Introduction
Substance use disorders (SUDs) are a public health crisis in the United States (U.S.), with over 46 million Americans meeting the definition for having an SUD (Office of the U.S. Surgeon General, 2022; SAMHSA, 2022). SUDs, defined as the recurrent use of alcohol and/or drugs that cause clinically significant impairment in daily life, have far-reaching consequences for both individuals and society (CDC, 2022). Mortality related to SUD is at a historic high with over 100,000 drug overdose deaths and nearly 140,000 deaths due to alcohol use disorder in 2021 (Ahmad et al., Reference Ahmad, Rossen and Sutton2021; SAMHSA, 2022). Beyond individual loss of life, SUD imposes significant costs on society via healthcare costs, criminal justice costs, lost productivity costs, and family and generational impacts. The total economic cost of SUD in the U.S. in 2019 was estimated to be approximately $3.7 trillion when including costs related to healthcare, criminal justice, productivity, public assistance administration, research and prevention, and quality of life lost (Recovery Centers of America, 2019).
Despite the significant costs and individual suffering imposed by SUDs, treatment resources do not meet the demands of those in need. In 2021, 95% of people ages 12 and older with SUD did not receive any type of treatment (SAMHSA, 2022). Of those who wanted to access treatment, commonly cited barriers to treatment included the lack of availability of different recovery support services, lack of insurance coverage, and costs associated with treatment (Park-Lee et al., Reference Park-Lee, Lipari, Hedden, Kroutil and Porter2017). Service gaps are plentiful along the entire SUD continuum of care including prevention, harm reduction, screening, referrals, inpatient and outpatient treatment, and other recovery support services (Blevins et al., Reference Blevins, Rawat and Stein2018; Krawczyk et al., Reference Krawczyk, Rivera, Jent, Keyes, Jones and Cerdá2022; Larney et al., Reference Larney, Peacock, Leung, Colledge, Hickman, Vickerman and Grebely2017; Lenahan et al., Reference Lenahan, Rainer, Baker, Goren and Waddell2023; Mintz et al., Reference Mintz, Hartz, Fisher, Ramsey, Geng, Grucza and Bierut2021; Tomko et al., Reference Tomko, Olfson and Mojtabai2022). Expansion of recovery support services has the potential to yield significant benefits for both individuals and society as a whole.
A number of cost–benefit analyses have been conducted on different treatment interventions for SUD, the majority of them finding that the economic benefits of treatment exceed the economic costs (Cartwright, Reference Cartwright2000; Fardone et al., Reference Fardone, Montoya, Schackman and McCollister2023). Positive net benefits have been found for youth prevention programs (Miller & Hendrie, Reference Miller and Hendrie2008), deflection and diversion programs (Aos et al., Reference Aos, Phipps and Barnoski2004; Carey & Finigan, Reference Carey and Finigan2004; Zarkin et al., Reference Zarkin, Cowell, Hicks, Mills, Belenko, Dunlap and Keyes2015), medication-assisted treatment (Fairley et al., Reference Fairley, Humphreys, Joyce, Bounthavong, Trafton, Combs and Oliva2021; Ijioma et al., Reference Ijioma, Pontinha, Holdford and Carroll2021), harm reduction (Ijioma et al., Reference Ijioma, Pontinha, Holdford and Carroll2021), and recovery housing (Cole et al., Reference Cole, Logan, Miller and Scrivner2021, Reference Cole, Logan and Scrivner2022, Reference Cole, Logan, White and Scrivner2023). Many of these cost–benefit analyses are limited to short-term follow-up studies of individuals, single-individual programs, or state systems’ monitoring of outcomes and involve a variety of different methods (Cartwright, Reference Cartwright2000). Due to the variety of data sources and methods employed in these analyses, it is difficult to compare the economic benefits of different treatment programs.
Economic analyses are often important to demonstrate the value of treatment services to support investments and associated expansion, but many recovery programs operate with relatively small operating budgets that are not conducive to the rigorous data collection needed to support individual program cost–benefit analyses (Ashworth et al., Reference Ashworth, Thompson, Fletcher, Clancy and Johnson2022). Further, in addressing community opposition and stigma, and addressing local stakeholders, many recovery programs need to demonstrate local impacts at the state level to secure funding and state support. As such, there is a need for an economic tool that is flexible enough to capture the economic benefits and costs of different recovery support programs that can be easily utilized and adapted by recovery program operators.
In this paper, we outline a tool that can be utilized by different recovery programs along the continuum of care that estimates the benefits and costs of SUD recovery programs. The goal of this tool is to provide owners and operators of recovery programs like recovery housing, residential treatment, and outpatient programs with an accessible and straightforward tool that can be easily adapted to specific needs to estimate the economic costs, benefits, and return on investment for programs. Economic benefits of SUD recovery programs include reduced healthcare utilization, reduced criminal justice involvement, and increased market and household productivity, as well as increased health and well-being as reflected by reduced morbidity and premature mortality. Economic costs of recovery programs include the annual operating costs including staffing, supplies, and programming, as well as any capital costs related to infrastructure and land purchases.
