Obesity, with its increasing prevalence and associated morbidity and mortality, is a global concern(Reference James, Leach and Kalamara1). A recent study of Hong Kong children has shown increasing rates of obesity from 1993 to 2005/6(Reference So, Nelson and Li2). Various reasons contribute to this phenomenon, but unhealthy food behaviour is considered one of the most important causes(Reference Bray and Popkin3–Reference Hui and Nelson5). Breakfast, long viewed as the most important meal of the day(Reference Affenito, Thompson and Barton6–Reference Widenhorn-Muller, Hille and Klenk9), may protect against obesity. Cross-sectional studies have reported a negative association between breakfast frequency and fatness(Reference Niemeier, Raynor and Lloyd-Richardson10–Reference Merten, Williams and Shriver13), although not consistently(Reference Hui and Nelson5, Reference Affenito, Thompson and Barton6, Reference Resnicow14, Reference Abalkhail and Shawky15). A recent cross-sectional prospective study showed inverse associations between breakfast frequency and BMI at two time points that remained largely independent of all confounding and dietary factors(Reference Timlin, Pereira and Story16). However, BMI does not distinguish among increased lean mass, bone or fat, whereas the percentage of body fat (PBF) might better reflect obesity. In the present study, we used both BMI and a previously described PBF-based definition of obesity in children(Reference Sung, So and Choi17) to evaluate their relationships with self-reported breakfast frequency and food consumption behaviours in a large representative population sample of Hong Kong Chinese children aged 9–18 years.
Materials and methods
Sampling method
A two-stage cluster sampling method was used, as described previously(Reference So, Nelson and Li2, Reference Sung, So and Choi17). Data from the Department of Education were used to compile a sampling frame of all schools in Hong Kong. In the first stage, one primary school and one secondary school were selected from each of the eighteen districts in Hong Kong. In the second stage, two classes in each grade were randomly selected from the schools. All students in the selected classes were invited to join the study.
Data collection
The parents of all the participants were invited to complete a questionnaire providing demographic information. The students were asked to complete a Rapid Dietary Behaviour Assessment questionnaire. The questionnaire represented daily and weekly dietary behaviours and was validated against the 24 h recall nutrient intake data of 235 adolescents. The percentage agreement between the questions and the dietary recall ranged from 73 to 95 %. Spearman's correlation coefficient r between food intake estimated from the 24 h recall and the questionnaire was 0·63 (P = 0·004)(Reference Guldan, Wong and Chan18). Breakfast frequency was assessed by a single question, ‘How many days over the past week did you have breakfast?’ Responses ranged from 0 to 7. Physical activity was assessed by two questions: (1) Do you currently take any regular exercise training class other than school physical education class? (2) If yes, please tick the frequency of training: once, twice, equal or above 3 times/week. When answering these questions, the children were shown a detailed list of typical extramural exercise activities and classes available in Hong Kong. These two questions were designed based on the physical activity guidelines for adolescents issued from the international consensus conference in 1994(Reference Sallis and Patrick19).
Measurement of growth parameters
A team of eight trained research staff visited the selected schools on a pre-arranged date to collect the anthropometric data. All instruments were standardised before the examination, and the balances were zero calibrated. Standing height without shoes was measured twice using a Harpenden Stadiometer (Holtain Limited, Crymych, Pembs, UK), and body weight and PBF were measured using a portable Tanita body fat monitor/scale (Tanita BF-522; Tanita Corporation, Tokyo, Japan) as described previously(Reference So, Nelson and Li2, Reference Sung, So and Choi17). The bioimpedence analysis for the estimation of body fat has been validated in local Chinese children by the study team using a Tanita scale(Reference Sung, Lau and Yu20).
Statistical analysis
As it was expected that secondary school adolescents would differ from primary school students in their eating behaviours and physical activities, these age as well as sex differences were also explored. Breakfast frequency was categorised into three groups to facilitate comparisons among skippers (ate breakfast 0–2 times/week), semi-skippers (ate breakfast 3–4 times/week) and non-skippers (ate breakfast 5–7 times/week) in univariate analyses for demographic data, personal characteristics and unhealthy food consumption behaviours(Reference Hui and Nelson5). The differences among groups were assessed by χ2 tests and ANOVA for categorical variables and continuous variables respectively. The primary comparison (between two groups) was made at a significance level of 0·05. The secondary comparisons (among three groups) were made at the significance level of 0·017, using Bonferroni's correction. To further assess the relative strength of association, we used linear regression models with BMI and PBF as the dependent variables and breakfast frequency (0–7 times/week) as the independent variable. Age, sex and exercise frequency were treated as potential confounders in the models. SPSS for Windows version 14 (SPSS, Inc., Chicago, IL, USA) was used in the analysis; all P values were two sided.
