Despite the fact that an estimated 30% of populations from areas of conflict have post-traumatic stress disorder (PTSD), Reference Steel, Chey, Silove, Marnane, Bryant and van1 very little evidence exists on how best to treat this condition. According to two Cochrane reviews on the treatment of PTSD, the best evidence exists for pharmacotherapy with selective serotonin reuptake inhibitors (SSRIs), mainly sertraline, and cognitive–behavioural therapy (CBT). Reference Bisson and Andrew2,Reference Stein, Ipser and Seedat3 A recent Cochrane review on the treatment of PTSD with a combination of psychotherapy and pharmacotherapy was inconclusive because of too few studies. Reference Hetrick, Purcell, Garner and Parslow4 These Cochrane reviews, however, have primarily focused on studies with patients with different types of trauma, including sexual assault or traffic accidents, with only a few studies included on war-trauma (mainly Western war veterans). In addition, most patients in trials specifically have PTSD, whereas traumatised refugees have several comorbidities. Reference Buhman, Mortensen, Lundstroem, Ryberg, Nordentoft and Ekstroem5 Even less evidence exists on the effectiveness of PTSD treatments in traumatised refugees. Several systematic reviews have been published over the past couple of years; Reference Crumlish and O'Rourke6,Reference Palic and Elklit7 however, the evidence base on effective treatments for traumatised refugees is extremely limited. Pharmacotherapies examined in trauma-affected refugees include SSRIs (paroxetine and sertraline) Reference Otto, Hinton, Korbly, Chea, Ba and Gershuny8,Reference Smajkic, Weine, Djuric-Bijedic, Boskailo, Lewis and Pavkovic9 and prazozine. Reference Boynton, Bentley, Strachan, Barbato and Raskind10,Reference Boehnlein and Kinzie11 With regard to psychotherapy for traumatised refugees, various forms of exposure therapy have been examined by a few groups of researchers using specific therapeutic approaches, including narrative exposure therapy Reference Neuner, Onyut, Ertl, Odenwald, Schauer and Elbert12,Reference Neuner, Schauer, Klaschik, Karunakara and Elbert13 and culturally adapted CBT. Reference Hinton, Chhean, Pich, Safren, Hofmann and Pollack14,Reference Hinton, Pham, Tran, Safren, Otto and Pollack15 Some promising results on CBT have been published, although the studies are of limited quality Reference Kruse, Joksimovic, Cavka, Woller and Schmitz16,Reference Paunovic and Ost17 or on patients with a common trauma such as sexual assault or torture. Reference Bass, Annan, McIvor Murray, Kaysen, Griffiths and Cetinoglu18,Reference Carlsson, Mortensen and Kastrup19 A couple of follow-up studies on traumatised refugees from Denmark (without a control group) have found limited evidence for improvement in the condition of the patients. Reference Carlsson, Mortensen and Kastrup19,Reference Palic and Elklit20 Given this limited and often conflicting evidence base, this study sought to evaluate various treatments for a ‘real-life’ clinical sample of traumatised refugees living in Denmark, using sertraline in combination with mianserin and psychoeducation, or CBT or a combination of medicine and psychotherapy.
Method
Trial design
The trial was a pragmatic randomised controlled 2 × 2 factor trial (registered with Clinicaltrials.gov, NCT00917397, EUDRACT no. 2008-006714-15). The allocation ratio to the four groups was 1:1:1:1.
Participants
Eligibility criteria for participants were based on the ICD-10 21 research criteria and included:
-
(a) age 18 years and older
-
(b) refugees and persons based in Denmark because of family reunification with a refugee
-
(c) PTSD according to the ICD-10 21 diagnostic criteria
-
(d) a history of war-related psychological trauma such as imprisonment, torture, inhuman and degrading treatment or punishment, organised violence, prolonged political persecution and harassment or war
-
(e) motivation to receive treatment
-
(f) written, voluntary informed consent.
Patients were excluded if they:
-
(a) Had a severe personality disorder (ICD-10 diagnosis F2x and F30.1-F31.9). Patients were not excluded solely based on psychotic symptoms, however, as these are prevalent in the study population.
-
(b) Were addicted to psychoactive substances (ICD-10 F1x.24-F1x.26). The use of benzodiazepines or morphine prescribed by a physician did not lead to exclusion as it was expected that many patients would take several different kinds of painkillers and tranquilisers.
-
(c) Had a need for somatic or psychiatric hospitalisation.
-
(d) Were pregnant or lactating.
Patients were screened for psychoses using chapters 1, 10, 14, 16, 17, 18 and 19 of the Schedules for Clinical Assessment in Neuropsychiatry (SCAN), version 2.1. Reference Wing, Babor, Brugha, Burke, Cooper and Giel22 Motivation to engage in treatment was assessed by the physician at the screening interview. Patients who based on clinical impression were judged to be clearly not motivated for treatment were not offered treatment at the clinic.
All data were collected at the Competence Center for Transcultural Psychiatry, which is part of the public psychiatric heathcare system of the greater Copenhagen area in Denmark. The Competence Center (henceforth called ‘the clinic’) offers out-patient treatment specifically to immigrants and refugees with mental health problems and specialises in treating patients with trauma related to war, torture or persecution.