When examining the costs and benefits of different recovery programs, we focus on three recovery service modalities in particular: a recovery house, a recovery campus, and a 30-day residential program as they represent multiple recognized pathways to recovery that vary in their service intensity, financial makeup, and average success rate. Recovery housing, an intervention model designed to support individuals in their recovery by providing stable housing and emphasizing abstinence and peer support, has been found to be associated with positive changes in recovery-related outcomes including substance use, employment, criminal justice involvement, and mental health (Jason & Ferrari, Reference Jason and Ferrari2010; Mericle, Slaymaker, et al., Reference Mericle, Slaymaker, Gliske, Ngo and Subbaraman2022b; Polcin, Reference Polcin2009; HUD, 2015). Based on studies conducted to-date, recovery housing has been found to be a cost-effective resource, especially in rural communities, due to the relatively high success rate and low cost of care (Ashworth et al., Reference Ashworth, Thompson, Fletcher, Clancy and Johnson2022; French et al., Reference French, Popovici and Tapsell2008). A recovery campus program combines aspects of sober living, peer support, clinical services, life skills education, and employment in one location to assist individuals in their recovery. The recovery campus presented in this paper is modeled from the Recovery Kentucky program which currently operates 18 centers serving nearly 2,000 individuals in Kentucky (Cole et al., Reference Cole, Logan, White and Scrivner2023). Short-term residential treatment programs are more clinically focused than both recovery housing and a recovery campus and include more intensive clinical services over a shorter period of time. Due to their intensive level of services, many residential inpatient programs have a higher cost of care (French et al., Reference French, Popovici and Tapsell2008). As many individuals going through residential inpatient programs do not receive adequate follow-up care upon program departure (Bass et al., Reference Bass, Urada, Khurana, Boustead and Joshi2023), especially care pertaining to health-related social needs, the success rate of such programs is often lower than that of recovery housing or recovery campuses (Arbour et al., Reference Arbour, Hambley and Ho2011; de Andrade et al., Reference de Andrade, Elphinston, Quinn, Allan and Hides2019).
We find that there are significant benefits associated with SUD treatment even with a more conservative modeling of recovery benefits. Specifically, we find that a representative recovery housing program in Florida yields a net benefit of $143 million dollars over 20 years with an associated return on investment of $22 per dollar invested. Further, we find that the net benefits of different treatment modalities including a recovery house, a recovery campus, and a residential inpatient program are positive, with returns on investment varying from nearly $22 to $1 per dollar invested. Altogether, we present a versatile tool that can serve a variety of recovery program types that provide location-specific assessments of the costs and benefits of recovery programs.
Methods
We begin by examining the benefits associated with recovery housing programs. Benefits from SUD recovery are numerous and include both direct and indirect benefits. Direct benefits can be captured via an individual’s willingness to pay for reductions in mortality risk and an increase in health and wellbeing, whereas indirect benefits arise from avoided costs pertaining to healthcare utilization, criminal justice involvement, decreased productivity, family and generational impacts, emotional impacts, and public administration. The full suite of indirect benefits from SUD recovery is difficult to quantify. As such, in this model, we focus on the reliably quantified and impactful benefits including avoided healthcare, criminal justice, and productivity costs.
Data
All benefits and costs that were included in this model were informed by the researcher’s experience working with SUD recovery programs, as well as the feedback from recovery program operators and individuals with SUD-lived experience. Specifically, estimates related to avoided healthcare costs and avoided market and household productivity costs were drawn from the economic analysis provided by the Recovery Centers of America (2019) which compiled numerous available datasets (as outlined in Table 1) to estimate the total economic cost of SUD in 2019. Avoided criminal justice cost estimates were informed by state-level criminal justice expenditure data from the Bureau of Justice Statistics (2017a). Table 1 provides an overview of the benefits included in the model, benefit subcategories, as well as associated data sources.
Table 1. Types of benefits included in the model and their associated data sources

First, we focus on quantifying the avoided healthcare costs per person served by a recovery program. We use an estimate of healthcare costs associated with SUD calculated by the Recovery Centers of America which estimated the total costs associated with SUD in the U.S. in 2019 (Recovery Centers of America, 2019). Healthcare costs included in their estimate are those associated with inpatient and outpatient hospital stays, specialty disease, health insurance administration, crime victim healthcare, treatment, and other costs associated with emergency services and prescriptions. In 2019, they estimated that direct healthcare costs associated with SUD were $118.5 billion. As we already calculate the cost associated with a recovery program elsewhere in the model, we subtract healthcare costs associated with SUD treatment and services (approximately $40.4 billion) to avoid double counting. Further, we subtract healthcare costs that are likely to remain after an individual enters long-term recovery, like costs from diseases associated with SUD (approximately $25.8 billion). As such, the total estimated healthcare cost of SUD in the U.S. in 2019, after subtracting SUD treatment costs and specialty disease costs, was approximately $52.35 billion (Recovery Centers of America, 2019). Specifically, this estimate includes healthcare costs related to inpatient and outpatient hospital utilization ($42.2 billion), other medical costs related to emergency services, primary care, prescription drugs ($7.59 billion), insurance administration ($2.53 billion), and crime victim healthcare ($33 million).
