis with the Hamilton Rating Scale for Depression score at follow-up as dependent variable (n = 791) including arm × debt interaction term as an independent variable in model 2
| Model 1 | Model 2 | |||||
|---|---|---|---|---|---|---|
| B | s.e. | P | B | s.e. | P | |
| Baseline Hamilton Rating Scale for Depression score | 0.296 | 0.061 | <0.001 | 0.297 | 0.061 | <0.001 |
| Arm of trial | –5.33 | 0.493 | <0.001 | –5.193 | 0.495 | <0.001 |
| Financially empowered | –2.519 | 0.503 | <0.001 | –2.482 | 0.501 | <0.001 |
| Body mass index | –0.155 | 0.062 | 0.012 | –0.168 | 0.062 | 0.007 |
| Age | 0.164 | 0.054 | 0.002 | 0.164 | 0.054 | 0.002 |
| Years education | –0.116 | 0.295 | 0.69 | –0.173 | 0.295 | 0.56 |
| Extended family structure | –0.658 | 0.534 | 0.22 | –0.629 | 0.532 | 0.24 |
| Low socioeconomic status rated by lady health worker | 0.400 | 0.244 | 0.10 | 0.375 | 0.243 | 0.12 |
| In debt | 1.610 | 0.526 | 0.002 | 1.647 | 0.525 | 0.002 |
| Arm × debt | –0.592 | 0.248 | 0.017 | |||
The addition to the multiple regression analysis of possible moderator variables showed that the interaction terms arm × age (P = 0.52) and arm × BMI (P = 0.34) and arm × socioeconomic status (P = 0.54) were not significant predictors. However, the interaction terms for debt and mother empowered financially were significant (P = 0.017 and P = 0.045 respectively).
ANCOVAR analyses for the moderators, debt and empowerment
Figure 2 shows that the reduction of HRSD score was very similar in the intervention arm for those women with and without household debt at baseline (mean adjusted HRSD scores at follow-up 5.8 (95% CI 4.9–6.7) and 5.1 (95% CI 4.1–6.2) respectively). For the control arm, however, the women without household debt had a lower mean adjusted HRSD scores at follow-up (9.0, 95% CI 7.9–10.0) than those with household debt (12.1, 95% CI 11.2–13.1). The effect sizes for the intervention for women with and without household debt were 0.80 and 0.55 respectively.
Figure 3 shows that the reduction of HRSD score was similar in the intervention arm for those women who were and were not financially empowered at baseline (mean adjusted HRSD scores at follow-up 4.68 (95% CI 3.7–5.6) and 6.35 (95% CI 5.4–7.3) respectively). For the control arm the women who were financially empowered had a lower mean follow-up HRSD score (mean 9.0, 95% CI 8.0–9.9) than those who were not empowered (mean 12.67, 95% CI 11.64–13.7). The effect sizes for women not empowered and empowered were 0.81 and 0.61 respectively.
For 235 women who were both in debt at baseline and not empowered financially, the follow-up HRSD score, adjusted for baseline value, was 13.6 (SEM = 0.68) in the control group and 6.9 (SEM = 0.64) in the intervention arm. The effect size was 0.936. For 347 women with either household debt or not financially empowered (not both) the effect size was 0.808. For 209 women empowered and not in debt the effect size was 0.50.
Changes in debt and empowerment
Of the 441 women who were in debt at baseline, a significantly higher proportion in the intervention group –79/233 (33.9%) –were no longer in debt at follow-up compared with 49/208 (23.6%) of the control group (P = 0.017). Of the 387 women who reported not being financially empowered at baseline, 40.3% (81/201) in the intervention group and 29.0% (54/186) in the control group reported being financially empowered at 6 months (P = 0.020).
Inclusion of these change scores in the multiple regression made no difference to the statistical significance of the arm of the trial indicating that changes in debt or empowerment did not mediate the effect of the intervention (Table 3).
