Every year, over 700 000 individuals tragically lose their lives to suicide, representing a global age-standardised suicide rate of 10.5 per 100 000 people in 2016.1 In 2020, Australia had a suicide death rate of 12.1 per 100 000 people, along with a self-harm hospital admission rate of 113 per 100 000 people.2 Current estimates of hospital-treated self-harm based on institutional administrative data are likely to underestimate the overall burden of self-harm in the population. This is because many instances of self-harm do not lead to hospital admission. It is important to note that prior self-harm represents the most significant risk factor for future self-harm or suicide.Reference Olfson, Wall, Wang, Crystal, Gerhard and Blanco3,Reference Hawton, Bergen, Cooper, Turnbull, Waters and Ness4 For example, Olfson et alReference Olfson, Wall, Wang, Crystal, Gerhard and Blanco3 found that the rate of repeated self-harm during the 12 months after non-fatal self-harm was 37 times higher than in the matched general population. Furthermore, self-harm has a significant impact on health outcomes and productivity loss.Reference Kinchin, Doran, Hall and Meurk5,Reference Kinchin and Doran6 Nguyen et alReference Braaf and Gabbe7 found that only one-third of people who had self-harmed and were discharged from hospital achieved ‘good recovery’ (as measured by the Glasgow Outcome Scale Extended) and, importantly, only half returned to work within 24 months of their self-harm. For these reasons, it is important to provide effective and cost-effective care for those who self-harm.
The body of evidence supporting the effectiveness of aftercare interventions aimed at preventing recurring self-harm episodes is steadily growing. Aftercare interventions are defined as interventions providing care for someone after they have had a self-harm episode. Research has demonstrated that psychological or psychosocial aftercare interventions are linked to a reduced risk of subsequent self-harm.Reference Hetrick, Robinson, Spittal and Carter8 However, it is worth noting that these interventions can be resource-intensive, as they often require specialised clinician training, which may not always be feasible to implement.Reference Pitman and Tyrer9 Furthermore, those who self-harm have demonstrated low adherence to intensive psychological and psychosocial interventions.Reference Lizardi and Stanley10,Reference Joubert, Petrakis and Cementon11 In view of this, brief aftercare interventions that focus on preventing recurrent self-harm and involve direct ongoing contact, along with the option for re-contact with clinical services if needed, may serve as a crucial and viable alternative.Reference Milner, Carter, Pirkis, Robinson and Spittal12 There are several forms of brief aftercare interventions, including supportive phone calls (i.e. telephone outreach), with or without care coordination, as well as follow-up services provided after the patient has been discharged from the acute care unit or emergency department.Reference Doupnik, Rudd, Schmutte, Worsley, Bowden and McCarthy13 A recent meta-analysis indicated a noteworthy decrease in the occurrence of subsequent self-harm episodes per individual when employing brief aftercare interventions that incorporated at least one of four main components: brief contact interventions, care coordination, safety planning interventions and/or other brief therapies. This reduction was observed when comparing these interventions with control groups that did not receive any intervention (odds ratio (OR): 0.69; 95% CI: 0.53 to 0.89).Reference Doupnik, Rudd, Schmutte, Worsley, Bowden and McCarthy13
There is a relative paucity of economic evaluations of brief aftercare interventions designed to prevent or reduce subsequent self-harm episodes, although there have been some economic studies of brief aftercare interventions (i.e. interventions with one or two of the components identified by Doupnik et alReference Doupnik, Rudd, Schmutte, Worsley, Bowden and McCarthy13). In particular, a pre–post study conducted in the USA found that for every US$1 invested in delivering follow-up calls after discharge to individuals who had been admitted to hospital or presented to an emergency department following self-harm, the estimated return on investment (ROI) ranged from US$1.7 to US$2.43, depending on whether individuals had commercial insurance or were covered by Medicaid.Reference Richardson, Mark and McKeon14 A recent model-based economic evaluation indicated that telephone outreach was more costly but more effective than usual care (i.e. defined as only one-third of people receiving an average of one initial diagnostic evaluation plus two 45-min psychotherapy sessions during the 12 weeks post-discharge), with an incremental cost-effectiveness ratio (ICER) of US$4300 per life year under a health sector perspective.Reference Denchev, Pearson, Allen, Claassen, Currier and Zatzick15 The combination of universal screening in the emergency department and a telephone-based intervention provided over a period of 12 months after the emergency department visit was deemed cost-effective, with an ICER of US$5020 per additional attempt or death prevented.Reference Dunlap, Orme, Zarkin, Arias, Miller and Camargo16 It is noteworthy that in the existing economic evidence, the effectiveness of brief aftercare interventions was estimated from a single study rather than a meta-analysis of individual studies; moreover, the single study was conducted in a USA context, and so its findings may not be applicable to other settings.
The current study is the first to evaluate the cost-effectiveness of a theoretical brief aftercare intervention that included all of the components identified by Doupnik et alReference Doupnik, Rudd, Schmutte, Worsley, Bowden and McCarthy13 (i.e. brief contact interventions, safety planning interventions, care coordination and/or other brief therapies) within the Australian context. We used different economic frameworks (ROI and cost–utility analysis; CUA) in our study and examined whether the brief aftercare intervention delivered to those who had been admitted to a hospital unit or presented to an emergency department for self-harm provides value for money.
