Findings from the Global Burden of Disease Study 2010, a comprehensive analysis of burden for 291 diseases and injuries and 67 risk factors, showed that mental and substance use disorders were responsible for 7.4% of global disability-adjusted life-years (DALYs) and 22.9% of global years lived with disability (YLDs), ranking 5th and 1st respectively (Reference Whiteford, Degenhardt and RehmWhiteford 2013, Reference Whiteford, Ferrari and Degenhardt2015). Some argue that these are underestimates and figures should be 13.0% of DALYs and 32.4% of years lived with disability (Reference Vigo, Thornicroft and AtunVigo 2016). Furthermore, there are important regional variations. Mental disorder DALYs are higher in Europe and highest in North Africa and the Middle East; substance use disorder DALYs are highest in Eastern Europe and Central Asia (Reference Whiteford, Ferrari and DegenhardtWhiteford 2015). Yet despite this burden, only a minority of people with mental disorders in high-income counties receive adequate treatment (Reference Kessler, Berglund and BruceKessler 2001). Treatment in low- and middle-income countries is much lower still (World Health Organization 2013). This treatment gap exists because of high stigma, low help-seeking, low recognition, low resources and lack of acceptable treatments offered promptly (Reference Clement, Schauman and GrahamClement 2015). Many sufferers do not recognise their own condition as warranting attention, do not think that treatment will be effective and wait 8 years or more to ask for help (Reference Kessler, Berglund and BruceKessler 2001).
Equally alarming is that patients with current or past mental disorders have accelerated mortality. One meta-analysis showed that the relative risk of mortality in those with mental disorders is 2.22 (95% CI 2.12–2.33), accounting for a median 10 years of life lost and 14.3% of deaths worldwide (8 million deaths each year) (Reference Walker, McGee and DrussWalker 2015). At least two-thirds of deaths among people with mental disorders are due to natural causes and about one in five to unnatural ones. Although progress has been made in reducing unnatural deaths (violent deaths and suicide) in this group, between 1982 and 2006 the risk of premature death due to cardiovascular disease more than doubled in comparison with that of the general population (Reference Brown, Kim and MitchellBrown 2010). The mental health mortality gap between observed and expected deaths has not improved despite increased recognition of the importance of physical comorbidity. Many factors, including background, lifestyle, economic disadvantage, unhelpful health behaviours (especially smoking), and difficulties accessing and adhering to medical treatments, are thought to contribute to premature mortality in severe mental illness (SMI) such as schizophrenia (Reference Olfson, Gerhard and HuangOlfson 2015). Mental health professionals may have unwittingly increased the risk of medical conditions, and possibly mortality, by recommending a variety of psychotropic drugs that contribute to cardiovascular disease, diabetes and obesity (Reference Mitchell, Vancampfort and SweersMitchell 2013a). However, the link between antipsychotics and premature mortality is complex (Reference Torniainen, Mittendorfer-Rutz and TanskanenTorniainen 2015). Adults with mental illness are also less likely than age-matched peers to receive adequate treatment for major medical conditions, which may compound risk of premature mortality (Reference Mitchell, Lord and MaloneMitchell 2012a; Reference Woodhead, Ashworth and BroadbentWoodhead 2016). In some cases, unequal quality of healthcare provision may explain much of the subsequent excess mortality (Reference Mitchell and LordMitchell 2010; Reference Druss, Bradford and RosenheckDruss 2011). Many people with physical health problems also have mental health problems and vice versa, yet medical science and training often fail to integrate these and teach the importance of comorbidity. Indeed, in all settings, but perhaps particularly in primary care, it is multiple morbidity that remains an unresolved challenge and a key barrier to achieving parity (Reference Mujica-Mota, Roberts and AbelMujica-Mota 2015; Reference Paddison, Saunders and AbelPaddison 2015). The aim of this article is to review the concept of parity of esteem as applied to mental–physical comorbidity.
The concept of parity of esteem
Given the headlines that mental disorders feature greater illness burden, greater mortality but lower treatment uptake than physical disorders, many have called for at least comparable attention to that given to major medical disorders. This is called parity of esteem: an initiative that recognises and aims to address inequalities between physical and mental healthcare, including preventable premature deaths (the mortality gap), lower-quality medical care (the treatment gap) and inferior resources for mental healthcare relative to the impact of mental health problems (the funding gap). In simple terms, parity of esteem refers to the concept that society should value mental health to the same degree that it values physical health.
In the USA, parity became law in 1996 under the Mental Health Parity Act (MHPA) and later under the Mental Health Parity and Addiction Equity Act (MHPAEA) of 2008. The MHPAEA requires that limits on mental health insurance benefits be no lower than any such limits on medical and surgical benefits. Reference Fleischhacker, Cetkovich-Bakmas and De HertFleischhacker et al (2008) suggested that parity in healthcare for people with mental illness should be regarded as a basic human right.
