Introduction
Nurses are the primary providers of end-of-life care (Ristevski et al. Reference Ristevski, Leach and Bolton2022), and being with someone who is dying is not only a privilege but an essential part of nursing practice (Cheong et al. Reference Cheong, Ha and Tan2019). However, research indicates that undergraduate nursing students are largely unprepared to provide competent palliative and end-of-life care in clinical practice (Gillan et al. Reference Gillan, Jeong and van der Riet2021a). For many undergraduate nursing students, providing end-of-life care is a challenging and anxiety-provoking prospect (Fabro et al. Reference Fabro, Schaffer and Scharton2014). Students’ key concerns relate to their lack of knowledge and experience in communicating with patients and families and are reported to have difficulty initiating and engaging in difficult conversations at the end of life (Bloomfield et al. Reference Bloomfield, O’Neill and Gillett2015; Kantor and Stadelman Reference Kantor and Stadelman2020; Kirkpatrick et al. Reference Kirkpatrick, Cantrell and Smeltzer2017). Students also report not knowing what to say and having difficulties dealing with emotional responses (Gillett et al. Reference Gillett, O’Neill and Bloomfield2016). It is imperative that nursing students are given opportunities to develop effective communication skills, have confidence to initiate difficult conversations, and are able to provide emotional support for patients in their care (Kantor and Stadelman Reference Kantor and Stadelman2020).
It is widely acknowledged that the most valuable learning experiences are obtained through experiential learning within clinical practice settings (Garrino et al. Reference Garrino, Contratto and Massariello2017). However, challenges in nursing education continue due to the limited availability of clinical placements (Sarabia-Cobo et al. Reference Sarabia-Cobo, Alconero-Camarero and Lavin-Alconero2016), especially in speciality areas of practice such as palliative care, where there are limited opportunities to develop communication skills focusing on difficult conversations (Bloomfield et al. Reference Bloomfield, O’Neill and Gillett2015).
In response to the limited access to clinical placements internationally, nursing educators are increasingly utilizing simulation in areas such as critical care (Bautista and Bartos Reference Bautista and Bartos2021), resuscitation (Demirtas et al. Reference Demirtas, Guvenc and Aslan2021), and teaching and assessment of psychomotor skills (Hoang et al. Reference Hoang, Copnell and Lawrence2022). Introducing simulated palliative and end-of-life care into undergraduate nursing curricula has the potential to provide students with end-of-life care experiences that may be absent in clinical placements. Palliative and end-of-life care simulation has the potential to enhance nursing students’ experiences with end-of-life care (Gillan et al. Reference Gillan, van der Riet and Jeong2014a, Reference Gillan, van der Riet and Jeong2016; Kirkpatrick et al. Reference Kirkpatrick, Cantrell and Smeltzer2017; Kunkel et al. Reference Kunkel, Kopp and Hanson2016) and can facilitate nursing students’ self-confidence and competence in providing palliative and end-of-life care in clinical practice (Alconero-Camarero et al. Reference Alconero-Camarero, Sarabia-Cobo and Gonzalez-Gomez2018).
In Australian nursing education, nursing students are widely exposed to simulation in a wide range of contexts; however, palliative care and end-of-life care simulations are still developing (Gillan et al. Reference Gillan, Jeong and van der Riet2014b). A recent review by Kirkpatrick et al. (Reference Kirkpatrick, Cantrell and Smeltzer2017) investigating the use of palliative care simulation in undergraduate nursing education found only 2 (n = 2) of the 19 articles originating from Australia (Gillan et al. Reference Gillan, van der Riet and Jeong2013, Reference Gillan, van der Riet and Jeong2016); and Hoang et al.’s (Reference Hoang, Copnell and Lawrence2022) scoping review of end-of-life care simulation in undergraduate nursing education identified 42 articles, with only 3 originating from Australia from the same authors (Gillan et al. Reference Gillan, van der Riet and Jeong2013, Reference Gillan, van der Riet and Jeong2016, Reference Gillan, Jeong and van der Riet2021b).
