In DSM-5 1 two new psychiatric diagnoses, somatic symptom disorder (SSD) and illness anxiety disorder (IAD), have replaced DSM-IV hypochondriasis. 2 There were several reasons for this. Primarily, the emphasis of medically unexplained symptoms in the DSM-IV hypochondriasis diagnosis was questioned because of the difficulty in judging whether a somatic symptom is medically explained or not. 1 Additionally, DSM-IV hypochondriasis required a misinterpretation of bodily sensations, even though many individuals can experience clinically relevant health anxiety without having marked somatic symptoms. About 75% of patients who would meet diagnostic criteria for DSM-IV hypochondriasis are now assumed to be diagnosed with DSM-5 SSD, which requires that the individual be clinically distressed by one or more somatic symptoms. 1 The remaining 25% are expected to meet criteria for IAD, which is characterised by high levels of anxiety about health, but where somatic symptoms are absent or only mild in intensity. 1 Both disorders are thus characterised by excessive concern about health but differ in terms of presence of somatic symptoms. As follows with all major revisions of diagnostic criteria, the knowledge about central aspects of SSD and IAD is currently limited. We know very little about the epidemiology, aetiology and – not least – how to effectively treat these disorders. Drawing from the literature on hypochondriasis it is, however, likely that SSD and IAD are highly prevalent in medical settings and that they are associated with substantial suffering, impairment and societal costs. Reference Barsky, Fama, Bailey and Ahern3–Reference Seivewright, Salkovskis, Green, Mullan, Behr and Carlin6
Our research group has shown that therapist-guided internet-delivered exposure-based cognitive–behavioural therapy (ICBT) can be highly effective in the treatment of hypochondriasis. Reference Hedman, Andersson, Andersson, Ljotsson, Ruck and Asmundson7,Reference Hedman, Axelsson, Gorling, Ritzman, Ronnheden and El Alaoui8 ICBT of this kind can be described as guided online bibliotherapy, where the most important part of treatment is a text that provides the patient with the tools for conducting successful exposure therapy. This approach to treatment has several important strengths, many of which give it the potential to greatly increase the availability of effective psychological treatment. ICBT is independent of geographical distance: it does not require scheduled appointments, and since core therapeutic principles are conveyed through a self-help text, therapists can treat up to five times as many patients as in regular therapy. As this form of treatment bears strong resemblance to self-help bibliotherapy an important question is whether therapist guidance and an internet-based treatment platform are necessary for achieving strong treatment effects. That is, could it be that unguided ICBT (U-ICBT) and bibliotherapy are simple yet effective alternatives to regular ICBT in the treatment of SSD and IAD? Considering the large unmet needs for this patient group in terms of accessibility to psychological treatment, we viewed this question highly relevant to investigate. Most importantly, to our knowledge, there is no previously published study on any form of treatment for SSD and IAD. The aim of this study was to investigate the efficacy of exposure-based ICBT, U-ICBT and bibliotherapy for SSD and IAD in a randomised controlled trial (RCT). We expected that all three treatments would lead to significant reductions of health anxiety, anxiety sensitivity, general anxiety, depressive symptoms and functional disability compared with an untreated control condition.
Method
Design
This was a RCT where 132 participants with SSD or IAD were randomised to therapist-guided ICBT (n = 32), unguided, i.e. U-ICBT (n = 33), unguided bibliotherapy (n = 34), or a control condition on a waiting list (n = 33). Participants were randomised in a 1:1:1:1 ratio with no restrictions or matching. All active treatments had the same content, but they differed in terms of therapist guidance and whether the treatment was delivered via the internet or as a self-help book. The treatments were 12 weeks long and after this period participants in the control condition were crossed over to treatment and thus not included in analyses at 6-month follow-up. The trial was conducted in Sweden between 21 January and 19 June 2014 using nationwide recruitment. All participants provided informed consent. The regional ethics review board in Stockholm approved the study and the trial was registered at Clinicaltrials.gov (identifier NCT01966705).