Interventions
At the beginning of the trial, all screened patients participated in a pre-trial assessment lasting 1–2 h divided into one to two sessions. Patients were included in the trial based on this assessment. All patients attended one session with a social worker at the beginning of the treatment to discuss their social situation. During the treatment period, there was also a limited opportunity to make additional appointments with the social worker as needed by the patient. Each patient ended with an evaluation session where the patient, physician, psychologist and social worker (if need be) were present.
Translation services were provided during assessment and treatment consultations on an as-needed basis (which was the case for 54% of patients). All of the interpreters were associated with the clinic and had experience in translating rating scales, psychotherapy and psychoeducational sessions. To determine programme adherence psychoeducation topics covered, psychotherapeutic methods used and cooperation with medical treatment were registered at each session.
Pharmacotherapy
Medicine consisted of sertraline gradually increased by 25–50 mg to a maximum dose of 200 mg. Patients reporting problems sleeping were supplemented with mianserin in doses of 10–30 mg at night, with doses titrated weekly by 10 mg. Patients who had too many side-effects from sertraline were switched to mianserin solely. Any other psychopharmacological treatment at baseline was ideally discontinued according to the Maudsley Guidelines. Reference Taylor, Paton and Kapur23 If patients had psychotic symptoms prior to treatment, antipsychotic treatment was continued. If the patient was not taking antipsychotic treatment at baseline, small doses of perphenazine were administered.
Psychoeducation
Psychoeducation for patients receiving antidepressants was provided by the doctor as part of the 45-minute consultation when medication was adjusted. Psychoeducation was manualised and covered the illness, treatment, sleep, lifestyle (including relaxation exercises), physical activity and social relations, pain, cognitive function and the influence of the illness on the family. Psychoeducation was also incorporated in the psychotherapy manual but was used on a more flexible basis and was more integrated with therapy. There was no overlap in content between psychoeducation approaches in therapy and as part of the sessions with a doctor.
Psychotherapy
CBT treatment was manualised and developed in cooperation with specialists in CBT. Treatment included core CBT methods, methods from acceptance and commitment therapy (ACT), mindfulness exercises and in vivo and visualised exposure. Psychologists trained in CBT and receiving supervision by specialists in CBT conducted the psychotherapeutic treatment. The use of the various methods in the manual was logged on a standard checklist so that a fidelity check could be made in the analysis. The four intervention groups were as follows.
Combination treatment
CBT, psychopharmacological treatment and consultations with a physician for 6 months, starting with 2 months of weekly treatment sessions with antidepressants and psychoeducation, followed by 4 months of CBT sessions weekly and monthly consultations with a physician for adjustment of antidepressant treatment. In total, the aim was for the treatment to consist of 10 consultations with a physician and 16 sessions with a psychologist.
Medicine
Psychopharmacological treatment, psychoeducation and consultations with a physician on a weekly basis for 2 months followed by a monthly consultation for a period of 4 months. The aim was for the treatment to consist of a total of 10 consultations with a physician.
Psychotherapy
CBT sessions with a psychologist over 6 months. The aim was for the treatment to consist of a total of 16 sessions with a psychologist. Any psychopharmacological treatment was administered by the referring physician and was ideally continued during the treatment period.
Waiting list
The control group was on the waiting list for 6 months. Any psychopharmacological treatment was administered by the referring physician and ideally continued during the treatment period.
Outcomes
The primary outcome measure of the study was PTSD severity as measured by the Harvard Trauma Questionnaire's (HTQ) Reference Oruc, Kapetanovic, Culhane, Lavelle, Miley and Forstbauer24–Reference Mollica, Caspi-Yavin, Bollini, Truong, Tor and Lavelle27 symptom part IV. Secondary outcome measures included Hopkins Symptom Checklist-25 (HSCL-25) Reference Oruc, Kapetanovic, Culhane, Lavelle, Miley and Forstbauer24,Reference Kleijn, Hovens and Rodenburg25,Reference Mollica, Wyshak, de Marneffe, Tu, Yang and Khuon28,Reference Mollica, Wyshak, de, Khuon and Lavelle29 to assess symptoms of depression and anxiety, Hamilton Rating Scale for Depression and for Anxiety (HRSD Reference Hamilton30 and HRSA Reference Hamilton31 ), Symptom Checklist-90 (SCL-90) Reference Derogatis32 somatisation scale, visual analogue pain scales (VAS), Reference Olsen, Montgomery, Boejholm and Foldspang33 Sheehan Disability Scale (SDS) Reference Sheehan and Sheehan34,Reference Lam, Michalak and Swinson35 to assess level of functioning, and WHO-Five Well-being Index (WHO-5). Reference Bech36 Ratings were completed at pre-trial assessment and at the end of treatment. HRSD and HRSA are clinician-administered, and the other scales are self-report measures. All self-report questionnaires were available in the six most common languages at the clinic (Arabic, Farsi, Bosnian/ Serbo-Croatian, Russian, Danish and English), which included the languages of 92% of patients. If no translation was available, an interpreter translated the official version into the language of the patient.