Ethics
The present study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving human subjects/patients were approved by the Joint Chinese University of Hong Kong and New Territories East Cluster Clinical Research Ethics Committee and the Ethics Committee of the Department of Health of the Hong Kong Government. Parents were informed about the study by a letter distributed through the school, together with a fact sheet explaining the study purpose and procedures. Parents were informed that any report of the survey would not include any personal details of individual children, and that all information would be grouped together for analysis. They were told that all children who take part in the study would be given a record of their body measurements, and that children with high blood pressure or other abnormal findings would be given a letter to a doctor at a nearby hospital for re-assessment. Verbal consent was obtained from all subjects before data collection.
Results
A total of eighteen primary and eighteen secondary schools (15 % government, 60 % aided and 25 % private schools), one from each of the eighteen Hong Kong districts, participated in the study. This reflected the overall distribution of school types for Hong Kong(Reference So, Nelson and Li2). All children in the present study were Chinese. The sample consisted of 3644 primary grade 4–6 students (52 % boys) and 7926 secondary grade 1–7 students (49 % boys) aged 9–18 years. There was an approximately equal distribution by age and sex in each grade, except the final two secondary years had fewer students. Of the primary and secondary school students, 7 % (n 520) 10 % (n 880), respectively, did not participate in the study, mainly as a result of being absent from school, reflecting response rates of 93 and 90 %; respectively. The students' overweight and obesity status was calculated according to the International Obesity Task Force BMI reference(Reference Cole, Bellizzi and Flegal21). The rates of overweight and/or obesity were greater in boys than those in girls across the entire age range (Table 1).
Table 1 Weight status, exercise frequency and breakfast frequency by primary or secondary school group and sex
(Number of students and percentages)
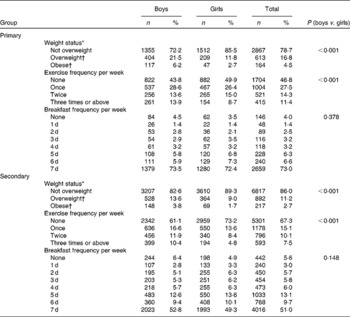
* Weight status was assessed according to the International Obesity Task Force (IOTF)(Reference Cole, Bellizzi and Flegal21).
† IOTF cut-off points for BMI for overweight and obesity by sex between 2 and 18 years, defined to pass through BMI of 25 and 30 kg/m2 at the age of 18 years.
Food consumption behaviour
The overall eating behaviours of the breakfast skippers appeared to follow a pattern that would be considered less healthy than that of the non-skippers, e.g. the skippers showed a greater consumption of instant noodles, candies or chocolates, sweetened carbonated drinks and deep-fried foods (Table 2). Girls from both primary and secondary schools reported a higher intake of candies or chocolates than did the boys. These food behaviours also showed significant associations with weight status (Table 3).
Table 2 Students following less healthy food behaviours by breakfast frequency and sex
(Number of students and percentages)

* Values were significantly different for skippers from those of non-skippers (boys, P < 0·001).
† Values were significantly different for skippers from those of non-skippers (girls, P < 0·001).
Table 3 Children's eating habits by International Obesity Task Force cut-offs
(Number of students and percentages)

* Values were significantly different between normal weight and overweight (P < 0·01).
† Values were significantly different between normal weight and obese (P < 0·01).