In the UK, the Equality Act 2010 placed a legal responsibility on health services to make reasonable adjustments to ensure that people with SMI are not disadvantaged compared with the general population in accessing healthcare. Parity was formally proposed in the 2011 governmental mental health strategy for England ‘No Health without Mental Health’. However, the concept was not well understood and implementation was slow. Consequently, the Department of Health asked the Royal College of Psychiatrists to develop a vision for ‘parity of esteem’ (Box 1), which was disseminated in 2013 (Royal College of Psychiatrists 2013). In February 2016, NHS England's Mental Health Taskforce produced a report and recommendations on mental healthcare (Mental Health Taskforce 2016).
BOX 1 Royal College of Psychiatrists’ definition of parity of esteem
Compared with physical healthcare, mental healthcare should be characterised by:
-
• equal access to effective, safe care
-
• equal efforts to improve the quality of care
-
• the allocation of resources on a basis commensurate with need
-
• equal status within healthcare education and practice
-
• equally high aspirations for patients
-
• equal status in the measurement of health outcomes
-
• holistic, integrated care with mental health considered alongside physical health
Parity of esteem can be viewed from the perspective of patients (the right to equal standards of quality of care in both mental and physical health), from the perspective of clinicians (equal focus on both mental and physical health) and from the perspective of commissioners (providers should devote the same time and resources to improving mental health as they do to physical health). In 2014, NHS England established a Parity of Esteem Programme. Mainly aimed at commissioners, its purpose is to focus effort and resources on improving clinical services and health outcomes (NHS England 2014). This has led to a call to action and payment incentives through the Commissioning for Quality and Innovation (CQUIN) framework to improve physical health in severe mental illness. In 2014, the British Medial Association (BMA) published a report on parity of outcomes that sets out steps that need to be taken in the following key areas (BMA Science and Education Department 2014):
-
• promoting prevention and early intervention strategies
-
• delivering ‘joined-up’ care
-
• enhancing training and workforce planning
-
• encouraging a greater research focus on mental–physical multimorbidity.
Examples of gaps in parity of esteem (inequalities in care)
Inequalities in mass screening
Inequalities in medical care of people with mental illness have been documented in preventive mass screening procedures. Reference Lord, Malone and MitchellLord et al (2010) reviewed 61 comparisons of preventive care, from 26 studies across Europe and North America, in individuals with and without psychiatric illness. Twenty-seven comparisons revealed inferior preventive healthcare in those with mental illness; conversely, 10 suggested superior preventive healthcare, and 24 reached inconclusive findings. However, in a more refined analysis focusing on mammography, Mitchell and colleagues found significantly reduced rates of mammography screening in women with mental illness (OR = 0.71, 95% CI 0.66–0.77), particularly SMI (OR = 0.54, 95% CI 0.45–0.65), not due to distress alone, but rather related to the diagnosis of mental illness itself (Reference Mitchell, Pereira and YadegarfarMitchell 2014).
Inequalities in dental care
People with SMI have higher rates of smoking and higher sugar intake (e.g. carbonated drinks). Patients brush their teeth infrequently and attend the dentist less often than the general population (Reference McCreadie, Stevens and HendersonMcCreadie 2004). A review of 57 studies reported a 61% lifetime prevalence of poor oral health and twice the rate of decayed, missing or filled teeth (Reference Wey, Loh and DossWey 2016). People with SMI have three times the odds of having lost all their teeth than the general community (Reference Kisely, Quek and PaisKisley 2011).
Inequalities in medical care
Several valuable reviews have highlighted the extent of inequalities in medical care (Reference Mitchell, Malone and DoebbelingMitchell 2009; Reference Lawrence and KiselyLawrence 2010; Reference Moore, Shiers and DalyMoore 2015). Inequalities are most notable in cardiovascular and diabetes care: for example, in primary care those with schizophrenia are less likely to have a record of cardiovascular disease (suggesting under-recognition) (Reference Smith, Langan and McLeanSmith 2013). One explanation is that these inequalities result from low attendance or adherence. Yet many people with mental ill health, in particular those with depressive disorders, seek help more often and use more general healthcare resources than those who are not unwell (Reference Stein, Cox and AfifiStein 2006; Reference Baune, Adrian and JacobiBaune 2007). Even when attendance is high, quality of care can be low (Reference Jones and CarneyJones 2005; Reference Salsberry, Chipps and KennedySalsberry 2005). Therefore predictors of adequate care should include measures of both quality and quantity, and deficits in either may result in failing care. Clinicians’ low confidence or knowledge regarding mental–physical comorbidity may also compromise medical care for this vulnerable population.