As we need a per person with a SUD estimate of healthcare costs, we then divide the total healthcare costs associated with SUD by the estimated number of people with a SUD ages 18 and up in 2017 as estimated by the National Survey of Drug Use and Health (SAMHSA, 2020). As the majority of healthcare cost estimates were informed by 2017 data, we use 2017 as our reference year for the number of people with a SUD. In 2017, there were an estimated 18,708,000 individuals who met the criteria for having an SUD (SAMHSA, 2020). As such, we divide our total estimated healthcare cost informed by the Recovery Centers of America (2019) estimate ($52.35 billion) by the number of individuals with a SUD in 2017 (18.71 million). This gives us average healthcare costs associated with SUD per person with an SUD in 2017 of $2,798. As healthcare costs vary by state, we then weigh the per person healthcare cost by comparing per capita healthcare spending in each state to the U.S. average. Finally, we adjust the per person healthcare cost by state to 2021 dollars to account for general inflation using the Economics and Pricing Tools package in R (Condylios, Reference Condylios2023). We present the adjusted value of avoided healthcare costs per person with an SUD for each state in the Supplementary Materials.
Next, we calculate avoided criminal justice costs per person served by a recovery program. As our tool is designed to capture benefits based on the location of the program, we use state-level criminal justice expenditures from 2017 provided by the Bureau of Justice Statistics (BJS, 2017a). These costs include wages, capital outlays, and other expenditures related to police protection, judicial and legal functions, and the Department of Corrections. The percentage of crime associated with SUD is difficult to measure, however, according to the Federal Bureau of Investigation’s Uniform Crime Reporting, approximately 25% of arrests in the U.S. were related to drug offenses or driving under the influence in 2017 (Criminal Justice Information Services Division, 2017). While this may underestimate the total number of criminal justice expenditures related to SUD, it provides a central estimate from which sensitivity analysis may be conducted. We are then able to calculate the individual SUD criminal justice cost by multiplying the state criminal justice expenditures by the percent of criminal justice expenditures related to SUD (25%) and dividing by the estimated number of individuals with an SUD per state in 2017 (SAMHSA, 2018). We then adjust the per-person criminal justice cost by state to 2021 dollars for inflation using the Economics and Pricing Tools package in R (Condylios, Reference Condylios2023). We present sensitivity analysis for the percent of criminal justice expenditure related to SUD in the Supplementary Materials as well as the adjusted value of avoided criminal justice costs per person with an SUD for each state in the Supplementary Materials.
Next, we examine productivity costs associated with SUD due to premature death, incarceration, absenteeism, and diminished productivity. To calculate the avoided productivity costs per person served by a recovery program, we use the total productivity costs estimated by Recovery Centers of America (2019). In 2019, the Recovery Centers of America estimated that productivity loss costs associated with SUD were approximately $206.75 billion. We subtract the productivity costs of SUD treatment (approximately $14.76 billion) from the total estimate as we are already accounting for the costs of treatment. As such, the estimated total annual productivity cost associated with SUD in our model is estimated to be approximately $192 billion per year (Recovery Centers of America, 2019). We then calculate the productivity cost per person with a SUD in 2019 by dividing the total productivity cost of SUD by the estimated number of people with an SUD in 2019, approximately 20.33 million (SAMHSA, 2020). Dividing $192 billion by 20.331 million, we find the average productivity cost per person with a SUD in 2019 was $9,443. Then, we adjust the average productivity cost per person with an SUD to 2021 dollars (approximately $10,009) to adjust for inflation using the Economics and Pricing Tools package in R (Condylios, Reference Condylios2023).
Finally, we examine the direct benefits of SUD recovery as captured by quality adjusted value of a statistical life year. The value of a statistical life year (VSLY) provides an economic measure of an individual’s tradeoffs between health-related risks and other consumption. VSLY can be calculated with the following formula, where
![]() $ L $
is the life expectancy of an individual,
$ L $
is the life expectancy of an individual,
![]() $ {r}_{\mathrm{VSL}} $
is the personal time discount rate, and
$ {r}_{\mathrm{VSL}} $
is the personal time discount rate, and
![]() $ \mathrm{VSL} $
is the value of a statistical (VSL) estimate used:
$ \mathrm{VSL} $
is the value of a statistical (VSL) estimate used:
 $$ \mathrm{VSL}\mathrm{Y}=\frac{r_{\mathrm{VSL}}\ast \mathrm{VSL}}{1-{\left(1+{r}_{\mathrm{VSL}}\right)}^{-L}} $$
$$ \mathrm{VSL}\mathrm{Y}=\frac{r_{\mathrm{VSL}}\ast \mathrm{VSL}}{1-{\left(1+{r}_{\mathrm{VSL}}\right)}^{-L}} $$
As VSL can differ by context and country in which it is estimated, we use a central VSL estimate ($8,989,328) informed by a systematic review of 21 health-related studies conducted in developed countries (Keller et al., Reference Keller, Newman, Ortmann, Jorm and Chambers2021). Assuming a standard life expectancy for those who enter long-term recovery, we set the life expectancy L to be 78 (CDC, 2024). Our annualized VSLY measure, as informed by Equation (1) and assuming a personal time discount rate of 3% (Li & Pizer, Reference Li and Pizer2021), is $299,545. As we are valuing nonfatal morbidity reductions, we use the quality-adjusted life years (QALY) metric to measure the increased utility of the health status of the individual (ICER, n.d.; Salomon, Reference Salomon and Quah2017). Estimates suggest that SUD reduces the quality of life by 0.13 and 0.20 QALYs, with higher estimates reserved for more severe SUDs (Nicosia et al., Reference Nicosia, Pacula, Kilmer, Lundberg and Chiesa2009). Based on SUD severity indicators commonly measured in recovery research, those who use recovery programs often have more severe SUDs requiring higher levels of care (Johnson et al., Reference Johnson, Rigg and Hopkins Eyles2020), thus we assume the added QALY from successful utilization of a recovery program is 0.20. As such, we calculate the added value of health improvement as QALY (0.20) multiplied by the VSLY ($299,545). From that calculation, we estimate that improved health status and reduced premature mortality risk per year are valued at $59,909. We present a sensitivity analysis around the personal discount rate (
![]() $ {r}_{\mathrm{VSL}} $
), the VSL central estimate (VSL), and the added QALY due to SUD treatment in the Supplementary Materials.
