Intradural pathologies, such as spinal intradural hematoma (SIDH) and arachnoid cysts, are rare causes of spinal cord compression. When an SIDH occurs, it typically manifests from vascular malformations, tumors, bleeding disorders, anticoagulant therapy, or following a trauma or infection.Reference Gehri, Zanetti and Boos 1 - Reference Chang, Samartzis, Luk, Cheung and Wong 5 Iatrogenic causes of SIDH include diagnostic lumbar punctures and epidural anesthesia.Reference Chang, Samartzis, Luk, Cheung and Wong 5 Spinal arachnoid cysts are thought to be caused by a congenital deficiency within the arachnoid or adhesions resulting from previous infection or trauma.Reference Hughes, Ugokwe and Benzel 6
Instances of SIDH following lumbar spine surgery are rare.Reference Gehri, Zanetti and Boos 1 , Reference Chang, Samartzis, Luk, Cheung and Wong 5 Most have been associated with accidental dural tear during the procedure.Reference Gehri, Zanetti and Boos 1 Few cases have been reported following spinal surgery where the dura remained intact.Reference Chang, Samartzis, Luk, Cheung and Wong 5 Similarly, there are few reports documenting an arachnoid cyst causing acute neurological injury following uncomplicated lumbar spinal surgery.Reference Valls, Naul and Kanter 7 To our knowledge, there have been no cases in which the preoperative imaging did not show any evidence of a preexisting cyst.
We report on a case of an acute concurrent SIDH and arachnoid cyst presenting immediately following uncomplicated lumbar decompression and fusion surgery. Permission to report this case was obtained from the patient.
A 72-year-old male presented after 10 years of increasing bilateral claudicant leg and lower back pain. Conservative management including physiotherapy, chiropractic manipulations, and uncomplicated epidural steroid injections had failed. Medical history was positive for non-insulin-dependent diabetes mellitus, and he was not on any anticoagulation therapy or acetylsalicylic acid. Preoperatively, his leg pain was 8 of 10 in severity and he scored 25 of 100 on the EuroQol 5D Health Scale. Physical examination revealed grade 4 of 5 weakness in the L5 myotome bilaterally. Preoperative needle electromyography revealed decreased activation of the peroneal muscles and borderline slowing of motor conduction velocity. No signs of myelopathy were present. Preoperative radiological investigations performed before and following epidural injections showed degenerative grade 1 spondylolisthesis at L4-L5 (Figure 1A, B) and no signs of intradural pathology. Dynamic flexion-extension radiography demonstrated instability at this level.
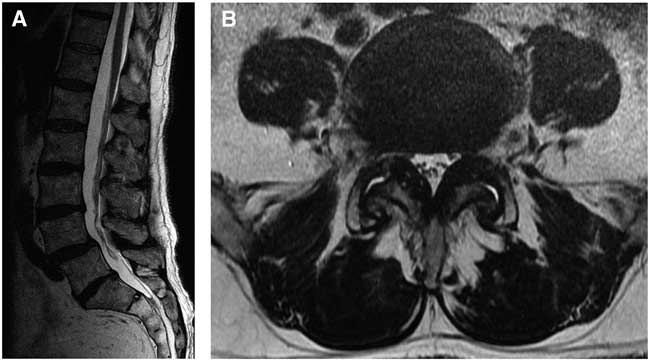
Figure 1 Preoperative T2 weighted sagittal (A) and axial (B) MRI scans from T10 to sacrum showing L4-L5 degenerative spondylolisthesis and lateral recess stenosis. No intradural pathology was noted.