Recruitment, inclusion criteria and participants
Information about the study was provided via mental health and primary care personnel, newspapers with national coverage and a study web portal through which all potential participants had to apply. Participants were required to (a) have a principal diagnosis of DSM-5 SSD or IAD, (b) be at least 18 years old, (c) be able to read and write in Swedish, (d) have no ongoing or prior episode of bipolar disorder or psychosis, (e) have no ongoing substance misuse or addiction, (f) have been on a stable dose for at least 2 months if on antidepressant medication and agree to keep the dose constant throughout the study, (g) not have severe depressive symptoms or serious suicidal ideation, (h) receive no concurrent psychological treatment for SSD/IAD and have no history of completed CBT for SSD/IAD during the past year, and (i) have no serious somatic disorder to which health anxiety would be an adequate response.
Nationwide recruitment was accomplished through telephone interviewing, which is a reliable method for structured psychiatric assessment. Reference Rohde, Lewinsohn and Seeley9 Potential participants who applied to the study underwent a 35–60 min diagnostic interview with a psychologist. Potential participants were given information about the study, for example that they would have to work with the treatment each week. To assess whether diagnostic criteria for SSD or IAD were met we used a structured diagnostic interview, the Health Preoccupation Diagnostic Interview (HPDI). Reference Axelsson, Andersson, Ljótsson, Wallhed Finn and Hedman10 The HPDI covers all DSM-5 criteria of SSD and IAD and can be administered with high interrater reliability. Reference Axelsson, Andersson, Ljótsson, Wallhed Finn and Hedman10 To assess the presence of other psychiatric disorders we used the Mini-International Neuropsychiatric Interview (MINI). Reference Sheehan, Lecrubier, Sheehan, Amorim, Janavs and Weiller11 As a frame of reference, the Anxiety Disorders Interview Schedule IV (ADIS) Reference Di Nardo, O'Brien, Barlow, Waddell and Blanchard12 was used to establish whether participants met criteria for DSM-IV hypochondriasis. Figure 1 displays the participant flow through the trial and Table 1 displays a description of the participants. Of the 132 participants included in the study, 50 (37.9%) first heard of the study via the internet, 15 (11.4%) via primary care, 10 (7.6%) via the Swedish national service for medical counselling, and 6 (4.5%) via out-patient psychiatric clinics. The remaining 50 (37.9%, 1 missing) participants were informed via other sources. Concerning diagnoses, 114 participants (86.4%) met criteria for SSD whereas 18 (13.6%) had IAD.

Fig. 1 Participant flow through the trial.
SSD, somatic symptom disorder; IAD, illness anxiety disorder; CBT, cognitive–behavioural therapy; ICBT, internet-based CBT, U-ICBT unguided internet-based CBT; 6MFU, 6-month follow-up.
Table 1 Characteristics of the participants
| ICBT (n = 32) |
U-ICBT (n = 33) |
Bibliotherapy (n = 34) |
Control condition (n = 33) |
|
|---|---|---|---|---|
| Gender | ||||
| Female | 24 | 24 | 24 | 26 |
| Male | 8 | 9 | 10 | 7 |
| Age, years | ||||
| Mean age (s.d.) | 38.6 (12.6) | 37.4 (11.6) | 35.4 (12.4) | 41.5 (13.5) |
| Minimum-maximum | 22–70 | 20–72 | 21–69 | 22–68 |
| Health anxiety disorder | ||||
| Somatic symptom disorder (SDD), n (%) | 26 (81.3) | 30 (90.9) | 28 (82.4) | 30 (90.9) |
| Illness anxiety disorder (IAD), n (%) | 6 (18.7) | 3 (9.1) | 6 (17.6) | 3 (9.1) |
| Hypochondriasis, n (%) | 28 (87.5) | 26 (78.8) | 33 (97.1) | 31 (93.9) |
| Years with SSD or IAD, mean (s.d.) | 7.2 (5.7) | 7.8 (6.4) | 10.2 (13.2) | 9.7 (12.4) |
| Global assessment of functioning (GAF), 2 baseline score (s.d.) | 60.2 (6.6) | 59.1 (6.1) | 60.9 (6.7) | 61.4 (5.8) |
| Occupational status | ||||
| Working full-time, n | 15 | 21 | 15 | 13 |
| Working part-time, n | 7 | 6 | 6 | 9 |
| Pensioner, on sick-leave or unemployed: n | 3 | 3 | 3 | 5 |
| Other, n | 7 | 4 | 10 | 9 |
| Marital and parental status | ||||
| Married or de facto, n | 28 | 29 | 31 | 27 |
| Parent, n | 21 | 21 | 18 | 20 |
| Psychiatric comorbidity, comorbid anxiety disorder: n | 20 | 24 | 14 | 19 |
| Stabilised psychotropic medication, SSRIs or SNRIs: n | 7 | 7 | 9 | 6 |
ICBT, Internet-based cognitive–behavioural therapy; U-ICBT, unguided Internet-based cognitive–behavioural therapy; SSRI, selective serotonin reuptake inhibitor; SNRI, selective serotonin–noradrenaline reuptake inhibitor.
