CLINICIAN'S CAPSULE
What is known about the topic?
Emergency department (ED) crowding is an international health system issue that increases cost and undermines patient care quality.
What did this study ask?
What throughput interventions are most effective at reducing ED length of stay and left without being seen left without being seen rates?
What did this study find?
While all intervention types reduced length of stay, triage and patient streaming interventions reported the largest reductions in length of stay and left without being seen rates.
Why does this study matter to clinicians?
Local implementation of the most effective intervention types could lessen ED crowding and contribute to increased patient and provider satisfaction.
INTRODUCTION
Emergency department (ED) crowding is an international health system problem that is worsening.Reference Schull, Slaughter and Redelmeier1 Crowding manifests as prolonged patient wait times and ED lengths of stay, along with increased patient mortality and morbidity.Reference Derlet and Richards2–Reference Shih, Ma and Chen5
Prior work has partitioned the causes of ED crowding into three domains: input, throughput, and output.Reference Asplin, Magid and Rhodes6 Input factors impact the volume and complexity of patients presenting to the ED. Output factors, including hospital bed capacity, affect the movement of patients out of the ED when they are discharged or admitted. Throughput factors, which determine the time required to assess and manage patients in the ED, are mostly dependent on ED staff and processes.Reference Handel, Hilton and Ward7,Reference Anderson, Lukas, Jones, Sharma and Bastani8
Many throughput interventions have been described, including physicians or advanced providers at triage, modified staffing models, point-of-care testing, and patient streaming (e.g., fast-track, split-flow).Reference Chan, Reilly and Salluzzo9 Research suggests that these are variably effective, but there are no systematic reviews describing their relative impact on ED throughput. Identifying the most effective throughput interventions will become increasingly important as demand on ED services grows. It will inform health leaders which are likely to be most effective in a given setting and where to direct further study. The objective of this systematic review is to evaluate and summarize the results of studies describing ED throughput interventions.
METHODS
Protocol and registration
Study scope and inclusion/exclusion criteria were registered with PROSPERO prior to the review (registration number CRD42019125651).
Search strategy
We conducted systematic database searches in Medline (Ovid 1946 to April 26, 2020), Embase (Ovid 1974 to April 26, 2020), CINAHL (EBSCO, 1982 to April 26, 2020), and the Cochrane Central Register of Controlled Trials (Ovid, to April 26, 2020) without the use of filters or language restrictions. A sensitive four-component search was designed based on the setting (ED), factor (throughput factors), outcomes (length of stay, left without being seen rate),10 and study design (interventional studies). The ED search term was adapted from an existing search filter.Reference Rogers, Shankar and Jerris11 Search strategies included free text terms and subject headings, where available. We downloaded article references and deduplicated these, using Endnote X8 software. Additional references were obtained through reference chaining of the returned articles. This study adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.Reference Tricco, Lillie and Zarin12
Eligibility criteria
Original research articles describing throughput interventions to reduce ED crowding were considered for inclusion. Studies had to have a concurrent or historical comparison group and report length of stay or left without being seen rates as outcomes. Studies were excluded if they were published only as abstracts, published in a language other than English, or lacked a comparator group.
Screening and data extraction
After eliminating duplicates, two reviewers (KG and CB) independently screened all titles and abstracts. Disagreements were resolved by consensus or, if necessary, by a third independent reviewer (EL). Inter-rater reliability was assessed using Cohen's kappa statistic. All remaining studies underwent a full-text review. Relevant data were extracted using a pre-prepared data sheet that included a title, authors, publication date, design, outcome measures, and main results.
Risk of bias
We used the Cochrane risk of bias tool (version 2) to assess randomized controlled trials and the National Heart, Lung, and Blood Institute (NHLBI) quality assessment tools for other study designs.13,Reference Sterne, Savović, Page, Page, Blencowe, Boutron, Cates, Cheng, Corbett, Eldridge, Hernán, Hopewell, Hróbjartsson, Junqueira, Jüni, Kirkham, Lasserson, Li, McAleenan, Reeves, Shepperd, Shrier, Stewart, Tilling, White, Whiting and Higgins14 Two independent reviewers (KG and CB) assessed risk of bias for all papers. Inter-rater reliability was calculated using Cohen's kappa statistic. Disagreements were resolved by consensus or, if necessary, by a third independent reviewer.