Inequalities in surgical care
Having a diagnosis of schizophrenia is linked to poor surgical outcomes. In a review of appendectomies in people with schizophrenia in the USA, Reference Cooke, Magas and VirgoCooke et al (2007) found that they presented late in the natural course of the illness (80% with advanced appendicitis, perforated or gangrenous at the time of surgery). Morbidity and mortality rates were much higher than in the control group. A systematic review and meta-analysis has confirmed that schizophrenia is associated with an increased rate of fractures (Reference Stubbs, Gaughran and MitchellStubbs 2015). In a US survey, SMI was also associated with higher odds of in-hospital post-operative complications following total hip or knee arthroplasty, with the rate of adverse events being most highly associated with a diagnosis of schizophrenia (Reference Buller, Best and KlikaBuller 2015). Similarly, two large studies from Taiwan and Japan showed significantly higher postoperative adverse outcomes, possibly with increased mortality, in people with schizophrenia when compared with those without mental disorders (Reference Liao, Shen and ChangLiao 2013; Reference Maeda, Babazono and NishiMaeda 2014).
Inequalities in assessing and monitoring comorbid physical ill health
Although there are many reasons for inequalities in mortality and morbidity, those relating to the attitudes and behaviour of clinicians are most concerning. For example, negative attitudes towards people with mental illness held by health-care professionals may mean that some physical symptoms are wrongly ignored or are attributed to mental disorder (Reference Thornicroft, Rose and KassamThornicroft 2007). In a survey of nearly 800 people living with schizophrenia in 27 European countries, 17% felt that they experienced discrimination when treated for physical health problems (Reference Harangozo, Reneses and BrohanHarangozo 2013). Similarly, a North American survey of 250 people with schizophrenia reported that 49% believed that doctors took their medical problems less seriously after discovering that they had a psychiatric diagnosis (National Alliance on Mental Illness 2008). A national survey in primary care in England showed that the percentage of patients who received the identical medical checks (body mass index, blood pressure, blood glucose and cholesterol) in the previous 15 months was much higher among patients with diabetes than those with SMI (97.3% v. 74.7%, P <0.001) (Reference Mitchell and HardyMitchell 2013b).
To improve this situation, numerous national and international guidelines have been published for the monitoring of physical health in people with mental illness (Reference De Hert, Vancampfort and CorrellDe Hert 2011). However, a recent review showed considerable variation in the level of detail, methodology and recommendations (such as timing of monitoring and proposed therapeutic interventions) (Reference Mitchell, Delaffon and VancampfortMitchell 2012b). In the UK, the National Institute for Health and Care Excellence (NICE) recommends annual monitoring of physical health for people with established psychosis (National Collaborating Centre for Mental Health 2014). NICE recommends more frequent monitoring by mental health services in the first year of a psychotic illness, with the responsibility subsequently transferred to primary care under shared-care arrangements. Numerous studies from the field of early intervention suggest that early physical health intervention and health promotion for patients with mental illness are likely to be the most important type of intervention (Reference Mitchell and De HertMitchell 2015a). The good news is that screening for physical comorbidity in SMI has indeed improved, but the bad news is that (with exceptions) it is still generally deficient (Reference Baller, McGinty and AzrinBaller 2015). For example, in the UK National Audit of Schizophrenia, a 12-month retrospective review was performed of the case records of 5091 people with a diagnosis of schizophrenia or schizoaffective disorder attending community mental health services in England and Wales. Data were collected on nine key aspects of physical health. Physical health monitoring was poor, with less than 25% of patients having all nine parameters documented; and where problems were identified, treatment was rarely offered (Reference Crawford, Jayakumar and LemmeyCrawford 2014).
Failure to address metabolic complications in psychiatric care
Data from the National Ambulatory Medical Care Survey from 1992 to 1996 in the USA found that, in 1600 office visits of patients with mental illness who were documented smokers, psychiatrists offered smoking-cessation counselling at 12% of the visits, and diet and exercise counselling at 6% and 4% of visits respectively (Reference Himelhoch and DaumitHimelhoch 2003). A more recent meta-analysis of comparative studies found equivalent rates of smoking-cessation advice given to medical v. psychiatric patients (Reference Mitchell, Vancampfort and De HertMitchell 2015b). This may appear to be an improvement, but as smoking is approximately twice as common in patients with mental illness the level of advice for this group should also be double.