Outcome measures
Primary outcome measure
The primary outcome measure was the 64-item Health Anxiety Inventory (HAI). Reference Salkovskis, Rimes, Warwick and Clark13 The HAI has been shown to possess good psychometric qualities including high test–retest reliability (r = 0.90), Reference Salkovskis, Rimes, Warwick and Clark13 high internal consistency (Cronbach's α = 0.95) Reference Salkovskis, Rimes, Warwick and Clark13 and good convergent and discriminant validity. Reference Hedman, Ljotsson, Andersson, Andersson, Lindefors and Ruck14 The HAI is also sensitive to change. Reference Salkovskis, Rimes, Warwick and Clark13,Reference Hedman, Ljotsson, Andersson, Andersson, Lindefors and Ruck14
Secondary outcome measures
The Illness Attitude Scales (IAS) Reference Speckens, Spinhoven, Sloekers, Bolk and van Hemert15 and the Whiteley Index (WI, 14-item version; yes/no response option) Reference Pilowsky16 were used as complementary measures of health anxiety. Anxiety sensitivity and general anxiety was assessed using the Anxiety Sensitivity Index (ASI) Reference Reiss, Peterson, Gursky and McNally17 and the Beck Anxiety Inventory (BAI), Reference Beck, Epstein, Brown and Steer18 respectively. We assessed depressive symptoms using the Montgomery–Åsberg Depression Rating Scale – Self-rated (MADRS-S) Reference Svanborg and Åsberg19 and functional impairment with the Sheehan Disability Scale (SDS). Reference Sheehan20
Assessment of treatment credibility, treatment satisfaction and adverse events
To assess treatment credibility the C-scale Reference Borkovec and Nau21 was used. Treatment satisfaction was measured with the Client Satisfaction Questionnaire-8 (CSQ-8). Reference Attkisson and Zwick22 After treatment, participants also reported whether they had experienced any adverse events during the treatment period. Adverse events were assessed through an item where participants were asked to state whether they had experienced any negative or unwanted effects of the treatment. If answering ‘Yes’, participants specified the adverse event in free text.
Assessment points
Assessments with the primary and secondary outcome measures were conducted at baseline, i.e. directly before treatment start and after the diagnostic interview, post-treatment and 6 months after treatment completion. The C-scale was administered 2 weeks after treatment start and adverse events were assessed at post-treatment.
Randomisation and procedures
A true random number service (www.random.org) was used for randomisation. Allocation concealment was ensured through randomisation of participants simultaneously after the decision of inclusion had been made, i.e. there was no foreknowledge about forthcoming allocations. Participants completed all assessments via the internet, which has been shown to be a reliable administration format. Reference Hedman, Ljotsson, Andersson, Andersson, Lindefors and Ruck14,Reference Hedman, Ljótsson, Rück, Furmark, Carlbring and Lindefors23 Potential mediators, which will be reported elsewhere, were measured on a weekly basis. Participants in all conditions received weekly automated SMS reminders to complete these measures. Before treatment start, participants were informed that there would be comprehensive assessments at post-treatment and 6-month follow-up.