Method
The current study involved an economic evaluation of a theoretical brief aftercare intervention over a period of 10 years. The study followed the guidelines and checklist provided by the Consolidated Health Economic Evaluation Reporting Standards to ensure comprehensive and standardised reporting of the health economic evaluation, as outlined in Supplementary Appendix 1 available at https://doi.org/10.1192/bjo.2023.525. The approach to modelling intervention effectiveness was based on a prior model developed to evaluate the cost-effectiveness of four suicide prevention strategies that formed part of the ACE Prevention study.Reference Mihalopoulos, Carter, Pirkis and Vos17 The effectiveness of a theoretical brief aftercare intervention was based on an effect size derived from a recent meta-analysis by Doupnik et al,Reference Doupnik, Rudd, Schmutte, Worsley, Bowden and McCarthy13 whereas the direct intervention cost was based on estimates from the Australian brief aftercare programme for prevention of repeated self-harm.Reference McGill, Whyte, Sawyer, Adams, Delamothe and Lewin18 In this study, a partial societal perspective was used to assess both the costs and health benefits. That meant that healthcare costs related to hospital admissions due to self-harm and the healthcare cost offsets and cost of productivity loss related to suicides were included in the base case analysis. The analysis did not consider time or travel costs incurred by people who had self-harmed and received brief aftercare intervention or by their carers and/or family members.
This study used two different economic evaluation frameworks: (a) an ROI analysis, which compared the cost-savings generated by the intervention with the total cost of implementing the intervention; and (b) a CUA, which compared the net costs of the intervention to the net health outcomes measured in quality-adjusted life years (QALYs). The results of the study are presented in the form of ROI ratios (cost-saving divided by intervention cost) and ICERs, representing the cost per QALY gained. The ICERs were evaluated using the commonly accepted willingness-to-pay threshold of $50 000 per QALY. The study used a 10-year time horizon and adjusted all costs to 2018 Australian dollars (AUD) using the most recent relevant health price deflators. Both costs and health benefits were discounted at a rate of 3% per annum.
Intervention description
As identified in the meta-analysis by Doupnik et al,Reference Doupnik, Rudd, Schmutte, Worsley, Bowden and McCarthy13 various components can be included in brief aftercare interventions. For the purpose of costing a pathway of a theoretical brief aftercare intervention in the Australian context, we chose an implemented intervention, the Way Back Support Service, which includes four components of a brief aftercare intervention.19 The Way Back was a non-clinical service for people aged 15 or over who presented to the emergency department or required hospital admission following self-harm and had the aim of connecting them to care.19,Reference Carter, McGill, Sawyer, Adams, Delamothe and Whyte20 The Way Back included (a) follow-up telephone contacts, (b) care coordination, (c) safety planning and (d) brief therapeutic intervention. A support coordinator initiated contact with the person after receiving their referral from the hospital to explain the scope and role of the support offered by the Way Back. An initial assessment appointment was organised post-discharge to identify the goals and needs of the consumers, to develop a safety plan and assist people to stay connected to informal and formal supports tailored to their individual needs and preferences.19 In this economic evaluation, the intervention was modelled for the entire population of people with self-harm in Australia, with the assumption that they would all have access to the Way Back.
Intervention effectiveness
We based our estimates of the effectiveness of the intervention on the recent meta-analysis of brief aftercare contact interventions by Doupnik et al,Reference Doupnik, Rudd, Schmutte, Worsley, Bowden and McCarthy13 in which a pooled effect size was calculated based on seven randomised controlled trials of brief aftercare suicide prevention interventions. The pooled estimate indicated significantly lower odds of subsequent self-harm reattempts (pooled OR: 0.69; 95% CI: 0.55 to 0.87) following an intervention compared with no intervention. There was no evidence pertaining to whether this reduction was maintained over time after the first year. Therefore, in the base case analysis, our model assumed a 50% decay effect regarding intervention effectiveness over the first 5 years and no effect of the intervention after that. Similar assumptions have been made in previous Australian economic evaluations of preventive interventions for mental disorders and suicide. We also conducted a sensitivity analysis, which assumed conservatively that the intervention had an effect only up to 12 months (and a 100% decay effect thereafter). Furthermore, it is noteworthy that the effectiveness of the Way Back used for intervention costing was not captured in this meta-analysis,Reference Doupnik, Rudd, Schmutte, Worsley, Bowden and McCarthy13 given that it had been recently published and did not meet the study design criteria to be included in the meta-analysis (i.e. it was a historical control study rather than a randomised controlled trial).Reference McGill, Whyte, Sawyer, Adams, Delamothe and Lewin18
Comparator (or no investment scenarios)
A ‘do nothing’ comparator or no intervention was chosen because it is not clear what constitutes standard or routine practice for people presenting with self-harm in the Australian context. This also meant that people could receive treatment as usual regardless of whether they received the brief aftercare intervention. The cost of a comparator, thus, was not included in the analysis.