The diagnosis of PTSD was obtained according to ICD-10 and DSM-IV 37 using the first 16 questions of HTQ. HSCL-25 is a shorter version of SCL-90 with a focus on anxiety and depression symptoms. Reference Oruc, Kapetanovic, Culhane, Lavelle, Miley and Forstbauer24–Reference Mollica, Wyshak, de, Khuon and Lavelle29 For both instruments, individual questions have a 1–4 Likert-scale format, with 4 being the most severe symptom level. The cut-off value for PTSD on HTQ is 2.5 and for depression and anxiety on HSCL-25 is 1.75. Depression and anxiety were further assessed with HRSD and HRSA, which are clinician-administered rating scales measuring the severity of depression based on a semi-structured interview. The items on the scales are scored in a 0–4 and 0–2 Likert format. Higher total scores equal greater symptom severity. The HSCL-25, HTQ, HRSD and HRSA have been used in many studies of refugees and torture survivors. Reference Hamilton30,Reference Hamilton31
Somatisation was rated using the somatisation section of the SCL-90, which has a 0–5 Likert format, with 5 being the highest symptom level. Reference Derogatis32 A VAS was used to estimate the level of pain in four different parts of the body: the back, upper extremities, lower extremities and head. VAS is widely used to assess intensity of symptoms and has previously been used to study pain in traumatised refugees and torture survivors. Reference Olsen, Montgomery, Boejholm and Foldspang33 On a VAS, the patient marks the symptom intensity on a 10 cm line, with 10 being the highest symptom intensity and 0 meaning no pain.
SDS is a self-report rating scale, which assesses the level of functioning in terms of family, work or activities of daily living and social networking by using three VASs from 0 to 10, with 10 being the lowest possible level of functioning. The scale has been used in a variety of psychiatric patient groups. Reference Sheehan and Sheehan34,Reference Lam, Michalak and Swinson35 To assess quality of life we used the WHO-5 scale, Reference Bech36 which is a widely used self-administered questionnaire with five questions (0–5 Likert scale, with 0 being the lowest score and 5 the highest). The theoretical raw score ranges from 0 to 25 and is transformed into a scale from 0 (worst thinkable well-being) to 100 (best thinkable well-being). Thus, higher scores mean better quality of life. The scale has been used to assess the quality of life in a series of psychiatric diagnostic groups. Finally, all patients were asked at the final evaluation whether they thought their condition had changed during treatment and whether this was because of the treatment received or other factors.
Sample size
Based on power calculations, we aimed at 50 patients to complete treatment in each group. With an estimated drop-out rate of 25%, this would require 270 patients to be included. Because of slightly higher drop out in the waiting list group, the trial was continued until 280 patients had been included. For 50 patients in each group, the power for the analysis of the quantitative outcome variables such as HTQ and HSCL-25 was calculated to be 32%, 70% and 93% if the differences between two groups corresponded to a standard deviation of 0.3, 0.5 and 0.7 respectively. Thus, power would be low if treatment effects were much smaller than 0.5 standard deviation; however, if there was no significant interaction between the CBT and the pharmacological treatment, it would be possible to compare groups with 100 individuals in each group. This provides substantially greater statistical power with the calculation for comparison of an average difference of 0.3, 0.5 and 0.7 s.d. showing power of 56%, 94% and close to a 100%. All power calculations were performed with a significance level of 5%.
Randomisation
Randomisation took place after the pre-trial assessment performed by a physician at the clinic. The randomisation sequence was computer generated by the Department of Biostatistics at University of Copenhagen, which was not otherwise involved in the research project. Randomisation was stratified by gender and total score on HTQ (above or below 3.2), so that patients with equal illness severity were allocated to all groups. The HTQ score of 3.2 reflected the mean score among the 50 patients who had been treated in the clinic before the trial was designed. Allocation was concealed by using sequentially numbered sealed envelopes. The envelopes were kept in an office physically separate from the clinic and were administered by secretaries, who were not associated with the research project. When a patient had been included in the trial, the physician telephoned the office administering the randomisation envelopes and patients were subsequently assigned to a treatment group.
Masking
It was not deemed possible to mask the patients, physician or psychologists to the treatment group because of the substantial differences between the treatment modalities. A masked outcome measure was obtained by rating all patients with HRSD and HRSA at baseline and follow-up. No similar observer-rating existed for PTSD. A group of medical students not otherwise involved in the treatment undertook the masked ratings and met regularly to increase rater reliability.
Statistical method
All statistical analyses were conducted in Stata 12 and 13. Pre-treatment scores were available for 280 patients, and post-treatment scores were available for 201–226 patients (226 for HTQ). To conduct intention-to-treat analyses with all 280 patients, a full information maximum likelihood (FIML) was used in analyses, which included both pre- and post-treatment scores. Stata's structural equation modelling procedure ‘sem’ was used to conduct these analyses which incorporates all available information including pre-treatment scores for patients without post-treatment scores. The primary and secondary quantitative outcome variables were analysed in several models: (a) linear regression analyses of pre-treatment scores; (b) linear regression of post-treatment scores in models including only medicine and psychotherapy as predictors; and (c) FIML with procedure sem to analyse post-treatment scores in models including medicine, psychotherapy and pre-treatment scores as predictors. Preliminary FIML analyses tested a model including pre-treatment scores, the two treatment factors and an interaction term. Since there were no significant interactions between medicine and psychotherapy, results are reported for models only including the two main effects. Significantly different distributions in the four treatment groups were found for country of origin and language, and these potentially confounding variables were included in models which also included the two treatment effects. All analyses of outcome variables were conducted with robust variance estimates.