Treatments
General description of the treatment model
In all treatment arms the treatment model was the same; the difference between the arms was the mode of delivery. The treatment model emphasised the role of avoidance and safety behaviours as maintaining factors of health anxiety. Reference Furer and Walker24,Reference Furer, Walker and Stein25 The main intervention of the treatment was systematic exposure to health anxiety-related situations or events, in combination with response prevention. As a means to increase the possibility that participants would conduct often highly anxiety-provoking exposure exercises, mindfulness training was also used. Mindfulness was thus not a stand-alone or main component, as in the studies by McManus et al, Reference McManus, Surawy, Muse, Vazquez-Montes and Williams26 but was used to enable exposure. The treatment has previously been shown to be effective for DSM-IV hypochondriasis Reference Hedman, Andersson, Andersson, Ljotsson, Ruck and Asmundson7,Reference Hedman, Axelsson, Gorling, Ritzman, Ronnheden and El Alaoui8,Reference Hedman, Ljótsson, Andersson, Rück, Andersson and Lindefors27 with effects lasting at least 1 year after completed treatment. Reference Hedman, Andersson, Lindefors, Andersson, Ruck and Ljotsson28
In all treatment arms, the intervention was 12 weeks long and built around 12 text modules, equivalent to sessions in conventional treatment. Each module comprised 5–15 pages of text that included the necessary information for behaviour change. For each module there were a set of homework assignments, which the participants were expected to work on on a daily basis. Participants had access to all 12 treatment modules from day 1, and were instructed to complete these in consecutive order (i.e. 1–12). Modules 1 and 2 introduced the CBT model and mindfulness training. The text conveyed that a substantial amount of time and effort was required for the treatment to be effective. Module 3 covered cognitive processes of relevance to health anxiety. Modules 4–10 focused on exposure and response prevention, including interoceptive-, in vivo- and included entailed a plan for relapse prevention. A more detailed description of the treatment content has been previously reported. Reference Hedman, Axelsson, Gorling, Ritzman, Ronnheden and El Alaoui8
Therapist-guided ICBT
Patients in the ICBT arm were provided with access to the treatment modules through a secure internet-based treatment platform. In general, therapist contact was in the form of email-like communication and the patient had the same therapist throughout the treatment. If participants were inactive, for example had not logged on for a week, the therapist would send an SMS, or more rarely, call the participant. Participants were instructed to report at least once a week to their therapist on how their work with the homework assignments was progressing. Participants were, however, always free to send messages to their therapist, who then responded within 2 work days. In the homework reports, participants were generally required to answer both theoretical questions, such as ‘why is avoidance problematic?’, and questions about their practical work, such as ‘describe what exposure exercises you have planned for next week’. After completing the homework for a given module, the participant was given feedback by the therapist and was subsequently encouraged to continue to the next module. Three licensed psychologists and one resident psychologist, all with extensive experience in conducting ICBT, delivered the treatments. On average, therapists spent 63.6 min (s.d. = 35.4) per treated patient and posted 18.4 text messages (s.d. = 9.6).
U-ICBT
This treatment arm was identical to guided ICBT except that no therapist support was provided. The homework assignments were the same but instead of writing a weekly report for a therapist, the participants were instructed to write down the answers to the questions and store them in the online treatment platform.
Bibliotherapy
Participants in this treatment arm were provided with the same modules as in ICBT and U-ICBT, but the modules – including homework assignments and worksheets – were provided as a comprehensive booklet of 154 pages. The booklet was mailed to patients with a brief cover letter explaining how to use the booklet and how to complete weekly assessments throughout the treatment period. At post-treatment, participants in this arm reported how many modules they had completed.