A method of simulation that is underutilized in nursing education is standardized patient (SP) simulation. SP simulation involves trained actors who act out a particular case scenario and take on many roles in the simulation, including patients, family members, or health professionals (Coates Reference Coates2021). In learning situations focusing on psychosocial settings where a human voice and emotion are needed, the use of SPs can be particularly valuable (Fink et al. Reference Fink, Linnard-Palmer and Ganley2014). The realism of a situation created when using SPs has the potential to consolidate the linking of theory to practice more effectively than when interacting with a manikin (Tamaki et al. Reference Tamaki, Inumaru and Yokoi2019). Scenarios involving patient actors allow students the opportunity to practice and improve on therapeutic communication skills (Halliday et al. Reference Halliday, Dorney and Landis2022), psychomotor skills (Sarmasoglu et al. Reference Sarmasoglu, Dinc and Elcin2016), and students self-efficacy (Escribano et al. Reference Escribano, Cabanero-Martinez and Fernandez-Alcantara2021) and are widely known as a better choice when compared to manikins when learning involves patients’ psychosocial or emotional responses (Fink et al. Reference Fink, Linnard-Palmer and Ganley2014).
Due to the increased realism of SPs, this is an exciting mode of simulation for the application of palliative care and end-of-life care education. However, there is limited research on the use of SPs in palliative and end-of-life care simulation for undergraduate nursing students, with only 3 research articles available in the literature, none of these studies arising from Australia. These studies used either a randomized controlled method (Tamaki et al. Reference Tamaki, Inumaru and Yokoi2019) or a quasi-experimental approach (Escribano et al. Reference Escribano, Cabanero-Martinez and Fernandez-Alcantara2021; Fink et al. Reference Fink, Linnard-Palmer and Ganley2014). The results of these studies showed that the SP simulation improved communication skills (including empathy, respect, and assertiveness) (Escribano et al. Reference Escribano, Cabanero-Martinez and Fernandez-Alcantara2021), increased self-efficacy and self-confidence with communication (Escribano et al. Reference Escribano, Cabanero-Martinez and Fernandez-Alcantara2021; Fink et al. Reference Fink, Linnard-Palmer and Ganley2014), and physical assessment and psychological care (Tamaki et al. Reference Tamaki, Inumaru and Yokoi2019). Knowledge and skill performance scores also increased significantly (Tamaki et al. Reference Tamaki, Inumaru and Yokoi2019). While these studies provided evidence to support SP as an effective method of teaching practical skills and communication skills, there was no focus on the psychosocial aspects of difficult conversations that occur as part of end-of-life care.
While there is a growing repertoire of palliative care simulation, the use of SPs is sparsely utilized in undergraduate nursing education in Australia. A recent scoping review on the use of simulation in undergraduate nursing education in Australia identified 9 out of 44 journal articles using SP simulation (Kunst et al. Reference Kunst, Henderson and Johnston2018), with only one focusing on palliative or end-of-life care (Gillan et al. Reference Gillan, van der Riet and Jeong2013) and none with a focus on communication at the end of life. Although the focus of this review was not specifically relating to palliative care or communication, this recent review does provide a snapshot of the types of simulation approaches used in Australian undergraduate nursing programs.
These studies indicate an increased interest in palliative care or end-of-life care simulation using SPs; however, there is a gap in simulation, specifically focusing on difficult conversations at the end of life. Only 3 research articles, one qualitative (Jeffers et al. Reference Jeffers, Lippe and Justice2022), one quantitative (Cannity et al. Reference Cannity, Banerjee and Hichenberg2021), and one mixed-method study (Bloomfield et al. Reference Bloomfield, O’Neill and Gillett2015), were found to directly address end-of-life care conversations. Major findings from these studies were increased self-confidence with communication at the end of life following SP simulation (Cannity et al. Reference Cannity, Banerjee and Hichenberg2021), increased confidence and competence with communicating with dying patients and their families (Bloomfield et al. Reference Bloomfield, O’Neill and Gillett2015), and “delivering bad news is difficult” (Jeffers et al. Reference Jeffers, Lippe and Justice2022: 202).