Data analysis
Included studies were summarized in tabular form, describing title, authors, study design, intervention, and primary outcomes. Study methods were reviewed to determine whether the interventions were implemented using existing ED resources (resource neutral) or whether they required additional resources.
Our intention was to perform meta-analyses and derive pooled estimates from studies of similar design and intervention type. We assessed statistical heterogeneity using the chi-squared statistic and the I-squared (I2) statistic, with I2 values of 25%, 50%, and 75% representing low, moderate, and high degrees of heterogeneity, respectively. These analyses revealed that only two studies were sufficiently similar to enable pooling. We combined and weighted these studies using the Mantel-Haenszel variance method and random effects models, and determined weighted mean differences (WMD) with a 95% confidence interval (CI) for length of stay. The remaining studies were not pooled due to high levels of methodological or statistical heterogeneity. Instead, effect sizes with corresponding 95% CIs were presented for each. Means and standard deviations (SDs) were calculated for each study outcome. For those that did not report SDs, we determined SD using reported CIs, p-values, interquartile ranges, or imputed values from other studies reporting similar outcomes in similar populations. Changes in left without being seen rates were reported as risk ratios (RR), representing a proportional increase or decrease.
RESULTS
Literature search
Of 3,284 papers identified, 211 met inclusion criteria after title/abstract screening. There were 163 disagreements between reviewers, all resolved by consensus (Cohen's kappa = 0.7). Of 211 papers that underwent a full-text review, 59 were excluded because they were not focused on throughput interventions, incorporated non-throughput interventions, or did not report key outcomes (length of stay or left without being seen). An additional 53 papers were excluded because they were published only in abstract form and lacked an adequate description of methods, results, or analysis. This left 97 papers appropriate for qualitative synthesis and two for quantitative synthesis.
Description of studies
Of the 99 studies, 52 were American, 17 were Australian, 15 were European, 8 were Canadian, 6 were Asian, and 1 was Jamaican. The studies were divided into seven categories based on intervention type. Triage interventions included triage process modifications but excluded strategies that directed patients away from the ED, as these modify input rather than throughput. Testing strategies included interventions to improve laboratory turnaround time or to introduce point-of-care testing. Alternative staffing models introduced scribes, nurses, physicians, paramedics, or nurse practitioners with innovative roles. Specific patient populations studied new approaches to specific populations (e.g., mental health assessment teams). Streaming interventions involved new care areas (e.g., fast-track) or separate care pathways for specific patient cohorts. Integrated approaches incorporated multiple-linked interventions. Interventions that did not fit the previous categories were classified as other.
Risk of bias
Of the 99 studies included, 91 were assessed using the NHLBI study quality assessment tools. Nineteen were rated good, 67 fair, and 5 poor. Eight studies were assessed using the Cochrane risk of bias tool (Version 2). Three had a low risk of bias, five had some concerns, and none had a high risk of bias. There were 15 interobserver disagreements (Cohen's k = 0.6), all resolved by consensus.
Pooled analyses
We pooled data from two studies on physician triage based on low statistical heterogeneity (<25%). One placed a supernumerary physician at triage, while the other moved a physician from ED bedside care to the triage area. Both demonstrated significant length of stay reductions compared to nurse-led triage (WMD: 11.7 minutes; 95% CI = 6.8–16.6).Reference Soremekun, Biddinger and White15,Reference Han, France, Levin, Jones, Storrow and Aronsky16
Non-pooled analyses
Due to clinical or statistical heterogeneity, the data from 92 remaining studies were not pooled. Outcomes for these studies are presented within the relevant intervention category.