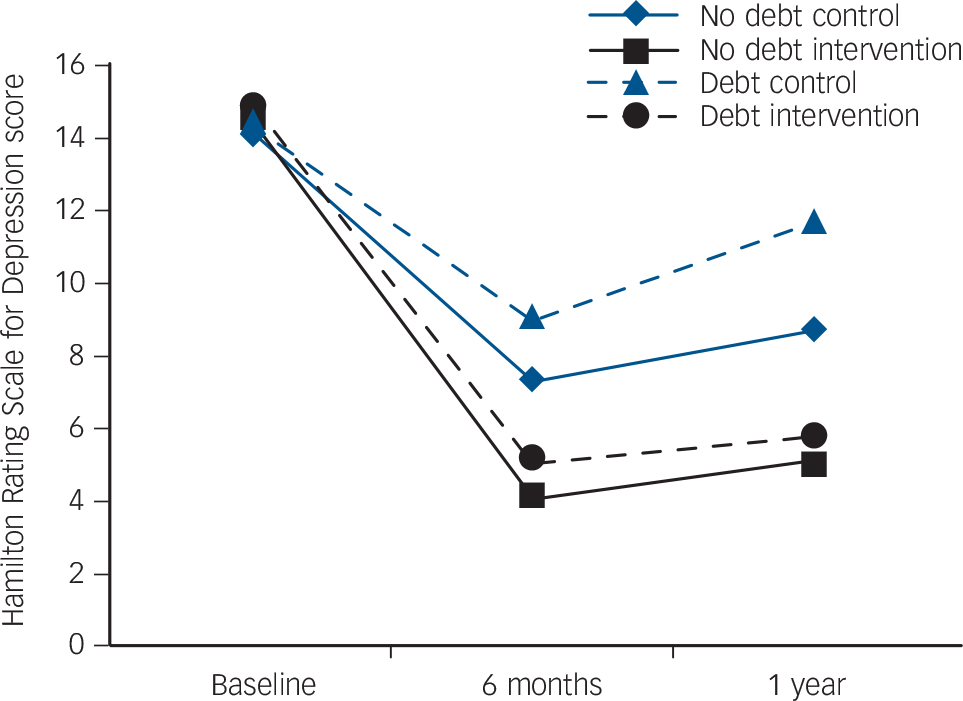
FIG. 2 Hamilton Rating Scale for Depression Score at baseline, 6 months and at follow-up for intervention and control groups, split by debt v. no debt.
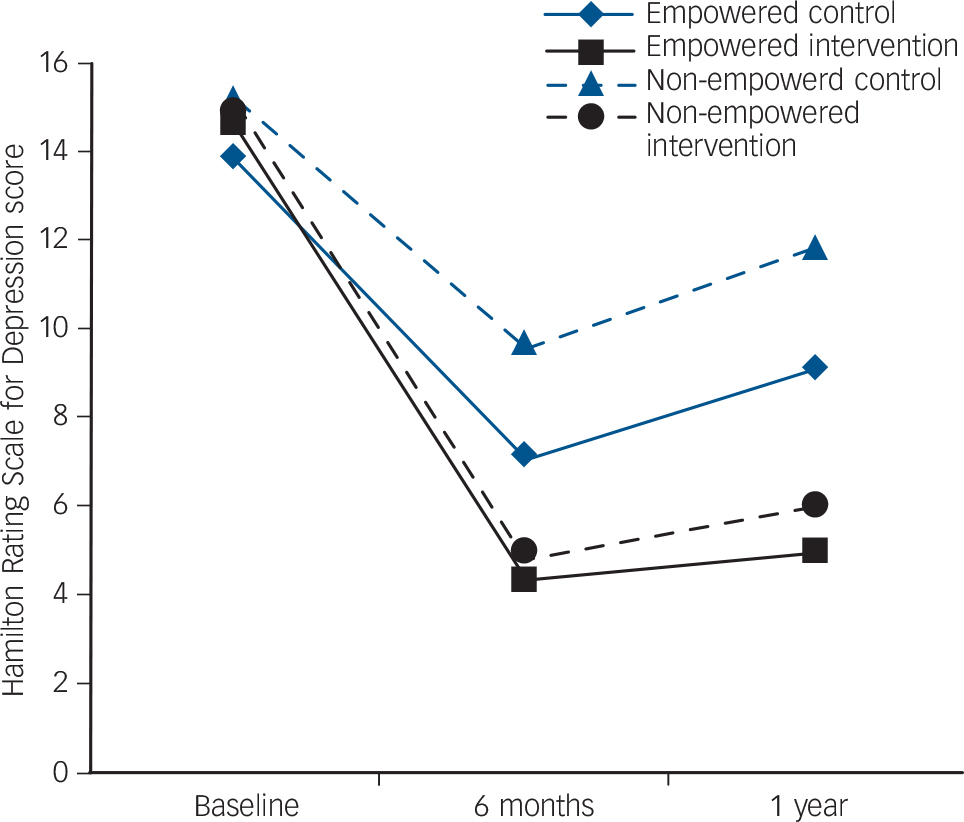
FIG. 3 Hamilton Rating Scale for Depression score at baseline, 6 months and at follow-up for intervention and control groups, split by women empowered v. not empowered.