Self-confidence is an important construct to develop for nursing students during their undergraduate degree. Nursing students who are self-confident in their knowledge and clinical skills are able to cope with complex clinical situations (Guerrero et al. Reference Guerrero, Ahmed and Attallah2022), including managing difficult conversations at the end of life. Measuring self-confidence was an important consideration for some of the identified studies; however, all but one of these studies used researcher-developed self-confidence scales (Escribano et al. Reference Escribano, Cabanero-Martinez and Fernandez-Alcantara2021). Escribano et al. (Reference Escribano, Cabanero-Martinez and Fernandez-Alcantara2021) used the “Self-efficacy in communication skills SE12 Scale,” which has shown internal consistency (Cronbach’s α 0.95) and test–retest reliability (interclass correlation coefficient 0.71).
Student satisfaction is important to evaluate as it is associated with greater engagement and motivation, which subsequently facilitates the learning process (Alconero-Camarero et al. Reference Alconero-Camarero, Sarabia-Cobo and Gonzalez-Gomez2018). Student satisfaction with the method of simulation is also important, as this has not been fully explored in previous studies in the context of palliative care. Only one study reported on satisfaction with SPs simulation (Fink et al. Reference Fink, Linnard-Palmer and Ganley2014). Satisfaction with the SP method in this study was measured by only 2 questions on the 10-item satisfaction survey, providing minimal evaluation data (Fink et al. Reference Fink, Linnard-Palmer and Ganley2014). While the results of the other studies demonstrated students’ acquisition of skills, there was no evaluation of students’ satisfaction with an SP being used as the method of simulation, which is an area lacking in nursing education (Escribano et al. Reference Escribano, Cabanero-Martinez and Fernandez-Alcantara2021; Tamaki et al. Reference Tamaki, Inumaru and Yokoi2019).
While the findings from these studies are positive, there are some limitations to be considered. One study was a pilot study with small numbers (n = 15 nursing students pre-test/post-test responses) (Bloomfield et al. Reference Bloomfield, O’Neill and Gillett2015). The SP experience in Cannity et al.’s (Reference Cannity, Banerjee and Hichenberg2021) study was only one small component of a day-long training session, therefore findings may be attributed to the whole course and not solely to the SP simulation. The primary purpose of the study by Jeffers et al. (Reference Jeffers, Lippe and Justice2022) was to use simulation to reflect on communication competence, therefore findings excluded any details on the student experience of interacting with the SP. Due to the limited number of studies on this topic, further studies involving the use of SP in end-of-life discussions are still needed (Bloomfield et al. Reference Bloomfield, O’Neill and Gillett2015).
The results of these studies show a significant gap in the literature on the use of SP simulation in palliative and end-of-life care, with a focus on difficult conversations at the end of life from an Australian perspective.
Thus the objective of our study was to assess nursing students’ satisfaction and self-confidence with palliative care and end-of-life care simulation using the Student Satisfaction and Self-Confidence in Learning Scale (SSSCLS) (National League of Nursing [NLN], 2005a) and the Simulation Design Scale (SDS) (NLN, 2005b), scales not previously used in SP palliative care or end-of-life care simulation, and address the gap in knowledge on palliative care and end-of-life care simulation using SPs focusing on difficult conversations.
Hypothesis
The hypothesis proposed for this study was: palliative care simulation using SP patients leads to high levels of satisfaction with the simulation methods used and high levels of self-confidence in mastering palliative care skills and managing difficult conversations relating to end-of-life care.
Methods
Study design
A descriptive post-intervention quantitative design.
Ethical considerations
The study received ethical approval from the university’s Human Research and Ethics Committee (approval no. deidentified). Students were advised on the participant information sheet, provided through email, that completing surveys was completely voluntary and anonymous, and that participation or non-participation had no impact on their studies within the degree. Once surveys were submitted, students were unable to withdraw as no identifying information was collected and individual responses were not identifiable.
Participation in the study involved post-simulation completion of the SSSCLS and SDS, which were distributed and collected by a staff member who was not involved in the research. Surveys were completed immediately following the simulation debriefing. Printed surveys reinforced anonymous survey completion/non-completion. The completion of surveys implied consent to participate.
Participants and setting
All nursing students enrolled in the 3rd year Palliative Care Nursing elective unit in the first semester of their final year of study in 2021 (n = 51) were invited to participate. Only students enrolled in this unit of study and who participated in the non-compulsory simulation days (n = 31) were eligible to participate in the study.