$ {r}_{\mathrm{VSL}} $
), the VSL central estimate (VSL), and the added QALY due to SUD treatment in the Supplementary Materials.
Model
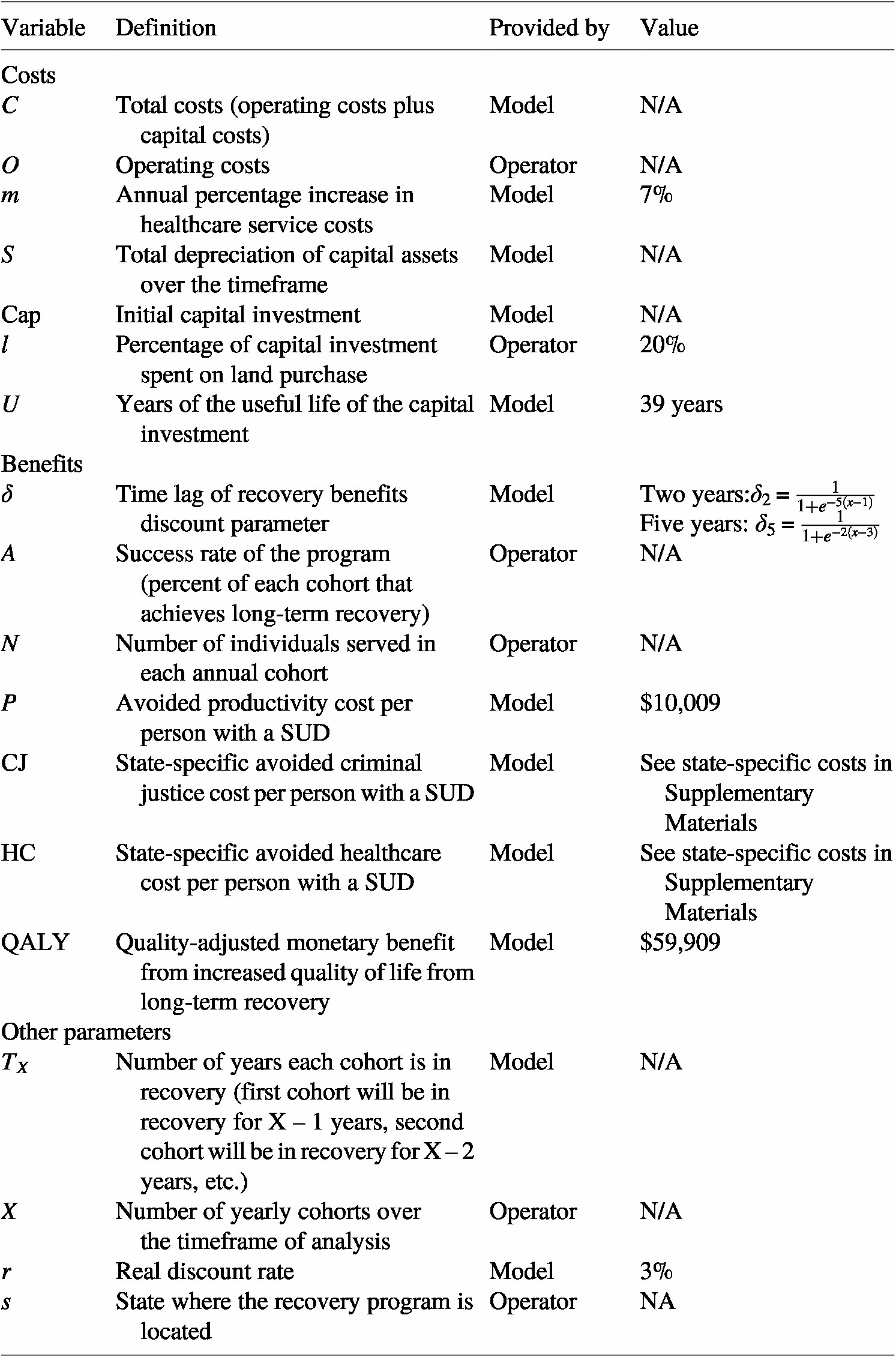
Next, we discuss calculations of the costs and benefits associated with recovery programs. Table 2 provides an overview of the parameters included in the calculations of costs and benefits associated with recovery programs, whether they are informed by the model or the recovery program operators when using the tool, and the value (if applicable) of that parameter.