It is clear that, if inequalities are to be addressed, clinicians must respond to physical health problems in patients with mental illness when they are discovered. Unfortunately, this often does not happen. In the largest controlled study of its type, Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE), 88% of patients with dyslipidaemia were untreated, as were 62% with hypertension and 38% with diabetes (Reference Nasrallah, Meyer and GoffNasrallah 2006). Reference Correll, Kane and ManuCorrell et al (2008) found that 62% of patients treated with second-generation (atypical) antipsychotics who had elevated low-density lipoprotein (LDL) levels did not receive medical treatment, despite the fact that they were in-patients. Reference Bernardo, Cañas and BanegasBernardo et al (2009) found that among in-patients with schizophrenia, only 60% of those with diabetes, 28% of those with hypertension and 14% of those with dyslipidaemia received active medical treatment. Several sources of evidence suggest that psychiatrists are slow to change drugs linked with metabolic syndrome even after complications occur (Reference Hermes, Sernyak and RosenheckHermes 2013). For example, in a multi-centre study in Denmark and Sweden, in consecutively screened in- and outpatients with schizophrenia spectrum disorders continuously treated for at least 3 months with atypical antipsychotics, the high rate of metabolic syndrome did not elicit much decisive action on the part of the treating psychiatrists (Reference Larsen, Fagerquist and HoldrupLarsen 2011). The most frequent action taken was dietary and exercise advice (for 75% of patients), while a laboratory or blood pressure follow-up was advised for 54% and 19% of patients respectively. Change of antipsychotic was recommended for only 10% of patients, and no action was taken for a further 11%.
Improving parity of esteem
Improving the physical health of patients with SMI
Population-based initiatives are promising but rare, although there is some evidence that fluoridated water reduces inequality in dental care for people with SMI (Reference Kisely, Quek and PaisKisely 2011). An initial Cochrane review in 2010 was unable to find a single randomised controlled trial reporting evidence on the effectiveness or cost-effectiveness of guidelines advising on the monitoring of physical health in people with severe mental health problems (Reference Tosh, Clifton and MalaTosh 2010). Since then there have been several randomised trials on programmes to prevent physical ill health in people with mental disorders, largely by addressing risk factors. These risk factors tend to exacerbate with time if not addressed (Reference Heald, Martin and PaytonHeald 2016). Interventions have focused on smoking cessation, weight management, glucose control or broader lifestyle intervention in depression/anxiety and SMI (Reference Barnett, Wong and HallBarnett 2008; Reference Park, McDaid and WeiserPark 2013; Reference Bruins, Jörg and BruggemanBruins 2014; Reference Vancampfort, Rosenbaum and SchuchVancampfort 2016; Reference Taylor, Stubbs and HewittTaylor 2017). One recent meta-analysis (Reference Park, McDaid and WeiserPark 2013) found that the drop-out rate was modest and a second found that overall, lifestyle interventions were effective in both weight loss and prevention of weight gain (Reference Vancampfort, Rosenbaum and SchuchVancampfort 2015). Reference Bruins, Jörg and BruggemanBruins et al (2014) identified 10 studies reporting on cardiometabolic risk factors, and these showed that lifestyle interventions led to significant improvements in waist circumference, triglycerides, fasting glucose and insulin, but not blood pressure and cholesterol. Two trials (Reference Bartels, Pratt and AschbrennerBartels 2013; Reference Green, Yarborough and LeoGreen 2015) found different outcomes. The In SHAPE trial focused on exercise (12 months of weekly sessions with a fitness trainer plus gym membership) (Reference Bartels, Pratt and AschbrennerBartels 2013). The prospective primary outcome was weight loss and the secondary outcomes were fitness, blood pressure, lipids and programme adherence. There was a clinically significant reduction in cardiovascular risk in 49% of participants and improvements in fitness and diet, but not in weight. In the STRIDE trial, participants attended weekly groups providing moderate exercise and dietary advice and achieved an average 4.4 kg weight loss over 6 months, but gained some of this weight back during the maintenance phase (Reference Green, Yarborough and LeoGreen 2015). More recently, the CHANGE trial failed to find a benefit of lifestyle coaching on 10-year risk of cardiovascular disease in patients with schizophrenia spectrum disorders and abdominal obesity (Reference Speyer, Brix Nørgaard and BirkSpeyer 2016).
Given the heterogeneity in outcomes, lessons from lifestyle intervention for other conditions, such as diabetes, may be warranted. For example, successful programmes tend to have multiple strategies (nutrition and physical activity), face-to-face contact, longer duration, longer follow-up and trained treatment providers (Reference Ward, White and DrussWard 2015). However, the biggest lesson is that the later we leave intervention for physical comorbidities such as obesity, the poorer the outcomes. The gold standard is prevention (Reference Moore, Shiers and DalyMoore 2015; Reference Mitchell and De HertMitchell 2015a). Therefore, the challenge is to recognise that all patients with SMI, and many with other mental health conditions, are at risk of physical complications and all such patients need a great deal of help and support to avoid weight gain, smoking, inactivity and frank metabolic conditions such as diabetes. Tools have been developed to assist healthcare professionals, for example, the Lester UK Adaptation of the Positive Cardiometabolic Health Resource (produced through collaboration between the Royal Colleges of General Practitioners and Psychiatrists and supported by the National Audit of Schizophrenia). This resource has been trialed in the Advancing Quality Alliance (AQuA) ‘Don't Just Screen – Intervene’ initiative across five early-onset psychosis services and it increased cardiometabolic risk-screening from 10 to 63% (Reference Greenwood and ShiersGreenwood 2016). Specific resources to assist mental health nurses (Reference White, Gray and JonesWhite 2009) and general practice nurses (Reference HardyHardy 2015a) have also been available in the UK for a number of years.