Statistical analysis
Statistical analyses were conducted on an intention-to-treat basis using SPSS version 22.0. Continuous outcome data were analysed using linear mixed-effects model (random intercept) regression analysis for repeated measurements. Such models reduce the risk of committing type 1 errors, give relatively unbiased parameter estimates in the presence of missing data, and have also been shown to be robust in the presence of heteroscedasticity of residuals. Reference Gueorguieva and Krystal29–Reference Verbeke and Molenberghs31 A restricted maximum likelihood approach was used as it produces conservative estimates of standard errors (Satterthwaite correction) when using small sample sizes. Reference Heck, Thomas and Tabata32 In the outcome analyses, each treatment was compared with the control condition (i.e. three comparisons) and all treatments were compared with each other omitting the control condition (i.e. three comparisons). Treatment credibility and adverse events were analysed using t-tests and nominal scale data with χ2 tests. Clinically significant improvement on the primary outcome measure, the HAI, was calculated using the criteria proposed by Jacobson & Truax. Reference Jacobson and Truax33 In the present study, this meant that participants had to make both a reliable change, i.e. an improvement of at least 21 units on the HAI, as well as meeting the criterion of absolute improvement, defined as a total score <70. As a reference, the mean HAI score of healthy controls has been estimated to be 28.9. Reference Salkovskis, Rimes, Warwick and Clark13 The number-needed-to-treat to achieve one case of remission in terms of clinically significant improvement was calculated as the inverse of the absolute risk reduction, comparing each of the treatments to the control condition. Within- and between-group effect sizes (Cohen's d) were calculated using pooled standard deviations. Based on previous RCT data testing the treatment for DSM-IV hypochondriasis Reference Hedman, Andersson, Andersson, Ljotsson, Ruck and Asmundson7 we expected a between-group difference (experimental conditions v. the control group) of 0.8 d. A priori power calculations showed that with an alpha level of 0.05 and 10% data attrition, 30 participants in each arm would be required to yield 80% power to detect a difference.
Results
Attrition and adherence
Of the 132 participants, 132 (100%) completed assessments at baseline and 127 (96%) at post-treatment. Of the 99 participants who were eligible to conduct 6-month follow-up assessments, i.e. excluding the control condition, 89 (90%) completed the assessments. Participants receiving therapist-guided ICBT completed on average 8.6 out of a possible total of 12 modules (s.d. = 3.0), whereas participants in the U-ICBT group completed 6.6 modules (s.d. = 3.6) and the bibliotherapy group 8.3 modules (s.d. = 3.3). Compared with the ICBT group, participants in U-ICBT completed significantly fewer modules (t 61 = 2.3, P = 0.025). No other comparisons between the treatment groups showed significant differences in completed modules (t 61–62 = 1.9 to 0.8, Ps = 0.064–0.709).
Treatment credibility
At week 2 the average C-scale score was 37.1 (s.d. = 6.9) in ICBT, 36.8 (s.d. = 7.9) in U-ICBT and 33.5 (s.d. = 8.3) in the bibliotherapy group. There were no significant differences between the treatment groups regarding treatment credibility as measured by the C-scale (t 61–63 = 0.2–1.9, Ps = 0.067–0.880).
Primary outcome measure
Figure 2 displays the improvement on the primary outcome measure, the HAI, and Table 2 presents means, standard deviations and effect sizes. Mixed-effects models analyses showed that all treatment groups made superior improvements from baseline to post-treatment on the HAI compared with the control condition, as revealed by significant interaction effects of group and time (F 1,62–63 = 28.0–36.6, Ps<0.001). There were no significant interaction effects between treatment group and time (F 1,60–61 = 0.2–0.7, Ps = 0.432–0.715) indicating similar improvement rates from baseline to post-treatment across the three treatments. As indicated by the between-group effect sizes in Table 2, all treatment groups made large improvements on the primary outcome measure compared with the control condition. Table 2 also shows that, for all treatment groups, within-group effect sizes were large and improvements on the primary outcome were maintained at 6-month follow-up.