Triage interventions
Six physicians in triage interventions (Table 1) reported length of stay changes between −82 minutes and +18 minutes (−20.7% to +7.2%).17–22 Five nurse practitioners or physician assistant-led triage interventions resulted in length of stay changes of −106 minutes to +19 minutes (−22% to +7.3%).23–27 Five team triage interventions reported length of stay reductions of 4 to 34 minutes (8%-16%).22,28–30 Two studies of telemedicine triage reported a 0.3- and 8-minute increases in length of stay, respectively.31, 32
Table 1. Overview of studies on interventions at triage and specific patient populations
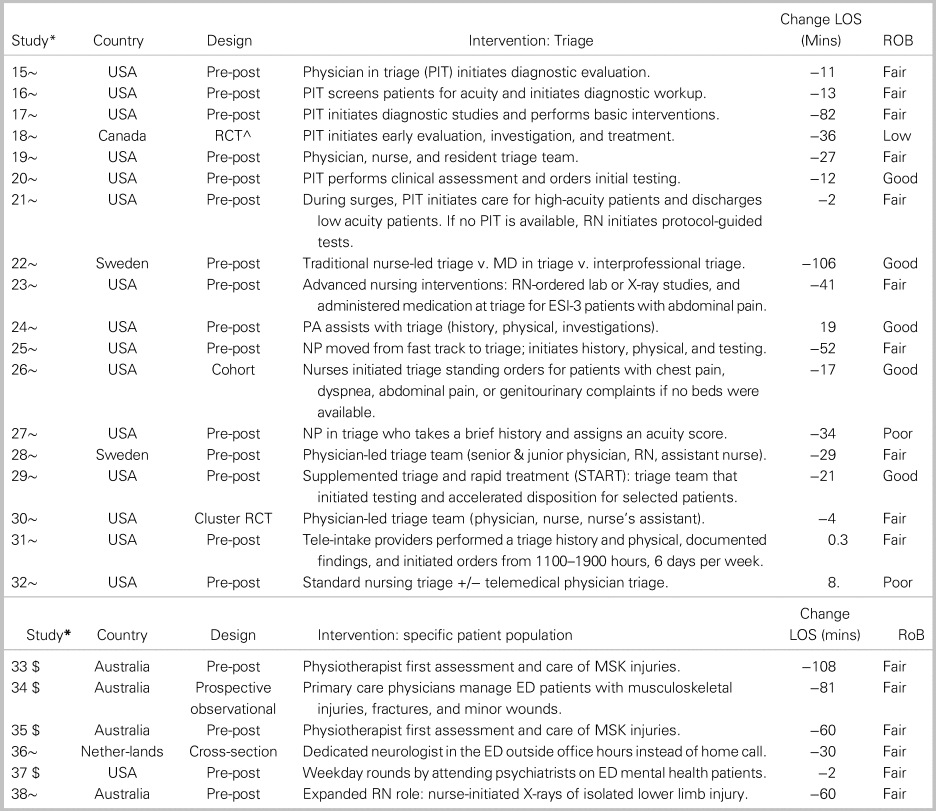
Notes: Studies are identified by reference number (see Appendix 1).
^RCTs were assessed using the Cochrane RoB-2 tool (low/some concerns/high risk of bias); “$” indicates that the intervention required additional resources; “~” indicates cost-neutral intervention; ^mixed methods study.
CPOE = computerized provider order entry; EDIS = ED information system; LOS = length of stay; MAU = medical assessment; mins = minutes; MS = musculoskeletal; PIT = physician in triage; RME = rapid medical evaluation unit; RoB = risk of bias.
Six physician at triage interventions also yielded significant left without being seen improvement (RR = 0.3 to 0.8), whereas three others reported non-significant results.17–22 One study of physician assistant-led triage reported a significant improvement (RR = 0.2), whereas one study of nurse practitioner triage and another using an undefined “triage liaison provider” reported non-significant results.24,25,27 Four team triage interventions generated left without being seen changes ranging from a meaningful improvement (RR = 0.6) to substantial deterioration (RR = 1.7).22,28–30
Specific patient populations
Five studies focused on the care of specific patient populations and reported length of stay reductions within these target populations, as opposed to the ED overall (see Table 2). Three reported 60- to 227-minute length of stay reductions after adding physiotherapists as primary providers for patients with musculoskeletal injuries.33–35 Another described a 30-minute (16%) length of stay reduction after stationing a neurologist in the ED.36 The introduction of weekday psychiatrist rounds on ED mental health patients did not significantly improve length of stay nor did an Rh testing protocol for pregnant women.37,38 Only one study measured left without being seen rates, reporting a significant improvement (RR = 0.6) associated with a dedicated neurologist in the ED.