Table 2. Parameters included in the costs and benefit equations
First, we discuss the costs captured in our model. We capture two aspects of costs associated with a recovery program. First, we capture the variable operating cost of a recovery program across each year. This cost can be assumed to be constant across all years or increase according to planned expansions in the number of individuals served. Further, we include capital costs that may be associated with a recovery program including the cost of purchasing land and construction of buildings. The cost function is as follows:
 $$ C=S+\sum \limits_{x=0}^X\left(O\left(1+m\ast X\right)\right)\ast {\left(1+r\right)}^{-x} $$
$$ C=S+\sum \limits_{x=0}^X\left(O\left(1+m\ast X\right)\right)\ast {\left(1+r\right)}^{-x} $$
where
![]() $ C $
is the total discounted costs,
$ C $
is the total discounted costs,
![]() $ S $
is the capital costs of the project as captured by the depreciation of the capital assets,
$ S $
is the capital costs of the project as captured by the depreciation of the capital assets,
![]() $ O $
is the base year operating cost for each cohort of recovery residents,
$ O $
is the base year operating cost for each cohort of recovery residents,
![]() $ m $
is the percentage increase in healthcare-related costs, and
$ m $
is the percentage increase in healthcare-related costs, and
![]() $ r $
is the real discount rate. Costs associated with providing healthcare services have been shown to be increasing by approximately 7% annually (PwC Health Research Institute, 2024). As such, we assume that the operating costs of recovery programs will likely see the same increase in service costs. As such, we set
$ r $
is the real discount rate. Costs associated with providing healthcare services have been shown to be increasing by approximately 7% annually (PwC Health Research Institute, 2024). As such, we assume that the operating costs of recovery programs will likely see the same increase in service costs. As such, we set
![]() $ m $
equal to 7% such that each year operating costs will increase by 7% from the base year. For example, if the recovery program has an annual operating cost of $100,000 in the first year, the operating cost will increase 7% in the second year ($107,000), 14% in the second year ($114,000), 21% in the third year ($121,000), and so on.
$ m $
equal to 7% such that each year operating costs will increase by 7% from the base year. For example, if the recovery program has an annual operating cost of $100,000 in the first year, the operating cost will increase 7% in the second year ($107,000), 14% in the second year ($114,000), 21% in the third year ($121,000), and so on.
As we want to account for the residual value that land and construction may have after the lifetime of the project, we calculate our total capital costs as follows:
where
![]() $ S $
is the total depreciation of capital assets over the timeframe of analysis,
Cap
is the initial capital investment,
$ S $
is the total depreciation of capital assets over the timeframe of analysis,
Cap
is the initial capital investment,
![]() $ l $
is the percentage of the capital investment that was spent on land,
$ l $
is the percentage of the capital investment that was spent on land,
![]() $ U $
is the years of useful life of the capital, and
$ U $
is the years of useful life of the capital, and
![]() $ X $
is the number of yearly cohorts each recovery program can serve in the timeframe of analysis. According to the above equation, we see that the capital cost is the initial capital investment minus the depreciated residual value of the investment at the end of the planning horizon. We assume standard straight-line depreciation for nonresidential property as outlined by the Internal Revenue Service (IRS, 2022), such that
$ X $
is the number of yearly cohorts each recovery program can serve in the timeframe of analysis. According to the above equation, we see that the capital cost is the initial capital investment minus the depreciated residual value of the investment at the end of the planning horizon. We assume standard straight-line depreciation for nonresidential property as outlined by the Internal Revenue Service (IRS, 2022), such that
![]() $ U $
is equal to 39 years and assumes approximately 20% of capital investments are spent on land.
$ U $
is equal to 39 years and assumes approximately 20% of capital investments are spent on land.