The patient underwent an uncomplicated L4-L5 posterior microdecompression (bilateral decompression via a unilateral approach with preservation of the spinous process and contralateral lamina) under microscopic visualization with L4-L5 minimally invasive transforaminal lumbar interbody fusion using a PEEK (Stryker; Hamilton, ON, Canada) banana-shaped cage and local bone graft. Instrumentation was augmented with bilateral cannulated percutaneous pedicle screw fixation placed using a combination of computer assisted three-dimensional navigation and fluoroscopy (Figure 2A, B). Neuromonitoring with electromyography, somatosensory-, and motor-evoked potential was used throughout and did not indicate any nerve encroachment. There was no excessive manipulation of the nerve roots for the decompression or cage insertion. Care was taken to ensure the dura was intact before final closure, including Valsalva maneuver, which did not elicit any cerebrospinal fluid leak. Bleeding was well controlled with bipolar electrocautery and Floseal (Baxter Corporation; Mississauga, ON, Canada) hemostatic agent, and there was no pooling of blood over the nerve roots before closure. Only sequential compression devices were used for thromboembolic prophylaxis. Initial postoperative examination was limited because of postanesthesia sedation, but the patient had motor function in all lumbar myotomes.
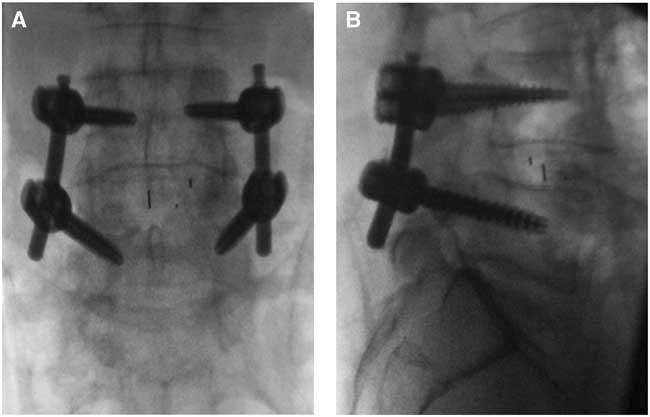
Figure 2 Intraoperative anteroposterior (A) and lateral (B) fluoroscopic images of L4-L5 interbody and pedicle screw fixation.
On postoperative day 1, the patient complained of increasing lower limb weakness with grade 2 of 5 strength in all lumbar nerve root distributions along with decreased sensation. Urgent magnetic resonance imaging (MRI) scans of the total spine revealed postoperative changes including an epidural hematoma causing severe central canal stenosis at L4-L5 and a superiorly located intradural collection causing severe displacement and compression of the adjacent nerve roots (L1-L5) (Figure 3A-C). There was heterogeneous T1 and T2 signal at the L4-L5 level in keeping with an extradural hematoma. A separate collection with high T2 and low-to-isointense T1 signal that extended superiorly to the L1 level represented an arachnoid cyst and intradural hematoma on imaging. This was classified as intradural because epidural fatty tissue was present without displacement of the dura mater.
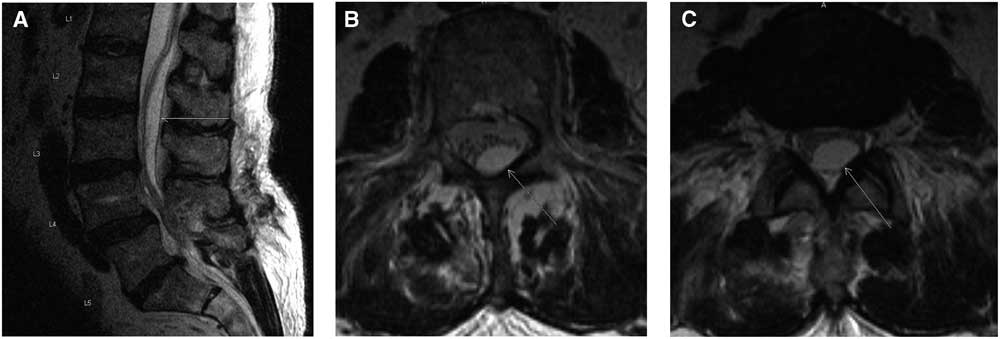
Figure 3 Immediate postoperative T2-weighted mid-sagittal (A), axial at L2 (B), and axial at L2-L3 (C) MRI scans. The arrow shows the intradural cyst with displacement of the cauda equina nerve roots anteriorly within the dural sac.