Breakfast frequency
The characteristics of the subjects in relation to breakfast frequency are shown in Table 4. Of the primary and secondary school students, 8 % (8·7 % of boys and 6·9 % of girls) and 14 % (14 % of boys and 15 % of girls), respectively, were breakfast skippers (ate breakfast 0–2 times/week). Breakfast skipping was more common among secondary students (P < 0·001). Based on the International Obesity Task Force criteria(Reference Cole, Bellizzi and Flegal21), the prevalence of obesity among breakfast skippers, semi-skippers and non-skippers, respectively, was 9·8, 10·6 and 3·8 % (P < 0·001) for primary school students and 3·9, 3·1 and 2·4 % (P < 0·001) for secondary school students. There was not only a larger percentage of primary children defined as being obese on the International Obesity Task Force cut-offs, but also a substantial BMI difference between primary breakfast skippers and semi-skippers compared with non-skippers. The differences in the BMI z-scores and PBF according to breakfast frequency are shown in Figs. 1 and 2. The BMI and PBF of the breakfast skippers were significantly larger than those of their non-skipping counterparts (P < 0·001). The estimated effects of breakfast frequency on BMI and PBF by sex were assessed by multiple linear regression (Table 5). The dose effects of breakfast frequency on BMI and PBF were, respectively, − 0·125 and − 0·219 for boys and − 0·165 and − 0·353 for girls per additional breakfast meal per week, i.e. the BMI and PBF of a boy who skips breakfast are higher than his non-skipping counterparts by 0·9 kg/m2 and 1·5 %, respectively, and by 1·2 kg/m2 and 2·3 %, respectively, for girls.
Table 4 Characteristics of the children according to breakfast frequency
(Mean values, standard deviations, number of students and percentages)
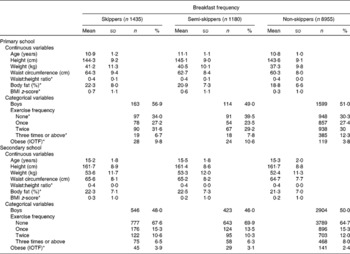
IOTF, International Obesity Task Force.
* Values were significantly different for skippers from those of non-skippers (P < 0·001).

Fig. 1 BMI z-score with breakfast frequency by sex. (a) Primary school children and (b) secondary school children.

Fig. 2 Percentage of body fat with breakfast frequency by sex. (a) Primary school children and (b) secondary school children.
Table 5 Estimated effect of breakfast and exercise frequency on body status in multivariate analysis models†
(Unstandardised coefficients and standard errors)
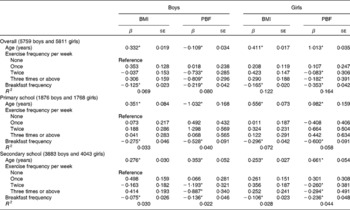
PBF, percentage of body fat; β, unstandardised coefficient.
* Values were significantly different (P < 0·05).
† Breakfast frequency ranges from 0 to 7 d.
Exercise frequency
Exercise frequency categorised into four groups (none, once, twice and three times or above a week) showed the non-skippers to be more active (Table 4). The effects of exercise frequency on BMI and PBF were assessed by multiple linear regression, and PBF was found to be inversely associated with exercise frequency among the secondary students for both boys and girls (Table 5).
Discussion
In a large representative sample of Hong Kong primary and secondary school children, we showed that breakfast eating patterns varied with age, with secondary school adolescents being more likely to skip breakfast than younger primary school-aged children. This is consistent with previous observations(Reference Barton, Eldridge and Thompson12, Reference Lytle, Seifert and Greenstein22–Reference Williams, O'Neil and Keast24). We also showed that BMI, as well as PBF, had inverse associations with breakfast frequency. This association between PBF and breakfast frequency has been reported in a New Zealand study of 5–11-year-old multi-ethnic children, which included 3 % Chinese children(Reference Duncan, Schofield and Duncan25). Breakfast eating has also been found to be negatively associated with visceral adiposity in overweight Latino youth(Reference Alexander, Ventura and Spruijt-Metz26). This negative association between BMI and PBF with breakfast frequency suggests that regular breakfast consumption could result in, or, alternatively, just reflect a healthier lifestyle. Exercise frequency was inversely associated with PBF but was not associated with BMI (Table 5). We have previously reported that both systolic and diastolic blood pressure in these children were decreased with increased exercise frequency(Reference So, Sung and Li27). This beneficial association of exercise with PBF but not with BMI could indicate that PBF better reflects adiposity and an unhealthy lifestyle than does BMI.