Results
From June 2009 until June 2011, 380 patients were screened for the trial and 280 patients were randomised: 71 to medicine and psychotherapy (77% completers), 71 to treatment with medicine (87% completers), 70 to treatment with psychotherapy (74% completers) and 68 to the waiting list (71% completers; see flow diagram shown in Fig. 1). The last patient finished treatment in December 2012.

Fig. 1 Flow diagram.
The study population
Table 1 shows the distribution in the four treatment groups at baseline with regard to demographics, trauma history, physical and mental conditions, and previous psychiatric treatment. We only found a significant difference between groups with regard to country of origin and language. Almost all patients had a diagnosis of depression (94%). The high levels of comorbidity are further reflected in the rating scores in Table 2.
Table 1 Description of patients at baseline

| Medicine | No medicine | ||||
| All (n = 217) |
Therapy (n = 55) |
No
therapy (n = 62) |
Therapy (n = 52) |
No
therapy (n = 48) |
|
| Male, n (%) | 128 (59) | 29 (53) | 35 (56) | 30 (58) | 34 (71) |
| Country, n (%)* | |||||
| Iraq | 79 (36) | 20 (36) | 23 (37) | 23 (44) | 13 (27) |
| Iran | 27 (12) | 9 (16) | 5 (8) | 8 (15) | 5 (10) |
| Lebanon | 26 (12) | 6 (11) | 13 (21) | 3 (6) | 4 (8) |
| Ex-Yugoslavia | 35 (16) | 5 (9) | 7 (11) | 8 (15) | 15 (31) |
| Afghanistan | 21 (10) | 9 (16) | 6 (10) | 6 (12) | 0 (0) |
| Other | 29 (13) | 6 (11) | 8 (13) | 4 (8) | 11 (23) |
| Language, n (%) | |||||
| Reads and speaks one of six translation languages* | 197 (92) | 54 (98) | 57 (92) | 45 (90) | 41 (85) |
| Needs translation for treatment | 118 (54) | 31 (56) | 35 (56) | 25 (48) | 27 (56) |
| Trauma history, n (%) | |||||
| Torture | 92 (43) | 20 (38) | 25 (41) | 22 (42) | 25 (52) |
| Refugee camp | 60 (28) | 13 (24) | 23 (38) | 11 (22) | 13 (28) |
| Danish asylum centre | 130 (63) | 33 (62) | 42 (71) | 28 (57) | 27 (59) |
| Ex-combatant | 51 (24) | 13 (24) | 8 (13) | 16 (31) | 14 (29) |
| Psychopathology (in addition to post-traumatic stress disorder), n (%) | |||||
| Depression according to ICD-10 | 204 (94) | 52 (95) | 59 (95) | 49 (94) | 44 (92) |
| Personality change after catastrophic events (ICD-10 code F62.0) | 59 (27) | 17 (31) | 15 (24) | 12 (23) | 15 (31) |
| Psychotic during treatment | 19 (9) | 6 (11) | 2 (3) | 7 (13) | 4 (8) |
| Previous substance abuse | 25 (12) | 4 (7) | 7 (11) | 7 (13) | 7(15) |
| Reports traumatic brain injury | 55 (46) | 13 (41) | 19 (54) | 12 (39) | 11 (52) |
| In treatment for somatic disorder | 78 (36) | 16 (29) | 22 (35) | 17 (33) | 23 (48) |
| Age, years: mean (s.d.) | 45 (9) | 45 (10) | 43 (9) | 46 (8) | 47 (8) |
| Years since arrival in Denmark, mean (s.d.) | 14.7 (6.1) | 13.8 (1) | 15.0 (6) | 15(6) | 15.0 (6) |
| Years since symptoms started, mean (s.d.) | 14.7 (10) | 15.1 (10) | 17.3 (10) | 12.5 (8) | 13.1 (10) |
* Significant difference between groups tested with Pearson's χ2 and linear regression P<0.05.