Table 2. Overview of studies on patient streaming interventions
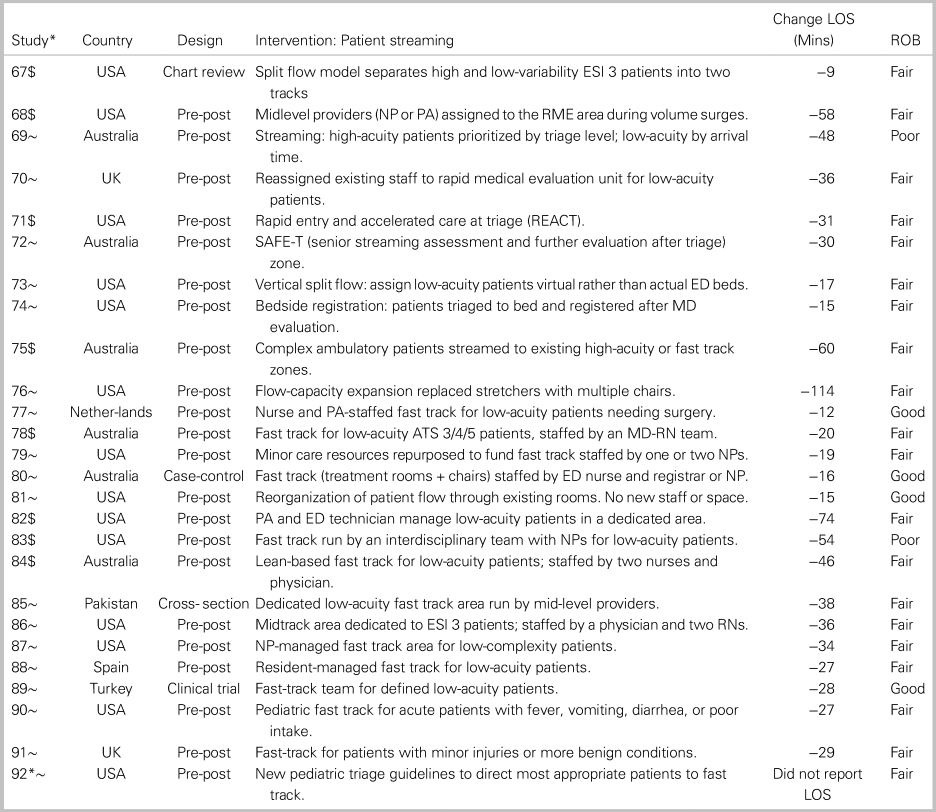
Notes: Studies are identified by reference number (see Appendix 1).
^RCTs were assessed using the Cochrane RoB-2 tool (low/some concerns/high risk of bias); “$” indicates that the intervention required additional resources; *Study 92 did not report length of stay, only left without being seen rate; “~” indicates cost-neutral intervention; ^mixed methods study.
CPOE = computerized provider order entry; EDIS = ED information system; LOS = length of stay; MAU = medical assessment; MS = musculoskeletal; PIT = physician in triage; RME = rapid medical evaluation unit; RoB = risk of bias.
Testing strategies
Twelve point-of-care testing intervention studies reported length of stay changes ranging from -114 minutes to +8 minutes (−26.8% to +3.8%), although three of these were non-significant findings (Table 3).39–50 Four studies on point-of-care testing or lab-ordering at triage reported length of stay reductions ranging from 22 to 174 minutes, but only one of these, at 29 minutes (16%), was significant.51–54 One study where triage nurses ordered X-rays using the Ottawa ankle rules reported a non-significant length of stay reduction of 28 minutes (6.4%).55,56 Length of stay changes were limited to the population of patients who underwent lab testing, and none of these studies reported effects on left without being seen.