Eligible population
The eligible population for the modelling was all individuals aged 15 years or older who presented to hospital following an episode of self-harm (similar to the eligibility criteria for the Way Back).19 According to a process and impact evaluation of the Way Back, of 1,120 participants initially identified, 821 people (approximately 73.3%) were eligible to receive the service. Therefore, approximately 73.3% were assumed to have taken up Way Back services in this study.Reference Carter, McGill, Sawyer, Adams, Delamothe and Whyte20
Health benefit modelling
We adopted a simple population-level Markov model developed by Mihalopoulos et alReference Mihalopoulos, Vos, Pirkis and Carter21 which simulated the transitions of each age–sex cohort among three different health states – no self-harm, self-harm and deceased (by suicide or other causes) – over a period of 10 years. The selection of a 10-year time horizon was based on previous evidence showing that it provides an adequate duration to evaluate the beneficial impacts of preventive interventions.Reference Le, Esturas, Mihalopoulos, Chiotelis, Bucholc and Chatterton22 People who engage in self-harm and are admitted to hospital enter the model and either take up or do not take up the brief aftercare intervention. At the end of the cycle, everyone enters the Markov phase of the model where they: (a) do not repeat self-harming behaviour; (b) repeat self-harming behaviour (with a non-fatal outcome); (c) die by suicide; or (d) die from other causes. The state transition diagram is presented in Fig. 1. The number of people who had a self-harm episode was determined from the rates of self-harm hospital admissions in Australia.2 The probability of fatal and non-fatal repeated self-harm each year following the index self-harm episode was estimated from the most recently published relevant international review of cohort studies and randomised controlled trials.Reference Carroll, Metcalfe and Gunnell23 Reduced probability of self-harm was included in the model by applying the odd ratios (converted to a probability) from Carroll et alReference Carroll, Metcalfe and Gunnell23 to the naturalistic estimates of self-harm described by Carrol et al.Reference Carroll, Metcalfe and Gunnell23 The model quantified the impact on health of a lower probability of repeated self-harm and subsequent suicide in the intervention scenario versus no intervention.
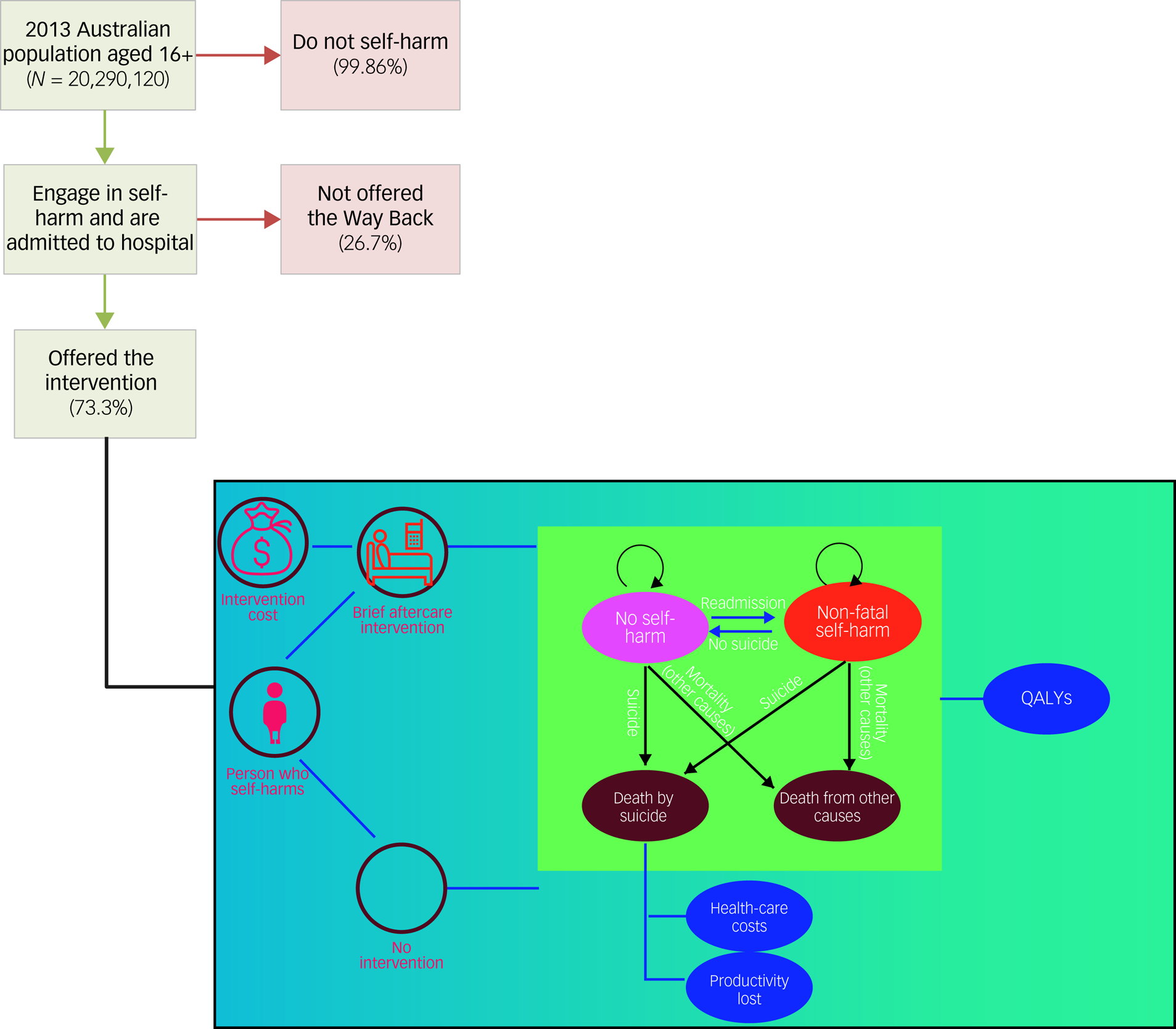
Fig. 1 The Way Back Service pathway and schematic model. QALYs, quality-adjusted life years.