Integrating mental and physical healthcare services
A recent King's Fund report (Reference Naylor, Das and RossNaylor 2016) emphasised the need to bring together physical and mental healthcare, rather than bridging the gaps between health and social care or between primary and secondary care. It identified ten priority areas for improvement (Fig. 1) and encouraged this through the following:
-
• vanguard sites led by NHS England, with integrated approaches to physical and mental health
-
• all health and social care professionals have a part to play in taking a ‘whole-person’ approach to physical and mental health
-
• medical Royal Colleges should redesign curricula so that all health professionals have a common foundation in mental as well as physical healthFootnote †
-
• local authorities should assess how mental health and well-being interact with other public health priorities
-
• commissioners should take advantage of new payment systems and contracting approaches to overcome some of the current barriers to integration
-
• mental health trusts should consider having a board-level champion for physical health, and vice versa in acute trusts.
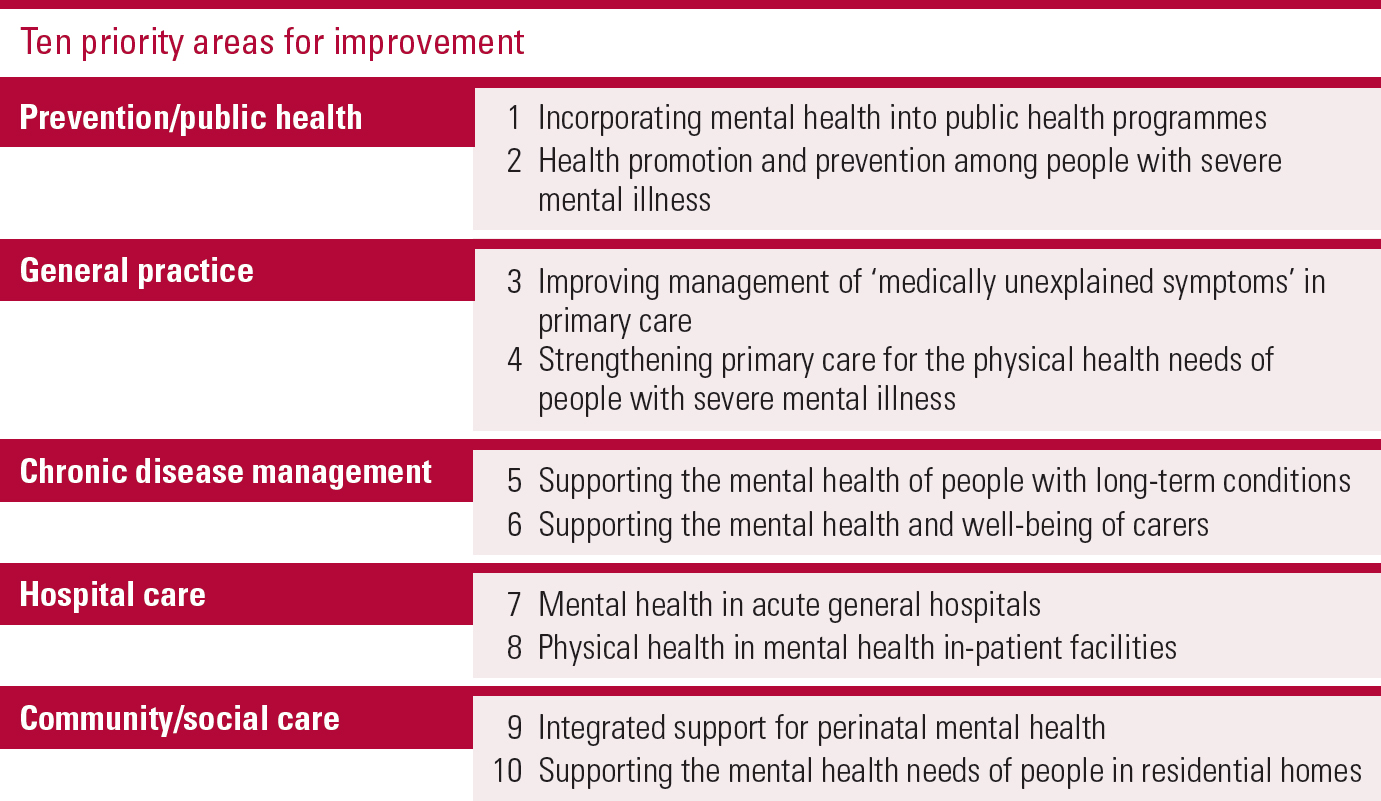
FIG 1 Ten priority areas for improvement in mental healthcare (from Reference Naylor, Das and RossNaylor et al (2016), redrawn with permission of The King's Fund).