The patient was brought back for an emergency spinal decompression and durotomy. Intraoperative findings revealed an extradural hematoma at the L4-L5 level. After durotomy, the arachnoid was noted to be bulging posteriorly and xanthochromic cerebrospinal fluid was observed and released. The nerve rootlets were noticed to be anteriorly displaced. An arachnoid cyst was found from L2-L5, which was then subsequently decompressed with fenestration. Postoperatively, the patient recovered partial motor and sensory function with grade 4 motor power. After 1 year, the patient indicated he was “somewhat satisfied” with the results of the spine surgeries. His leg pain was 6 of 10 in severity, and he scored 65 of 100 on the EuroQol 5D Health Scale. Repeat MRI scans demonstrated no recurrences at 1 year follow-up (Figure 4A-C).
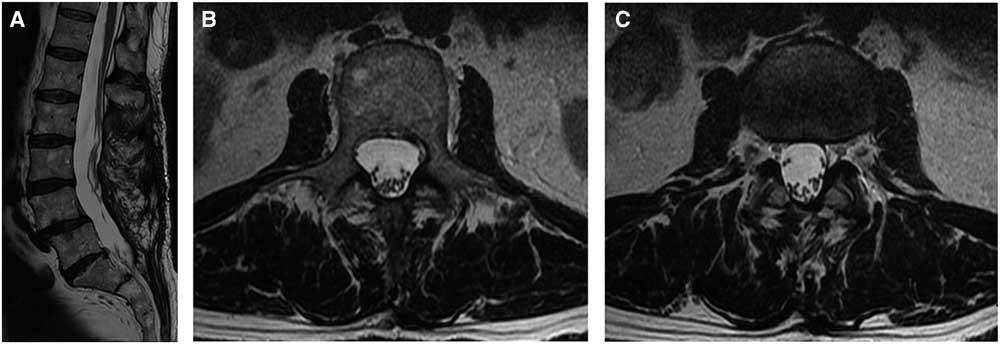
Figure 4 One year postoperative T2-weighted mid-sagittal (A), axial at L2 (B), and axial at L2-L3 (C) MRI scans showing the resolution of the intradural cyst.
This is the first case report describing an acute postoperative intradural complication proximal to the level of surgery. Few cases have reported acute spontaneous arachnoid cyst developing postoperatively and even fewer report concomitant intradural hematomas.Reference Nath, Mishra, Deo and Satapathy 2 - Reference Nesterenko, Dewan, Nair and Peroutka 4
Basaldella et alReference Basaldella, Orvieto, Dei Tos, Della Barbera, Valente and Longatti 8 summarizes four theorized mechanisms for arachnoid cyst formations: a ball-valve mechanism; an osmotic gradient; a congenital malformation; and hypersecretory fluid production. It is possible that the trauma of the surgery created an inflammatory event that led to an acute hypersecretive fluid production; iatrogenic trauma is the most commonly recognized factor leading to this. Gehri et alReference Gehri, Zanetti and Boos 1 describe intradural hematoma following a minor dural tear intraoperatively. Chang et alReference Chang, Samartzis, Luk, Cheung and Wong 5 attributes intradural hematoma to traumatic blunt dissection of an adherent dura. In our case, dissection was meticulously carried out under magnification via operating microscope and neuromonitoring revealed no events.
Given the minimal dural manipulation, we theorize that decompression of the dura at L4-L5 led to a sudden change in the lumbar cerebrospinal fluid flow and pressure. This increase of flow followed by decreased flow related to the epidural hematoma may have tipped the homeostatic condition toward an acutely expanding arachnoid cyst, possibly via a ball-valve mechanism above the level of surgery.
Immediate recognition and diagnosis of an expanding intradural pathology is essential, especially in a patient with progressive postoperative weakness. MRI scanning is the imaging modality of choice when questioning development of an intradural pathology.Reference Chang, Samartzis, Luk, Cheung and Wong 5 Intradural and nerve root exploration is a requisite whenever there is suspicion of intradural pathology because not all cysts spontaneously resolve with evacuation of extradural hematoma alone.
Disclosures
The authors do not have anything to disclose.