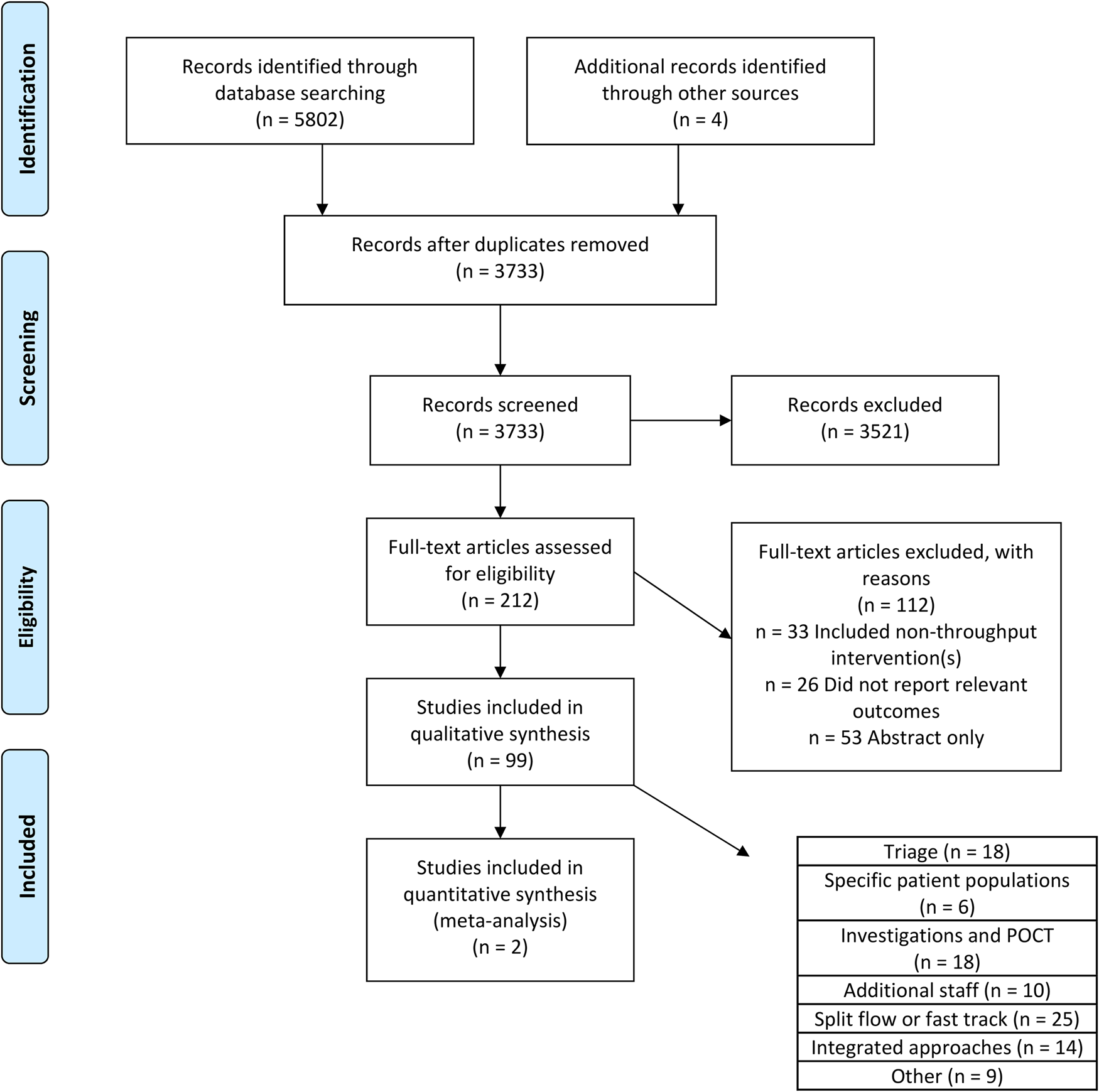
Figure 1. PRISMA flow diagram.