Cost-effectiveness frameworks
The ROI framework was chosen for the primary analysis comparing the cost-savings produced by the intervention relative to costs of the intervention. This ratio is technically a benefit/cost ratio, which has been used in previous ROI studies in AustraliaReference Mihalopoulos, Le, Engel, Lal, Lee and Bucholc24 and in the UK.Reference McDaid, Park, Knapp, Wilson, Rosen and Beecham25 Interventions with ROI ratios greater than one are considered cost-saving, indicating that the cost-savings outweigh the total cost of the intervention. A CUA was adopted for the secondary analysis, in which QALYs were used as a metric to measure health gains. QALYs combine both the quantity gains from reduced mortality and the quality gains from improvements in health-related quality of life. Utility weights were employed to adjust each year lived in a specific health state on a scale ranging from 0 (representing death) to 1 (indicating perfect health). The utility weights of health states for those who do not engage in self-harm or engage in self-harm that is not fatal were estimated to be 0.64 (95% CI: 0.33 to 0.95) and 0.54 (95% CI: 0.29 to 0.79), respectively, as sourced from a population study.Reference van Spijker, van Straten, Kerkhof, Hoeymans and Smit26 Among those who do not engage in self-harm, the utility weights of some individuals’ health states may be low (i.e. 0.64), indicating the impact of previous experience of self-harm. Given the overlap in 95% confidence intervals of utility scores between these health states, in the probabilistic analysis, the utility score of the self-harm health state was constrained to the utility score of the non-fatal self-harm health state plus the difference in utility scores between these health states (i.e. 0.1). The cost-effectiveness results were presented in the form of an ICER, which was calculated by dividing the difference in costs between the intervention and no intervention by the difference in QALYs gained. Table 1 provides a comprehensive overview of all input parameters and their corresponding uncertainty ranges related to health benefits in this study.
Table 1 Input parameters and uncertainty ranges for health benefit and costing
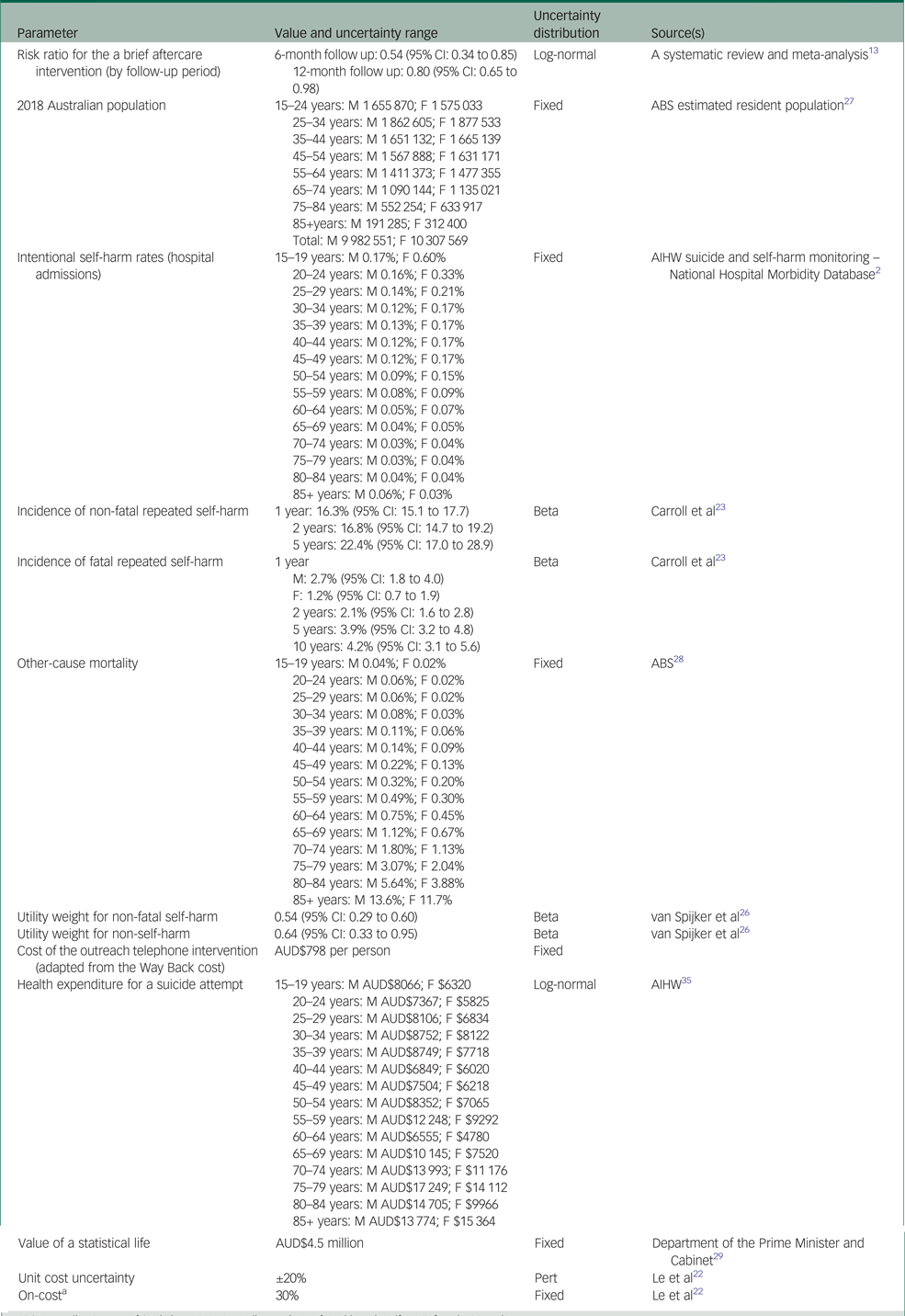
ABS, Australian Bureau of Statistics; AIHW, Australian Institute of Health and Welfare; F, female; M, male.
a. Wage rates were adjusted to incorporate 30% on-costs, i.e. additional loadings to account for administration costs, leave, superannuation, etc.
Intervention costs
As mentioned above, the Way Back was chosen as an example for costing a theoretical brief aftercare intervention in Australia. This study assumed a steady-state scenario where the intervention operates with the presence of trained staff and the required infrastructure to deliver it effectively. Therefore, operating, and overhead costs were excluded from the analysis, although training costs during the intervention were included. The Way Back cost was assumed to be equivalent to the cost of the Way Back as implemented in the Hunter New England Mental Health Service and Hunter Primary Care in Newcastle, New