Encouraging health-seeking behaviour
A Healthwatch briefing published in February 2016 stated that 77 out of the 152 local Healthwatch groups reported that mental health was the most important health and social care priority to their local people (Healthwatch England 2016). Its authors suggested that engaging individuals in their own care makes a real difference in enabling mental health services to deliver for people.
Help-seeking is influenced by stigma. There have been attempts to address inequalities by initiatives to reduce stigma in the general population, with the expectation that this would influence help-seeking and clinicians’ attitudes (Time to Change 2008). However, there is limited evidence that stigma interventions are effective in reducing perceived or self-stigma (Reference Griffiths, Carron-Arthur and ParsonsGriffiths 2014); this suggests that there is a need for healthcare services to take a much more proactive approach in encouraging and assisting people with mental illness to access appropriate care and treatment. Recognising this, the British Medical Association (BMA) has developed pragmatic recommendations in three areas: mortality, prevention and early intervention, and training and workforce planning (Box 2).
BOX 2 Summary of the British Medical Association's parity of esteem recommendations
Mortality
-
• A national mortality review system should be implemented across the UK
Promoting prevention and early intervention strategies
-
• The integration of intellectual disability, mental and physical healthcare should be improved
-
• The wider application of the collaborative care model should be explored
-
• To strengthen collaborative care, generalists in and out of hospitals should work closely with a multidisciplinary team to support patients with co- or multi-morbidities in a more integrated way
-
• A liaison psychiatry service (including paediatric, intellectual disability and older adult liaison) should be made available in all hospitals
-
• Mental health trusts should appoint a liaison physician (in psychiatric wards) to support the physical health needs of hospital in-patients with mental health problems and intellectual disabilities
-
• Health professionals with responsibilities for commissioning and/or public health should ensure that they place equal value on mental and physical health when setting their commissioning priorities
-
• Mental health should be integrated into all aspects of the work of commissioners and public health directors
-
• Commissioners must have accurate, accessible information on the physical, mental and intellectual disability needs of the population that they are serving
-
• It is strongly recommended that commissioning bodies should ensure that at least one commissioner is a mental health and/or intellectual disability professional
-
• Healthcare providers must ensure that they are compliant with their duties under the Equality Act 2010
-
• Providers’ compliance with legislation and guidelines should be monitored by healthcare regulators and inspectors such as Monitor and Healthcare Improvement Scotland
Training and workforce planning
-
• Undergraduate and postgraduate medical training should shift from teaching mental health separately in a ‘module’ format to integrating mental health and intellectual disability into the core curriculum
-
• There should be adequate workforce planning to ensure that all Foundation Programme doctors and general practitioners (GPs) in training have a placement in psychiatry, liaison psychiatry or intellectual disability – this is an area for action for the Royal College of Psychiatrists and the Royal College of General Practitioners
-
• All doctors should understand diagnostic overshadowing, comorbidity problems and the requirements of the Mental Capacity Act 2005 and the Equality Act 2010
-
• All healthcare professionals should undertake mental health and intellectual disability awareness training as part of their continuing professional development
(Adapted from: BMA Science and Education Department, BMA Board of Science 2014)
Addressing and improving the mortality gap
Addressing the mortality gap requires a comprehensive series of changes rather than change in one particular disparity. The BMA recommends that a national mortality review system be implemented across the UK (Box 2). This would make information available to healthcare providers about the circumstances of deaths and the care provided in the period leading up to a death. Similarly, the Mental Health Taskforce recommends that NHS England should define a quantified national reduction in premature mortality among people with SMI, and an operational plan to begin achieving it from 2017/2018 (Mental Health Taskforce 2016). Failures in care or systems could then be addressed to prevent deaths and improve services in the future.
The key reversible areas that might reduce the mortality gap include addressing unhelpful health behaviours (especially smoking), reducing metabolic risks (e.g. obesity, inactivity) before and after starting psychiatric treatment, prompt recognition and treatment of medical comorbidities and improving quality of medical care for patients with known mental illness. Unfortunately, the evidence that specific interventions reduce excess mortality in those with mental ill health is currently sparse (Reference Baxter, Harris and KhatibBaxter 2016). Two Cochrane reviews on health outcomes in people with SMI allocated to integrative community care management or intensive case management found no effect on mortality, and seven studies of lifestyle intervention in SMI found no effect on all-cause mortality (see Reference Baxter, Harris and KhatibBaxter 2016).