Table 3. Overview of studies on testing strategies and alternative staffing models
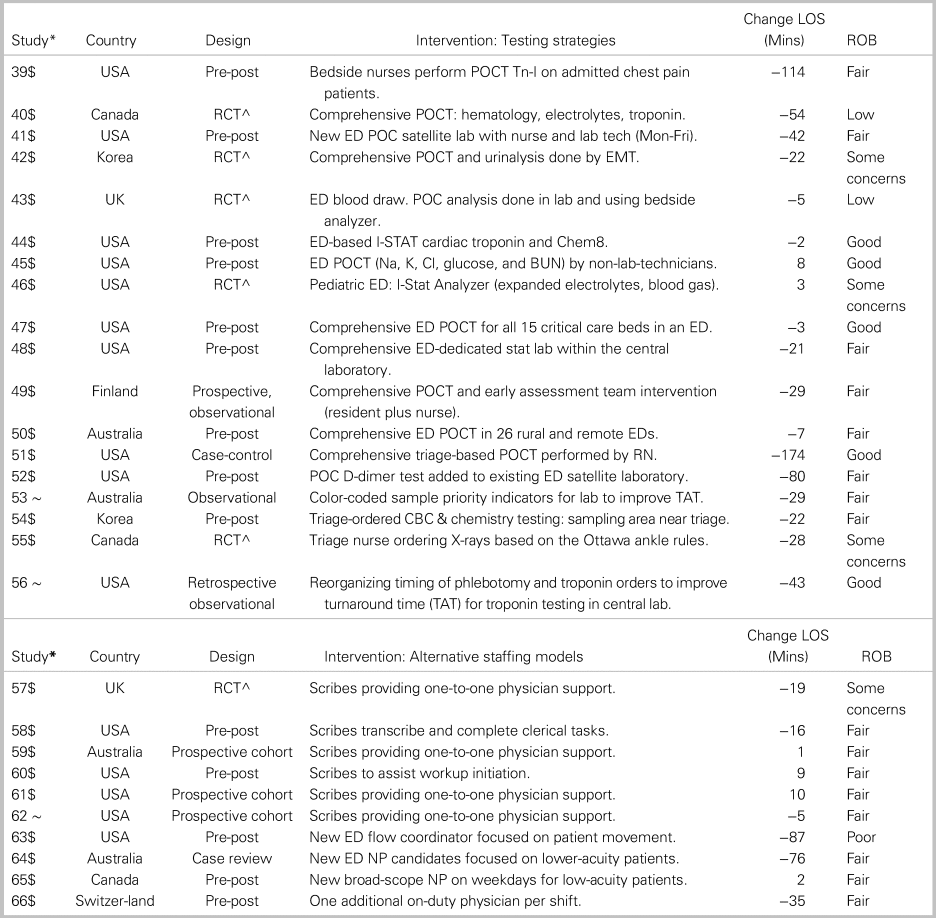
Notes: Studies are identified by reference number (see Appendix 1).
^RCTs were assessed using the Cochrane RoB-2 tool (low/some concerns/high risk of bias); “$” indicates that the intervention required additional resources; “~” indicates cost-neutral intervention; and ^mixed methods study.
LOS = length of stay; MAU = medical assessment; MS = musculoskeletal; NP = nurse practitioner; PIT = physician in triage; POCT = point-of-care testing; ROB = risk of bias.