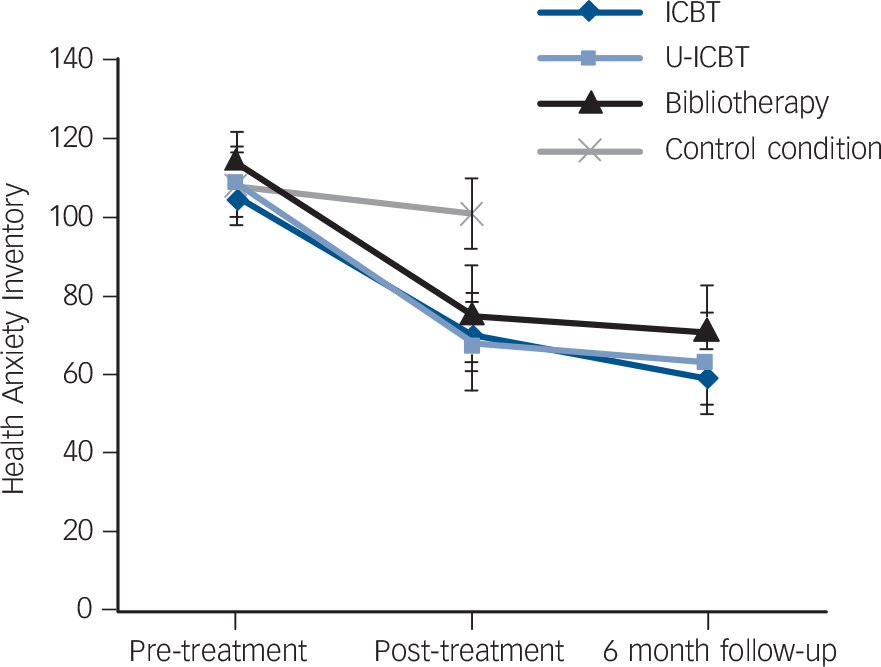
Fig. 2 Change in the primary outcome measure – the Health Anxiety Inventory.
Error bars represent 95% confidence intervals. CBT, cognitive–behavioural therapy; ICBT, internet-based CBT, U-ICBT, unguided internet-based CBT.
Table 2 Means and effect sizes (Cohen's d) on primary outcome measure
| Mean (s.d.) | Effect size (95% CI) | |||||
|---|---|---|---|---|---|---|
| Health Anxiety Inventory (scale range: 0–192) |
Pre-treatment | Post-treatment | 6-month follow up |
Within-group, pre–post treatment |
Within-group, pre–post treatment, pre–6-month follow-up |
Between-group,
a
post-treatment |
| ICBT | 105.5 (21.4) | 69.7 (24.8) | 59.5 (31.3) | 1.55 (0.87–2.22) | 2.23 (1.31–3.14) | 1.27 (0.72–1.79) |
| U-CBT | 109.1 (25.8) | 68.3 (35.6) | 62.9 (34.2) | 1.31 (0.84–1.78) | 1.52 (0.90–2.15) | 1.02 (0.49–1.53) |
| Bibliotherapy | 114.5 (21.3) | 75.5 (35.0) | 71.5 (31.3) | 1.35 (0.88–1.82) | 1.61 (1.05–2.16) | 0.80 (0.28–1.30) |
| Control condition | 108.2 (24.1) | 100.1 (26.1) | – | 0.29 (0.15–0.42) | – | Reference |
ICBT, therapist-guided internet-delivered exposure-based cognitive–behavioural therapy; U-ICBT, unguided internet-delivered exposure-based cognitive–behavioural therapy; Bibliotherapy, unguided exposure-based cognitive–behavioural bibliotherapy.
a. Between-group effect sizes are based on the control condition as comparator.
Secondary outcome measures
Online Table DS1 presents means, standard deviations and effect sizes for the secondary outcome measures. There were significant interaction effects of group and time (baseline to post-treatment) on the complementary health anxiety measures IAS and WI (F 1,62–63 = 20.4–30.3, Ps<0.001), indicating larger reductions of health anxiety in all treatment groups compared with the control condition. There were no significant baseline to post-treatment differences in health anxiety reduction on the IAS and the WI (F 1,62–63 = 0.1–0.5, Ps = 0.489–0.895) when comparing the three treatment groups. Between-group effect sizes on the IAS and WI were large for all three treatment groups, using the control condition as comparator. All three treatment groups made superior baseline-to-post-treatment improvements compared with the control condition in terms of anxiety sensitivity as measured with the ASI (F 1,62–63 = 12.4–18.1, Ps = 0.001), and there were no significant interaction effects between the three treatment groups (F 1,62–63 = 0.0, Ps = 0.899–0.950). Compared with the control condition, the U-ICBT group and the bibliotherapy group made significantly larger reductions in general anxiety as measured with the BAI and depressive symptoms as measured with the MADRS-S (F 1,63–64 = 4.0–8.1, Ps = 0.006–0.049), whereas the ICBT group did not (F 1,63 = 0.4–3.1, Ps = 0.079–0.506). There were no significant differences between the three treatment groups in improvement on the BAI or the MADRS-S (F 1,61–64 = 0.0–2.3, Ps = 0.137–0.818). The ICBT group made significantly larger improvements regarding functional impairment as measured with the SDS compared with the control condition (F 1,61 = 5.2, P = 0.026), but the U-ICBT and bibliotherapy group did not (F 1,64 = 1.2–2.8, Ps = 0.100–0.280). There were no significant differences in improvement on the SDS between the treatment groups (F 1,64 = 0.1–1.3, Ps = 0.250–0.729).