Promoting prevention and early intervention strategies
The BMA states that integration of intellectual disability, mental and physical healthcare should be improved (Box 2). Despite this, reform has been slow, with little evidence that inequalities are reducing (Reference Brekke, Siantz and PahwaBrekke 2013). Models of integrated care include embedding of general practitioners (GPs) or hospital specialists within mental health programmes, housing medical and mental health services together, and collaborative care between independent physical and mental healthcare providers. A number of studies involving collaborative care to address risk factors for poor health in schizophrenia have reported improvement of physical and mental quality of life (Reference Woltmann, Grogan-Kaylor and PerronWoltmann 2012), but only two (the PCARE study and the SMAHRT study) have attempted to improve medical care directly. In the PCARE study (Reference Druss, von Esenwein and ComptonDruss 2010), the intervention group received an average of 59% of recommended preventive services, compared with 22% in the usual-care group. They also received a significantly higher proportion of evidence-based services for cardiometabolic conditions (35% v. 28%) and were more likely to receive a physical examination. In the SMAHRT study (Reference Kilbourne, Goodrich and LaiKilbourne 2013), patients receiving the intervention had reduced systolic and diastolic blood pressure, as well as reduced manic symptoms. However, when collaborative care is implemented in practice, there are limited changes to processes of care, as physical health and mental health professionals often maintain their physical and mental health role boundaries (Reference Wells, Sherbourne and SchoenbaumWells 2000; Reference Knowles, Chew-Graham and CoupeKnowles 2013). In general, there is often a cultural divide between researchers, practitioners and administrators which can prevent research becoming standard clinical practice (Reference Eccles, Grimshaw and WalkerEccles 2005).
The BMA recommends that commissioners place equal value on mental and physical health when setting their commissioning priorities (Box 2), yet financial incentives for prevention in primary care within the Quality and Outcomes Framework (QOF) such as screening for depression and measuring all cardiovascular disease risk factors in people with SMI have been removed in both England and Wales (Reference Graham, Chitnis and TurnerGraham 2014). As the contacts that these patients have with GPs have reduced significantly over the past 20 years – from 13 a year (Reference Nazareth and KingNazareth 1992) to just 3 a year (Reference Reilly, Planner and HannReilly 2012) – and they have little contact with practice nurses (Reference Wells, Sherbourne and SchoenbaumWells 2000), there is not much chance to provide opportunistic screening. In psychiatric hospitals there is substantial variation in quality of care, for example, in care received by patients with schizophrenia (Reference Jørgensen, Mainz and SvendsenJørgensen 2015). This is despite the CQUIN described earlier and the option of local CQUINs. Financial incentive schemes in healthcare can lead to improvements in the quality of care for rewarded activities, but they can also lead to neglect of the non-incentivised aspects of patient care (Reference Doran, Kontopantelis and ValderasDoran 2011). Additionally, the targets of these incentives can be met and guidance can be followed without any real commitment from the organisation to making sustainable changes that will improve practice.
Overall funding for mental healthcare has suffered. Total investment in mental health services across England decreased in real terms by 1% between 2010–2011 and 2011–2012, and by 2.3% between 2011–2012 and 2013–2014, despite a 13.3% increase in the average number of referrals being handled by community mental health teams (Mental Health Strategies 2012; Reference BuchananBuchanan 2013). A report by the Mental Health Taskforce (2016) stated that, in 2013–2014, the NHS spent £9.2 billion on mental health services – less than a tenth of its budget – even though one in four people experience a mental health problem each year. The report announced that by 2020, new funding should increase access to evidence-based psychological therapies for conditions such as anxiety, depression and stress and to a screening programme to ensure that more people with severe mental health problems get help for physical health conditions such as heart disease and diabetes (as required by the Equality Act 2010). The chief executive of the mental health charity Mind, who led the taskforce, was reported to have said that, although the extra funding was crucial, some stigma around mental illness ‘still prevails, right the way inside the health service, as it does in society, and this needs to change’ (Reference TriggleTriggle 2016). There is evidence to suggest that the negative attitudes of healthcare professionals towards people with a mental illness are detrimental to recovery and reduce their use of healthcare services (Reference Horsfall, Cleary and HuntHorsfall 2010). Improving the attitudes of healthcare professionals looking after people with mental illness could have a major positive impact on the health of this group. Research has shown that educational interventions can be effective in decreasing stigmatising attitudes among healthcare professionals, especially those in general healthcare who have little or no formal mental health training (Reference Henderson, Noblett and ParkeHenderson 2014).