South Wales, Australia. This specific site was chosen because it is the only site where a costing of the Way Back in practice has been conducted.Reference McGill, Whyte, Sawyer, Adams, Delamothe and Lewin18 In this costing analysis, costs of the Way Back were calculated by summing the costs for (a) staff who delivered the intervention, (b) staff training and professional development, and (c) staff travel. The total cost of the Way Back was estimated at AUD$615 per person. As the unit cost of the intervention may vary depending on the geographic area or specific context, we applied ±20% uncertainty around this unit cost.
Cost-savings
Cost-savings included healthcare cost-savings related to averting further episodes of non-fatal self-harm and costs related to suicides. In this study, the former cost-saving was sourced from Australian Institute of Health and Welfare (AIHW) health expenditure data2 and the costs attributable to category U01 ‘Suicide and self-inflicted injuries’. To estimate the financial value society assigns to the reduction of death risk, one approach is to use the concept of the value of a statistical life (VSL). However, measures of QALYs and VSL may be at risk of double counting.Reference Ananthapavan, Moodie, Milat and Carter30 We therefore used a weighted average of healthcare and productivity costs associated with a suicide death sourced from KPMG (2013)31 for estimating the cost-savings associated with suicide deaths in the base case analysis, and we used the VSL in the sensitivity analysis. The weighted average cost of a suicide reported by KPMG was AUD$714 681, estimated by summing (a) the direct costs of suicide relating to coronial injuries, police and ambulance services, and counselling support to family/friends of the person who had died, and (b) the indirect costs of suicide including the lost economic contribution of an individual owing to premature mortality.31
Uncertainty and sensitivity analyses
To account for parameter uncertainty (i.e. sampling error) and its impact on the model outputs, uncertainty analyses were performed alongside each cost-effectiveness model. A Monte Carlo simulation consisting of 3000 iterations was conducted in Excel for each uncertainty analysis. This allowed the estimation of incremental costs, QALYs, ICERs and ROI ratios, along with their corresponding 95% uncertainty intervals. The uncertainty iterations were visually represented on a cost-effectiveness plane to provide a comprehensive understanding of the results. Detailed information regarding the uncertainty parameters can be found in Table 1.
To assess the robustness of the findings, sensitivity analyses were conducted, considering the impact of varying model parameters and assumptions. Five alternative scenarios were explored within these sensitivity analyses, allowing a comprehensive evaluation of the potential influence on the results.
Sensitivity analysis 1: modelling short-term intervention effectiveness only, such that the intervention was not effective after the first year (i.e. assuming a 100% decay rate after 1 year, instead of a 50% annual decay rate as in the base case analysis).