Alternative ED staffing models
Two studies reported that ED scribes were associated with significant length of stay reductions of 16–19 minutes (5.3%−9.9%),57 but three others found non-significant increases of 1–10 minutes (Table 3).58–62 Hess et al. reported that scribes increased left without being seen rates (RR = 1.5), whereas Murphy et al. reported that the addition of a nurse flow coordinator reduced length of stay by 87 minutes (32%) and decreased left without being seen rates (RR = 0.7).60,63 Three studies added nurse practitioners or additional physician shifts, and reported length of stay changes ranging from +2 to −76 minutes.64–66
Streaming
Nine studies looked at the impact of split-flow processes that created patient streams based on acuity, presenting complaint, or ability to ambulate, and reported significant overall ED length of stay reductions from 9–60 minutes (4.0%-41.6%) (Table 2).67–75 Fast-track interventions are similar to split flow but apply specifically to mid-/low-acuity ambulatory patients who are likely to be discharged quickly after assessment. Fourteen of 15 fast-track studies showed statistically significant overall ED length of stay reductions ranging from 12–114 minutes (10%-47.5%).76–91 One split-flow study assessed left without being seen rates, finding a 43% reduction (RR = 0.6).71 Of seven fast-track studies that assessed left without being seen rates, six reported significant reductions (RR = 0.5–0.8).79,83,84,86–88, 92
Integrated approaches
Several investigators implemented multiple interventions simultaneously (Table 4). Twelve of 15 reported significant overall ED length of stay reductions ranging from 2 to 114 minutes (1%-41%).93–106 Five studies also documented left without being seen rates, with four reporting significant improvements (RR = 0.02–0.8). The most substantial improvements were seen with tailored ED process redesign, a combination of streaming, team-based assessment and early senior consultation.95–97,106
Table 4. Overview of studies on integrated approaches and other interventions
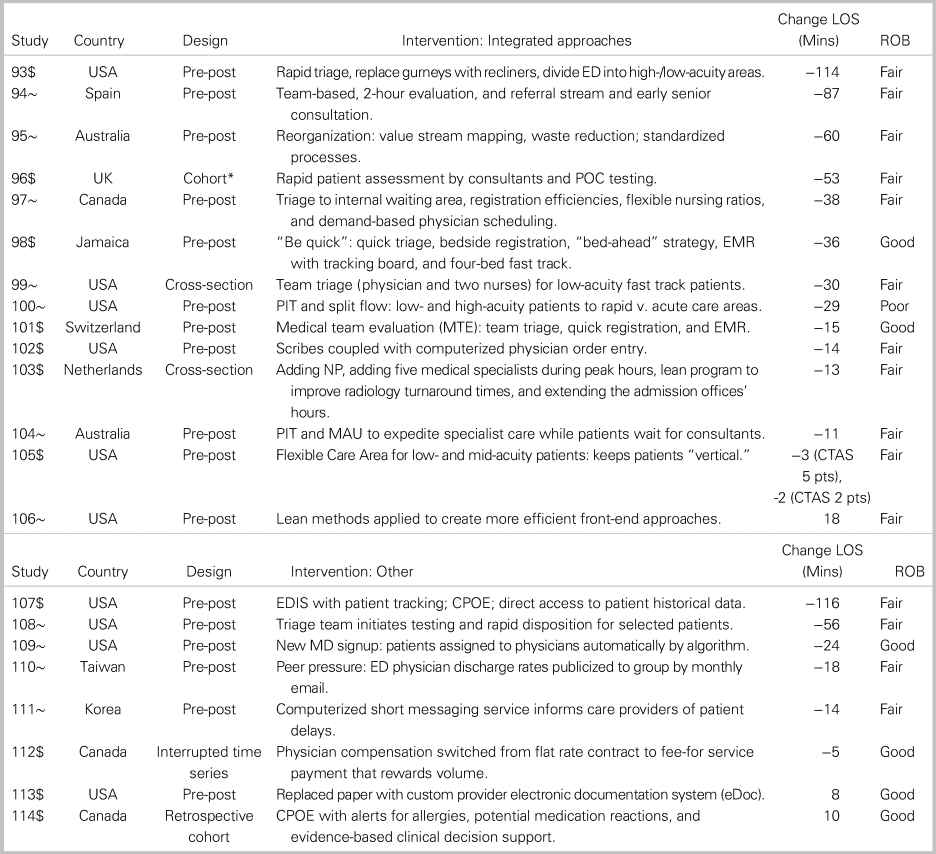
Notes: Studies are identified by reference number (see Appendix 1).
^RCTs were assessed using the Cochrane RoB-2 tool (low/some concerns/high risk of bias); “$” indicates that the intervention required additional resources; “~” indicates cost-neutral intervention; and ^mixed methods study.
CPOE = computerized provider order entry; EDIS = ED information system; LOS = length of stay; MAU = medical assessment; MS = musculoskeletal; PIT = physician in triage; pts = patients; RME = rapid medical evaluation unit; ROB = risk of bias.