Table 2 Outcomes: pre-treatment and post-treatment scores for each intervention group a

| Outcome | Medicine | Medicine + therapy |
Waiting list |
Therapy | Medication v. no medication regression coeffecient (95% CI) |
P | Therapy v. no therapy regression coeffecient (95% CI) |
P |
|---|---|---|---|---|---|---|---|---|
| HTQ | ||||||||
| Pre-treatment | 3.3 (0.5) | 3.2 (0.6) | 3.3 (0.5) | 3.3 (0.5) | 0.02 (− 0.12 to 0.16) | 0.83 | − 0.07 (− 0.21 to 0.07) | 0.31 |
| Post-treatment | 3.2 (0.6) | 3.2 (0.7) | 3.2 (0.5) | 3.3 (0.7) | 0.07 (− 0.08 to 0.22) | 0.39 | 0.06 (− 0.09 to 0.21) | 0.46 |
| HSCL-25 | ||||||||
| Pre-treatment | 3.1 (0.5) | 3.1 (0.5) | 3.1 (0.7) | 3.2 (0.6) | − 0.05 (− 0.19 to 0.10) | 0.51 | − 0.05 (− 0.19 to 0.09) | 0.48 |
| Post-treatment | 3.0 (0.7) | 3.0 (0.7) | 3.1 (0.6) | 3.0 (0.6) | 0.05 (− 0.11 to +0.20) | 0.54 | − 0.05 (− 0.20 to 0.11) | 0.55 |
| HRSD | ||||||||
| Pre-treatment | 26.3 (5.8) | 24.3 (5.6) | 23.6 (6.7) | 23.8 (5.4) | − 1.64 (− 3.17 to −0.11) | 0.04 | − 1.01 (− 2.51 to 0.49) | 0.19 |
| Post-treatment | 24.3 (7.4) | 22.2 (7.4) | 25.1 (6.3) | 23.9 (5.9) | 1.91 (0.40 to 3.42) | 0.01 | − 1.01 (− 2.58 to 0.56) | 0.21 |
| HRSA | ||||||||
| Pre-treatment | 28.3 (6.8) | 27.2 (7.4) | 26.5 (8.0) | 26.2 (6.9) | − 1.07 (− 3.01 to 0.88) | 0.28 | − 0.37 (− 2.29 to 1.54) | 0.70 |
| Post-treatment | 26.9 (9.1) | 26.6 (9.5) | 29.7 (6.8) | 27.1 (8.1) | 1.82 (− 0.23 to 3.87) | 0.08 | − 1.06 (− 3.17 to 1.05) | 0.33 |
| SCL-90 | ||||||||
| Pre-treatment | 2.6 (0.9) | 2.6 (0.9) | 2.7 (0.7) | 2.7 (0.8) | 0.12 (− 0.08 to 0.31) | 0.26 | 0.10 (− 0.11 to 0.30) | 0.35 |
| Post-treatment | 2.7 (1.0) | 2.6 (0.9) | 2.8 (0.8) | 2.8 (0.8) | 0.07 (− 0.12 to 0.26) | 0.48 | − 0.05 (− 0.23 to 0.14) | 0.64 |
| SDS | ||||||||
| Pre-treatment | 8.1 (1.9) | 7.8 (2.1) | 7.4 (2.2) | 7.8 (2.0) | − 0.21 (− 0.71 to 0.30) | 0.43 | 0.21 (− 0.29 to 0.72) | 0.40 |
| Post-treatment | 8.1 (2.3) | 7.7 (2.5) | 8.1 (1.7) | 8.3 (1.8) | 0.46 (− 0.41 to 0.97) | 0.07 | − 0.05 (− 0.56 to 0.47) | 0.86 |
| WHO-5 | ||||||||
| Pre-treatment | 13.8 (14.1) | 15.7 (16.9) | 12.0 (15.2) | 13.2 (13.0) | − 2.16 (− 5.90 to 1.59) | 0.26 | 1.57 (− 2.23 to 5.37) | 0.42 |
| Post-treatment | 16.5 (20.4) | 17.1 (20.2) | 13.9 (16.4) | 13.0 (14.3) | − 3.61 (− 7.98 to 0.77) | 0.11 | − 1.19 (− 5.64 to 3.26) | 0.60 |
HTQ, Harvard Trauma Questionnaire (1-4,1 best score); HSCL-25, Hopkins Symptom Checklist - 25 (1-4,1 best score); HRSD/A Hamilton Rating Scale for Depression/Anxiety (0-4, 0 best score); SCL-90, Symptom Checklist - 90 (1-4,1 best score); SDS, Sheehan Disability Scale (0-10, 0 best score); WHO-5, WHO-Five Well-being Index (0-100,100 best score); +, improvement of condition; −, worsening of condition.
a. Post-treatment regression coefficients are adjusted for baseline.
The treatment
A summary table of the treatment in the four groups can be found in the online supplement. Two patients in the group assigned to receive both psychotherapy and medical treatments only received psychotherapy. All patients received the planned treatment in the group receiving only medical treatment. Six patients in the group assigned to receive only psychotherapy also received treatment with sertraline or mianserin, and 27% of patients in this group received another type of antidepressant. In the group receiving no treatment, five patients received trial medicine and 21% received other antidepressants at some point during the trial.
All patients in the two groups receiving medical treatment also received psychoeducation. The mean number of sessions with a physician was nine in groups receiving medical treatment. The mean maximum dose of sertraline was 132.1 mg (+/− 56 mg) and 20.0 (+/− 10 mg) of mianserin. The end dose of both drugs was slightly lower at 119.3 mg sertraline (+/− 66 mg) and 15.7 mg (+/− 12 mg) mianserin.
All patients allocated to psychotherapy received psychotherapeutic treatment. The treatment consisted of, on average, 12 sessions. Although 10% of patients did not receive treatment using any of the core CBT methods (cognitive diamond, working with schemata, restructuring of thoughts and working with avoidance), 58% of patients received treatment using these methods at least five times. Of the patients receiving therapy, 90% were treated with core cognitive methods, 70% with ACT, 83% with mindfulness exercises and 19% with trauma-focused exposure therapy. When defining CBT as consisting of the use of CBT methods (restructuring of thoughts, cognitive diamond, working with avoidance and schemata or in vivo exposure) only 28% of patients receiving psychotherapy lived up to this criterion, and only 7% of patients had worked with trauma-focused exposure (visualised or interoceptive) three or more times.