Sensitivity analysis 2: the cost associated with a death was based on the VSL at AUD$4.5 million measured in 2018 dollars recommended by the Department of the Prime Minister and Cabinet of the Australian Government (2014).29 This estimation was derived from the assumption that an individual in good health would have an average life expectancy of another 40 years.
Sensitivity analysis 3: regarding the CUA, we examined the higher utility scores (0.90, equivalent to population normsReference Hawthorne, Korn and Richardson32 v. 0.64) for those who had not self-harmed.
Sensitivity analysis 4: reducing the intervention costs by 20%.
Sensitivity analysis 5: increasing the intervention costs by 20%.
We also conducted two threshold analyses to vary the effect size until the intervention was not cost-saving (ICER = 0) or not cost-effective under the common value-for-money threshold of $50,000 per QALY (ICER = $50 000 per QALY). These threshold analyses were conducted with the assumption of a 50% decay effect regarding intervention effectiveness over the first 5 years.
Results
Cost-effectiveness
Table 2 presents results for the base case analysis. The total cost of implementing the Way Back services at a national level was AUD$12.9M (95% uncertainty interval: 11.1M to 14.7M). The modelled intervention subsequently produced AUD$20.4M (95% uncertainty interval: −68.7M to 2.2M) in cost-saving owing to reductions in healthcare costs associated with non-fatal self-harm (AUD$9.9M) and monetary value related to suicide death (AUD$10.5M). The ROI ratio for the intervention was determined to be 1.58 (95% uncertainty interval: −0.17 to 5.33). This meant that for every AUD$1 invested, there would be an estimated return of AUD$1.58. When analysing health outcomes, we found that the theoretical brief aftercare intervention resulted in 222 QALYs gained (95% uncertainty interval: −45 to 563). The mean ICER of the modelled intervention, compared with no intervention, was found to be dominant, with a 95% uncertainty interval ranging from dominant to AUD$189 851 per QALY gained. This indicates that the intervention not only generated positive health benefits but also resulted in net cost-savings.
Table 2 Cost-effectiveness summary for the Way Back delivered following self-harm (base case analysis, 50% decay effect up to 5 years)
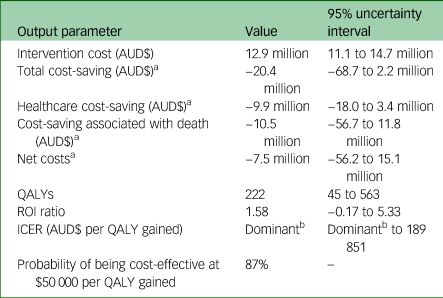
AUD$, Australian dollars; ICER, incremental cost-effectiveness ratio; QALY, quality-adjusted life year; ROI, return on investment.
a. Negative costs denote cost-savings (if positive costs which denote an expense).
b. A dominant ICER signifies that the intervention is both cost-saving and produces greater health impacts when compared to the comparator.
Uncertainty and sensitivity analysis
As shown in Fig. 2, the likelihood of the theoretical brief aftercare intervention being cost-effective at a willingness-to-pay threshold of $50 000 per QALY was 87.0%. Table 3 presents the results of the sensitivity analyses. Overall, the results were robust to changes made across each of the five sensitivity analyses, with ROIs ranging from 1.06 to 6.99. Using the VSL to estimate monetary value on death had the largest impact on the ROI, resulting in a more than fourfold increase in the ROI from 1.58 to 6.99.
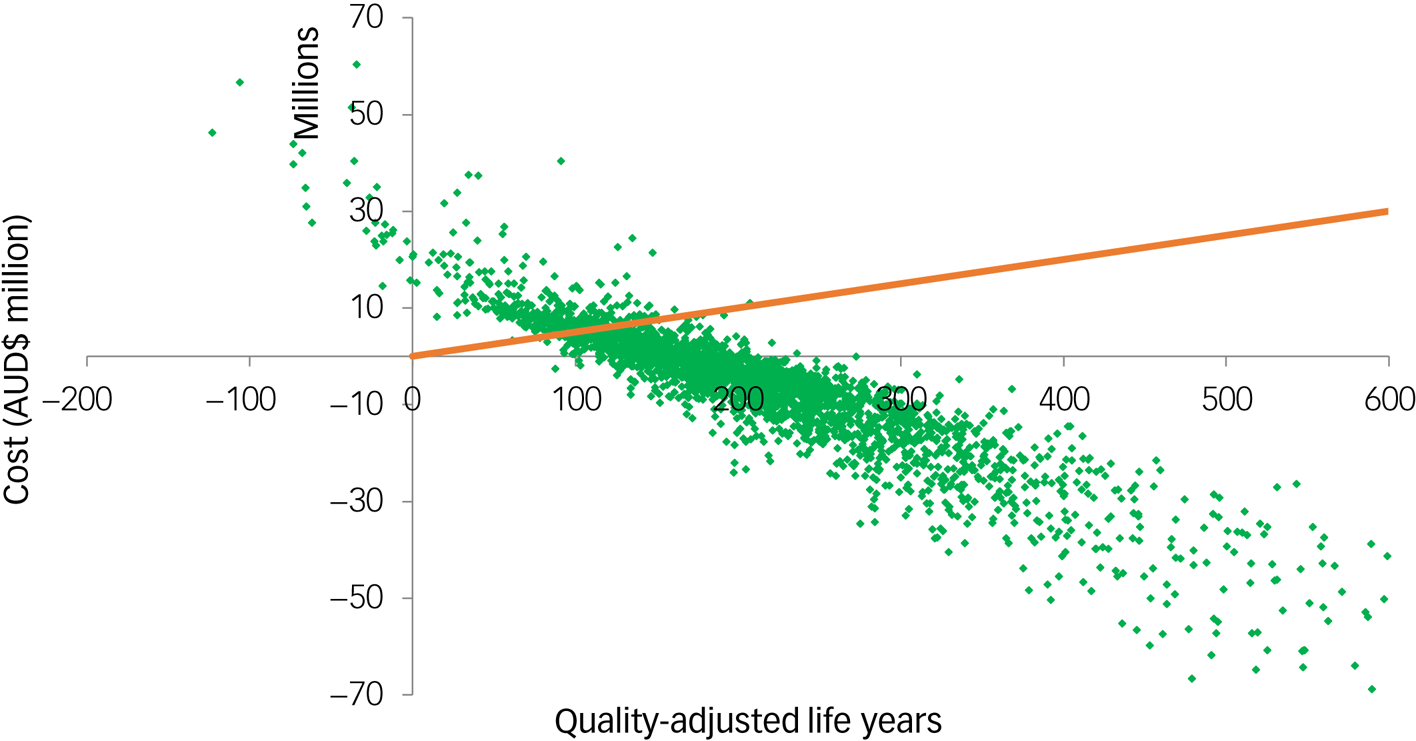