Four palliative care simulation days were conducted over 4 weeks at a large metropolitan university in Australia. Simulations consisted of 2 different clinical scenarios, each delivered twice. The first simulation was set in an outpatient palliative care clinic (delivered during the first 2 simulation weeks), and the second simulation was an inpatient hospital scenario (delivered during the last 2 simulation weeks). Students self-enrolled into simulation sessions according to their own availability. Repeating simulation sessions gave students some flexibility in attending simulation days.
Intervention
Palliative care simulation was introduced into the palliative care elective unit in 2020 with the aim of improving student experiences and preparation for providing palliative and end-of-life care in clinical practice. The simulation intervention was underpinned by the Palliative Care Curriculum for Undergraduates (PCC4U) teaching resources and clinical case scenarios. Two clinical scenarios were delivered as SP simulation during 4 face-to-face workshops. The first scenario was female in her thirties with advanced breast cancer attending an outpatient palliative care clinic for advice on symptom management and psychosocial support. The second case was a male in his sixties with advanced metastatic bowel cancer in the hospital for pain and symptom management (more information can be found at https://pcc4u.org.au).
The NLN Jeffries Simulation Theoretical Framework (Jeffries and Rogers Reference Jeffries, Rogers and Jeffries2012) was used to guide the development and delivery of the simulation experiences. Simulation design characteristics included the simulation fidelity using trained SPs, scenario development using the evidence-based resources from PCC4U, pilot testing of simulation scenarios prior to the study, clearly identified learning objectives, and student support during the simulation experience (Jeffries et al. Reference Jeffries, Rodgers and Adamson2015).
Pre-simulation, students had access to the simulation scenarios, pre-simulation readings, and the relevant PCC4U modules and videos, this is consistent with the International Nursing Association for Clinical Simulation and Learning (INACSL) best practice standards for simulation (INACSL Standards Committee, McDermott et al. Reference McDermott, Ludlow and Horsley2021).
On the simulation days and prior to the simulation, students attended a lecture and a tutorial on the assessment and management of palliative care symptoms and communication in preparation for the application of knowledge during the simulation experience.
The simulation experience consisted of a 10-min pre-brief to orientate students to the clinical simulation space, reassure psychological safety by establishing a safe and non-judgmental environment within the simulation experience, and reaffirm the simulation learning objectives.
Students completed simulations in groups of up to 8 that consisted of 4 active participants and up to 4 observers. The simulations began with a verbal handover of the patient, followed by the clinical scenario, which lasted approximately 20 min.
Simulations were followed by a 20–25 min simulation debriefing led by the simulation facilitator, an experienced nursing educator with training in simulation and extensive experience with palliative care in clinical practice, using a standardized approach to simulation debriefing that included an adaptation of the Plus-Delta model, as aligned with the INACSL best practice standards for debriefing (INACSL Standards Committee, Decker et al. Reference Decker, Alinier and Crawford2021). All participants participated in simulation debriefing.