Clinically significant improvement
At post-treatment, the proportion of participants in remission, i.e. meeting criteria for clinically significant improvement on the primary outcome measure, the HAI, was: ICBT 53%, U-ICBT 48%, bibliotherapy 44%, control condition 0%. At 6-month follow-up, the corresponding proportions were 53, 48 and 47%. Consequently, χ2-tests showed that a significantly larger proportion of participants in all treatments were clinically significantly improved compared with those in the control condition (χ2 1 = 18.8–23.7, Ps<0.001). There were no significant differences between the three treatment arms (χ2 1 = 0.1–0.5, Ps = 0.464–0.720). At both post-treatment and 6-month follow-up, the number needed to treat to achieve one case of remission in terms of clinically significant improvement was 1.9 in ICBT and 2.1 in U-ICBT. The corresponding numbers needed to treat in the bibliotherapy group were 2.3 and 2.1.
Treatment satisfaction
Out of a possible total score of 32 on the CSQ-8, the mean post-treatment score in the ICBT group was 26.4 (s.d. = 4.6). Among participants who received U-ICBT and bibliotherapy, the corresponding means were 24.8 (s.d. = 4.1) and 24.0 (s.d. = 5.5). There were no significant differences in treatment satisfaction between treatment groups (t 60 = 0.7–1.8, Ps = 0.073–0.501).
Adverse events
Data on adverse events were collected at post-treatment and showed that 6 participants (19%) in ICBT, 4 (12%) in U-ICBT, 3 (9%) in bibliotherapy and 2 (6%) in the control condition experienced an adverse event during the treatment period. There were no significant differences in terms of adverse events between the four trial arms (χ2 1 = 0.1–2.6, Ps = 0.108–0.722). The most commonly reported adverse event was increased anxiety. There were no reports of serious adverse events.
Discussion
To our knowledge, this is the first study investigating the effect of any form of treatment on the new DSM-5 disorders SSD and IAD. Using a randomised controlled design, 12 weeks of exposure-based CBT in the form of guided or unguided internet treatment or bibliotherapy led to large and significant improvements on the primary outcome compared with the control condition. The three treatments produced similar effects and there were no significant differences in improvements between them on any of the health anxiety measures. Effects were maintained at long-term follow-up and the number needed to treat to achieve one case of clinically significant improvement was about two. This study showed that an exposure-based treatment with minimal or no therapist guidance can be highly effective in the treatment of SSD and IAD.
As there are no previously reported treatment studies of SSD and IAD the results found in the present trial cannot be directly compared with other psychological and pharmacological treatments. In comparison with treatment of DSM-IV hypochondriasis the effects of the present study are similar to those of previous studies investigating the same treatment model delivered as therapist-guided ICBT Reference Hedman, Andersson, Andersson, Ljotsson, Ruck and Asmundson7,Reference Hedman, Axelsson, Gorling, Ritzman, Ronnheden and El Alaoui8 and as CBT delivered in a face-to-face format. Reference Hedman, Ljótsson, Andersson, Rück, Andersson and Lindefors27 Considering that 86% of participants in this study met diagnostic criteria for SSD this suggests that treatment models designed to target maintaining mechanisms of hypochondriasis are also valid to be applied in the treatment of SSD.