Fig. 2 Cost-effectiveness plane of the brief aftercare intervention for suicide prevention: cost–utility analysis.
Table 3 Scenario analysis results
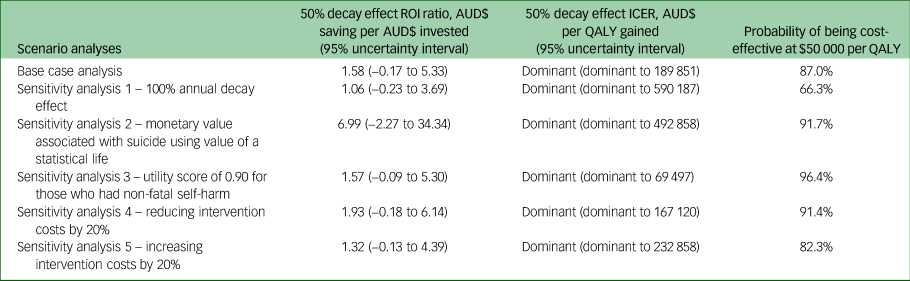
AUD$, Australian dollars; ICER, incremental cost-effectiveness ratio; QALY, quality-adjusted life year.
Threshold analysis indicated that the intervention was no longer cost-saving if it prevented only 20% of people with suicide reattempts (effect size 0.80) at the first year or not cost-effective if it prevented 12% of people with suicide reattempts (effect size 0.88) at the first year and 50% decay of effectiveness within the first 5 years.
Discussion
The findings of the current study indicate that a theoretical brief aftercare intervention (based on the costs associated with the Way Back Service and the effect size from a meta-analysis of studies not including the Way Back) was likely to be cost-effective within the Australian context, irrespective of whether a ROI analysis or CUA was used. This is the first study to use different economic evaluation frameworks to analyse whether brief aftercare interventions provide good value for money compared with no intervention. The results of this study demonstrated a considerable level of robustness to variations in input parameters and assumptions during the sensitivity analyses. It is worth noting that the monetary value associated with suicide was the parameter with the greatest impact on the cost-effectiveness outcomes. Although there was a high likelihood that the intervention would be considered cost-effective compared with a willingness-to-pay threshold of $50 000 per QALY gained, with two-thirds of uncertainty iterations falling below this threshold, it is important to note that the wide uncertainty intervals around the ICER indicate some probability that the intervention may not be cost-effective when compared to no intervention. Furthermore, threshold analysis indicated that if effect size was reduced by approximately 28%, the intervention would be no longer cost-effective.
The findings of the current model-based evaluation were relatively consistent with previous economic evaluations which support telephone outreach services as a cost-effective intervention for preventing repeated self-harm.Reference Richardson, Mark and McKeon14,Reference Denchev, Pearson, Allen, Claassen, Currier and Zatzick15 Our ROI ratio was slightly lower than that reported in the US study conducted by Richardson et al.Reference Richardson, Mark and McKeon14 This might have been because our study included services that involve additional intervention components compared with the telephone outreach interventions that were economically evaluated.Reference Richardson, Mark and McKeon14,Reference Denchev, Pearson, Allen, Claassen, Currier and Zatzick15 The Way Back intervention not only included telephone follow-up but also care coordination to assist consumers to stay connected to informal and formal supports. Furthermore, the current study also included training costs associated with the brief aftercare intervention of interest; these were not included in previous economic evaluations. Research to explore the best effective and cost-effective aftercare models for suicide prevention should be performed to support the best funding allocation.