TABLE 3 Multiple regression analysis with Hamilton Rating Scale for Depression score at follow-up as dependent variable (n =791) including change in debt and change in financial empowerment as independent variables
| B | s.e. | P | |
|---|---|---|---|
| Baseline Hamilton Rating Scale for Depression score | 0.296 | 0.061 | <0.001 |
| Arm of trial | –4.915 | 0.497 | <0.001 |
| Financially empowered | –0.416 | 0.631 | 0.510 |
| Body mass index | –0.116 | 0.062 | 0.064 |
| Age | 0.159 | 0.054 | 0.003 |
| Years of education | –0.049 | 0.066 | 0.456 |
| Extended family structure | –0.766 | 0.530 | 0.149 |
| Low socioeconomic status rated by lady health worker | 0.279 | 0.243 | 0.251 |
| In debt | –0.945 | 0.943 | 0.316 |
| Change in debt | 0.583 | 0.182 | 0.001 |
| Change in empowerment | –0.875 | 0.183 | <0.001 |
Debt, financial empowerment and outcome of the intervention
In addition to the variables shown in Table 2 as predictors of higher depression score at follow-up (older age, being in debt, not being empowered financially and high BMI), MSPSS score indicating low family support and unsatisfactory chilla (intense social support from family members for 40 days after the birth) were additional predictors. Number of young children, a husband with very little formal education, socioeconomic status assessed by the LHW and social support from outside of the family were not predictors of depression score at follow-up when included in this multiple regression analysis.
In logistic regression analyses adjusting for age, years of education, BMI, depression score and family support (model 1 in Table 4) the intervention arm of the trial was associated directly with a reduced likelihood of being in debt at follow-up (B = 0.73, 95% CI 0.53–0.99). The arm of the trial was also associated with an increased likelihood of the woman being financially empowered (B = 1.93, 95% CI 1.40–2.66) (model 1 in Table 5). Neither of these results could be explained by baseline depression severity, support from family or duration of education (model 1 in Tables 4 and 5).
When 6-month follow-up assessments were added to the logistic regression (model 2) it is clear that debt at follow-up was associated with baseline debt, few years of education, BMI, HRSD score at 6 months and mother not financially empowered at 6 months (Table 4).
TABLE 4 Logistic regression analysis with debt at 12 months follow-up as dependent variable (n = 784)Footnote a
| Model 1 | Model 2 | |||||
|---|---|---|---|---|---|---|
| B | s.e. | P | B | s.e. | P | |
| Age | 0.025 | 0.017 | 0.127 | 0.024 | 0.017 | 0.160 |
| Arm of trial | –0.314 | 0.159 | 0.049 | –0.019 | 0.173 | 0.912 |
| Baseline Hamilton Rating Scale for Depression score | –0.009 | 0.020 | 0.630 | –0.032 | 0.021 | 0.123 |
| Body mass index | –0.056 | 0.020 | 0.005 | –0.050 | 0.021 | 0.014 |
| Years of education | –0.054 | 0.021 | 0.009 | –0.048 | 0.021 | 0.023 |
| Multidimensional Scale of Perceived Social Support, family baseline | –0.002 | 0.013 | 0.876 | 0.008 | 0.014 | 0.535 |
| Financially empowered | –0.154 | 0.175 | 0.380 | 0.102 | 0.192 | 0.596 |
| In debt | 1.616 | 0.163 | <0.001 | 1.593 | 0.167 | <0.001 |
| Hamilton Rating Scale for Depression score at 6 months | 0.050 | 0.015 | 0.001 | |||
| Financially empowered at 6 months | –0.494 | 0.192 | 0.010 | |||
| Multidimensional Scale of Perceived Social Support, family at 6 months | –0.016 | 0.017 | 0.337 | |||
| Relationship with husband | 0.009 | 0.091 | 0.920 | |||
a. Model 1 includes baseline variables only. Model 2 includes variables also measured at 6 months.