Overall, the mean duration of treatment was about 6 months for all four groups, although the therapy group received slightly shorter treatment of only 5.2 months. By the end of the trial, a total of 7% of patients were in treatment with benzodiazepines and 7% with antipsychotics. In the waiting list control group, this was slightly higher (13%). No patients were re-categorised but included as receiving planned treatment in the intention-to-treat analyses.
Outcomes
Table 2 shows pre- and post-treatment scores for the four groups. Preliminary FIML analyses of the post-treatment scores adjusted for pre-treatment scores showed no significant interactions between the two treatments for the primary outcome measure HTQ or any of the secondary outcomes. Analyses of pre-treatment scores in models including main effects of the two treatments showed that HRSD pre-treatment scores were significantly higher in patients receiving medicine (P<0.04). Apart from that there were no significant differences among the groups in pre-treatment scores. Analyses of post-treatment scores in models including main effects of the two treatments, but not pre-treatment scores showed no significant effects of psychotherapy or medicine. Finally, FIML models including main effects of the two treatments and adjustment for pre-treatment scores showed no significant effects of psychotherapy, whereas treatment with antidepressants in combination with psychoeducation was associated with significant improvements on HRSD scores (P<0.02). Figure 2 illustrates the significant changes graphically. These effects remained significant when adjusted for the potential confounders, country and language.
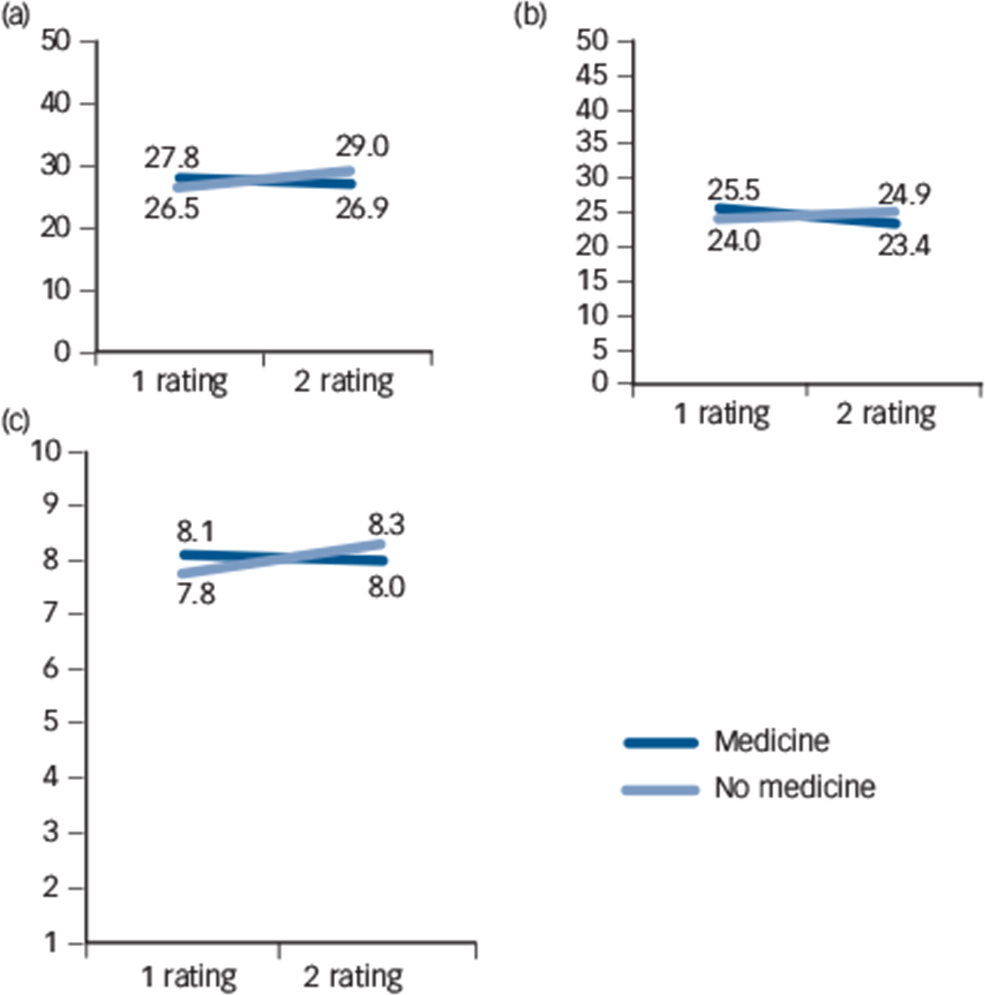
Fig. 2 Significant differences in effect size between group receiving medicine and group not receiving medicine. (a) Masked observer-rating of anxiety (Hamilton Rating Scale for Anxiety); (b) Masked observer-rating of depression (Hamilton Rating Scale for Depression); (c) Self-rating of level of functioning (Sheehan Disability Scale).