Training and workforce planning
The Mental Health Taskforce's report for the NHS in England suggests that Health Education England (HEE) should work with NHS England, Public Health England (PHE), professional bodies, charities, experts-by-experience and others to develop a costed multidisciplinary workforce strategy for the future shape and skills mix of the workforce that addresses training needs for both new and existing NHS-funded staff (Mental Health Taskforce 2016). It recommends that core training should include basic mental health awareness, mental health law, public mental health, compassion and communication skills, common physical health problems, shared decision-making, prevention of mental illness, empowering people to understand their own strengths and to use self-help strategies, and promote carer involvement as well as information sharing.
So far, educational initiatives funded by HEE have been regional and they have not been rolled out nationally. One example is the practice nurse project, which was led by one of us (S.H.) and funded by Health Education North Central East London (HENCEL) (Reference Hardy and KingsnorthHardy 2015b). This 10-module training developed for practice nurses covers most areas recommended by HEE and was successfully delivered by mental health nurses working in the practice nurses’ localities. Although frequently cited as an example of good practice, there has been no vehicle to disseminate it countrywide. S. H. now works one day a week with a small charity (the Charlie Waller Memorial Trust) and through this offers the course for identified trainers free of charge. She has found that organisations are very interested, but appear to struggle with setting up their own training plan. The problems are mainly due to the inability to release nurses from practice both to receive training and to train others. This suggests the need to educate commissioners as well as clinicians to enable learning to take place. A national plan as recommended by the taskforce could resolve some of these problems. Once staff have received training, organisations need to enable them to teach their peers and put their learning into practice.
Conclusions
Parity of esteem continues to be a major concern. Five years after the government's mental health strategy ‘No Health without Mental Health’ (the aim of which was to improve outcomes, physical health and experience of care for people with mental health problems and to reduce avoidable harm and stigma), a new report appeared highlighting deficits and making recommendations (Mental Health Taskforce 2016). This shows continuing inadequate provision and worsening outcomes, suggesting that policies on their own change neither practice nor provision. All clinicians need to be aware of parity of esteem, as do all commissioners. Careful planning and organisation are required so that extra funding is used to reduce inequalities in care and ultimately equalise parity of esteem between physical and mental health.
MCQs
Select the single best option for each question stem
-
1 The increased mortality among people with current or past mental disorders:
-
a is mostly attributable to suicide
-
b is exclusively due to the psychotropic drugs that contribute to cardiovascular disease
-
c is because people with mental disorders do not understand healthy eating and the benefit of exercise
-
d is due to a combination of factors, including lifestyle, economic disadvantage, unhelpful health behaviours and psychotropic drugs
-
e is because people with mental disorders do not want to stop smoking.
-
-
2 Parity of esteem is:
-
a a pledge that recognises and aims to address inequalities between physical and mental healthcare
-
b guarantee that there will be more nurses and doctors to care for people with mental disorders
-
c focus on training mental health professionals to recognise medical disorders
-
d an exercise to reduce waiting times for treatment of mental disorders
-
e law in the UK to ensure that people with mental disorders get equal care to those with physical disorders.
-
-
3 NICE recommends monitoring of physical health for people with established psychosis. In the first year of a psychotic illness, monitoring should be by:
-
a the GP or practice nurse
-
b the mental healthcare professionals treating the psychotic illness
-
c unspecified professionals
-
d any healthcare professional in contact with the patient
-
e health trainers.
-
-
4 Regarding lifestyle and severe mental illness, research has shown that:
-
a people with SMI have broadly the same rate of smoking as aged-matched population controls
-
b the majority of people with SMI are not interested in lifestyle intervention programmes
-
c lifestyle programmes do not improve risk factors in people with SMI in the short or long term
-
d drug-naive people with SMI have normal rates of smoking and hypertension
-
e successful programmes to assist people with SMI to improve lifestyle tend to have multiple strategies administered over a sustained period.
-
-
5 Training and workforce planning is one of the recommendations of the Mental Health Taskforce to the NHS in England. For new and existing NHS-funded staff, this should include:
-
a cognitive–behavioural therapy in combination with improving access to psychological therapies (IAPT)
-
b basic mental health awareness, compassion and communication skills, mental illness prevention, and empowering people to understand their own strengths and to use self-help
-
c recognised qualification and endorsement from the Royal College of Psychiatrists
-
d certificate in communication skills training
-
e access to a newly developed online parity of esteem course endorsed by the Royal College of Psychiatrists and the Royal College of Physicians.
-
MCQ answers
| 1 | d | 2 | a | 3 | b | 4 | e | 5 | b |




eLetters
No eLetters have been published for this article.