Instruments
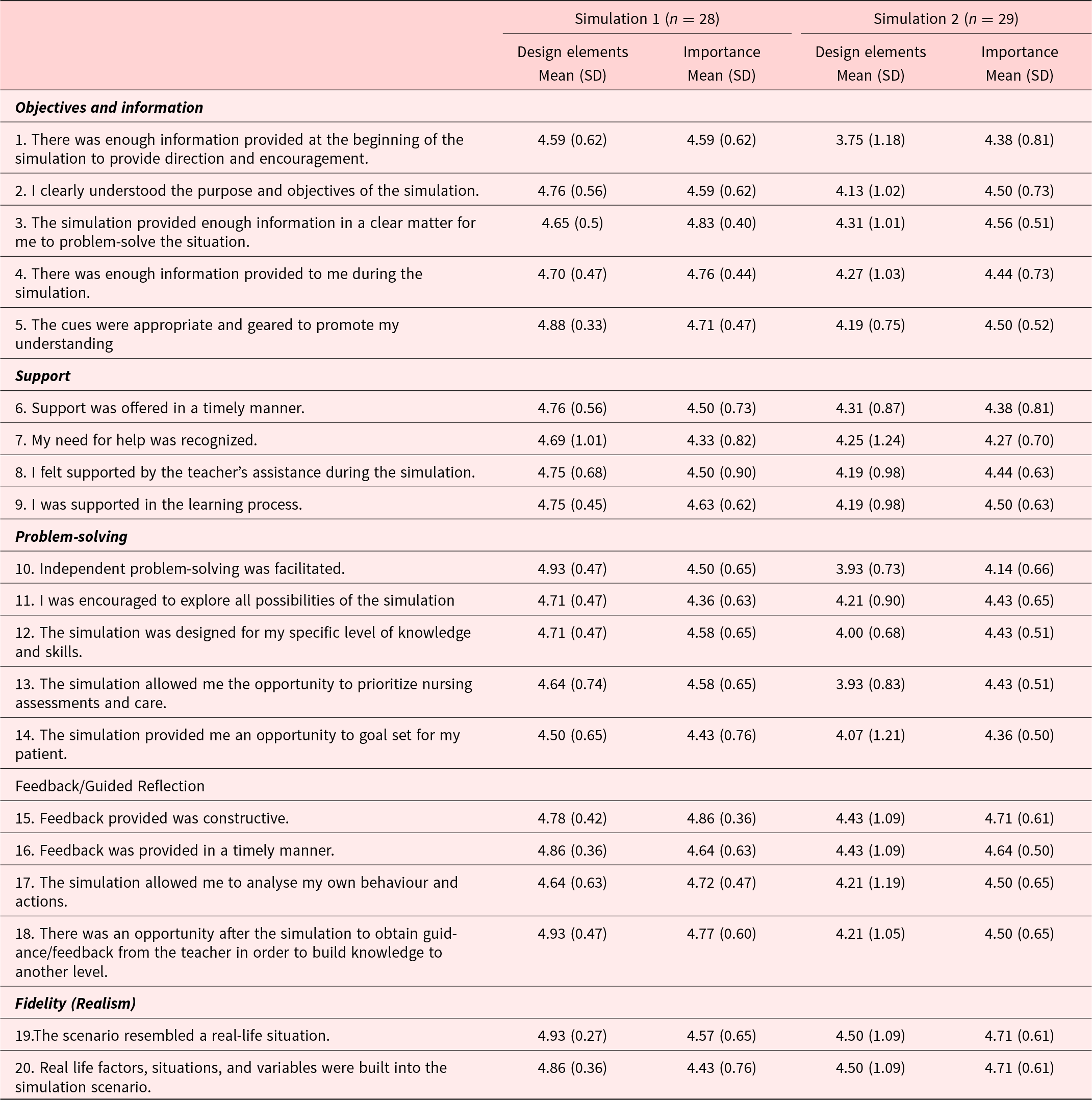
The instrument consisted of 2 surveys: the SSSCLS and the SDS. The SSSCLS was used to measure student satisfaction and self-confidence in learning through simulation. This 13-item instrument using a 5-point Likert scale (1 = strongly disagree to 5 = strongly agree) is designed to measure student satisfaction with the simulation activity (5 items) and self-confidence in learning (8 items). The original scale had a Cronbach’s α of 0.94 for student satisfaction and 0.87 for student self-confidence (NLN 2019). In this study, Cronbach’s α was 0.92 for student satisfaction and 0.86 for self-confidence. The SDS, a 20-item instrument using a 5-point scale (1 = strongly disagree to 5 = strongly agree), was designed to evaluate 5 design features of the simulations. The features rated are objectives/information (5 items), student support (4 items), problem-solving (5 items), guided reflection or feedback (4 items), and fidelity (2 items). The original scale had a Cronbach’s α of 0.92 for the presence of design features and 0.96 for the importance of features (Jeffries 2012). In this study, Cronbach’s α was 0.98 for the design feature element and 0.97 for importance.
Data analysis
Post-intervention SSSCLS and SDS scores were loaded into Excel and Statistical Package for the Social Sciences (SPSS) Version 26 to generate survey datasets. Post-test SSSCLS and SDS data were analyzed using descriptive statistics (mean; standard deviation [SD]). Participant characteristics are not included in the analysis, as this was perceived to potentially impact participant confidentiality (Rosenzweig et al. Reference Rosenzweig, Hravnak and Magdic2008).