Study strengths and limitations
The study possesses several notable strengths. First, it employed reasonable and well-founded assumptions based on the most up-to-date literature to construct the economic model, effectively capturing both the benefits and costs associated with the intervention. In addition, the inclusion of two distinct economic evaluation frameworks within a single study context enhanced the robustness of the study's conclusions. The use of both uncertainty analysis and sensitivity analysis in the simulation model further contributed to the study's reliability by enabling us to identify the variables that exerted the greatest influence on the findings.
However, some caution should be exercised in interpreting the results of the study. The evidence of effectiveness of brief aftercare interventions (including telephone contacts, emergency or crisis cards, and postcard or letter contacts) that we used as inputs to the model mostly came from underpowered trials with small sample sizes.Reference Milner, Carter, Pirkis, Robinson and Spittal12 In the meta-analysis by Doupnik et al,Reference Doupnik, Rudd, Schmutte, Worsley, Bowden and McCarthy13 the pooled result for brief aftercare interventions was heavily influenced by one large studyReference Miller, Camargo, Arias, Sullivan, Allen and Goldstein33 that accounted for a large proportion of the study participants. Nevertheless, even when this study was excluded from the pooled-effects estimate, the combined effect of the interventions consistently indicated a reduction in subsequent suicide attempts.Reference Doupnik, Rudd, Schmutte, Worsley, Bowden and McCarthy13 In addition, the evidence for effectiveness was limited to studies with time horizons of only 1 year. A historical controlled study found that no significant differences were observed between the Way Back intervention and the control group in terms of the proportion of individuals with any readmissions for suicide re-attempts or the number of readmissions during the follow-up period.Reference McGill, Whyte, Sawyer, Adams, Delamothe and Lewin18 Further research on the implementation, acceptability, feasibility and sustainability of brief aftercare interventions is therefore needed so that local, more specific estimates of their short-term and long-term effectiveness can be generated. Furthermore, research to explore which of various different aftercare models are the most effective and cost-effective for suicide prevention should be carried out to support the best funding allocation.
Several limitations may affect the validity of our study's findings. First, the lack of studies with follow-up periods of more than 1 year made it difficult to be certain about the long-term effectiveness of the intervention. Second, the intervention cost was based on the data provided by the Hunter New England Mental Health Services, where only self-poisoning patients were included. This may limit the generalisability of our findings to different healthcare settings, particularly with respect to costs, especially in low- and middle-income countries. Third, the study used a partial societal perspective, which meant that some benefits associated with self-harm prevention were not captured (e.g. impact on carers and family members) (O'Dea & TuckerReference O'Dea and Tucker34). This means that the benefit of the intervention may have been underestimated. However, including these costs would make the intervention more favourable with higher ROI.
Clinical implications
A modelled brief aftercare intervention is likely to be a cost-effective intervention for repeated self-harm prevention for those who have had an index self-harm episode according to both ROI analysis and CUA. Our results indicate that for each AUD$1 invested in 2018, there would be an associated return of AUD$1.58. These findings highlight the potential cost-effectiveness of the intervention. However, further research is necessary to explore the implementation of this intervention in practice and gather more evidence on its effectiveness and long-term outcomes.
Supplementary material
Supplementary material is available online at https://doi.org/10.1192/bjo.2023.525.
Data availability
All relevant data are provided in the paper and the supplementary material.
Author contributions
Conceptualisation: L.K.-D.L., A.F., J.P., C.M. and L.R. Data curation: L.K.-D.L., A.F., K.K., K.A., P.B., A.P., M.S., G.C. and L.R. Formal analysis: L.K.-D.L., A.F. and L.R. Funding acquisition: C.M., L.R. and J.P. Methodology: L.K.-D.L., A.F., L.R., J.P. and C.M. Project administration: L.K.-D.L. and L.R. Supervision: J.P. and C.M. Validation: L.K.-D.L., A.F., K.K., K.A., P.B., A.P., M.S., J.P., C.M., G.C. and L.R. Visualisation: L.K.-D.L. Writing – original draft: L.K.-D.L., A.F., L.R. Writing – review and editing: L.K.-D.L., A.F., K.K., K.A., P.B., A.P., M.S., J.P., C.M., G.C. and L.R.
Funding
This work was funded through the Australian Government National Suicide Prevention Leadership and Support Programme. J.P. is supported by a National Health and Medical Research Council (NHMRC) Investigator Grant and holds a Partnership Project Grant (Nos 1173126 and 1191874). K.A. is supported by an NHMRC Early Career Fellowship (No. 1157796) and an Early Career Researcher Grant of the University of Melbourne (No. ECR1202020).
Declaration of interest
J.P. reports receiving fellowship and grant funding from the NHMRC and grant funding from the Australian Institute of Health and Welfare outside the present work.









eLetters
No eLetters have been published for this article.