A complication of conducting economic analyses of recovery programs is the modeling of the recovery process itself. SUD recovery is often not a linear process where a treatment intervention occurs, and a person enters recovery for the rest of their life. SUD is a chronic, relapsing disease and studies have shown that people seeking recovery have an average of five recovery attempts before long-term recovery is achieved (Kelly et al., Reference Kelly, Greene, Bergman, White and Hoeppner2019). Further, once long-term recovery is achieved, there may be a delay before the benefits of recovery start accruing. Research assessing different aspects of recovery across time, including recovery capital, quality of life, and psychological distress, found that many recovery indicators take between 2 and 5 years to reach the same levels as individuals who do not have a SUD (Kelly et al., Reference Kelly, Greene and Bergman2018). As such, we include a discount parameter,
![]() $ \delta $
, to model the time-lag of recovery benefits. Specifically, we present cases where
$ \delta $
, to model the time-lag of recovery benefits. Specifically, we present cases where
![]() $ \delta $
is equal to one to represent a linear and immediate model of recovery, where
$ \delta $
is equal to one to represent a linear and immediate model of recovery, where
![]() $ \delta $
is a logistic function where benefits begin to be fully accrued after two years and a case where
$ \delta $
is a logistic function where benefits begin to be fully accrued after two years and a case where
![]() $ \delta $
is a logistic function where benefits begin to fully accrue after 5 years.Footnote
1
$ \delta $
is a logistic function where benefits begin to fully accrue after 5 years.Footnote
1
To calculate the present value of benefits from a recovery program, we sum the benefits associated with recovery (avoided criminal justice, productivity, and healthcare costs and reduced morbidity and premature mortality) for each annual cohort served by the recovery program that enters long-term recovery overall cohorts served. The present value of benefits of recovery programs is as follows:
 $$ B(s)=\sum \limits_{x=1}^X(\sum \limits_{t=0}^{T_X}[\delta (t)\ast (N\ast A)\ast [P+\mathrm{C}\mathrm{J}(s)+\mathrm{H}\mathrm{C}(s)+\mathrm{Q}\mathrm{A}\mathrm{L}\mathrm{Y}]]\ast {(1+r)}^{-t}) $$
$$ B(s)=\sum \limits_{x=1}^X(\sum \limits_{t=0}^{T_X}[\delta (t)\ast (N\ast A)\ast [P+\mathrm{C}\mathrm{J}(s)+\mathrm{H}\mathrm{C}(s)+\mathrm{Q}\mathrm{A}\mathrm{L}\mathrm{Y}]]\ast {(1+r)}^{-t}) $$
where
![]() $ X $
is the number of yearly cohorts each recovery program can serve in the timeframe of analysis,
$ X $
is the number of yearly cohorts each recovery program can serve in the timeframe of analysis,
![]() $ T $
is the number of years each cohort of recovery program participants is in recovery,
$ T $
is the number of years each cohort of recovery program participants is in recovery,
![]() $ \delta (t) $
is the time-lag of recovery benefits discount parameter,
$ \delta (t) $
is the time-lag of recovery benefits discount parameter,
![]() $ r $
is the real discount rate,
$ r $
is the real discount rate,
![]() $ N $
is the number of individuals served in each annual cohort,
$ N $
is the number of individuals served in each annual cohort,
![]() $ A $
is the success rate of the program defined as the percent of individuals that achieve long-term recovery due to the recovery program,
$ A $
is the success rate of the program defined as the percent of individuals that achieve long-term recovery due to the recovery program,
![]() $ P $
is the avoided productivity cost per person with a SUD,
$ P $
is the avoided productivity cost per person with a SUD,
![]() $ \mathrm{CJ}(s) $
is the state-specific avoided criminal justice cost per person,
$ \mathrm{CJ}(s) $
is the state-specific avoided criminal justice cost per person,
![]() $ \mathrm{HC}(s) $
is the state-specific avoided healthcare cost per person, and
$ \mathrm{HC}(s) $
is the state-specific avoided healthcare cost per person, and
![]() $ \mathrm{QALY} $
is the quality-adjusted monetary benefit from the increased quality of life due to the recovery program. The estimated value of a recovery program is a function of the state in which it is located,
$ \mathrm{QALY} $
is the quality-adjusted monetary benefit from the increased quality of life due to the recovery program. The estimated value of a recovery program is a function of the state in which it is located,
![]() $ s $
. Specifically, the avoided healthcare and criminal justice costs differ by the state in which the program is located. Because we do not include dynamic modeling of individuals’ lifespans who achieve long-term recovery, the planning horizon or number of yearly cohorts each program can serve,
$ s $
. Specifically, the avoided healthcare and criminal justice costs differ by the state in which the program is located. Because we do not include dynamic modeling of individuals’ lifespans who achieve long-term recovery, the planning horizon or number of yearly cohorts each program can serve,
![]() $ X $
, has a maximum value of 30 as it is unlikely that those who enter long-term recovery due to the program would continue to live and accrue benefits more than 30 years past when they entered the recovery program.
$ X $
, has a maximum value of 30 as it is unlikely that those who enter long-term recovery due to the program would continue to live and accrue benefits more than 30 years past when they entered the recovery program.
Benefits are calculated such that all individuals in a cohort that achieve long-term recovery accrue benefits associated with recovery for the remaining timeframe of analysis. For example, if a recovery program serves 20 annual cohorts, the timeframe of analysis would be 20 years. The individuals that achieve long-term recovery in the 1st year of the program’s operation would accrue recovery benefits for 19 years and the individuals that achieve long-term recovery in the 2nd year of the program would accrue recovery benefits for 18 years. Total benefits each year is a cumulative sum of the benefits in a year by all individuals that have achieved long-term recovery in all years prior. For example, the total annual benefits in year 3 of the program would be the annual benefits accrued from recovery for those individuals who entered long-term recovery in years 1 and 2.
Finally, the present value of net benefits is calculated by subtracting the total costs informed by Equation (2) from the total benefits informed by Equation (4). Additionally, the return on investment of a recovery program is calculated by dividing the net benefits by the total costs.