Two important findings of the present study were that neither a therapist nor the internet as a mode of delivery was required for achieving large effects of clinical relevance. Also, participants' satisfaction with treatment was largely the same in all three treatments. That therapist support seemed to be of limited additional value could be viewed as unexpected against the background that previous meta-analytic studies on other psychiatric disorders than SSD/IAD/hypochondriasis have suggested therapist support may be of high relevance (for example Spek et al Reference Spek, Cuijpers, Nyklicek, Riper, Keyzer and Pop34 ). A limitation in the body of knowledge is, however, that few published studies have used a randomised controlled design where only therapist guidance, i.e. present or not, has been manipulated. In studies where that has actually been done, therapist guidance has not been consistently associated with significantly larger effects (for example Furmark et al, Reference Furmark, Carlbring, Hedman, Sonnenstein, Clevberger and Bohman35 Berger et al Reference Berger, Hammerli, Gubser, Andersson and Caspar36 ). It is important to point out that there are several different kinds of internet-based treatments and that the one used in the present study is conducted in a highly structured treatment context. We regard it as likely that this structured setting, where the patient makes a commitment to work intensively with the treatment for 12 weeks and is informed that there will be comprehensive follow-up assessments, is an important factor for the large effects and the low attrition rates seen in all the active treatment arms.
Clinical implications
We regard the findings of the present study to be of high relevance from a clinical perspective. First, this study indicates that SSD and IAD can be effectively treated with exposure-based CBT. Second, as these treatments required minimal or even no therapist contact they have the potential to be used to increase accessibility to psychological treatment for these patient groups. Third, the similar effects found in bibliotherapy and internet-based treatments suggest that the former may be an effective, practical and cost-effective option for psychiatric or primary care clinics that are unable to set up an internet-based treatment platform. Fourth, this study provides evidence of similarity between DSM-IV hypochondriasis and SSD in two respects. There was a high proportion of patients meeting diagnostic criteria for both disorders, and the exposure-based treatment – which was the same as that used in previous trials on hypochondriasis – showed similar effects as in hypochondriasis trials using the same primary outcome. Reference Hedman, Andersson, Andersson, Ljotsson, Ruck and Asmundson7,Reference Hedman, Axelsson, Gorling, Ritzman, Ronnheden and El Alaoui8 This may suggest that previous knowledge on hypochondriasis to a large extent is applicable to SSD. As described by Rief & Martin, Reference Rief and Martin37 it should, however, be noted that the new SSD diagnosis fits a wide variety of symptoms and we regard it as plausible that the present sample, mainly characterised by health anxiety, thus represents only a portion of the entire SSD population.
Strengths and limitations
Central strengths of the present study were the randomised design, the well-validated outcome measures, the thorough diagnostic assessment and the low attrition rates. Limitations included that the number of participants with an IAD diagnosis was too low to allow investigation of whether diagnosis, i.e. SSD v. IAD, moderated the outcome. Also, power to detect differences between the active treatments was limited. The effect sizes of the present study, however, suggest that potential true differences between treatments may be of limited clinical relevance. It would also have been desirable to have 6-month follow-up between-group comparison with the control condition, but for ethical reasons those participants were crossed over to treatment after 12 weeks. The type of control group used, i.e. where participants did not receive active treatment, also deserves comment. As stated by Mohr et al, Reference Mohr, Spring, Freedland, Beckner, Arean and Hollon38 in this early trial phase, a no-treatment control group can be justified as it protects against traditional threats to internal validity and it can detect possible adverse effects caused by the experimental condition. It is also a reasonable control group from a stakeholder perspective, meaning that the increased power of this type of control group reduces the risk of type 2 errors, which could hinder implementation of a new potentially useful treatment. Finally, a previously conducted RCT testing this treatment for DSM-IV hypochondriasis showed that it is superior to an active psychological treatment, Reference Hedman, Axelsson, Gorling, Ritzman, Ronnheden and El Alaoui8 indicating that there is a specific effect of systematic exposure and response prevention. Important areas for future research are to compare the treatment with face-to-face CBT, to investigate whether exposure behaviours mediate the treatment effect and to conduct effectiveness studies in routine care settings.
We conclude that exposure-based CBT delivered as therapist-guided or unguided internet treatment or as unguided bibliotherapy can be highly effective in the treatment of SSD and IAD. These treatments have several central advantages with one of the most important being that these treatments can drastically increase accessibility to effective psychological treatment.
Funding
This research was funded by the Karolinska Institutet and Stockholm County Council, neither of which had any role in the design, execution or publication of the study.







eLetters
No eLetters have been published for this article.