Corresponding analysis for financial empowerment at follow-up (model 2 in Table 5) showed that this was associated with financial empowerment at baseline, low 6-month HRSD score, high family support scores at 6 months and good relationship with husband. Physical violence from the husband was associated with a lack of empowerment at follow-up but this did not add significantly to the model when the relationship with the husband was included. The same applied to the relationship with the mother-in-law (details available from the authors on request). We conclude from these analyses that the intervention had a greater direct effect on empowerment than on debt reduction. Furthermore, the beneficial effect of the intervention on empowerment and debt reduction were part of a range of improvements, which also included depression reduction and increased social support.
Discussion
Main findings
The main new finding of this study indicates that our intervention, based on CBT principles but involving the family and using LHWs as ‘agents of change’, was effective even for women who reported being in debt and/or not empowered financially. The latter two variables were moderators of treatment and the effect sizes show that improvement in depression was greater for those women who reported household debt and/or not being financially empowered. Second, the intervention was associated with a reduction of households in debt and an increase in women reporting that they were financially empowered but neither of these factors mediated the effect of the intervention on depression.
TABLE 5 Logistic regression analysis with mother financially empowered at follow-up as dependent variable (n = 784)Footnote a
| Model 1 | Model 2 | |||||
|---|---|---|---|---|---|---|
| B | s.e. | P | B | s.e. | P | |
| Age | 0.024 | 0.017 | 0.171 | 0.035 | 0.019 | 0.059 |
| Arm of trial | 0.657 | 0.165 | <0.001 | 0.207 | 0.185 | 0.263 |
| Baseline Hamilton Rating Scale for Depression score | –0.034 | 0.020 | 0.086 | 0.004 | 0.022 | 0.845 |
| Body mass index | 0.024 | 0.021 | 0.235 | 0.018 | 0.022 | 0.401 |
| Years of education | 0.036 | 0.021 | 0.098 | 0.023 | 0.023 | 0.326 |
| Multidimensional Scale of Perceived Social Support, family baseline | 0.031 | 0.013 | 0.018 | 0.013 | 0.014 | 0.379 |
| Financially empowered | 1.594 | 0.175 | <0.001 | 1.662 | 0.190 | <0.001 |
| In debt | –0.215 | 0.167 | 0.197 | 0.054 | 0.196 | 0.783 |
| Hamilton Rating Scale for Depression score at 6 months | –0.061 | 0.015 | <0.001 | |||
| In debt at 6 months | –0.333 | 0.196 | 0.090 | |||
| Multidimensional Scale of Perceived Social Support, family at 6 months | 0.081 | 0.017 | <0.001 | |||
| Relationship with husband | 0.255 | 0.095 | 0.007 | |||
a. Model 1 includes baseline variables only and Model 2 includes variables also measured at 6 months.
Strengths and limitations
Before considering the results further it is necessary to recognise the strengths and limitations of the study. The results come from data collected in a large RCT, which was based on a population-based sample of women with clinical depression during the last trimester of pregnancy. The intervention and control groups were similar on a wide range of sociodemographic characteristics and the intervention was effective in reducing depression. Reference Rahman, Malik, Sikander, Roberts and Creed1 The findings of the current study must be regarded as exploratory, however, as we did not have an a priori hypothesis with regard to moderators, Reference Kraemer, Wilson, Fairburn and Agras20,Reference Pincus, Miles, Froud, Underwood, Carnes and Taylor21 although our study was based on the predictors of persistent depression arising from our previous study in a similar sample. Reference Rahman and Creed8 In our analysis we did us a specific test of the interaction between baseline factors and interventions. Reference Pincus, Miles, Froud, Underwood, Carnes and Taylor21 We did not, however, have any test of reliability and validity for our measures of debt and empowerment. Our assessment instruments have been validated in this population. Reference Husain, Akhter, Duddu and Rahman22
It has been suggested that identification of moderators should be undertaken whenever possible as this can specify for whom, or under what conditions, the treatment works, to guide the design of future RCTs and to advance our understanding of the nature of clinical disorders. Reference Kraemer, Wilson, Fairburn and Agras20,Reference Kraemer, Frank and Kupfer23 Kraemer et al stated that ‘if a treatment has its effects by influencing a particular process this finding establishes the importance of the process in maintaining the disorder’. Reference Kraemer, Wilson, Fairburn and Agras20 Our finding that reducing household debt and increasing the financial empowerment of women are associated with improved depression demonstrates the importance of these factors in maintaining depression. Moreover, we found that these factors, together with low family support and unsatisfactory chilla, were more strongly associated with follow-up depression score than those in our previous study (number of young children, a husband with very little formal education, low socioeconomic status and general social support), emphasising the importance of identifying these crucial aspects of the women's environment (debt, empowerment, family support) when treating their depression. The data presented here focus on the moderating effect of household debt and financial empowerment, as the other variables we considered as possible mediators did not fulfilled the requirements of mediators. Reference Kraemer, Wilson, Fairburn and Agras20