Results
In this section, we present results from a series of use cases as well as sensitivity and break-even analyses regarding key parameters. Table 3 shows the benefits, costs, net benefits, and return on investment for a baseline recovery program that was parameterized to be representative of an average recovery housing program serving 50 residents annually. Specifically, the representative recovery housing program has an average annual operating cost of $250,000 per year and an initial capital cost of $670,000. We set the location of the recovery house in Florida as Florida has the highest estimated number of recovery houses in the U.S. (Mericle et al., Reference Mericle, Patterson, Howell, Subbaraman, Faxio and Karriker-Jaffe2022a). We set the success rate, the percentage of residents served that enter long-term recovery for the entire time horizon, at 35% as indicated by studies on recovery housing length of stay (Aase et al., Reference Aase, Jason, Ferrari, Li and Scott2014; Jason et al., Reference Jason, Davis and Ferrari2007a; Jason et al., Reference Jason, Salina and Ram2016; Jason et al., Reference Jason, Olson, Ferrari, Majer, Alvarez and Stout2007b). Finally, we set the time horizon of the analysis at 20 years such that the recovery program is serving 20 yearly cohorts.
Table 3. Benefits, costs, and return on investment of Baseline Recovery Program* across different models of recovery including linear model, 2-year time lag of benefits, and 5-year time lag of benefits

* Parameter values informed by program: Number of yearly cohorts (X) = 20, Number of residents served in each annual cohort (N) = 50, state where program is located (s) = Florida, operating costs (O) = $250,000 per year, capital investments (Cap) = $670,000, Percentage of each cohort that achieves long-term recovery (A) = 35%.
With no time lag of benefits factored into our calculation, we find that the present value of net benefits of a representative recovery house is positive and substantially large. Specifically, we find that total benefits are estimated to be $199 million and total costs of the recovery program are estimated to be $6.5 million, leading to net benefits of approximately $192.6 million over 20 years. The majority of the benefits accrued come from morbidity and premature mortality risk reductions (77%), with the next largest portion of benefits being accrued from avoided productivity costs (13%). Avoided healthcare and criminal justice costs both accounts for approximately 6% and 5%, respectively, of the total benefits accrued from the recovery housing program. The return on investment with no time lag of benefits is approximately $29.80 per dollar invested into the program. More conservative estimates of the economic impacts of a representative recovery house also show significant economic benefits. Including a two-year time lag in the accrual of benefits decreases the net benefits by approximately 5.5% or $10.6 million. Similarly, including a 5-year time lag decreases the net benefits by 25.5% or $49.2 million. Even with a more conservative estimate of the value of a recovery housing program that includes a 5-year time lag, the return on investment of the program is substantial at $22.19 per dollar invested.
Next, we examine the economic value of different types of recovery programs, including a singular recovery housing program, a recovery campus program, and a residential inpatient program. We parameterize the recovery housing program based off a representative recovery house serving 100 residents in Florida with an operating cost of $500,000 per year, capital costs of $1.34 million, and a success rate of 35% (Ashworth et al., Reference Ashworth, Thompson, Fletcher, Clancy and Johnson2022). We examine a recovery campus that serves 100 individuals annually in Florida with an operating cost of $2.8 million per year, capital costs of $12.5 million, and a success rate of 45% (Cole et al., Reference Cole, Logan, White and Scrivner2023). Finally, we parameterize a residential inpatient program based off research on the average costs of residential programs as well as a search of nonprofit residential inpatient program capital costs (French et al., Reference French, Popovici and Tapsell2008). Specifically, we examine a residential clinical program in Florida serving 100 people each year with an annual operating cost of $3.9 million, capital costs of $3.5 million, and a success rate of 23%. Table 4 shows the economic benefits, costs, and return on investment across the three treatment modalities.
Table 4. Economic characteristics, benefits, and costs across different recovery program types assuming a 5-year time lag in benefits

We find positive net benefits across all recovery programs examined, with the highest return on investment attributed to the recovery housing program ($22.19), followed by the recovery campus ($4.18), and finally the residential clinical program ($1.01). Recovery housing has a higher rate of return on investment due to its significantly lower costs and comparable success rates compared to the recovery campus and residential clinical programs. A recovery campus program yields 8% more in net benefits than recovery housing but at a significantly higher cost. While the residential clinical program has the lowest return on investment and net economic benefits of the three treatment modalities examined, it still yields over $99 million in net benefits across 20 years.
As the success rate of the program can be the most difficult to estimate, especially for smaller programs with limited data collection capacities, we conduct sensitivity analyses for each recovery program type across different success rate assumptions. The present value of net benefits for the recovery house is positive given a success rate of approximately 2%. The present value of net benefits for the recovery campus and the residential inpatient program are 9% and 12%, respectively.
Discussion
In this paper, we present an adaptable tool that can be utilized by a variety of different types of recovery programs to assess the economic costs and benefits associated with their program. We find that, for representative cases of different types of recovery programs including recovery housing, a recovery campus, and a residential clinical program, that the net present value of the programs is positive. We find that a representative recovery house serving approximately 100 people has a total economic value of almost $143 million over 20 years. We find that even for more costly, high-intensity treatment models like residential clinical programs, the net benefits of the program are positive, with a return on investment of over $1 per dollar invested over 20 years. Although there is often much uncertainty about the actual success rates of different recovery programs, we show that net benefits of different programs remain positive even at success rates as low as 12%.