Effect sizes (Cohen's d) were calculated as the ratio of the post-treatment regression coefficients to the pre-treatment standard deviation. Corresponding to the non-significant effects, the effect sizes were generally small. For HRSD, the regression coefficient was 1.91 and Cohen's d was 0.32.
At the end of the treatment, 88% thought their condition had changed for the better because of treatment. Only one patient (in the medicine only group) thought their condition had worsened during treatment and 13% thought that improvement in their condition was because of factors other than treatment.
Adverse reactions
Both sertraline and mianserin have been thoroughly tested for their safety in other settings. In this trial, we only registered adverse reactions not listed in the product summary. Furthermore, planned admission to hospital was not considered a serious adverse event. Overall, 75% of patients treated with sertraline and 70% of patients treated with mianserin reported known or unknown adverse reactions. Only 13% had unknown adverse reactions. By the end of the trial, 11% of patients treated with sertraline had discontinued the treatment because of adverse reactions and 16% of patients discontinued treatment with mianserin. In the groups receiving psychotherapy, 10% of patients reported discomfort because of the CBT.
Discussion
In the present study, which to our knowledge is the largest effectiveness trial on the treatment of traumatised refugees in a Western setting, we found no effect of flexible CBT and antidepressants on PTSD. We found a significant, but small improvement in observer-rated symptoms of depression in patients receiving treatment with sertraline, mianserin and psychoeducation. We found no effect of psychotherapy and no interaction between treatment with psychotherapy and medicine. It is difficult to evaluate whether the small changes observed on HRSD are clinically and functionally meaningful as most patients remain above cut-off for depression on the rating after treatment. Given the number of statistical tests, the small effect observed on HRSD may be a type 1 error, although the known antidepressive effects of the medication suggest that this is not the case.
All previous randomised controlled trials (RCTs) on this patient population have been based on much smaller patient samples in each treatment arm. Reference Crumlish and O'Rourke6 An advantage of our current study is the inclusion of a waiting list control and a comparison of each treatment alone with a combination treatment. This helps to establish the effect of the various modalities separately given that to date no ‘standard treatment’ exists. In this study, we compared active treatment with a waiting list, where patients continued pre-trial treatment during the study period, meaning that 32% of patients received antidepressants including trial drugs and 13% were in treatment with antipsychotics. Using a 2 × 2 factorial design is also a cost-effective way of undertaking resource-demanding research on a complex patient group. Finally, this is a pragmatic trial, meaning that treatment is implemented under realistic circumstances and not in an expert environment or with a group of patients selected for their cultural background or lack of comorbid diseases. Very few exclusion criteria were used so that the patients included would be more representative of real-world patients receiving treatment at a trauma clinic where patients have chronic mental health problems (see Tables 1 and 2), several comorbidities and have been in treatment before. Thus, many of those included patients would have been excluded from a PTSD efficacy trial. The design, however, also means that it is not possible to separate the effect of the individual treatment elements such as psychoeducation, sertraline and mianserinin in the group receiving medicine.
Although an effort has been made to follow the CONSORT guidelines for pragmatic RCTs, the study suffers from certain methodological challenges. We did not find it possible to mask health professionals and patients to the treatment, and even though treatment was manualised there was some variability in the treatment offered, because of adverse reactions, high cancellation rates of sessions by the patients, and that patients in the group receiving only psychotherapy and the group on the waiting list continued their previous medical treatment during the trial. This resulted in low total numbers of sessions, low maximum dose of medicine and crossover between groups. There was a higher drop-out rate in the waiting list group and treatment was often delayed after the initial screening and rating, and ratings often were delayed after treatment had ended. However, the results are very consistent and clear, so the few extra patients who dropped out of treatment are unlikely to have influenced the outcome of the study, and given that there was no change in the waiting list group, it is unlikely that delay in the initiation of treatment has affected the treatment results. We used rating scales that had been validated in other populations with the same language, but we did not validate the ratings specifically in our study sample. Thus, it is unknown how the self-ratings have been influenced by culture and language differences, which may have decreased the sensitivity of self-report instruments to detect minor improvements. This is suggested by the fact that improvement was detected on masked HRSD observer-ratings, but not on the HSCL-25 self-report anxiety and depression scales. A supplementary analysis only including patients who completed the assigned treatment showed significant effects of medication for both HRSD and HRSA (data not shown).
Our primary outcome measure was self-reported PTSD which may also have been less sensitive than observer-assessed PTSD. It is a general problem that scales used in refugee studies are poorly validated, although a review of assessment scales found HTQ to be one of the better symptom scales in this field. Reference Hollifield, Warner, Lian, Krakow, Jenkins and Kesler38 Treatment adherence was monitored by counting sertraline and mianserin tablets returned at each appointment with the physician and the methods used in psychotherapy were registered at each session. However, the patients often forgot to bring their medicine so an accurate accounting of adherence was not possible for many patients. The effect size (Cohen's d) observed for HRSD was small compared with other trials on the effects of antidepressants on PTSD. Reference Stein, Ipser and Seedat3,Reference Ferreri, Lavergne, Berlin, Payan and Puech39,Reference Chung, Min, Jun, Kim, Kim and Jun40 Few of these studies, however, have focused on patient populations with the multitude of mental health, somatic and social problems as patients seen in this study.