Other throughput interventions
Eight interventions did not fit well within a defined category (Table 4).107–114 Five of these led to length of stay reductions, including an ED patient tracking system, a dedicated early assessment clinical team, and computerized order entry. Physician transition from contract to fee-for-service payment did not significantly reduce length of stay, nor did computerized provider order entry or electronic documentation systems. Only two studies in this category reported left without being seen outcomes. Automatically assigning patients to physicians by algorithm led to a 7% increase (RR = 1.1), whereas computerized order entry led to a 51% decrease (RR = 0.5).109,114
DISCUSSION
Interpretation
This systematic review summarizes evidence describing the effectiveness of throughput interventions. Overall, 80 of 94 studies reported modest improvements, almost irrespective of approach. A consistent modest improvement from diverse interventions, in part, could reflect publication bias. It also suggests the possibility that, in many cases, observed benefits may relate more to enhanced focus on operational improvement (Hawthorne effect) than to specific effects of the intervention.
Prior studies
Previous systematic reviews have focused on interventions in triage, patient streaming, or nurse practitioners or scribes in the ED.Reference Abdulwahid, Booth, Kuczawski and Mason115–Reference Cabilan and Boyde120 Our findings are congruent with the findings of these reviews.
Strengths and limitations
We found a paucity of high-quality evidence describing ED throughput interventions. Most studies used observational pre-post designs, which are vulnerable to bias and fail to account for confounders. High levels of heterogeneity precluded data pooling in all but two cases, making robust comparisons within and between intervention categories difficult. Only a handful of papers studied concurrent controls, and few assessed sustainability of the observed improvements. Further, while all of the studies assessed the impact of throughput interventions on length of stay or left without being seen, these outcomes are affected by other factors that were not described or incorporated in analyses. None of the studies provided meaningful cost-effectiveness analyses, and, in cases where new resources were committed or existing staff redeployed, the opportunity costs (potential benefits of alternative approaches) were not discussed. Finally, given the large number of EDs continually involved in operational improvement, the relatively small number of studies that we identified suggests that the overall positive outcomes seen in this data set, in part, could reflect publication bias.Reference Ospina, Kelly, Klassen and Rowe121
Clinical implications
The optimal intervention for a given ED and hospital system will depend on a number of factors, including the available staff and their expertise, physical space and funding, and the ED's case mix. ED leaders interested in improving throughput should evaluate the feasibility of implementing a given intervention type within their ED, and then look to the studies that reported the greatest reductions in length of stay within that intervention type for guidance. A quality improvement approach using Plan-Do-Study-Act cycles could enable an ED to relatively quickly and cost-effectively trial an intervention, and iterate upon it as needed.
Streaming and fast track were the most consistently effective intervention types, showing length of stay reductions in every case, ranging from 9 to 114 minutes. Introducing a fast track and optimizing care processes for important case-mix groups seem an obvious starting point for EDs with throughput challenges, though they do require expanding or reworking the ED space.
Earlier physician or provider assessment at triage is an effective strategy that makes use of existing resources and modestly improves ED length of stay. Several studies evaluated scribes, nurse practitioners, or other providers in non-triage roles. These changes involve additional staffing costs, and, while some appeared potentially promising, supporting evidence was of insufficient quality or quantity to warrant any strong recommendations. New diagnostic testing and point-of-care testing strategies were also associated with incremental cost, and reductions in length of stay were limited to relevant patient subsets (e.g., those requiring troponin testing), making these interventions best suited to EDs where a large number of patients have similar presentations.
If there is a unifying theme in the “integrated approaches” category, it would be optimizing process efficiency. While some interventions showed large overall length of stay reductions, they were generally more complex and costly. We advise readers to review these approaches and to prioritize other intervention types.
Research implications
Future research should apply more robust study designs, including randomized trials, stepped wedge implementations and interrupted time series analyses, and consider reporting a broader range of outcomes, including quality measures of patient satisfaction, and staff satisfaction.
CONCLUSION
Introducing a fast track and optimizing processes for important case-mix groups are likely to enhance throughput. Expediting diagnostic and treatment decisions by shifting physician-patient contact to the earliest possible process point (e.g., triage) is an effective cost-neutral strategy to improve flow. Evidence is insufficient to warrant recommendations for or against alternative staffing models. Focusing ED staff on operational improvement is likely to improve performance, regardless of the intervention type.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/cem.2020.426.
Competing interests
None declared.