Our results highlight the importance of considering the multifaceted impacts of SUD both on individuals and society as a whole. Cole and coauthors estimate that, in 2023, the Recovery Kentucky centers had an estimated $2 return on investment (Cole et al., Reference Cole, Logan, White and Scrivner2023). Comparatively, our model suggests that a recovery campus program parameterized similarly to the Recovery Kentucky centers would lead to a $4 return on investment as we account not only for avoided costs but also the additional indirect benefits of improved quality of life and reduced premature morbidity due to SUD. Cost–benefit analyses that account only for the indirect costs in terms of lives lost due to SUD or only the direct costs of criminal justice, healthcare, and productivity are not capturing the full picture of the benefits that recovery entails.
Our model has several limitations that are important to note. First, we model recovery as a linear process where individuals going through the program either enter long-term recovery or they do not. Recovery is not a linear process, with most individuals in long-term recovery indicating that they had attempted to recover five or more times before finally entering long-term recovery (Kelly et al., Reference Kelly, Greene and Bergman2018, Reference Kelly, Greene, Bergman, White and Hoeppner2019). To account for some of the nonlinearity of the recovery process, we include a time lag in the model where benefits from being in recovery do not fully start accruing until five years after leaving the program. Further, long-term recovery does not necessarily mean total abstinence from substances for everyone. Recovery from SUD is increasingly being recognized as meeting recovery goals, even if those goals include moderation of use rather than complete abstinence (Eddie et al., Reference Eddie, Bergman, Hoffman and Kelly2022; SAMHSA, 2012; Stea et al., Reference Stea, Yakovenko and Hodgins2015; Witkiewitz & Tucker, Reference Witkiewitz and Tucker2020). As such, this modeling tool may not be applicable to programs that promote moderation and harm reduction as the full suite of benefits included in the model may not apply. Additionally, longitudinal studies are needed to quantify health service utilization, productivity, criminal justice involvement, and QALYs related to these clinical outcomes of harm reduction programs.
Second, our model does not capture all the costs or benefits associated with recovery programs. Our model does not account for the generational impacts of SUD, nor the impact SUD can have on children whose caregivers have a SUD and associated child welfare service costs, such as foster care. Further, we do not account for all the public assistance and prevention costs that are associated with SUD. On the cost side, we do not account for the lost utility individuals may face from withdrawing from different substances, nor the opportunity cost of time residents may have during treatment. Our model focused on the largest, most reliably quantified costs and benefits associated with recovery programs to provide an estimate of the economic costs and benefits. Future research is also needed to expand this model, specifically modeling the generational impacts of SUD, as well as examining ways in which the individual costs of SUD treatment are better captured.
Finally, our model and the estimates of the avoided healthcare, productivity, and criminal justice costs are all based on data that were collected prior to the COVID-19 pandemic. While this does allow for estimates of the costs of SUD without the distortions caused by the pandemic, it does not account for the increased incidence of SUD in the past five years, nor the increasing impacts of fentanyl in the drug supply. Mortality and morbidity associated with SUD have increased significantly in the past five years in part due to the rise of synthetic opioids like fentanyl and the COVID-19 pandemic (Alexander et al., Reference Alexander, Stoller, Haffajee and Saloner2020; Becker & Fiellin, Reference Becker and Fiellin2020; Hedegaard, Reference Hedegaard2021). As such, the data used to estimate the costs of SUD in this model may underestimate the real costs of SUD in the U.S. Further, our data sources for many of the avoided costs differed in the year for which data was available. Healthcare and criminal justice cost estimates were informed primarily by data from 2017, whereas productivity cost data was informed by estimates from 2019. This discrepancy may impact the relative share of benefits that can be attributed to each type of benefit and neglect to capture any changes that might have occurred between those two years that may have fundamentally changed cost estimates. Future work and iterations of this model will benefit by using the most up-to-date data to ensure the costs of SUD are accurately captured.
Altogether, we present an adaptable and customizable tool for cost–benefit analyses of recovery programs that can be used by recovery programs across the U.S. Such analyses can help recovery program operators communicate with stakeholders about their economic value, plan service expansions, and document outcomes.Footnote 2
Supplementary material
The supplementary material for this article can be found at http://doi.org/10.1017/bca.2024.26.
Acknowledgments
We want to thank Fletcher Group leadership and outreach and engagement specialists for their continued support of research efforts and recovery housing across the U.S. Specifically, we would like to thank Grant Meyer, Joe Smallman, and Nathaniel Conklin for their constructive feedback.
Funding statement
This publication was supported by the Health Resources and Services Administration (HRSA) of the US Department of Health and Human Services (HHS) under grant number UD9RH33631-01-00 as part of an award totaling $3.3 M with 0% financed with nongovernmental sources. The contents are those of the authors and do not necessarily represent the official views of, nor endorsed by HRSA, HHS, or the US Government.
Competing interest
The authors have no potential conflicts of interest or financial disclosure.