The lack of effect of psychotherapy may reflect various limitations in the study and the psychotherapeutic treatment implemented. The psychotherapy offered was of fairly short duration. Reference Otto, Hinton, Korbly, Chea, Ba and Gershuny8,Reference Neuner, Onyut, Ertl, Odenwald, Schauer and Elbert12–Reference Hinton, Pham, Tran, Safren, Otto and Pollack15,Reference Paunovic and Ost17,Reference Palic and Elklit20 Translation takes time and given that 54% of sessions were translated; the limited length of sessions may very well have affected the results of the trial. Only 25% of psychotherapy patients received exposure treatment and the majority of patients were only exposed to trauma once or twice. The rare use of exposure was because of both patients who did not want to try this method and the reluctance of therapists who also had problems identifying which trauma to expose the patient to in cases of multiple trauma over long periods of time. The psychotherapy was not culturally adapted as patients from diverse cultural backgrounds were included in the trial. This may have influenced results as cultural adapted therapy has shown positive results in Indochinese patients. Reference Hinton, Chhean, Pich, Safren, Hofmann and Pollack14,Reference Hinton, Pham, Tran, Safren, Otto and Pollack15 Finally, the psychotherapy was targeted at treating PTSD, but the patients had several other disorders including depression, somatisation, anxiety, enduring personality change, psychotic symptoms, long-term consequences of traumatic brain injury, pain and other types of somatic disease. The patients in the trial had very severe PTSD. That their condition is chronic and treatment-resistant was evident from the low level of functioning and quality of life at baseline in spite of the long time the patients had been settled in Denmark and the fact that the majority of patients had been unsuccessfully treated with antidepressants or other psychiatric treatment previously. Therefore, the duration of treatment might have been too short as CBT treatment for personality disorder, for instance, typically follows a course of 12–18 months' duration.
No serious adverse events or reactions were observed, which is to be expected considering that the drugs have been well tested in a variety of other settings. However, a high number of patients stopped medicine before the end of the trial because of side-effects. This could possibly be because of differences in the CYP450 system and pharmacodynamics, which have been shown to differ in transcultural populations. Reference Noerregaard41 However, the maximum dose reached in all groups treated with antidepressants was low compared with other studies. Reference Friedman, Marmar, Baker, Sikes and Farfel42,Reference Panahi, Moghaddam, Sahebkar, Nazari, Beiraghdar and Karami43 It would have been an obvious advantage if the medicine adherence of patients and serum concentrations had been checked with blood samples.
Patients were comparable to other Danish clinical studies of traumatised refugees with regard to pre-treatment ratings, trauma background, socioeconomic factors and psychopathology, Reference Carlsson, Mortensen and Kastrup19,Reference Palic and Elklit20 and the trial therefore has high external representativeness. The settings under which the trial took place are representative of treatment conditions in the psychiatric healthcare system and the treatment in the trial is well defined and thoroughly described. These trial settings and the flexibility in treatment manuals are well suited to evaluate the effectiveness of this standard treatment in a clinical setting given that previously published trials were either conducted in highly specialised settings or in post-conflict countries. There were very different patient populations in other studies as the majority of RCTs on traumatised refugees are either evaluating treatment of Indochinese patients in North America or African patients in their region of origin. Reference Neuner, Onyut, Ertl, Odenwald, Schauer and Elbert12–Reference Hinton, Pham, Tran, Safren, Otto and Pollack15
In contrast to other studies on traumatised refugee populations, we found a limited effect of sertraline and mianserin treatment on level of functioning, depression and anxiety, and no effect of treatment on PTSD in a pragmatic clinical setting. However, no published trials with traumatised refugees had a waiting list control group and the few medical trials published regarding traumatised refugees compared treatment as usual with another treatment. Reference Otto, Hinton, Korbly, Chea, Ba and Gershuny8,Reference Smajkic, Weine, Djuric-Bijedic, Boskailo, Lewis and Pavkovic9,Reference Neuner, Onyut, Ertl, Odenwald, Schauer and Elbert12 We found no effect of CBT as implemented in this trial and there is no interaction between treatment with antidepressants and psychotherapy and no added effect of psychotherapy, whereas a smaller previous trial comparing CBT with CBT and sertraline found a larger effect of combination treatment. Reference Otto, Hinton, Korbly, Chea, Ba and Gershuny8
This study provides important knowledge about the treatment of traumatised refugees. The study covers a severely traumatised population with scores at the high end of the PTSD and depression scales and with substantial impairment and complex trauma histories. The provision of flexible CBT over an average of 12 sessions and treatment with antidepressants resulted in no symptom improvement for the primary target of PTSD, but medication had a minor impact on clinically rated depression. The psychotherapists found it difficult to implement prolonged exposure therapy, and there is an urgent need for the mental health community involved in the care of highly traumatised refugee populations to find effective models of clinical intervention, which can be implemented in real-world clinical settings.
Acknowledgements
We thank all patients and employees at Competence Center for Transcultural Psychiatry for making this study possible and Brian L Odlaug for proofreading the manuscript.







eLetters
No eLetters have been published for this article.