Results
A total of n = 57 post-simulation surveys were completed (simulation 1, n = 28/31; simulation 2, n = 29/31), with a response rate of 90.32% and 93.54% (simulation 1 and simulation 2, respectively). The descriptive statistics for the SSSCLS are presented in Table 1. Due to the nature of this study being a descriptive post-intervention study and lacking a control group, it is difficult to assess if the high evaluative scores were directly related to the simulation experience, and thus the results should be interpreted with caution.
Table 1. Student Satisfaction and Self-Confidence in Learning Scale

We hypothesized that using SPs in palliative care simulation would lead to high levels of satisfaction with the simulation method and high levels of self-confidence in mastering palliative care skills and managing difficult end-of-life conversations, and our results support this hypothesis. The results from the SSSCLS and SDS show that overall, students had a high level of satisfaction and self-confidence in caring for a simulated palliative patient. Results also indicate that both the simulation and the teaching methods used during the simulated learning experience were also very positive.
In simulation 1, of note are the high mean scores (greater than 4 in the Likert scale 1–5) for all but one question, “it is the instructor’s responsibility to tell me what I need to learn of the simulation activity” (3.88 ± 1.15). The highest score (5.00 ± 0.00) was for the question “I enjoyed how my instructor taught the simulation.”
In simulation 2, there was a similar pattern of high mean scores. The highest score in this group was for the item “it is my responsibility as the student to learn what I need to know from this simulation activity” (4.64 ± 0.49). The item “it is the instructor’s responsibility to tell me what I need to learn of the simulation activity” in this group also received the lowest score (3.79 ± 1.25).
The students in this study reported the simulation design elements (SDS) positively. Three items had equally high scores for simulation 1. These were “independent problem solving was facilitated” (4.93 ± 0.47), “there was an opportunity after the simulation to obtain guidance/feedback in order to build knowledge to another level” (4.93 ± 0.47), and “the scenario resembled a real-life situation” (4.93 ± 0.27). The lowest score for simulation 1 was for the item “the simulation provided me an opportunity to goal set for my patient” (4.50 ± 0.65).
For simulation 2, 2 items scored equally highly, “the scenario resembled a real-life situation” (4.50 ± 1.09) and “real life factors, situations and variables were built into the simulation scenario” (4.50 ± 1.09). The lowest score was for item “there was enough information provided at the beginning of the simulation to provide direction and encouragement” (3.75 ± 1.18).
In terms of items of importance, “feedback provided was constructive” was rated the highest in both simulations. Simulation 1 had a slightly higher mean (4.86, SD ± 0.36) compared with simulation 2 (4.71 ± 0.61). Of lowest importance was “my need for help was recognised” (4.33 ± 0.82) for simulation 1 and “independent problem solving was facilitated” (4.14 ± 0.66) for simulation 2. The findings of the SDS portion of the survey are presented in Table 2.
Table 2. Simulation Design Scale
Discussion
The simulation scenarios used in this research were based on the PCC4U resources. The PCC4U project, funded by the Australian Government Department of Health, aims to improve the confidence and skills of the Australian health-care workforce to meet the population’s palliative care needs (PCC4U 2022). The resources developed by PCC4U are evidence-based and provide a range of clinical scenarios to support learning (PCC4U 2022). During this research, we used 2 clinical scenarios to support student’s learning, with a focus on communication when approaching difficult conversations at the end of life. The simulation used SPs playing the roles of Michelle, who was based in an outpatient clinic setting, and William, who was an inpatient. The use of SPs gave students the opportunity to undertake difficult conversations in the context of both settings and provided students the chance to practice vital communication skills required by all health-care professionals (Paal et al. Reference Paal, Brandstotter and Lorenzi2019). These findings support other research using SPs that have shown improvement in communication skills in the context of palliative care or end-of-life care communication (Bloomfield et al. Reference Bloomfield, O’Neill and Gillett2015; Jeffers et al. Reference Jeffers, Lippe and Justice2022).