A recent US study suggested that regular breakfast consumption might be protective against childhood obesity(Reference Gleason and Dodd8). However, the important, yet unanswered, question is whether the inverse relationship between regular breakfast consumption and unhealthy weight and eating behaviours is causal. Although breakfast has long been considered ‘the most important meal of the day’, it is conceivable that overweight children, perhaps with the support of their parents, may consciously skip breakfast to reduce food consumption. Conversely, regular breakfast consumption could have genuine health benefits. The importance of breakfast has been addressed by a number of studies(Reference Matthys, De and Bellemans7, Reference Gleason and Dodd8, Reference Timlin, Pereira and Story16, Reference Birch and Fisher28). It has been suggested that skipping breakfast may lead to reduced satiety later in the day with resultant overeating and/or increased consumption of more energy-dense unhealthy foods(Reference Martin, Normand and Sothier29). In addition to potential nutrition benefits, regular breakfast consumption has been shown to improve students' attendance, attentiveness and achievement, and to reduce discipline problems in school(Reference Widenhorn-Muller, Hille and Klenk9, Reference Vanelli, Iovane and Bernardini30, Reference Lien31). Children who skip breakfast were less able to distinguish among similar images, showed increased errors, had slower memory recall and lower scores on cognitive tests(Reference Pollitt, Cueto and Jacoby32–Reference Chandler, Walker and Connolly35). However, a number of other studies have reported no such beneficial effects(Reference Dickie and Bender36–Reference Hoyland, Dye and Lawton38). As suggested in the present study, skipping breakfast may also be associated with poorer overall nutritional choices. A number of observational studies have shown that compared with skippers regular breakfast eaters have a higher diet quality with an increased intake of fibre, Ca, vitamins A and C, riboflavin, Zn and Fe, and a decreased intake of energy, fat and cholesterol(Reference Aranceta, Serra-Majem and Ribas39). Despite these potential benefits, breakfast is the most commonly skipped meal(Reference Williams, O'Neil and Keast24, Reference Buzzard, Faucett and Jeffery40). The provision and quality of breakfast is potentially under greater parental control than lunch, and therefore could be an important focus for improving the nutritional quality of children's diets.
The strengths of the present study include the size and representativeness of the sample(Reference So, Nelson and Li2) and high response rates. Inclusion of PBF measurements enabled the relationship of body fat to be examined with breakfast frequency. In addition, availability of a physical activity measure, an important contributor to weight status(Reference Pollitt, Leibel and Greenfield33), enables its use as a covariate in regression analysis. Limitations of the present study include its cross-sectional design. Longitudinal studies are required to better delineate the association between breakfast habits and weight status during the transition from childhood to adolescence, as well as any causal nature of this relationship. The self-reported questionnaire could have introduced biases into the study. The recall period was limited to the past week to try to minimise recall bias, but the study did not explore why or for how long had the children skipped breakfast. Breakfast frequency was defined by a single simple question and was unable to assess the quality and quantity of breakfast. Clearly, such data would be invaluable to better understand the relationships between obesity and breakfast frequency. More detailed information on what children eat for breakfast would be useful in future studies to help answer the question whether the inverse associations identified between BMI/PBF and breakfast frequency are causal. The two simple questions used to assess physical activity give only limited insight into the nature and the intensity of overall activity. The heterogeneous nature of the various activities undertaken by children made it impossible for us to characterise or quantify these activities, but the answers to these questions probably reflect an intention to participate in additional physical activity outside school. Despite the important limitation of the simplicity of the questions on breakfast frequency and exercise, it is also possible that such questions could have utility from a public health perspective if they can be further validated to reflect general behaviours.
Conclusion
Using a simple screening question of the frequency of eating breakfast during the past week, we showed that eating breakfast 2 times/week or less was associated with higher BMI, BMI z-scores and PBF in a large population sample of children aged 9–18 years. Breakfast eating may simply be a marker for other behaviours and social/environmental factors associated with overweight and obesity. Alternatively, this association may be causal. Further evaluation is needed to determine whether the successful promotion of a regular healthy breakfast habit could have a beneficial role in combating the obesity epidemic.
Consent
Parents were asked to inform the school if they did not wish their child to participate in the study, and verbal consent was obtained from the children.
Acknowledgements
We thank the school principals, teachers, parents and students who participated in the study. The present study received financial support from the Departmental funds and the Hong Kong Paediatric Society. There are no conflicts of interest. The authors' contributions were as follows: H. K. S. coordinated the study, assisted in the supervision of data collection and drafted the manuscript; E. A. S. N., R. Y. T. S. and A. M. L. prepared the proposal and supervised the study; J. Y. undertook the recruitment and clinical assessments; G. S. G. and P. C. N. made substantial contributions to the conception of the study and revised the manuscript. All the authors contributed to the submitted form of the manuscript, and read and approved the final manuscript.