Implications
The main findings are important as nearly all studies of depression in low-income countries find debt or poverty to be associated with depression so it has been suggested that depression and poverty can interact in a vicious circle. Reference Patel, Kleinman, Patel and Kleinman24 More recently it has been observed in a qualitative study of women in India that women's financial empowerment and mental health are ‘inextricably linked’. Reference Kermode, Herrman, Arole, White, Premkumar and Patel9 Our intervention appears to be a way of breaking the vicious circle of depression with debt or lack of empowerment. It is noteworthy that, although low socioeconomic status was associated with a high depression scores at follow-up, it was debt that was a moderator of outcome, hence debt may be more amenable to change than poverty. Although only having a few years of formal education predicted debt at follow-up, this was not so for empowerment, which is a strength of the approach taken by the LHWs in the intervention arm.
Our intervention, the ‘Thinking Healthy Programme’, was developed to provide a culturally appropriate, feasible and evidence-based psychological intervention for women living in very poor communities in rural Pakistan. It was delivered by ordinary female community health workers to overcome the lack of trained specialist therapists in low-income settings. We believe the community health workers were effective as therapists partly because they could readily engage with the local women, but also because they understood fully their social stressors. This meant they could use problem-solving effectively as part of the therapy to address these stressors.
The improvement in financial empowerment can be seen as a direct effect of the intervention, even though it was not a specific focus of the intervention. The intervention focused on the mother's care of herself, including her diet and appearance; it aimed to boost self-esteem. Another specific focus was the modification of family behaviour where it was important for child healthcare. This involved engaging the father as well as the mother. These aspects of the intervention might well have encouraged empowerment of the women, even though this was not a specific aim. Reduction of debt was rather less directly associated with the intervention. It probably arose as a result of the LHWs’ freedom to seek solutions to the problems faced by many families as part of a child-focused agenda. Thus, debt would have been highlighted as a major problem in approximately half of the families and this could have led to the LHW gently encouraging mothers and families to take small steps to better themselves financially. Future interventions for depression in women in low- and middle-income countries might usefully incorporate this element of problem-solving in addition to the cognitive and behavioural aspects of a CBT-like intervention.
The fact that the intervention was associated with the household coming out of debt is immensely important in a low-income setting such as rural Pakistan, where debt can have disastrous effects on a family. In this setting household debt may result from a catastrophic health problem in a family member 25 but the intervention was associated also with infants having fewer episodes of diarrhoeal illness and higher rates of immunisation so the benefits of our intervention go beyond improvement in the mothers’ mental health. An intervention targeting maternal mental health may have economic benefits for the household.
We strongly advocate the case for including mental health interventions, especially those targeting women and children, in programmes of poverty alleviation. Similarly, the use of local non-specialist workers to deliver therapies may be a very effective strategy to deliver psychological interventions in poor communities.
Funding
The study was funded by the Wellcome Trust, UK, through a career development fellowship in tropical medicine awarded to A.R. The fellowship was awarded through the Wellcome Trust Tropical Centre at the Liverpool School of Tropical Medicine and hosted by the University of Manchester and the Institute of Psychiatry, Rawalpindi.
Acknowledgements
We would like to thank the Human Development Research Foundation, Islamabad, for logistic assistance; the Ministry of Health, Government of Punjab, for their permission to do this study; Fareed Minhas at Rawalpindi for his unflinching support and encouragement; and Zaeem Haq for assistance with the development of training materials and supervision of the lady health workers.











eLetters
No eLetters have been published for this article.