Both groups were particularly satisfied with the instructor’s teaching method. Facilitation of simulation requires a skilled instructor who has the education, skill, and ability to guide, support, and seek out ways to assist participants in achieving expected outcomes (INACSL Standards Committee, Persico et al. Reference Persico, Belle and DiGregorio2021). In this study, the instructor had content knowledge of palliative care in addition to simulation pedagogy and therefore could support students to achieve the required learning outcomes. Both groups also indicated overall high levels of self-confidence in relation to mastering palliative care skills and the palliative care content of the simulation activities, and that they were developing the skills and obtaining the knowledge required for clinical practice. This is a positive finding, while simulation has been found to increase nursing students’ satisfaction and self-confidence (Cura et al. Reference Cura, Kocatepe and Yildirim2020; de Oliveira Costa et al. Reference de Oliveira Costa, de Medeiros and Dias Coutinho2020; Dincer and Ataman Reference Dincer and Ataman2020; Olaussen et al. Reference Olaussen, Heggdal and Tvedt2020; Zapko et al. Reference Zapko, Ferranto and Blasiman2018; Zulkosky et al. Reference Zulkosky, Minchhoff and Dommel2021), to date there is limited research on student satisfaction or improved self-confidence with palliative care or end-of-life care simulation.
The overall trend of higher scores in student’s satisfaction and self-confidence was evident for simulation 1 where students contributed to addressing both psychological and physical needs of the patient and were challenged and supported to address difficult conversations as the scenario unfolded. This scenario, based in an outpatient setting, focused on communication and symptom management compared with a hospital-based pain management scenario in simulation 2. A possible explanation for this is that simulations based in primary care-type contexts have been found to be well liked by students, in part due to the scenarios not being as time-critical and dependent on checklists as more acute scenarios (Lunde et al. Reference Lunde, Moen and Jakobsen2021).
In this study, the results of the SDS indicated that perceptions of simulation design elements for both simulations were high overall. Both simulations used an SP, and consistent with other research, the use of a simulation methodology, which is the most realistic, enables students to feel as though they are learning in a real clinical context and offers an active learning experience (Escribano et al. Reference Escribano, Cabanero-Martinez and Fernandez-Alcantara2021; Rosenzweig et al. Reference Rosenzweig, Hravnak and Magdic2008; Tamaki et al. Reference Tamaki, Inumaru and Yokoi2019). Although SPs were used for both simulations, the scenarios were different, and this may be reflected in the slightly higher fidelity and realism score for the outpatient scenario, which is possibly easier to recreate than a hospital scene. These positive findings are of value in confirming that SPs are useful in creating a realistic clinical situation to prepare students for real-world practice in both care settings. It also provides justification for the expense in an educational era, which may have limited funding for activities such as simulation (So et al. Reference So, Chen and Wong2019).
In terms of the importance of items on the SDS, receiving feedback that was constructive rated the highest for both simulations. Students may not have had exposure to palliative care during their clinical placements, therefore, they value being guided through purposeful discussion of their actions during the simulation through debriefing (Thidemann and Söderhamn Reference Thidemann and Söderhamn2013). By increasing confidence and competence in end-of-life care among students, this may, in turn, be translated into clinical practice and has the potential to improve end-of-life care for patients and their families.
Both clinical scenarios focused on patients with different cancers and of different age groups. Michelle, a young woman with a young family undergoing treatment for breast cancer, and William, aged in his early 60s with metastatic bowel cancer, are clinical scenarios rarely seen in the sparse palliative care simulation literature. Recent palliative care simulation literature using SPs and approaching difficult conversations have used non-cancer diagnoses such as heart failure and Chronic Obstructive Pulmonary Disease (COPD) (Jeffers et al. Reference Jeffers, Lippe and Justice2022). The only research of this kind that used cancer diagnosis also used metastatic bowel cancer diagnosis of a middle-aged male (Bloomfield et al. Reference Bloomfield, O’Neill and Gillett2015). To date, this study is the first of its kind to use a scenario with a younger female patient with advanced breast cancer. This study gave participants the opportunity to apply clinical skills to patient symptoms beyond non-cancer diagnoses and of varying age groups.
Of the available studies assessing self-confidence and satisfaction with palliative or end-of-life care simulation, there is very limited research using validated instruments such as SSSCLS. Alconero-Camarero et al. (Reference Alconero-Camarero, Sarabia-Cobo and Gonzalez-Gomez2018), using low-fidelity simulation, in their descriptive, observational, and correlational study used 3 scales (SSSCLS Spanish version; Questionnaire for dealing with stress; Trait Meta-Mood Scale-24) with 2nd year nursing students (n = 74). Fabro et al. (Reference Fabro, Schaffer and Scharton2014) used the SSSCLS in conjunction with the Educational Practices Questionnaire to evaluate student learning (n = 21) from palliative care simulation using a high-fidelity manikin and the student playing the role of the patient’s daughter.
While these studies add to the limited available research on palliative care simulation, the simulation modalities used are either low- or high-fidelity simulation. Our study is the first that we are aware of that has used SPs and been evaluated using the SSSCLS. There were no studies found on palliative care or end-of-life care simulation using the SDS. To our knowledge, this is the first study to use both the NLN-developed SSSCLS and SDS for assessing palliative care or end-of-life care simulation.
Recommendations for research and practice
The INACSL 2020–2023 simulation research priorities provide targeted areas of focus to address known gaps in the literature on simulation and to address the INACSL vision that simulation and innovation transform lives (Franklin and Luctkar-Flude Reference Franklin and Luctkar-Flude2020). Among these research priorities are interprofessional simulation, psychomotor skill retention, and transition to practice (Franklin and Luctkar-Flude Reference Franklin and Luctkar-Flude2020).
To address these key research priorities and gaps in the literature, from this research, it is recommended that palliative care and end-of-life care interprofessional simulation, which include undergraduate health students from a range of professions, focusing on patient outcomes would be of benefit to further develop skills surrounding communication at the end of life. In addition, longitudinal studies that evaluate specific time points post-simulation along a time continuum may give more insight into the immediate and long-term effects that palliative care and end-of-life care simulation have on nursing students’ skill retention and on new graduates transitioning to clinical practice.
While palliative care and end-of-life care simulation are developing, there are few studies that explore the impact that palliative care and end-of-life care simulation have on clinical practice for both undergraduate nursing students and new graduates. Furthermore, there are few studies on SP simulation and even fewer with a focus on communication at the end of life. This study on SP simulation focusing on difficult conversations at the end of life is the first of its kind, originating from Australia. The results of our study showed that nursing students reported high levels of self-confidence and satisfaction with this novel and innovative mode of simulation. A recommendation from our research is a change in simulation practice with the adoption of SPs in the roles of patients, family members, and caregivers.
Limitations
The small convenience sample of nursing students enrolled in an elective unit of study from a single site restricts the generalizability of the results. The post-intervention only study design limits the interpretation of results. While this was a restriction imposed by factors outside the authors’ control, future studies will aim to include pre- and post-intervention surveys response to allow for comparison of results. In addition, a mixed-method approach that provides the opportunity for qualitative responses would also have strengthened this research and will be considered for future research on this topic. While this study included students who actively participated in the simulation scenarios as well as observers, there was no opportunity to rotate roles so each student could actively participate in the simulations, nor did this research involve comparison between active participants and observers. Future research is planned to include a comparison of roles between participant and observer to determine differences in participants’ experiences and whether there is a difference in knowledge retention between the 2 groups.
Conclusion
Nursing students have limited exposure to palliative care and end-of-life care experiences during their clinical placements, and students report feeling unprepared to provide quality end-of-life care in clinical practice. Little is known of student’s self-confidence and satisfaction with palliative and end-of-life care simulation. This study is contributing to the limited available research on palliative care simulation and shows promising results in the development of self-confidence and satisfaction in learning about palliative and end-of-life care. SP simulation focusing on difficult conversations has been found to assist in developing students’ communication skills with patients and families at the end of life.
Acknowledgments
The authors wish to thank the nursing students who participated in this research project and would like to acknowledge David Klug and Kylie Ash from PCC4U.
Funding
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Competing interests
The authors report no competing interests.





